Abstract
A 47-year-old man presented with episodes of altered mental state initially felt to be complex partial seizures, but which were in fact hypoglycaemic episodes. An insulinoma was confirmed and eventually localised. He underwent an abdominal computed tomography scan and intraoperative laparoscopy, but required selective venous sampling to localise the tumour. Fifteen months after his surgery there is no evidence of recurrence of his insulinoma.
Background
Hypoglycaemia/neuroglycopaenia is sometimes overseen in patients presenting with signs of impaired brain function. An insulinoma is a rare insulin producing tumour and can be difficult to diagnose and localise. Symptoms often lead to misdiagnosis as a neurological or psychiatric disorder.
Case presentation
In November 2006, a 47-year-old man was referred to the neurology clinic for investigation of three episodes of “altered mental state”. The first episode occurred in February 2006, when his wife witnessed him become acutely confused for 5 min. He felt weak, light headed and behaved strangely, stuffing paper instead of lettuce between two slices of bread. Two similar events happened in April and October. The last episode was preceded by perioral tingling and resolved when his wife gave him some chocolate. His senses seemed heightened and he described it as the best chocolate he had ever had. He never lost consciousness, nor was there any involuntary movement.
Investigations
A full blood count, urea and electrolytes, and thyroid function test were normal. A random blood glucose was 3.2 mmol/l. An electroencephalogram (EEG) was normal and a magnetic resonance imaging (MRI) scan of the brain showed a small aneurysm of the anterior communicating artery, felt to be incidental. Initially it was felt that his attacks could be complex partial seizures and he was started on lamotrigine.
When reviewed in February 2007, the patient reported that his funny turns were occurring more frequently. His wife had noted that his attacks resolved after he was given sugary foods and she had obtained a blood glucose meter. During his most severe attack she recorded a blood sugar concentration of 1.3 mmol/l. It was concluded that his attacks were due to neuroglycopaenia and he was referred for endocrine assessment.
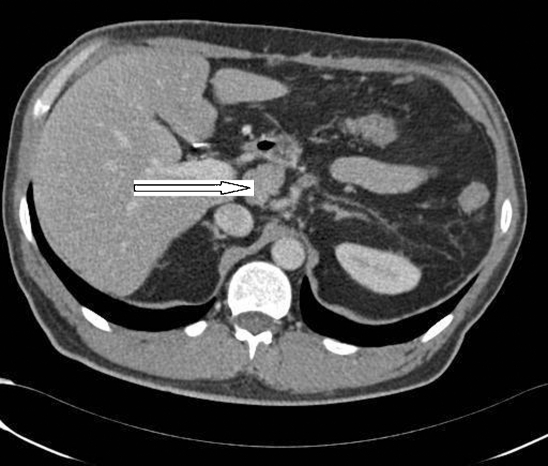
An insulinoma was confirmed by a fasting blood sugar of 1.3 mmol/l and high insulin and C peptide levels. His lamotrigine was stopped. An abdominal computed tomography (CT) scan with contrast showed the pancreas to be normal with no enhancing pancreatic mass lesion seen. However, there was a 2.6 cm soft tissue mass at the coeliac axis (fig 1) with another smaller node behind the splenic vein. An octreotide scan was unhelpful. The patient was referred to the surgeons and he underwent a laparoscopy with intraoperative ultrasound in August 2007. No masses were seen in the pancreas but a small mass was detected at the coeliac axis. He was referred for selective venous sampling, which showed high insulin and C peptide values around the area consistent with the abnormalities round the coeliac axis.
Figure 1.
2.6 cm soft tissue mass at the coeliac axis.
Treatment
He underwent distal pancreatectomy with splenectomy in January 2008.
Outcome and follow-up
Histology showed multiple insulin secreting microadenomas which appeared to have been completely excised. The patient’s serum calcium and prolactin values were checked to exclude multiple endocrine neoplasia type 1 (MEN1). The results were normal. Following his surgery, he lost about 12 kg in weight since he no longer needed to have frequent snacks. When last reviewed in April 2009, there was no evidence of recurrence of his insulinoma.
Discussion
Insulinomas are rare with an estimated incidence of four cases per million people per year. An insulinoma is the most common cause of hypoglycaemia resulting from endogenous hyperinsulinism.1 It is a curable cause of potentially lethal hypoglycaemia. In 1927, Wilder established the association between hyperinsulinism and a functional islet cell tumour.2 In 1929, Graham achieved the first surgical cure of an islet cell adenoma. Insulinomas can be difficult to diagnose. Symptoms often lead to misdiagnosis as a neurological or psychiatric disorder.3
Insulinomas are characterised clinically by the Whipple triad: episodic hypoglycaemia, central nervous system (CNS) dysfunction temporally related to hypoglycaemia (confusion, anxiety, stupor, paralysis, convulsions, coma), and dramatic reversal of CNS abnormalities by glucose administration. Weight gain occurs in 20–40% of patients.
Imaging studies should only be done after the diagnosis has been confirmed biochemically, because 80% of insulinomas are <2 cm in size and may not be visible by CT scan.
Octreotide scanning localises about half of insulinomas. Pancreatic venous sampling for insulin, via the percutaneous transhepatic route, can successfully localise insulinomas.4 Intraoperative ultrasound can be very useful in identifying occult tumours. About 90% of insulinomas are benign. They may be single or multiple tumours; 80% are solitary adenomas. Insulinomas can occur as part of MEN 1 syndrome, in association with pituitary, parathyroid, and other pancreatic islet tumours (for example, insulinomas, gastrinomas). Less than 10% of insulinomas are associated with MEN-1.
Insulinoma resection achieves cure in 90% of patients and is the therapy of choice.5 Medical treatment with diazoxide or octreotide is indicated in patients with malignant insulinomas and in those who will not or cannot undergo surgery. These measures are designed to prevent hypoglycaemia and, in patients with malignant tumours, to reduce the tumour burden.
Learning points
Hypoglycaemia/neuroglycopaenia is sometimes overlooked in patients presenting with signs of impaired brain function.
An insulinoma is a rare insulin producing tumour and can be difficult to diagnose and localise.
Symptoms often lead to misdiagnosis as a neurological or psychiatric disorder.
Insulinoma resection achieves cure in 90% of patients and is the treatment of choice.
Footnotes
Competing interests: None.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Service FJ. Hypoglycemic disorders. N Engl J Med 1995; 332: 1144–52 [DOI] [PubMed] [Google Scholar]
- 2.Wilder RM, Allan FN, Power MH, et al. Carcinoma of the islands of the pancreas. JAMA 1927; 89: 348 [Google Scholar]
- 3.Dizon AM, Kowalyk S, Hoogwerf BJ. Neuroglycopenic and other symptoms in patients with insulinomas. Am J Med Mar 1999; 106: 307–10 [DOI] [PubMed] [Google Scholar]
- 4.Norton JA, Shawker TH, Doppman JL, et al. Localization and surgical treatment of occult insulinomas. Ann Surg 1990; 212: 615–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Norton JA, Whitman ED. Insulinoma. Endocrinologist 1993; 3: 258–67 [Google Scholar]