Abstract
Yersinia pestis, the causative agent of bubonic, septicemic, and pneumonic plague, is classified as a CDC category A bioterrorism pathogen. Streptomycin and doxycycline are the “gold standards” for the treatment of plague. However, streptomycin is not available in many countries, and Y. pestis isolates resistant to streptomycin and doxycycline occur naturally and have been generated in laboratories. Moxifloxacin is a fluoroquinolone antibiotic that demonstrates potent activity against Y. pestis in in vitro and animal infection models. However, the dose and frequency of administration of moxifloxacin that would be predicted to optimize treatment efficacy in humans while preventing the emergence of resistance are unknown. Therefore, dose range and dose fractionation studies for moxifloxacin were conducted for Y. pestis in an in vitro pharmacodynamic model in which the half-lives of moxifloxacin in human serum were simulated so as to identify the lowest drug exposure and the schedule of administration that are linked with killing of Y. pestis and with the suppression of resistance. In the dose range studies, simulated moxifloxacin regimens of ≥175 mg/day killed drug-susceptible bacteria without resistance amplification. Dose fractionation studies demonstrated that the AUC (area under the concentration-time curve)/MIC ratio predicted kill of drug-susceptible Y. pestis, while the Cmax (maximum concentration of the drug in serum)/MIC ratio was linked to resistance prevention. Monte Carlo simulations predicted that moxifloxacin at 400 mg/day would successfully treat human infection due to Y. pestis in 99.8% of subjects and would prevent resistance amplification. We conclude that in an in vitro pharmacodynamic model, the clinically prescribed moxifloxacin regimen of 400 mg/day is predicted to be highly effective for the treatment of Y. pestis infections in humans. Studies of moxifloxacin in animal models of plague are warranted.
Yersinia pestis is a Gram-negative coccobacillus that is the causative agent of plague (12, 34). It is classified by the CDC as a category A bioterrorism agent. In nature, this microbe is perpetuated by fleas that transmit the bacterium from infected to noninfected rodents (6, 34). Humans are not part of the natural life cycle of Y. pestis. However, humans can be infected with Y. pestis through the bite of an infected flea. The bacterium is transported from the skin to local lymph nodes via the lymph system, most commonly resulting in bubonic plague. The infection can spread to the bloodstream, causing septicemic plague, and to the lungs, resulting in secondary pneumonic plague. Uncommonly, humans are infected by inhaling infected respiratory droplets from animals or other humans who have plague pneumonia, causing primary plague pneumonia (14, 18, 42). In the 14th century, plague was responsible for killing one-third of the human population in Europe (38). A pandemic in Asia that began in 1855 killed more than 12 million people in India and China alone (34).
Y. pestis has been used as a weapon of biowarfare. The first documented use was in 1346, when Mongols catapulted plague-infected corpses into the Crimean city of Caffa (43). In World War II, the Japanese reportedly released Y. pestis-infected fleas while flying in airplanes over China (34). A number of countries, including the former Soviet Union, have weaponized Y. pestis (1, 23). It is believed that if Y. pestis were used today as an agent of bioterrorism or biowarfare, it would be disseminated via the aerosol route, causing primary plague pneumonia (23).
Streptomycin and the tetracyclines are the only antibiotics approved by the U.S. Food and Drug Administration (FDA) for the treatment of plague. These recommendations are based on limited case studies of humans and several studies of small animals. However, streptomycin is not available in the United States and several other countries, and the treatment outcomes for the tetracyclines in animal models provide conflicting results (13, 36, 37). Gentamicin is considered an alternative to streptomycin on the basis of in vitro susceptibility data, several animal studies, and small case studies of humans (9, 12, 13, 33). However, the relative efficacies of streptomycin, gentamicin, and doxycycline for the treatment of infection due to Y. pestis, particularly pneumonic plague, have not been adequately studied.
The mortality associated with untreated bubonic plague is about 40%, whereas the mortalities of untreated septicemic and pneumonic plague approach 100% (16). Human case studies in the United States report that the fatality rates for antibiotic-treated bubonic, septicemic, and pneumonic plague are 14%, 22%, and 57%, respectively (14). Importantly, resistance to streptomycin, gentamicin, and tetracycline has been documented in Y. pestis strains found in nature and has been generated in laboratories (21, 23, 28, 30, 35). Thus, there is a need to identify additional classes of antibiotics that are active against plague.
Moxifloxacin is a fluoroquinolone antibiotic approved by the U.S. FDA for the treatment of acute bacterial sinusitis, acute exacerbation of chronic bronchitis, community-acquired bacterial pneumonia, uncomplicated and complicated skin and skin structure infections, and complicated intraabdominal infections caused by susceptible microorganisms (31). Although moxifloxacin is not approved by the U.S. FDA for the treatment of plague in humans, in vitro susceptibility studies show that it has potent activity against Y. pestis (40; H. Heine, unpublished data). Moxifloxacin is also efficacious in treating experimental plague pneumonia in an animal infection model (40; Heine, unpublished). However, the dose and frequency of administration of moxifloxacin that optimize treatment outcomes for plague in humans are unknown.
In this study, we conducted 10-day dose range and dose fractionation studies for moxifloxacin in an in vitro hollow-fiber (HF) pharmacodynamic (PD) model to identify the lowest drug exposure and the pharmacodynamic index linked with treatment efficacy against Y. pestis and with suppression of amplification of moxifloxacin-resistant bacterial subpopulations. Then, using Monte Carlo simulations, we determined the clinical dosage and frequency of administration of moxifloxacin that are predicted to optimize treatment efficacy for plague infections in humans and to prevent the emergence of resistance during therapy.
(Parts of this work were presented at the 47th Interscience Conference on Antimicrobial Agents and Chemotherapy, 17 to 20 September 2007.)
MATERIALS AND METHODS
Bacterial isolate.
Yersinia pestis ΔCO92 was provided by H. Heine, U.S. Army Medical Research Institute of Infectious Diseases, Frederick, MD. Y. pestis ΔCO92 is an avirulent mutant of the fully virulent Y. pestis CO92 strain. It lacks the pCD1 plasmid and hence the low calcium response stimulon. It also lacks a capsule. Y. pestis ΔCO92 has in vitro growth kinetics similar to those of its wild-type progenitor (unpublished data). Stocks of the organism were stored at −80°C in 10% glycerol. For each experiment, a sample taken from the frozen stock was incubated on blood agar plates at 35°C for 24 h. Then colonies taken from the overnight culture were suspended in Mueller-Hinton II broth (MHB; BBL, Sparks, MD) to a concentration of 108 CFU/ml. The bacterial suspension was diluted to the desired concentration, if required, and was used immediately.
Antibiotic.
Pharmaceutical-grade moxifloxacin was purchased commercially as premixed solutions for intravenous administration. The drug was stored at room temperature. For each study, an aliquot of moxifloxacin was diluted to the desired concentration with cation-adjusted MHB or water. The drug solutions were used immediately.
Susceptibility studies.
The susceptibility of Y. pestis ΔCO92 to moxifloxacin was determined by using a broth macrodilution method with MHB according to CLSI guidelines (15) and by agar dilution using Mueller-Hinton agar (MHA; BBL, Sparks, MD). The broth and agar susceptibility studies were conducted simultaneously. The final bacterial inoculum was approximately 5 × 105 CFU/ml or 104 CFU per spot for the broth or agar susceptibility method, respectively. The inocula were confirmed by quantitative cultures. The MIC was defined as the lowest concentration of antibiotic that demonstrated no visible growth after 24 h of incubation at 35°C. The minimal bactericidal concentrations (MBCs) were determined by streaking the surfaces of blood agar plates with 25 μl of samples taken from the clear tubes of the macrobroth susceptibility studies. After 48 h of incubation at 35°C, the colonies were enumerated. The MBC was defined as the concentration of drug that resulted in >99.9% kill of the bacterium relative to the concentration of the bacterium that was present in the test tubes at 0 h.
Mutation frequencies.
The mutation frequencies of Y. pestis ΔCO92 with 1.25×, 2.5×, and 5× the MIC of moxifloxacin were determined by inoculating 5 ml of 108-CFU/ml bacterial suspensions onto the surface of MHA containing these concentrations of moxifloxacin. These multiples of the MIC were chosen for mutation frequency determinations because they are the lowest multiples of the MIC for the Y. pestis parent strain that are likely to identify isolates of Y. pestis with efflux pump overexpression, a single point mutation in gyrA, and two point mutations in gyrA, respectively, based on preliminary data for Y. pestis (data not shown) and changes in MICs reported for a wild-type Escherichia coli strain and isogenic isolates with single and double mutations in gyrA (32). Quantitative cultures were conducted on the bacterial suspensions. All cultures were incubated at 35°C for 72 h. Then the colonies were enumerated, and the mutation frequencies were calculated.
In vitro hollow-fiber PD model.
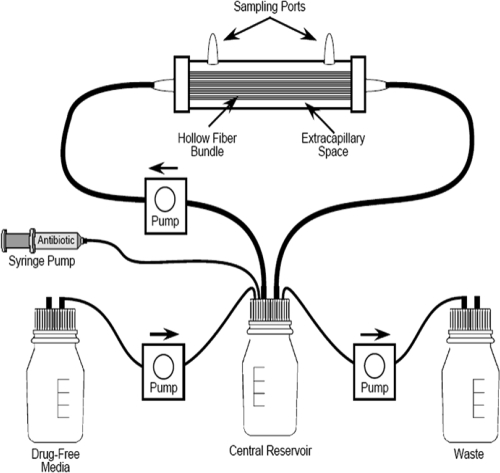
The hollow-fiber PD model has been described previously (19, 28, 29) (Fig. 1). Bacteria that were inoculated into the extracapillary space of hollow-fiber cartridges (FiberCell Systems, Frederick, MD) were exposed to fluctuating concentration-time profiles that simulated those reported in the literature for a drug regimen (31). Over the course of an experiment, bacterial samples were collected from the hollow-fiber system for quantitative cultures to determine the antimicrobial effect of each regimen on the bacterium studied. Medium samples were collected from each experimental arm over the first 48 h of a study, and the drug concentration in each sample was measured to confirm that the targeted concentration-time profiles for the drug were simulated.
FIG. 1.
Schematic of an in vitro hollow fiber system experimental arm.
Dose range studies.
Moxifloxacin dose range studies were conducted to determine (i) the minimum (breakpoint) exposure to moxifloxacin that effectively sterilized the HF systems and (ii) a separate minimum (breakpoint) exposure that would prevent the emergence of resistance during therapy. For each experiment, colonies of Y. pestis were taken off the surfaces of agar cultures that had been grown overnight at 35°C in ambient air. The bacteria were suspended in MHB to a concentration of 108 CFU/ml. The suspension was inoculated into the extracapillary spaces of eight HF cartridges, and the experiment was initiated by infusing the antibiotic.
Seven of the HF systems were treated with simulated human (half-life [t1/2], 12 h) concentration-time profiles for doses of 0 to 600 mg of moxifloxacin given once every 24 h (q24h). The pharmacokinetic (PK) profiles for moxifloxacin that were simulated in the HF systems were extrapolated from mean human PK values found in the manufacturer's drug package insert (31). Approximately 50% of moxifloxacin is bound to human serum proteins (31). The simulated PK profiles were for the non-protein-bound (free) fraction of moxifloxacin. The eighth HF system arm was not treated with moxifloxacin and served as the growth control.
At 0, 0.2, 1, 2, 3, 4, 6, 8, and 10 days of an experiment, 1 ml of the bacterial suspension was taken from the extracapillary space (peripheral compartment) of each HF system and was replaced with fresh medium. The bacteria were washed twice with normal saline to prevent drug carryover and were then quantitatively cultured onto drug-free agar and agar containing 1.25× and 2.5× the MIC of the treatment drug to characterize the effect of each antibiotic regimen on the drug-susceptible and drug-resistant bacterial populations. After the plates were incubated at 35°C for 72 h, the colonies were enumerated.
Serial medium samples taken from the central reservoir over the first 48 h were assayed for moxifloxacin concentrations by high-pressure liquid chromatography-tandem mass spectrometry (HPLC-MS-MS) to confirm that the desired pharmacokinetic profiles were achieved. The drug concentrations measured were within 10% of the targeted values (data not shown).
Agar dilution MICs were determined for mutants grown on moxifloxacin-supplemented agar that was inoculated with bacterial samples on days 0, 4, 6, and 10 of the in vitro studies. Three isolates were studied for each time point of each experimental arm.
Dose fractionation studies.
Two dose fractionation studies were conducted with moxifloxacin to determine the pharmacodynamic indices (Cmax [maximum concentration of the drug in serum]/MIC ratio, AUC [area under the concentration-time curve]/MIC ratio, or time above the MIC [T>MIC]) that were linked with the killing of the moxifloxacin-susceptible population and with prevention of the amplification of resistant mutants. HF cartridges were inoculated with 15 ml of Y. pestis at 108 CFU/ml. Then total daily dosages of moxifloxacin were administered to HF systems either as 1-h bolus infusions once every 24 h or as continuous infusions for 10 days. An HF system arm that did not receive antibiotic served as the control arm. For any total daily dosage, giving the total dosage as a single dose once per day maximized the Cmax/MIC ratio, while administration of this dose as a continuous infusion maximized T>MIC. For each total daily dose, the same AUC/MIC ratio was generated regardless of whether that total dose was given as a single daily bolus or as a continuous 24-h infusion.
The regimens and the targeted PK-PD values for simulation in the two dose fractionation studies are shown in Table 1. In the first experiment, the non-protein-bound (free) PK profiles for 50 to 250 mg/day of moxifloxacin, given q24h and as continuous infusions, were simulated. Based on the results of this experiment, a narrower range of dosages was evaluated in the second dose fractionation study in order to examine more dosages that fell on the steep portion of the dose-response curve.
TABLE 1.
Pharmacokinetic-pharmacodynamic values for the free (non-protein-bound) fraction of moxifloxacin obtained in the dose fractionation studies
| Total moxifloxacin dose (mg/day) | Pharmacokinetic-pharmacodynamic valuea for moxifloxacin: |
|||||
|---|---|---|---|---|---|---|
| Given once daily |
Given as a continuous infusion |
|||||
| fCmax/MIC | fAUC/MIC | fT>MIC (h) | fCmax/MIC | fAUC/MIC | fT>MIC (h) | |
| First expt | ||||||
| 50 | 4.8 | 63.5 | 24 | 2.6 | 63.5 | 24 |
| 100 | 9.6 | 127.0 | 24 | 5.3 | 127.0 | 24 |
| 150 | 14.4 | 190.5 | 24 | 7.9 | 190.5 | 24 |
| 200 | 19.2 | 254.0 | 24 | 10.9 | 254.0 | 24 |
| 250 | 24.0 | 317.5 | 24 | 13.2 | 317.5 | 24 |
| Second expt | ||||||
| 100 | 9.6 | 127.0 | 24 | 5.3 | 127.0 | 24 |
| 150 | 14.4 | 190.5 | 24 | 7.9 | 190.5 | 24 |
| 175 | 16.8 | 222.2 | 24 | 9.3 | 222.2 | 24 |
| 200 | 19.2 | 254.0 | 24 | 10.9 | 254.0 | 24 |
f, free (non-protein bound).
Bacterial samples taken from the HF systems were quantitatively cultured over the 10-day study onto antibiotic-free agar and agar containing 1.25× and 2.5× the MIC of moxifloxacin in order to characterize the effect of each regimen on the total bacterial population and the populations with decreased susceptibilities to moxifloxacin. Medium samples were collected over the first 48 h of each experiment. The concentrations of moxifloxacin in these samples were measured by LC-MS-MS to confirm that the targeted concentration-time profiles for moxifloxacin were achieved.
LC-MS-MS assay for moxifloxacin.
Mueller-Hinton II broth samples were diluted with HPLC water (0.05 ml of sample in 1 ml of water) and were analyzed by LC-MS-MS. The LC-MS-MS system comprised a Shimadzu Prominence HPLC system and an Applied Biosystems/MDS Sciex API5000 LC-MS-MS.
Chromatographic separation was performed using a Thermo Scientific Hypersil Gold C18 column (5 μm particle size of packing material, 150 mm length, 4.6 mm diameter) with a mobile phase of 80% 0.1% formic acid in water and 20% methanol at a flow rate of 0.8 ml/min. Moxifloxacin concentrations were obtained by using LC-MS-MS, monitoring the MS-MS transition from m/z 402 to m/z 384. The analysis run time was 3.0 min. The assay was linear over a range of 0.005 to 5.0 μg/ml (r2, >0.994).
The interday coefficients of variation (CVs) for the quality control samples analyzed in replicates of three at three concentrations (0.01 μg/ml, 0.1 μg/ml, and 1 μg/ml) on each analysis day ranged from to 4.21 to 8.19%, and the accuracies (% recovery) for the same quality control samples ranged between 99.4 to 103%.
Pharmacokinetic analysis.
Since computer-controlled pumps were employed to simulate a one-compartment model in the central reservoir of the hollow-fiber systems, the concentration-time curves were analyzed employing a one-compartment open model with zero-order, time-delimited input and first-order output. The ADAPT II package of programs of D'Argenio and Schumitzky (17) was employed (identification module). A maximum-likelihood approach was taken.
Sequencing of mutants from the dose range study.
The quinolone resistance-determining regions (QRDRs) of the gyrA, gyrB, parC, and parE genes of randomly selected isolates recovered from moxifloxacin-supplemented agar in the HF dose range experiments were amplified by PCR using a Eppendorf Mastercycler gradient thermocycler (Eppendorf AG, Hamburg, Germany) and were then sequenced using an ABI 3730 DNA analyzer (Applied Biosystems, Foster City, CA). The primers used for DNA amplification were adapted from those described by Lindler et al. (25) and are shown in Table 2. Amplification was achieved using an initial denaturing step of 95°C for 2 min, followed by 30 cycles of 94°C for 45 s, 60°C for 45 s, and 72°C for 1.5 min, with a final extension step of 72°C for 10 min.
TABLE 2.
Primers used to amplify the QRDRs of Y. pestis ΔCO92 gyrA, gyrB, parC, and parE
| Target | Orientation | Primer sequencea |
|---|---|---|
| GyrA | Forward | 5′-ATGAGCGACCTTGCCAGAG-3′ |
| Reverse | 5′-TACTCCATCAGCCCTTCAATG-3′ | |
| GyrB | Forward | 5′-GTCGAATACTTATGACTCCTCAAG-3′ |
| Reverse | 5′-CGATATCGTCTTTCATGGTGGAG-3′ | |
| ParC | Forward | 5′-GATCGGGCGTTGCCGTTTATCGG-3′ |
| Reverse | 5′-TTGGCTAAGTGGCGGAGTTTC-3′ | |
| ParE | Forward | 5′-TTGTCTCCGGTGTTGTCAAA-3′ |
| Reverse | 5′-GTTTGCGTTTCAGTTGCTCA-3′ |
Adapted from those described by Lindler et al. (25).
Moxifloxacin dose range studies for a Y. pestis LLRM.
Moxifloxacin dose range studies were conducted for a low-level resistant mutant (LLRM) of Y. pestis that was isolated on antibiotic-supplemented agar in one of the dose range studies described above. This low-level resistant mutant had a moxifloxacin MIC of 0.25 mg/liter. The wild-type Y. pestis strain had a MIC of 0.06 mg/liter. Sequencing studies demonstrated no point mutations in the QRDRs of gyrA, gyrB, parC, and parE. The mutation frequency of the LLRM isolate with 2.5× the MIC of moxifloxacin was −8.40 log CFU.
In this dose range study, six hollow-fiber systems were inoculated with 15 ml of the LLRM strain at 5 × 105 CFU/ml. Thus, approximately 7.5 × 106 CFU (6.9 log CFU) of bacteria was placed in each HF cartridge. The total number of the LLRM bacteria inoculated into the hollow-fiber systems was approximately 2 log CFU less than the mutation frequency for mutants that expressed additional resistance mechanisms. Thus, these hollow-fiber systems were unlikely to be inoculated with bacteria with additional genetically encoded resistance mechanisms. Therefore, these experimental arms examined the effects of the moxifloxacin regimens on the kill of the LLRM (and not on the selection of mutants with additional resistance mechanisms).
Five of the hollow-fiber systems were treated with simulated human serum concentration-time profiles for 200 to 800 mg moxifloxacin given q24h. The sixth hollow-fiber system received no drug and served as the control arm.
Three other hollow-fiber system arms were inoculated with 15 ml of the parental Y. pestis strain at 108 CFU/ml (moxifloxacin MIC, 0.06 mg/liter), as was done in the dose range studies described above for this wild-type bacterial isolate, and were treated with simulated regimens for the free fraction of the PK profiles of 0, 200, and 250 mg moxifloxacin given q24h. The higher concentration of the parent strain was used to confirm that the drug exposures for this strain performed as they did in the previous hollow-fiber experiments.
Treatment lasted 10 days. Bacterial samples were cultured on antibiotic-free agar and on agar supplemented with 2.5× the MIC of moxifloxacin for the respective bacterial strains in order to determine the effect of each regimen on the bacterial strains inoculated into the hollow-fiber system and on mutant populations with reduced susceptibility to moxifloxacin. The drug concentrations measured in the media of the hollow-fiber systems over time were within 10% of the targeted values (data not shown).
Monte Carlo simulations.
From dose range and dose fractionation experiments, the lowest exposures of moxifloxacin that optimally killed wild-type Y. pestis and prevented resistance amplification were identified for regimens in which the drug was given on a q24h schedule of administration or as a continuous infusion. From the dose fractionation studies, the pharmacodynamic indices linked with bacterial kill and with resistance suppression were identified.
Since moxifloxacin is approved by the U.S. FDA for once-daily administration for infections due to other bacterial species, Monte Carlo simulations (with 9,999 virtual human subjects) were employed to determine the probability that the human clinical regimen of 400 mg moxifloxacin given orally q24h would achieve the exposure intensity identified in the dose range and dose fractionation studies that was predicted to optimally kill the susceptible Y. pestis population and to suppress the amplification of resistant subpopulations. The steady-state pharmacokinetic parameters employed in the Monte Carlo simulations were reported for 15 volunteers given 400 mg moxifloxacin orally q24h for 10 days (41). Target attainment was calculated using the results of the Monte Carlo simulations in conjunction with the moxifloxacin MIC distribution for 30 unique clinical strains of Y. pestis, which was determined by one of us (H. Heine) using the microdilution broth technique described by the CLSI (15). The moxifloxacin MICs were 0.015 mg/liter for 1 of these isolates, 0.03 mg/liter for 23 isolates, and 0.06 mg/liter for 6 isolates.
The ADAPT II package of programs of D'Argenio and Schumitzky was employed for the simulations (17). Both normal and log-normal models were evaluated. The distribution was chosen as a function of the fidelity with which the original parameter values and their dispersions were re-created by the simulations.
RESULTS
MIC, MBC, and mutation frequency values.
The MIC and the MBC of Y. pestis ΔCO92 were both 0.06 mg/liter. The MIC value was the same for susceptibility studies that were conducted in broth or on agar. The mutation frequencies with 1.5×, 2.5×, and 5× the MIC of the parent strain were −7.44, −8.40, and less than −8.94 log CFU, respectively.
Dose range studies.
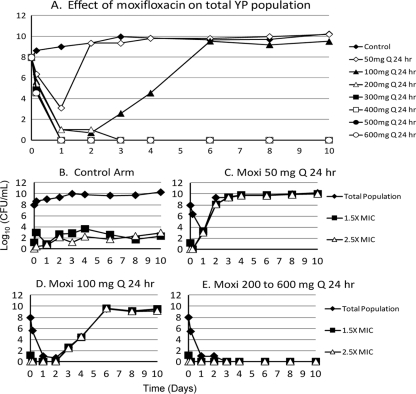
Once-daily moxifloxacin dosing was conducted to determine (i) the minimum (breakpoint) exposure of moxifloxacin that effectively sterilized the hollow-fiber systems and (ii) the minimum (breakpoint) exposure that prevented the emergence of resistance during therapy. Untreated, Y. pestis grew well, with resistant mutants increasing in proportion to the total population (Fig. 2 A and B). There was a clear demarcation of moxifloxacin doses associated with treatment success and failure. Moxifloxacin at doses of 50 and 100 mg q24h caused a transient decrease in the total bacterial population for 1 and 2 days, respectively, followed by treatment failure (Fig. 2A). Figures 2C and D show that failure with these dosages was due to rapid selection of resistance. In contrast, simulated exposures for ≥200 mg moxifloxacin per day rapidly killed the drug-susceptible population without amplifying resistant populations (Fig. 2E). The moxifloxacin MICs for the Y. pestis mutants that were amplified with the regimens of 50 and 100 mg moxifloxacin q24h were 0.5 to 1 mg/liter. The moxifloxacin MIC for the parent strain was 0.06 mg/liter. Simulated regimens of ≥200 mg moxifloxacin given q24h killed these mutants and therefore prevented the emergence of resistance. These results were observed in two experiments.
FIG. 2.
Dose range study of moxifloxacin against Y. pestis ΔCO92. (A) Microbiological effect of each regimen on the total bacterial population. (B through E) Effects of individual drug regimens on the total population and the populations that were resistant to 1.5× and 2.5× the MIC values for the parent strain.
Dose fractionation studies.
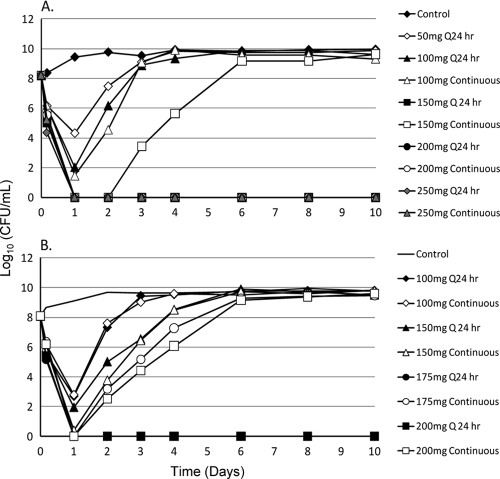
Two separate dose fractionation studies were conducted with moxifloxacin to determine the pharmacodynamic indices (Cmax/MIC ratio, AUC/MIC ratio, or time above the MIC) that were linked with kill of the moxifloxacin-susceptible population and with prevention of the amplification of resistant mutants. The dosages examined in the second experiment were revised based on the results of the first dose fractionation study.
In the first dose fractionation study, simulated human serum concentration-time profiles for total daily dosages of 100, 150, 200, and 250 mg of moxifloxacin were administered to HF systems either as 1-h infusions given once q24h or as continuous infusions. For the second study, simulated human serum concentration-time profiles for 100, 150, 175, and 200 mg/day of moxifloxacin were fractionated. Over the first 24 h of both dose fractionation trials, each pair of HF systems in which the same total daily dose of moxifloxacin was administered once daily and as a continuous infusion showed similar extents of kill of the drug-susceptible bacterial population (Fig. 3A and B). This suggests that the AUC/MIC ratio was the pharmacodynamic index linked with the killing of the moxifloxacin-susceptible Y. pestis population.
FIG. 3.
Two dose fractionation studies for moxifloxacin against Y. pestis ΔCO92. The effect of each regimen on the total bacterial population is shown. The regimens selected for fractionation in the second experiment (B) were selected based on the results of the first study (A).
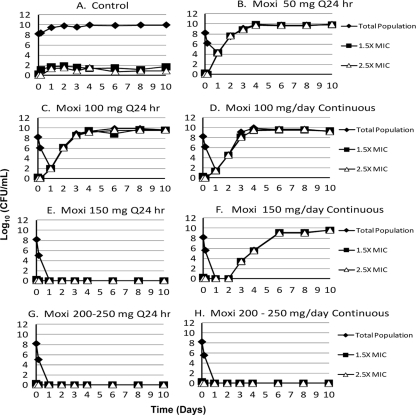
With regard to resistance amplification, in the first dose fractionation trial (Fig. 3A), 100 mg moxifloxacin/day failed due to the emergence of resistance, regardless of whether this total daily dosage was administered as a single daily bolus or as a continuous infusion. In contrast, 150 mg moxifloxacin given q24h eradicated Y. pestis, while the same total daily dose given as a continuous infusion failed. Treatment failure for suboptimal moxifloxacin regimens was due to the amplification of resistance (Fig. 4). The simulated exposures for 200 mg moxifloxacin per day given once daily and as a continuous infusion both killed the wild-type population and prevented emergence of resistance.
FIG. 4.
Effect of each fractionated regimen on the total and less-susceptible Y. pestis populations for the first dose fractionation study. (The effects of the antibiotic on the total bacterial population are also shown in Fig. 3A.) The moxifloxacin MICs for the less-susceptible populations were at least 1.5× and 2.5× higher than that for the parent strain.
In the second dose fractionation study (Fig. 3B), 150 mg moxifloxacin per day failed, regardless of whether this dose was administered once every 24 h or as a continuous infusion. However, the 175-mg q24h regimen (a dose that was added to the second dose fractionation study based on the results of the first trial) and the 200-mg q24h regimen were successful, while the same daily dosages given as continuous infusions failed. Failure was due to resistance amplification (data not shown). These data suggest that for Y. pestis, the pharmacodynamic index for moxifloxacin linked with the prevention of resistance was the Cmax/MIC ratio. Further, the lowest simulated dosage that prevented resistance amplification was 175 mg moxifloxacin q24h.
DNA sequencing of mutants amplified with suboptimal moxifloxacin regimens.
The MIC of moxifloxacin for the Y. pestis parental strain ΔCO92 was 0.06 mg/liter. Mutants amplified with suboptimal moxifloxacin regimens had MICs of 0.5 to 2 mg/liter. The results of the sequencing of the QRDRs of gyrA, gyrB, parC, and parE are given in Table 3. Mutations were found only in the QRDR of gyrA.
TABLE 3.
MICs and QRDR mutations in mutants of Y. pestis ΔCO92 amplified with suboptimal moxifloxacin regimens in the moxifloxacin dose range studiesa
| Mutant source | Moxifloxacin MIC (mg/liter) | Mutation in GyrA |
|---|---|---|
| Mutation frequency isolates | 1 | Ser83Ile or Ser83Arg |
| Mutation frequency isolates | 0.5 | Asp87Tyr or Gly81Cys |
| Control, day 3 | 0.25 | NMb |
| Control, day 10 | 1 | Asp82Gly |
| 50 mg/day, days 3, 4, and 10 | 1 | Ser83Arg |
| 100 mg/day, days 3, 6, and 10 | 0.5-1 | Asp82Gly |
The MIC of moxifloxacin for the wild-type parent isolate was 0.06 mg/liter. Neither the wild type nor the mutants had any mutations in the QRDRs of GyrB, ParC, and ParE.
NM, no mutation identified.
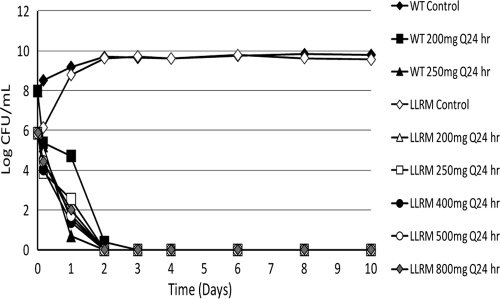
Moxifloxacin dose range studies using a Y. pestis LLRM.
Moxifloxacin dose range studies were conducted for an LLRM for which the moxifloxacin MIC was 0.25 mg/liter. The mutation frequency for the LLRM with 2.5× the MIC was −8.4 log CFU. The Y. pestis parent strain (moxifloxacin MIC, 0.06 mg/liter) served as a control. In a dose range study in which the human serum concentration-time profiles for moxifloxacin were simulated, ≥200 mg moxifloxacin given once daily eradicated both the wild-type and the LLRM strain (Fig. 5). The rates of kill of the LLRM and parent strains by moxifloxacin were similar. Thus, 200 mg moxifloxacin given once daily was equally effective in killing the wild-type and LLRM strains of Y. pestis.
FIG. 5.
Dose range study for moxifloxacin against the low-level resistant mutant (LLRM) of Y. pestis (moxifloxacin MIC, 0.25 mg/liter). The wild-type (WT) Y. pestis strain ΔCO92 (moxifloxacin MIC, 0.06 mg/liter) was studied as a comparative control.
Monte Carlo simulations.
The dose fractionation studies demonstrated that the simulated PK profile for 175 mg moxifloxacin q24h was the minimum dose and frequency of administration that resulted in kill of the wild-type Y. pestis population and prevented resistance amplification in our in vitro HF pharmacodynamic model. It should be noted that this simulated dose has one specific AUC and hence one AUC/MIC ratio. It is the exposure that is the target and not the drug dose. Because 50% of a population will have an AUC less than that produced by the median exposure to moxifloxacin, we know that 50% of a population will fail to achieve the exposure target if a dose of 175 mg is employed. In order for an acceptably large portion of the population to achieve the exposure target, a larger dose must be administered. We decided to examine a 400-mg dose, because this is the licensed moxifloxacin dose. Monte Carlo simulations predicted that the clinically prescribed regimen of 400 mg moxifloxacin given orally q24h would kill the wild-type Y. pestis strain and prevent the emergence of resistance in 100% of virtual human subjects infected with Y. pestis strains for which the moxifloxacin MICs were 0.015 and 0.03 mg/liter and in 99.9% of persons infected with Y. pestis isolates for which the moxifloxacin MIC was 0.06 mg/liter.
We took the expectation over the distribution of moxifloxacin MIC values for a collection of 30 isolates examined by one of us (H. S. Heine). In taking an expectation, one takes the product of the target attainment fraction at a specific MIC value, for the clinical 400-mg daily moxifloxacin dose and the fraction of the isolates at that MIC value. The sum of all these products is the expectation. That is, for all MIC values, the “expected” probability of attaining exposure values that optimally kill Y. pestis and suppress resistance is calculated. This value was 99.8% for optimal cell kill and 99.7% for suppression of the amplification of resistant subpopulations.
DISCUSSION
Streptomycin is considered the treatment of choice for bubonic, septicemic, and pneumonic plague based on a small number of clinical case reports and results of animal infection models (11, 23). Previously, in an in vitro pharmacodynamic model, we demonstrated that the simulated human serum concentration-time exposures for a recommended clinical regimen for the treatment of plague (1 g streptomycin given every 12 h) readily amplified the drug-resistant subpopulation, leading to treatment failure (28). In a nonhuman primate model of plague septicemia and pneumonia, McCrumb et al. (30) reported that 29% of subjects failed treatment with streptomycin due to the emergence of streptomycin-resistant Y. pestis mutants. Since Y. pestis can be transmitted from person to person (11, 23), the dissemination of drug-resistant mutants may have a profound impact on the efficacy of streptomycin in mass treatment efforts that would be implemented in response to an act of bioterrorism or biowarfare. Furthermore, a naturally occurring streptomycin-resistant strain of Y. pestis has caused plague in humans (21).
The use of fluoroquinolones as monotherapy for the treatment of plague in humans is limited to a single case report in which a man with septicemic plague was successfully treated with ciprofloxacin (24). However, in vitro MIC results and in vivo studies conducted in mice suggest that fluoroquinolones, including moxifloxacin, have potent activity against Y. pestis (8, 13, 20, 39, 40). In an in vitro hollow-fiber pharmacodynamic model, Louie et al. (28) showed that the simulated clinical regimen of 500 mg levofloxacin q24h rapidly sterilized the experimental arm containing Y. pestis and thus prevented the emergence of resistance. In the current study, we demonstrated that stimulated regimens of moxifloxacin at dosages of ≤150 mg q24h quickly amplified Y. pestis mutants with increased MICs to moxifloxacin of 0.5 to 2 mg/liter and that the increased MIC values were caused by single point mutations in gyrA. But simulated regimens of ≥175 mg/day of moxifloxacin, administered once daily, were highly effective in killing moxifloxacin-susceptible Y. pestis and in preventing the amplification of bacterial populations with decreased susceptibilities to this drug.
Dose fractionation studies showed that the AUC/MIC ratio was the pharmacodynamic index linked with killing of the moxifloxacin-susceptible population of Y. pestis within hollow-fiber systems. This finding is consistent with the findings of pharmacodynamic studies of other fluoroquinolones against Staphylococcus aureus, Streptococcus pneumoniae, and Escherichia coli (3, 4) Furthermore, the AUC/MIC ratio was shown to be the pharmacodynamic index for the killing of wild-type Bacillus anthracis by fluoroquinolone antibiotics in a murine model of inhalational anthrax (2, 26).
However, the Cmax/MIC and not the AUC/MIC ratio was the pharmacodynamic index for moxifloxacin that was linked with preventing the emergence of resistance during therapy for Y. pestis. The Cmax/MIC ratio has also been shown to be the pharmacodynamic index for the suppression of resistance to the fluoroquinolone enoxacin by S. aureus, E. coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa, to rifampin by Mycobacterium tuberculosis, and to linezolid by Bacillus anthracis (7, 22, 29). In contrast, the time above the MIC was the pharmacodynamic index linked with the prevention of resistance to moxifloxacin and ciprofloxacin for the treatment of infection due to Bacillus anthracis (19, 26). These results show that one cannot assume that the pharmacodynamic index for resistance prevention that is identified for a drug using one bacterial species is applicable to all other bacterial species.
Since the AUC/MIC ratio is linked with kill of moxifloxacin-susceptible Y. pestis and the Cmax/MIC ratio is linked with the prevention of resistance, the administration of moxifloxacin using a once-daily schedule should optimize kill of the drug-susceptible population of Y. pestis and should minimize the probability that mutants with decreased susceptibilities to this drug would be amplified during therapy. The hollow-fiber dose range experiments conducted in this project showed that 175 mg moxifloxacin q24h (fCmax [Cmax for the free, unbound fraction of the drug]/MIC, 16.8) was the minimum once-daily dosage of this antibiotic that prevented the emergence of resistance for the strain of Y. pestis that was examined. Monte Carlo simulations predicted that, in the clinic, this fCmax/MIC exposure should be achieved in 99.7% of humans who are treated with an oral regimen of 400 mg moxifloxacin q24h.
Currently, moxifloxacin is not approved by the U.S. FDA for the treatment of human infections due to Y. pestis. Moxifloxacin at a dose of 400 mg given once daily is approved by the U.S. FDA for the treatment of pneumonia and other serious infections due to several “nonplague” bacteria. Our dose range study showed that the simulated moxifloxacin regimens of ≥200 mg q24h were also sufficient to kill a low-level resistant mutant of Y. pestis for which the moxifloxacin MIC was 0.25 mg/liter. Information on the distribution of MICs in wild-type Y. pestis is limited. A strain of Y. pestis examined by Steward et al. (40) had a moxifloxacin MIC of <0.125 mg/liter. H. S. Heine et al. (unpublished data) reported that 100% of 30 unique wild-type Y. pestis isolates had moxifloxacin MICs of ≤0.06 mg/liter. The isolate used in this project had a moxifloxacin MIC of 0.06 mg/liter. Hence, the MICs for these wild-type strains were lower than that for the LLRM examined in this project. In the dose range study, moxifloxacin doses of ≥200 mg q24h killed the LLRM bacterium at the same rate as the wild-type strain, indicating that all dosages of ≥200 mg of q24h evaluated provided maximum antimicrobial effects (Emax) for both bacterial isolates, even though the moxifloxacin MIC for the LLRM was four times higher than that for the parent strain.
Doxycycline and streptomycin are approved by the U.S. FDA for the treatment of Y. pestis infections. Streptomycin is currently unavailable in many countries, including the United States (12). Gentamicin at 5 mg/kg/day is considered an equivalent substitute for streptomycin for the treatment of Y. pestis infections on the basis of outcomes in animal models and small case studies involving bubonic and septicemic plague (9, 12, 13, 23, 33). However, no comparative studies exist to prove this assumption for the treatment of pneumonic plague. Furthermore, the dosages and frequencies of administration of doxycycline, streptomycin, and gentamicin that optimize the treatment outcome and prevent the emergence of resistance in Y. pestis are unknown. In this study, we identified the dosage and schedule of administration for moxifloxacin that achieve both of these end points.
Based on our data, moxifloxacin should be evaluated further in animal models for the treatment of bubonic, septicemic, and pneumonic plague. It provided rapid kill of a pansusceptible Y. pestis isolate in our in vitro hollow-fiber pharmacodynamic model and did not select for resistance at clinically achievable exposures. In contrast, streptomycin in the simulated clinical regimen of 1 g given q12h rapidly selected for resistance in seven of the eight hollow-fiber experiments that our group has conducted to date (28; also unpublished data). Recently, we reported that simulated clinical regimens of gentamicin at dosages of 4 to 6 mg/kg of body weight given once daily within an in vitro hollow-fiber pharmacodynamic model provided unreliable killing of high inocula of Y. pestis ΔCO92. Failures were due to the emergence of resistance to this antibiotic. Simulated gentamicin regimens of 7 mg/kg/day were required to consistently prevent resistance amplification in our in vitro hollow-fiber pharmacodynamic model (27). In humans with bubonic plague, gentamicin and doxycycline therapies are associated with cure rates of 94 to 97% (9, 33). However, insufficient information is available on the efficacy of any antibiotic for the treatment of pneumonic plague because of the rarity of naturally occurring pulmonary disease due to Y. pestis.
Moxifloxacin has other advantages over streptomycin and gentamicin. First, the aminoglycosides streptomycin and gentamicin are both ototoxic and nephrotoxic (5, 10). Doxycycline may cause gastrointestinal side effects, including abdominal pain, nausea, vomiting, and diarrhea. In contrast, extensive clinical use of moxifloxacin has proven that this drug has an excellent safety profile and is well tolerated by humans. Second, the supply of streptomycin is limited or unavailable in the United States and other countries, while moxifloxacin is readily available. This factor makes it impractical to rely on streptomycin for large-scale treatment and prophylaxis of plague in a bioterror or biowarfare scenario. Third, streptomycin and gentamicin must be administered intravenously (i.v.) or intramuscularly, and streptomycin is injected twice daily. Doxycycline is administered orally or intravenously twice daily. Moxifloxacin is available as both oral and i.v. formulations and is administered once daily (31). These properties of moxifloxacin should increase patient acceptance and compliance with antibiotic therapy should future in vivo studies in animal infection models confirm that moxifloxacin at 400 mg q24h is useful for the treatment of plague, especially if the drug were to be given to a large population of people who had pneumonic plague as a consequence of an act of bioterror or biowarfare.
Acknowledgments
This work was supported by grant P01AI060908 from the National Institute of Allergy and Infectious Diseases.
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases, the National Institutes of Health, or the U.S. Army.
None of the authors has any conflicts of interest to disclose.
Footnotes
Published ahead of print on 29 November 2010.
REFERENCES
- 1.Alibek, K., and S. Handelman. 1999. Biohazard. Random House, New York, NY.
- 2.Ambrose, P. G., et al. 2007. Pharmacokinetics-pharmacodynamics of gatifloxacin in a lethal murine Bacillus anthracis inhalation infection mode. Antimicrob. Agents Chemother. 51:4351-4355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andes, D., and W. Craig. 2002. Pharmacodynamics of the new fluoroquinolone gatifloxacin in murine thigh and lung infection models. Antimicrob. Agents Chemother. 46:1665-1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andes, D., and W. Craig. 2003. Pharmacodynamics of the new des-f(6)-quinolone garenoxacin in a murine thigh infection model. Antimicrob. Agents Chemother. 47:3935-3941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Appel, G. B. 1990. Aminoglycoside nephrotoxicity. Am. J. Med. 88(Suppl. C):16S-20S. [DOI] [PubMed] [Google Scholar]
- 6.Bacot, A. W., and C. J. Martin. 1914. Observations on the mechanism of the transmission of plague by fleas. J. Hyg. (Lond.) 13(Suppl.):423-439. [PMC free article] [PubMed] [Google Scholar]
- 7.Blaser, J., B. B. Stone, M. C. Groner, and S. H. Zinner. 1987. Comparative study with enoxacin and netilmicin in a pharmacodynamic model to determine importance of ratio of antibiotic peak concentration to MIC for bactericidal activity and emergence of resistance. Antimicrob. Agents Chemother. 31:1054-1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bonacorsi, S. P., M. R. Scavizzi, A. Guiyoule, J. H. Amouroux, and E. Carniel. 1994. Assessment of a fluoroquinolone, three beta-lactams, two aminoglycosides, and a cycline in treatment of murine Yersinia pestis infection. Antimicrob. Agents Chemother. 38:481-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boulanger, L. L., et al. 2004. Gentamicin and tetracyclines for the treatment of human plague: review of 75 cases in New Mexico, 1985-1999. Clin. Infect. Dis. 38:663-669. [DOI] [PubMed] [Google Scholar]
- 10.Brummett, R. E., and K. E. Fox. 1989. Aminoglycoside-induced hearing loss in humans. Antimicrob. Agents Chemother. 33:797-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butler, T., and D. T. Dennis. 2005. Yersinia species, including plague, p. 2691-2701. In G. L. Mandell, J. E. Bennett, and R. Dolin (ed.), Principles and practices of infectious diseases, 6th ed. Elsevier/Churchill Livingstone, Philadelphia, PA.
- 12.Butler, T. 2009. Plague into the 21st century. Clin. Infect. Dis. 49:736-742. [DOI] [PubMed] [Google Scholar]
- 13.Byrne, W. R., et al. 1998. Antibiotic treatment of experimental pneumonic plague in mice. Antimicrob. Agents Chemother. 42:675-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. 1997. Fatal human plague—Arizona and Colorado, 1996. MMWR Morb. Mortal. Wkly. Rep. 46:617-620. [PubMed] [Google Scholar]
- 15.Clinical and Laboratory Standards Institute. 2006. Document M7-A7. Methods for dilution antimicrobial susceptibility testing for bacteria that grow aerobically. Approved standard, 7th ed. Clinical and Laboratory Standards Institute, Wayne, PA.
- 16.Cohen, R. J., and J. L. Stockard. 1967. Pneumonic plague in an untreated plague-vaccinated individual. JAMA 202:365-366. [PubMed] [Google Scholar]
- 17.D'Argenio, D. Z., and A. Schumitzky. 1997. ADAPT II. A program for simulation, identification, and optimal experimental design. User manual. Biomedical Simulations Resource, University of Southern California, Los Angeles, CA. http://bmsr.usc.edu/.
- 18.Dennis, D., and F. Meier. 1997. Plague, p. 21-47. In C. R. Horsburgh and A. M. Nelson (ed.), Pathology of emerging infections. ASM Press, Washington, DC.
- 19.Deziel, M. R., et al. 2005. Identification of effective antimicrobial regimens for use in humans for the therapy of Bacillus anthracis infections and post-exposure prophylaxis. Antimicrob. Agents Chemother. 49:5099-5106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frean, J. A., L. Arntzen, T. Capper, A. Bryskier, and K. P. Klugman. 1996. In vitro activities of 14 antibiotics against 100 human isolates of Yersinia pestis from a southern African plague focus. Antimicrob. Agents Chemother. 40:2646-2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galimand, M., et al. 1997. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N. Engl. J. Med. 337:677-680. [DOI] [PubMed] [Google Scholar]
- 22.Gumbo, T., et al. 2007. Concentration-dependent Mycobacterium tuberculosis killing and prevention of resistance by rifampin. Antimicrob. Agents Chemother. 51:3781-3788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Inglesby, T. V., et al. 2000. Plague as a biological weapon: medical and public health management. JAMA 283:2281-2290. [DOI] [PubMed] [Google Scholar]
- 24.Kuberski, T., L. Robinson, and A. Schurgin. 2003. A case of plague successfully treated with ciprofloxacin and sympathetic blockage for treatment of gangrene. Clin. Infect. Dis. 36:521-523. [DOI] [PubMed] [Google Scholar]
- 25.Lindler, L. E., W. Fan, and N. Jahan. 2001. Detection of ciprofloxacin-resistant Yersinia pestis by fluorogenic PCR using the LightCycler. J. Clin. Microbiol. 39:3649-3655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Louie, A., et al. 2007. Dose-ranging and dose-fractionation studies of moxifloxacin against Bacillus anthracis, abstr. A-1442, p. 36. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 27.Louie, A., et al. 2008. Pharmacodynamic optimization of gentamicin against Yersinia pestis in an in vitro pharmacodynamic model, abstr. A-1827, p. 30. Abstr. 48th Annu. Intersci. Conf. Antimicrob. Agents Chemother. (ICAAC)-Infect. Dis. Soc. Am. (IDSA) 46th Annu. Meet. American Society for Microbiology and Infectious Diseases Society of America, Washington, DC.
- 28.Louie, A., M. R. Deziel, W. Liu, and G. L. Drusano. 2007. Impact of resistance selection and mutant growth fitness on the relative efficacies of streptomycin and levofloxacin for plague therapy. Antimicrob. Agents Chemother. 51:2661-2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Louie, A., et al. 2008. Use of an in vitro pharmacodynamic model to derive a linezolid regimen that optimizes bacterial kill and prevents emergence of resistance in Bacillus anthracis. Antimicrob. Agents Chemother. 52:2486-2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCrumb, F. R., Jr., A. Larson, and K. F. Meyer. 1953. The chemotherapy of experimental plague in the primate host. J. Infect. Dis. 92:273-287. [DOI] [PubMed] [Google Scholar]
- 31.Medical Economics Co. 2000. Physicians' desk reference, p. 2157-2165. Medical Economics Co., Montvale, NJ.
- 32.Morgan-Linnell, S. K., and L. Zechiedrich. 2007. Contributions of the combined effects of topoisomerase mutations toward fluoroquinolone resistance in Escherichia coli. Antimicrob. Agents Chemother. 51:4205-4208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mwengee, W., et al. 2006. Treatment of plague with gentamicin or doxycycline in a randomized clinical trial in Tanzania. Clin. Infect. Dis. 42:614-621. [DOI] [PubMed] [Google Scholar]
- 34.Perry, R. D., and J. D. Fetherston. 1997. Yersinia pestis—etiologic agent of plague. Clin. Microbiol. Rev. 10:35-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rasoamanana, B., P. Coulanges, P. Michel, and N. Rasolofonirina. 1989. Sensitivity of Yersinia pestis to antibiotics: 277 strains isolated in Madagascar between 1926 and 1989. Arch. Inst. Pasteur Madagascar 56:37-53. [PubMed] [Google Scholar]
- 36.Russell, P., S. M. Eley, D. L. Bell, R. J. Manchee, and R. W. Titball. 1996. Doxycycline or ciprofloxacin prophylaxis and therapy against experimental Yersinia pestis infection in mice. J. Antimicrob. Chemother. 37:769-774. [DOI] [PubMed] [Google Scholar]
- 37.Russell, P., et al. 1998. Efficacy of doxycycline and ciprofloxacin against experimental Yersinia pestis infection. J. Antimicrob. Chemother. 41:301-305. [DOI] [PubMed] [Google Scholar]
- 38.Slack, P. 1989. The black death past and present. 2. Some historical problems. Trans. R. Soc. Trop. Med. Hyg. 83:461-463. [DOI] [PubMed] [Google Scholar]
- 39.Smith, M. D., et al. 1995. In vitro antimicrobial susceptibilities of strains of Yersinia pestis. Antimicrob. Agents Chemother. 39:2153-2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Steward, J., et al. 2004. Efficacy of the latest fluoroquinolones against experimental Yersinia pestis. Int. J. Antimicrob. Agents 24:609-612. [DOI] [PubMed] [Google Scholar]
- 41.Sullivan, J. T., et al. 1999. Pharmacokinetics of a once-daily oral dose of moxifloxacin (BAY 12-8039), a new enantiomerically pure 8-methoxy quinolone. Antimicrob. Agents Chemother. 43:2793-2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Werner, S. B., et al. 1984. Primary plague pneumonia contracted from a domestic cat at South Lake Tahoe, CA. JAMA 251:929-931. [PubMed] [Google Scholar]
- 43.Wheelis, M. 2002. Biological warfare at the 1346 siege of Caffa. Emerg. Infect. Dis. 8:971-975. [DOI] [PMC free article] [PubMed] [Google Scholar]