Abstract
Rhinoliths consist of a central nidus with calcification resulting in calcareous concretions within the nasal cavity. They are uncommon in the literature despite a propensity particularly in children to insert foreign bodies into their nose and ears. We present the case of a 62-year-old woman with a longstanding undetected rhinolith with mild uncharacteristic symptoms. Radiographic examination revealed anatomical alteration of the inferior turbinate that was attributed to the long presence of the rhinolith in the nasal cavity. The management of the rhinolith and a review of the literature are presented.
Background
Rhinoliths consist of a nidus that has undergone calcification resulting in calcareous concretions within the nasal cavity. A variety endogenous or exogenous objects can trigger the deposition of salts.1
It is not known how long it takes a rhinolith to form. A growth period of up to 15 years for the formation and eventual detection of a rhinolith has been reported.2
These entities can be asymptomatic for a long time before symptoms develop. Patients complain mainly of unilateral nasal obstruction and/or purulent rhinorrhea. Headache, epistaxis, localised pain, and nasal and oral malodour can also be present.1 3 4 5 Rhinoliths may be detected during an ear, nose and throat (ENT) examination due to the nasal symptoms, or incidentally during radiological examination of the face.
We present the case of a woman with an undetected rhinolith, who had long been treated unsuccessfully by her pneumonologist on account of a non-productive cough, and had also sought a dental consultation because of oral malodour.
Case presentation
A 62-year-old female Greek patient reported to our ENT clinic after a consultation with her dentist because of oral malodour that had persisted for a year despite thorough personal dental hygiene. The clinical dental examination was unremarkable. A postero-anterior plain radiograph of the skull showed a radiopaque circular mass located on the floor of the left nasal cavity.
Her medical history included a multinodular goitre badly controlled with medication, and a cough lasting for several months despite treatment.
Anterior rhinoscopy revealed a greyish-brown mass covered with a purulent secretion on the floor of the anterior third of the left nasal cavity beyond a mild horizontal projection of the anterior septum (figure 1). The object displaced the anterior atrophic edge of the inferior turbinate superiorly. A rigid endoscopic examination (0o, 4 mm) revealed oedematous mucosa along the nasal cavity and a thin linear purulent secretion extending to the choana.
Figure 1.
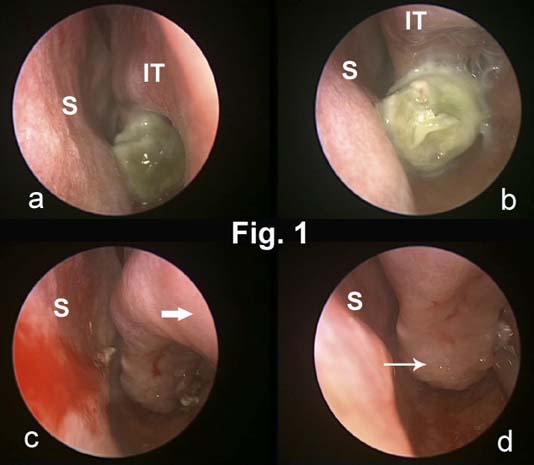
(A,B) Endoscopic view of the rhinolith on the floor of the left nasal cavity before and after mobilisation. (C) Left nasal cavity after removal of the rhinolith. Marked atrophy of the head (bold arrow) and anterior third of the inferior turbinate is visible. (D) Mild polypoid degeneration of the turbinate mucosa posterior to the rhinolith (slim arrow) can be seen. IT, inferior turbinate; S, septum.
CT scan showed a well-defined ovoid-shaped mass measuring about 1.1×1.2 cm with a dense radiopaque border and a central radiolucent area (nucleus) (figure 2). The mass was located on the floor of the nasal cavity just below the inferior turbinate with absence of bone erosion. Clear atrophy of the osseous and mucosal elements of the anterior third of the inferior turbinate was visible. The level of origin of the inferior turbinate from the lateral nasal wall was displaced superiorly along its entire length, resulting in a higher inferior nasal meatus in contrast to the right side (figure 2). The sinuses were free of pathological findings.
Figure 2.
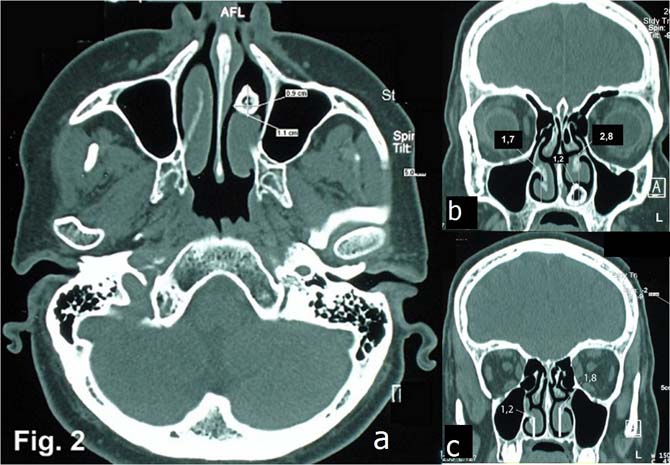
Axial CT image (A) shows a radiopaque object with a radiolucent core (anteroposterior, sagittal dimensions were 9×11 mm) in the anterior third of the left nasal cavity. Atrophy of mucosa and os turbinalis is visible. Coronal CT views of the anterior (B) and middle (C) third of the inferior nasal meatus show the height difference between the left (2.8 cm/1.8 cm) and right (1.7 cm/1.2 cm) meatus. No other anatomical alterations were detected.
The patient denied the introduction of a foreign body into her nose.
Based on these findings the diagnosis of a rhinolith was established and an endoscopic-assisted removal proposed. Because of her history of unsuccessfully treated goitre, the patient was referred to endocrinologists who considered a subtotal thyroidectomy.
Treatment
Both procedures took place during the same operation under general anaesthesia. With a rigid 0o nasal endoscope the object was visualised and mobilised with a freer dissector. We crushed the outer laminations of the rhinolith to minimise its size and removed the approximately 9×10 mm core. The gross macroscopic appearance of the mass was that of a hard core surrounded by laminations. The turbinate mucosa located behind the mass showed mild polypoid degeneration. No bleeding was encountered and no nasal anterior packing was needed. Identification of the nidus composition was not possible.
Outcome and follow-up
The patient had an uneventful postoperative follow-up and her symptoms disappeared.
Discussion
Rhinoliths are rarely reported in the literature despite the propensity observed particularly in children to insert foreign bodies into their nose and ears.
As the name suggests (‘lith’ means stone) they are hard objects, probably produced after a chronic inflammatory reaction activated by intranasal insertion of a foreign body, which acts as a nidus upon which mineral salts are deposited.1 The exact pathogenesis is unknown, but precipitating factors such as chronic inflammation, the presence of bacteria and obstruction of nasal secretions are thought to lead to the deposition of siderite, ferrihydrite or mineral salts such as calcium carbonate, calcium phosphate and magnesium phosphate around the nidus, resulting in calcareous concretions.1 2 4 6 7 8
The foreign body can be exogenous or endogenous. Exogenous bodies include buttons, stones, sand, peas, beads, fruit seeds and remnants of nasal tampons, while endogenous bodies include blood clots, epithelial debris, teeth and bone sequestra.1 8 9 The main entry route is via the anterior nares, with some suggestion of retronasal entry in the event of emesis.6
Rhinoliths are mainly found on the nasal cavity floor, but the frontal and maxillary sinuses have also been reported. They usually present unilaterally and are more often diagnosed in the third decade of life with a female predilection and rare manifestation in children.4 6 10
Bartholin first described rhinoliths in 1654 and the first chemical analysis was conducted by Axmann in 1829.4 11
Typical presenting symptoms are unilateral nasal obstruction, purulent nasal discharge, malodour and epistaxis, but crusting, localised pain, chronic headache, anosmia and swelling of the nose and surrounding face have been documented.4 6 10 Rhinoliths often remain asymptomatic or with only subtle signs for a long time.2 12
As our patient had no nasal symptoms, she did not attend an ENT specialist. Her main complaints were oral malodour and a year-long non-productive cough. She denied the insertion of any foreign body into her nose.
The first radiographic description of a rhinolith was presented by Macintyre in 1900.4 13 Postero-anterior plain x-ray, panoramic radiography and CT scan are the standard modalities for diagnosis. A CT scan is superior because of its ability to show small calcification deposits and detailed information on the contiguous structures, thus helping in the differential diagnosis. The commonly seen radiological features are central radiolucency (if there is an organic nidus) with surrounding radiopacity. There may be laminations and a corrugated surface.1 4 13 14 15
The CT scan of our patient showed the typical features of a rhinolith, as well as alteration in the anatomy of the lateral wall of the left nasal cavity. The level of origin of the left lower turbinate was dislocated superiorly along the entire length resulting in a higher inferior meatus. The bony and mucosal elements of the anterior third of the turbinate were atrophic. These findings, in conjunction with the absence of other anatomic malformations, suggested a very longstanding (probably since childhood) intranasal object resulting in altered outgrowth of the concha. The patient could not recall any acute or extended chronic nasal inflammation during her adult life.
Although clinical examination, endoscopy and CT scan are almost definitively diagnostic, in the differential diagnosis we should also consider osteoma, haemangioma, calcified nasal polyps, odontoma, impacted teeth, dermoid, chondrosarcoma, osteosarcoma, and tubeculous and syphilitic calcification.4 6 10
Complications reported in the literature include erosions/perforation of the septum/palate and recurrent inflammatory processes such as sinusitis, middle otitis or dacryocystitis.4 6
We assume that the anatomical alteration in our patient was a complication of the rhinolith without any impact on her well-being. Slight polypoid degeneration in the conchal mucosa was also detected.
Removal through the nostrils or endoscopically assisted removal are the most frequently used methods. The rhinolith can be removed as an intact object or after crushing to reduce its size. Lithotripsy could also be used to disintegrate the rhinolith. In rare complicated cases where the open route is necessary, lateral rhinotomy can be performed.1
Learning points.
-
▶
Rhinoliths are rare entities, with an estimated incidence of 1:10 000 otolaryngological outpatient examinations.
-
▶
The slow growth and subtle or absent symptoms demand a high index of suspicion so as to establish the diagnosis as soon as possible.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Hadi U, Ghossaini S, Zaytoun G. Rhinolithiasis: a forgotten entity. Otolaryngol Head Neck Surg 2002;126:48–51 [DOI] [PubMed] [Google Scholar]
- 2.Shaw LC. Rhinolith of endogenous origin: A rare entity. Surg Pract 2007;11:48–50 [Google Scholar]
- 3.Yuca K, Caksen H, Etlik O, et al. The importance of rigid nasal endoscopy in the diagnosis and treatment of rhinolithiasis. Auris Nasus Larynx 2006;33:19–22 [DOI] [PubMed] [Google Scholar]
- 4.Singh RK, Varshney S, Bist SS, et al. A case of rhinolithiasis. Online J Health Allied Scs 2008;7(2):7 [Google Scholar]
- 5.Dib GC, Tangerina PR, Abreu EC, et al. Rhinolithiasis as cause of oronasal fistula. Rev Bras Otorrinolaringol 2005;71:101–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patil K, Guledgud MV, Malleshi SN. Rhinolith. Indian J Dent Res 2009;20:114–6 [DOI] [PubMed] [Google Scholar]
- 7.Orhan K, Kocyigit D, Kisnisci R, et al. Rhinolithiasis: an uncommon entity of the nasal cavity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:28–32 [DOI] [PubMed] [Google Scholar]
- 8.Senkal HA, Süslü AE, Ünal ÖF. A rare cause of rhinolithiasis: ectopic tooth. Int J Pediatr Otorhinolaryngol Extra 2006;1:249–52 [Google Scholar]
- 9.Aksungur EH, Binokay FB, Biçakçi K, et al. A rhinolith which is mimicking a nasal benign tumor. Eur J Radiol 1999;31:53–5 [DOI] [PubMed] [Google Scholar]
- 10.Sumbullu MA, Tozoglu U, Yoruk O, et al. Rhinolithiasis: the importance of flat panel detector-based cone beam computed tomography in diagnosis and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;107:e65–7 [DOI] [PubMed] [Google Scholar]
- 11.Appleton SS, Kimbrough RE, Engstrom HI. Rhinolithiasis: a review. Oral Surg Oral Med Oral Pathol 1988;65:693–8 [DOI] [PubMed] [Google Scholar]
- 12.Ezsiás A, Sugar AW. Rhinolith: an unusual case and an update. Ann Otol Rhinol Laryngol 1997;106:135–8 [DOI] [PubMed] [Google Scholar]
- 13.Royal SA, Gardner RE. Rhinolithiasis: an unusual pediatric nasal mass. Pediatr Radiol 1998;28:54–5 [DOI] [PubMed] [Google Scholar]
- 14.Pitt SK, Rout PG. Rhinoliths presenting during routine radiography: two cases. Dent Update 2000;27:505–7 [DOI] [PubMed] [Google Scholar]
- 15.White SC, Pharoah MJ. Oral radiology principles and interpretation. Fifth edition St. Louis:Mosby; 2000 [Google Scholar]


