Abstract
The efficiency of malaria prevention during pregnancy was compared between three studies in Benin for malaria infection of the placenta (MIP) and low birth weight (LBW). The first was carried out when chloroquine prophylaxis was still recommended, the second was an intermittent preventive treatment in pregnancy (IPTp) clinical trial comparing sulfadoxine pyrimetamine (SP) versus mefloquine, and the third was an observational study after SP-IPTp national implementation. We showed an association between the use of IPTp and the reduction of LBW (10% with national IPTp and 8.7% in IPTp trial versus 15.7% in pre-trial study). The effect on MIP was better in the trial (2.9% versus 11.2% and 16.7% for national IPTp and pre-trial studies, respectively). In spite of a good overall compliance with the national IPTp (with 84% of women taking at least one dose of SP), there are still failures in adherence to the directly observed therapy (DOT) scheme and needs for better training of health staff.
Introduction
Intermittent preventive treatment in pregnancy (IPTp) with sulfadoxine pyrimetamine (SP) has been recommended by the World Health Organization (WHO) to protect women from malaria during pregnancy since early 2000s.1 Malaria during pregnancy is responsible for maternal anemia and low birth weight, which are major risk factors for morbidity and mortality during the first 1 year of life.2–4 Before 2004, malaria prophylaxis with chloroquine (CQ) was the official policy for pregnant women in all West African countries, but the quick increase of parasite resistance to the drug justified a radical change to SP-IPTp.1
In Benin, the new national guidelines recommending the use of IPTp with SP instead of CQ were only applied to the whole territory in 2006. In 2004, a study was set up in the city of Ouidah to assess the efficacy of CQ prophylaxis in pregnant women during 1 year before the onset of an IPTp clinical trial.5 This trial was carried out between 2005 and 2008 to compare SP-IPTp with IPTp combined with mefloquine (MQ), with the aim to identify an alternative molecule to replace SP when it loses its efficacy.6,7 In June 2007, a third study was carried out in Tori Bossito, a rural zone in the neighborhood of Ouidah, focusing on the occurrence of first malaria infections in infants. In this area, the national SP-IPTp had been implemented for over year.8
The objective of this paper is to compare the efficiency of malaria prevention during pregnancy in the three studies (before the national implementation of IPTp when CQ prophylaxis was still recommended, in a clinical trial testing IPTp with SP versus MQ, and in the context of national IPTp) for the two indicators: malaria infection of the placenta (MIP) and birth weight. In the last part of the paper, the results of the Tori Bossito (TB) study are specifically analyzed to understand the characteristics of the distribution of IPTp through the national health system and the consequences on public health issues.
Methods
Ouidah studies.
The designs of the two studies have been described elsewhere.5,7 Briefly, an observational study followed by a clinical trial was set up in Ouidah, a town located 23 km west of Cotonou in Benin, an area where malaria transmission is high with two seasonal peaks (Figure 1). In 2004, while the national guidelines were still for the prescription of a weekly CQ prophylaxis, all women attending the two main maternity clinics of the area (Kindji and Hôpital de Zone) were studied at delivery. Placental infections were determined, and birth weights were measured. In the following years (2005–2008), a clinical trial was conducted in the same maternity clinics to compare SP and MQ for IPTp. Women > 3 months pregnant, with no recent intake of SP or MQ and no history of intolerance to these drugs, were included in the clinical trial. The drug intakes were strictly supervised by well-trained midwives during antenatal visits (ANVs) and scheduled to be administrated at the second and third trimester of pregnancy.
Figure 1.
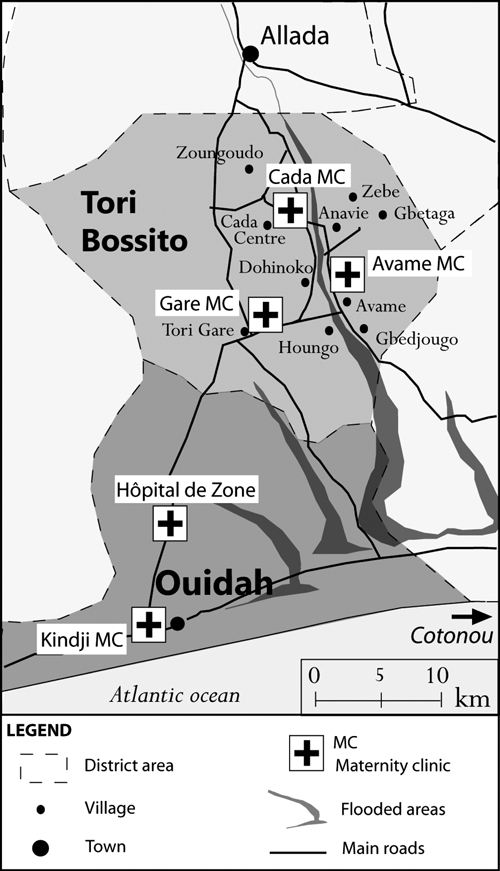
The two study sites of Ouidah (two maternity clinics) and Tori Bossito (three maternity clinics), Benin (from Charlotte Pierrat, IRD UMR 216, Paris, France).
Tori Bossito study.
The Tori Bossito study was carried out in a rural area of Benin located 17 km north of Ouidah (Figure 1). All women living in nine villages of the area and delivering in one of the three main health centers providing birth attendance (Tori Avame, Tori Cada, and Tori Gare) were enrolled. This study investigated the relationship between MIP and the occurrence of malaria infections in infants during their first months of life. It was designed to follow 600 newborns clinically and parasitologically during 18 months. This paper focuses on the mothers who were included between June 2007 and July 2008. They all had received IPTp with SP through the national health system as recommended by the WHO.1 Details about the area and the women have been described extensively elsewhere.8
In particular, data relative to the use of IPTp or CQ during pregnancy were collected from the women after delivery and health records: number of doses and date of last intake of IPTp, intake of CQ (yes/no), and duration of prophylaxis.
All protocols were approved by the ethics committee of the Republic of Benin and the Institut de Recherche pour le Développement (IRD) ethics committee.
Human immunodeficiency virus status of women.
Human immunodeficiency virus (HIV) infection is known to be associated with increased risk of malaria and low birth weight (LBW), and it may have affected the occurrence of MIP and LBW. In the clinical trial, HIV screening was routinely undertaken by the national program during the trial, but the HIV status of women was only determined for 50% of women.9 HIV-positive women were excluded from the analysis. Generally, the prevalence of HIV is low (2%) in this area.10 At the time of the pre-trial, there was no determination of HIV status in the clinics of Ouidah. In Tori Bossito, the national program for HIV diagnosis during pregnancy began its activities in 2007. Only one maternity clinic (Tori Gare, where recruitment was the lowest) proposed HIV status determination, and only 9% (57/617) of all women of the study were tested for HIV infection (one HIV-positive woman with a normal birth weight). Considering the overall low HIV prevalence, we decided not to take into account these data.
Biological methods.
In all studies, thick and thin blood smears were performed on the peripheral and placental blood of the mothers at delivery. Plasmodium falciparum asexual blood forms were counted on Giemsa-stained smears. A blood smear was declared negative when no parasite was detected after the count of 500 white cells.8
Statistical procedures.
Comparison between studies.
The results of the three studies were compared by univariate analysis on MIP, LBW, and other covariates, such as gravidity status, education of women, number of ANVs, and use of impregnated bed nets. Because the efficacy of IPTp with MQ and SP were very close at the end of the clinical trial, both arms were kept pooled for the present analysis.9 When non-parametric methods were required, a Fisher exact test or Kruskall–Wallis test was applied.
Risk factors for MIP and LBW.
In a second analysis, risk factors for MIP and LBW were analyzed by logistic regression on the pooled data from the three studies. For the analysis of birth weight, only live singleton births were selected. The identification of each study (Ouidah cross-sectional, Ouidah randomized trial, and Tori Bossito cross-sectional), representing both the type of prevention (CQ, IPTp with SP or MQ, and national IPTp with SP) and the quality of supervision, was defined as a covariate and included in the statistical model.
For the multivariate analysis, all variables with a P value of below 0.20 in univariate analysis were initially introduced into the model removed after a backward step-wise selection procedure, leaving only variables with a P value below 0.05 in the final model. All analyses were performed using Stata v. 8.0 (Stata Corp., College Station, TX).
Results
In all three studies, women were studied during a complete year (2004 for the Ouidah pre-trial study, 2005 for the Ouidah clinical trial, and 2007–2008 for the Tori Bossito study) to account for seasonal variations in malaria transmission.
Study populations.
In Ouidah, recruitment was done in the same maternity clinics (Kindji and Hopital de zone) for both studies. Data analysis was performed on 1,090 women in the pre-trial study and in 609 women in the clinical trial (restricted to the first 1 year of the study and women taking SP or MQ). In the pre-trial study, 95% of the women had taken CQ, with a mean self-reported duration of prophylaxis of 5 months. In the clinical trial, with a close follow-up of the women, 95% had received two IPTp doses. Analysis on LBW was done after excluding twins (47) and stillbirths (62; 55 in the pre-trial study and 7 in the trial).
In Tori Bossito, 660 women were eligible for the study. Among them, 31 refused or did not meet inclusion criteria; 629 deliveries were observed in the three maternity clinics of the area, resulting in 656 newborns (603 singletons, 25 twins, and 1 triplet). Ten pregnancies ended with a stillbirth. Data were missing for 12 women who had stillbirths or early neonatal death and their offspring. Finally, analysis of the mothers was done on 617 women. Excluding twins and triplets, 590 newborns could be analyzed for LBW.
Women and newborns characteristics.
In the two studies carried out in Ouidah, 24% of the women were primigravidae, and 50% did not receive scholar education. The average age of women was 25 years, and 68% were from the Fon ethnic group. More information about women's characteristics for these two studies is presented elsewhere.5,7
In Tori Bossito, 14.8% of the women were primigravidae, and 84.8% of the women did not receive scholar education. The average age of women was 27.5 years (standard deviation [SD] = 5.6); 72.5% were from the Tori ethnic group, 10.6% were from the Fon ethnic group, and 16.9% were from other groups (Yoruba, Mina, and others). Of the women, 32.6%, 47.9%, and 19.5% delivered in the maternity clinics of Tori Avamè, Tori Cada, and Tori Gare, respectively (Table 1).
Table 1.
Comparison between the three studies in Benin
| Ouidah pre-trial study (2004–2005) | Ouidah clinical trial (2005–2008) | Tori Bossito (2007–2008) | P* | |
|---|---|---|---|---|
| Number of women | 1,090 | 609 | 617 | |
| Area | Semi-rural | Semi-rural | Rural | |
| Malaria prophylaxis | CQ | IPTp (SP or MQ) | IPTp SP (±CQ) | |
| Gravidity status | ||||
| Multigravidity | 823 (75.5) | 464 (76.2) | 522 (85.2) | |
| Primigravidity | 267 (24.5) | 145 (23.8) | 91 (14.8) | P < 10−3 |
| Mean age (years) | 25.4 (SD = 5.9; range = 13–44) | 25.2 (SD = 5.5; range = 15–45) | 27.4 (SD = 5.6; range = 16–49) | P < 10−3 |
| Age class | ||||
| ≤ 20 | 255 (23.8) | 141 (23.1) | 84 (13.8) | |
| 21–25 | 373 (34.8) | 230 (37.8) | 149 (24.4) | P < 10−3 |
| 26–30 | 244 (22.8) | 145 (23.8) | 217 (35.5) | |
| > 30 | 200 (18.6) | 93 (15.3) | 161 (26.3) | |
| Education of women | ||||
| No education | 527 (50.1) | 289 (47.4) | 519 (84.8) | |
| Partial primary | 359 (34.2) | 231 (37.9) | 64 (10.5) | |
| Complete primary | 165 (15.7) | 89 (14.6) | 19 (3.1) | |
| Secondary or more | 0 (0) | 0 (0) | 10 (1.6) | P < 10−3 |
| Number of ANVs | ||||
| ≤ 3 ANVs | 400 (37.2) | 157 (26.3) | 255 (43.7) | |
| > 3 ANVs | 676 (62.8) | 439 (73.7) | 329 (56.3) | P < 10−3 |
| Placental malaria† | ||||
| Yes | 176 (16.7) | 17 (2.9) | 68 (11.2) | |
| No | 876 (83.3) | 568 (97.1) | 538 (88.8) | P < 10−3 |
| Bed net use | ||||
| No | 246 (24.4) | 155 (25.4) | 204 (33.7) | |
| Yes | 764 (75.6) | 454 (74.55) | 401 (66.3) | P < 10−3 |
| Gender | ||||
| Female | 568 (52.1) | 285 (46.9) | 288 (49.2) | P = 0.11 |
| Male | 522 (47.9) | 323 (53.1) | 298 (50.8) | |
| Average birth weight (g) | 2,876.2 (SD = 491.2; range = 800–5,000) | 3,059.8 (SD = 433.3; range = 1,340–4,434) | 2,979.0 (SD = 402.2; range = 1,430–4,460) | P < 10−3 |
| LBW | ||||
| No | 916 (84.3) | 556 (91.3) | 529 (90.0) | P < 10−3 |
| Yes | 171 (15.7) | 53 (8.7) | 59 (10.0) |
CQ = chloroquine; MQ = mefloquine; IPTp = intermittent preventive treatment; ANVs = antenatal visits; CI = confidence interval; SD = standard deviation.
Statistically significant (P < 0.05).
Defined as the presence of asexual stage parasites in the placental thick blood smear.
Comparison of the three studies.
Table 1 presents the comparison of the three studies in terms of MIP, LBW, and covariates. The comparison between women from the pre-trial study and the clinical trial in Ouidah, already presented in Briand and others,7 showed no difference on general characteristics between the two groups of women. However, the proportions of primigravidae, type of education of women, number of ANVs, and rates of impregnated bed nets varied significantly between Ouidah and TB. The proportion of primigravidae was lower in the TB study (14.8% versus 24.5% and 23.8% in the Ouidah pre-trial and clinical trial, respectively), and women were slightly older. Women from the rural area of TB were more frequently unschooled than those in the already urbanized zone of Ouidah (84.8% versus 50.1% and 47.4%). Concerning ANVs, the clinical trial showed that 73.7% of women had attended more than three visits (probably related to the investigators' good supervision of women). These proportions were 62.8% in the pre-trial study and only 56.3% in the rural area of Tori Bossito. The use of impregnated bed nets was lower in TB (66.3%) than in Ouidah (approximately 75% in both studies).
Rates of MIP and LBW varied significantly between the three studies. The proportion of MIP was 16.7% during the Ouidah pre-trial study, 2.9% in the Ouidah clinical trial, and 11.2% in the TB study. For LBW, proportions were close to each other in the Ouidah clinical trial and in TB (8.7% and 10%, respectively) compared with 15.7% in the pre-trial study. The mean birth weight was 2,979 g in TB, 3,059.8 g in the Ouidah clinical trial, and 2,876.2 g in the Ouidah pre-trial.
Risk factors for MIP and LBW.
When analyzing the pooled data from the three studies, placental malaria was found to be significantly associated with the women's gravidity and the study, as shown in Table 2. Primigravidae had a 2.3-fold increased risk to present MIP at delivery compared with multigravidae. After adjusting on gravidity, the effect of age on MIP disappeared. Women from the Ouidah clinical trial, whose IPTp was given in a context of strict supervision, or women taking the national IPTp in TB had significantly reduced risks to present MIP compared with women from the Ouidah pre-trial study who were still taking a CQ prophylaxis (adjusted odds ratio [aOR] = 0.15, 95% CI = 0.09–0.24 and aOR = 0.67, 95% CI = 0.50–0.91, respectively).
Table 2.
Factors associated with MIP
| Factor | Univariate analysis | Multivariate analysis | P* | |
|---|---|---|---|---|
| Crude OR (95% CI) | Adjusted OR (95% CI) | |||
| Study | ||||
| Pre-trial Ouidah | 176/1,052 (16.7) | 1.00 | 1.00 | |
| Trial Ouidah | 17/568 (2.9) | 0.15 (0.09–0.25) | 0.15 (0.09–0.24) | P < 10−3 |
| Tori Bossito | 68/608 (11.2) | 0.63 (0.47–0.85) | 0.67 (0.50–0.91) | P = 0.01 |
| Age class | ||||
| ≤ 20 | 87/468 (18.6) | 1.00 | ||
| 21–25 | 91/730 (12.5) | 0.62 (0.45–0.86) | ||
| 26–30 | 48/588 (8.2) | 0.39 (0.27–0.57) | ||
| > 30 | 31/438 (7.1) | 0.33 (0.22–0.51) | ||
| Gravidity status | ||||
| Multigravidity | 167/1,754 (9.5) | 1.00 | 1.00 | |
| Primigravidity | 93/489 (19.0) | 2.23 (1.69–2.94) | 2.29 (1.72–3.05) | P < 10−3 |
| Bed net use | ||||
| No | 81/584 (13.9) | 1.00 | ||
| Yes | 167/1,573 (10.6) | 0.74 (0.55–0.98) | ||
CI = confidence interval; OR = odds ratio.
Statistically significant result (P < 0.05).
Similarly, LBW was found to be associated with the occurrence of MIP, gravidity status, use of bed nets, number of ANVs, newborn's gender, and study (Table 3). Women presenting MIP had an increased risk to give birth to an LBW baby (aOR = 1.66, 95% CI = 1.15–2.40; P = 0.01). Primigravidae had an over 2-fold increased risk to have a LBW newborn compared with multigravidae (aOR = 2.50, 95% CI = 1.87–3.36; P = 10−3). As for MIP, the effect of age disappeared after adjusting on gravidity. Female babies were more at risk than males to suffer from LBW (P < 10−2). Women sleeping under bed nets and women having attended more than three ANVs had significantly less LBW than women who did not use bed nets or had poor attendance to ANVs (Table 3). Finally, taking IPTp in the clinical trial (Ouidah) or through the national context of implementation (TB) had a protective effect on LBW, with an aORs = 0.55 (95% CI = 0.38–0.78) and aOR = 0.57 (95% CI = 0.40–0.81), respectively, compared with the use of CQ during pregnancy in the Ouidah pre-trial study (P value < 10−2 for both).
Table 3.
Factors associated with LBW
| Factor | Univariate analysis | Multivariate analysis | P* | |
|---|---|---|---|---|
| Deliveries (%) | Crude OR (95% CI) | Adjusted OR (95% CI) | ||
| Study | ||||
| Pre-trial Ouidah | 171/1,087 (15.7) | 1.00 | 1.00 | |
| Trial Ouidah | 53/609 (8.7) | 0.51 (0.37–0.71) | 0.55 (0.38–0.78) | P < 10−2 |
| Tori Bossito | 59/588 (10.1) | 0.60 (0.44–0.82) | 0.57 (0.40–0.81) | P < 10−2 |
| Placental malaria | ||||
| No | 220/1,956 (11.2) | 1.00 | 1.00 | |
| Yes | 56/257 (21.8) | 2.20 (1.58–3.05) | 1.66 (1.15–2.40) | P < 10−2 |
| Age class | ||||
| ≤ 20 | 96/477 (20.1) | 1.00 | ||
| 21–25 | 92/745 (12.4) | 0.56 (0.41–0.76) | ||
| 26–30 | 50/594 (8.4) | 0.36 (0.25–0.53) | ||
| > 30 | 38/446 (8.5) | 0.37 (0.25–0.55) | ||
| Gravidity status | ||||
| Multigravidity | 172/1,782 (9.7) | 1.00 | 1.00 | |
| Primigravidity | 110/500 (22.0) | 2.64 (2.03–3.43) | 2.50 (1.87–3.36) | P < 10−3 |
| Bed net use | ||||
| No | 101/596 (16.9) | 1.00 | 1.00 | |
| Yes | 167/1,600 (10.4) | 0.57 (0.44–0.75) | 0.70 (0.52–0.94) | P < 10−2 |
| Number of visits | ||||
| ≤ 3 ANVs | 127/799 (15.9) | 1.00 | 1.00 | |
| > 3 ANVs | 145/1,429 (10.1) | 0.60 (0.46–0.77) | 0.64 (0.48–0.84) | P < 10−2 |
| Gender | ||||
| Male | 116/1,139 (10.2) | 1.00 | 1.00 | |
| Female | 166/1,142 (14.5) | 1.50 (1.16–1.93) | 1.60 (1.22–2.12) | P < 10−2 |
Twins and stillbirths were excluded from analysis of LBW. CI = confidence interval; OR = odds ratio.
Statistically significant result (P < 0.05).
Malaria prevention in TB.
In this area where the national IPTp policy was implemented, 84% (511/608) of the women declared having received at least one dose of IPTp during their pregnancy. Rates of IPTp coverage according to the maternity clinic were 96% in Tori Avamè and 78% in both Tori Cada and Tori Gare. Among women who reported IPTp intakes with doses notified in health records, 17.3% (85/492) had taken one dose, and 82.7% (407/492) had two doses of SP or more; 8.9% (54/608) of all women were still taking CQ prophylaxis alone, and 7.1% (43/608) had not taken any prophylaxis (CQ or IPTp). We eliminated this last group from the following analysis. We analyzed the relation between malaria prevention and MIP or LBW in the following groups: (1) use of IPTp (at least one dose) with or without CQ and (2) use of CQ alone.
In the study area, a significant effect of the maternity clinic where the delivery had occurred was found, with an increased risk to present MIP in women delivering in Tori Cada and Tori Gare maternity clinics compared with Tori Avamè (aOR = 2.42, 95% CI = 1.23–4.78; P = 0.01 and aOR = 2.48, 95% CI = 1.12–5.49; P = 0.02, respectively). There was no influence of SP-IPTp compared with CQ prophylaxis on the occurrence of MIP or LBW (8.9% versus 15.1% and 9.4% versus 7.8% respectively; not significant). The relationships between MIP or LBW and gravidity or use of bed nets in Tori Bossito were similar as in the pooled analysis; primigravidity was a risk factor for both MIP and LBW, and the use of bed nets was a risk factor for LBW only (data not shown).
Discussion
One year after the national implementation of SP-IPTp in Benin, we showed that the overall compliance in the area of Tori Bossito was good, with a substantial effect on the reduction of LBW. This effect was close to the results obtained in a randomized trial in the nearby area of Ouidah (10% and 8.7% LBW, respectively) and much higher than the proportion observed in the pre-trial observation year (15.7%), when women were still taking a weekly CQ prophylaxis. However, the anti-parasite efficacy was not as good as in the trial (11.2% of placenta infection in the delivering women of Tori Bossito versus an overall 2.9% in the trial, 2.1% in the MQ group, and 3.7% in the SP group) in an area where in vivo resistance to SP may reach 50% in children below 5 years.11
Although populations of women were similar between the clinical trial and the pre-trial study7 in Ouidah, differences were observed with women from Tori Bossito, although the two sites were only 17 km apart. The latter women were less educated and had a lower attendance to ANVs, which may be characteristic of rural areas. Women from Tori Bossito were older, and only 15% were primigravidae, possibly because of migrations of young women to Cotonou for employment. There are several risks of biases in comparing observational studies (Ouidah pre-trial study and Tori Bossito study) and a controlled trial and more generally, in comparing investigations held in comparable sites but at different times. However, even if there may exist differences in malaria transmission between sites or differences in terms of treatment seeking or patient management between maternities, the effect of the study site on MIP or LBW stayed unchanged after adjusting on the characteristics of the populations, and we are confident that the differences observed between the sites on these indicators were mainly attributable to the type and the mode of administration of anti-malarial prevention.
In Tori Bossito, the question of intake of SP-IPTp or CQ during pregnancy was asked to the women by the supervisor, and doses were copied from the health records. The quality of this interview variable is questionable, particularly for the number of intakes of SP. Also, some local practices were found to differ from the official recommendations; for instance, in the maternity clinic of Tori Cada, two SP doses were given to the pregnant women at the first ANV, but they were given with the instruction to postpone the intake of the second dose. However, SP-IPTp seemed to be more efficacious than CQ prophylaxis in reducing MIP (8.9% and 15.1%, respectively), even if the difference was not significant. Despite a possible selection of the women taking only CQ in the study area, these results are consistent with the proportion of MIP evidenced by the pre-trial study (16.7%) and the very high rate of in vivo resistance to CQ (85.7%) found in Ouidah children in 2005.11 More surprising is the proportion of LBW, slightly higher in the SP-IPTp than in the CQ women, although not significantly. Even if the number of women was small in the CQ group and the selection of these women was probably biased, one cannot rule out the possibility of a direct effect (other than anti-parasitic) of CQ on birth weight, as previously suggested in the pre-trial.5 A similar study performed in 2005 assessed the impact of a national IPTp program on prevalence of maternal peripheral infection and LBW in Gabon. It compared two cross sectional surveys, when CQ was still recommended and 2 years later, after national IPTp implementation. The prevalence of maternal peripheral infection dramatically dropped from 10.5% to 1.7% (risk ratio = 0.16; P < 0.001), whereas the decrease in LBW was less pronounced (11.7% versus 10.3%). These results support the main findings of our analysis, showing the strong anti-parasitical efficacy of SP compared with CQ and the possible paradoxical effect of CQ on LBW.12
In 2000, African leaders decided at the Abuja conference to ensure that 60% of pregnant women could benefit from insecticide treated mosquito nets (ITNs) and have access to IPTp by 2005.13 However, in 2005, only one-half of the countries had adopted IPTp.14 The five first countries (Uganda, Tanzania, Malawi, Zambia, and Kenya) that began to use IPTp in the 1990s because of high rates of resistance to CQ still had, in their majority, low rates of coverage after several years of implementation. Based on the experiences of these countries, Hill and Kazembe14 in 2006 and Crawley and others15 in 2007 aimed to identify facilitating factors and operational challenges to improve IPTp distribution, which, in turn, may benefit West African countries implementing this policy. Low attendance to ANVs and long delays before the first visit (especially in women hiding their pregnancy) were among the main reasons for low coverage in Uganda.16 In Gambia and Tanzania as well, the intake of two SP doses was quite uncommon.17,18 In Tori Bossito, women are well-followed during their pregnancy, with an average of four ANVs; however, it seems, regarding to anterior studies, that even high rates of attendance to ANVs are not sufficient for a good IPTp coverage and uptake,14 because the quality of service delivery and the community perceptions and behavior have a great importance as well.14
Among the factors that need to be improved, one of the main ones is the poor adherence to the official recommendations. In the particular context of the clinical trial, doses were strictly supervised by well-trained midwives in accordance with the directly observed therapy (DOT) scheme, and women were looked after by investigators for the second dose. In Tori Bossito, compliance with the recommendations that IPTp should be given under supervision was lower. Surprisingly, the IPTp coverage was not correlated with the staff and equipment of the structures. It was in the best-equipped clinic, Tori Cada, that midwives delivered the two SP doses simultaneously, thus misusing the DOT scheme. Similar observations were made in other African countries.19,20
Alternately, the low effect of IPTp on reducing MIP in Tori Bossito may also be partly related to the increase of parasite resistance to SP since 2004, when rates were found to be high in Ouidah (50% of parasite resistance to SP).11 According to Brabin and others,21 there is a need to evaluate IPTp and its implementation, coverage, and efficacy regularly. Even if SP is still providing substantial benefit to pregnant women in areas of parasite resistance to SP (until 25%, according to ter Kuile and others22), data about in vivo resistance to SP by the mean of studies on school-aged children are not available anymore. The level of parasite resistance to SP has to be assessed in every area of malaria transmission, in addition to in vitro studies and studies detecting molecular markers of resistance, by the regular observation and analysis of several indicators (rates of LBW, MIP, peripheral infection, and anemia).21,23
In conclusion, even if IPTp implemented in the area of Tori Bossito still lacks adherence to the DOT scheme, with variations from one clinic to the other, the overall compliance in pregnant women is among the highest recorded in Africa and in 2006, reached the Roll Back Malaria (RBM) objective of 80% of women taking IPTp by 2010.24 In terms of efficacy, the results of the strategy were quite encouraging on the reduction of LBW, but some progress has to be made to improve the anti-parasite effect on the placenta in a context of moderate parasite resistance to SP, probably related to an inadequate number and spacing of IPTp doses actually taken. In the near future, health workers and midwives should be trained to better apply the IPTp strategy and particularly, the DOT scheme.
ACKNOWLEDGMENTS
We are grateful to all the women and infants of Tori Bossito who agreed to participate to this project, the midwives, nurses, and health helpers of maternity health centres, the Faculté des Sciences de la Santé (FSS), the Institut des Sciences Biomédicales Appliquées de Cotonou (ISBA), and the Programme National de Lutte contre le Paludisme (PNLP) for their institutional support.
Footnotes
Financial support: The following institutions provided support: Agence Nationale de la Recherche (ANR), Institut de Recherche pour le Développement (IRD), Ministère de la Recherche et des Technologies, France, Fondation de France, and Fondation Mérieux.
Authors' addresses: Agnès Le Port, Célia Dechavanne, Valérie Briand, José Guerra, Isabelle Choudat, Florence Migot-Nabias, André Garcia, and Michel Cot, IRD/UMR 216, Mère et Enfant Face aux Infections Tropicales, Faculté des Sciences Pharmaceutiques, Université Paris, Paris, France, E-mails: Agnes.Leport@ird.fr, celia_dv@yahoo.fr, valerie.briand@gmail.com, jose8293@hotmail.com, isa.chou@gmail.com, Florence.Migot-Nabias@ird.fr, Andre.Garcia@ird.fr, and Michel.Cot@ird.fr. Gilles Cottrell, IRD, UMR216, Mère et Enfant Face aux Infections Tropicales, Cotonou, Benin, E-mail: Gilles.Cottrell@ird.fr. Aziz Bouraima and Benjamin Fayomi, Institut des Sciences Biolomédicales Appliquées (ISBA), Université d'Abomey Calavi Champ de Foire, Cotonou, E-mails: azlesage@yahoo.fr and bfayomi2@yahoo.fr. Achille Massougbodji, Faculté des Sciences de la Santé (FSS), UER de Parasitologie, Université de Cotonou, Cotonou, Bénin, E-mail: massougbodjiachille@yahoo.fr.
References
- 1.World Health Organization . A Strategic Framework for Malaria Prevention and Control during Pregnancy in the Africa Region. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 2.Steketee RW, Nahlen BL, Parise ME, Menendez C. The burden of malaria in pregnancy in malaria-endemic areas. Am J Trop Med Hyg. 2001;64:28–35. doi: 10.4269/ajtmh.2001.64.28. [DOI] [PubMed] [Google Scholar]
- 3.Steketee RW, Wirima JJ, Hightower AW, Slutsker L, Heymann DL, Breman JG. The effect of malaria and malaria prevention in pregnancy on offspring birthweight, prematurity, and intrauterine growth retardation in rural Malawi. Am J Trop Med Hyg. 1996;55:33–41. doi: 10.4269/ajtmh.1996.55.33. [DOI] [PubMed] [Google Scholar]
- 4.McCormick MC. The contribution of low birth weight to infant mortality and childhood morbidity. N Engl J Med. 1985;312:82–90. doi: 10.1056/NEJM198501103120204. [DOI] [PubMed] [Google Scholar]
- 5.Denoeud L, Fievet N, Aubouy A, Ayemonna P, Kiniffo R, Massougbodji A, Cot M. Is chloroquine chemoprophylaxis still effective to prevent low birth weight? Results of a study in Benin. Malar J. 2007;6:27. doi: 10.1186/1475-2875-6-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Briand V, Cottrell G, Massougbodji A, Cot M. Intermittent preventive treatment for the prevention of malaria during pregnancy in high transmission areas. Malar J. 2007;6:160. doi: 10.1186/1475-2875-6-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briand V, Denoeud L, Massougbodji A, Cot M. Efficacy of intermittent preventive treatment versus chloroquine prophylaxis to prevent malaria during pregnancy in Benin. J Infect Dis. 2008;198:594–601. doi: 10.1086/590114. [DOI] [PubMed] [Google Scholar]
- 8.Le Port A, Cottrell G, Dechavanne C, Pierrat C, Bouraima A, Massougbodgi A, Chandre F, Martin-Prevel Y, Migot-Nabias F, Cot M, Garcia A. First malaria infections among infants in Benin: biological, environmental and genetic determinants. Description of the study site, general methodology and study population. 2010. (submitted) [Google Scholar]
- 9.Briand V, Bottero J, Noel H, Masse V, Cordel H, Guerra J, Kossou H, Fayomi B, Ayemonna P, Fievet N, Massougbodji A, Cot M. Intermittent treatment for the prevention of malaria during pregnancy in Benin: a randomized, open-label equivalence trial comparing sulfadoxine-pyrimethamine with mefloquine. J Infect Dis. 2009;200:991–1001. doi: 10.1086/605474. [DOI] [PubMed] [Google Scholar]
- 10.Institut National de la Statistique et de l'Analyse Économique (INSAE) Demographic and Health Survey (DHS) Benin, 2006. 2007. http://www.measuredhs.com/pubs/pub_details.cfm?ID=733 Final Report. Available at. Accessed October 15, 2010. [Google Scholar]
- 11.Aubouy A, Fievet N, Bertin G, Sagbo JC, Kossou H, Kinde-Gazard D, Kiniffo R, Massougbodji A, Deloron P. Dramatically decreased therapeutic efficacy of chloroquine and sulfadoxine-pyrimethamine, but not mefloquine, in southern Benin. Trop Med Int Health. 2007;12:886–894. doi: 10.1111/j.1365-3156.2007.01859.x. [DOI] [PubMed] [Google Scholar]
- 12.Ramharter M, Schuster K, Bouyou-Akotet MK, Adegnika AA, Schmits K, Mombo-Ngoma G, Agnandji ST, Nemeth J, Afene SN, Issifou S, Onnas IN, Kombila M, Kremsner PG. Malaria in pregnancy before and after the implementation of a national IPTp program in Gabon. Am J Trop Med Hyg. 2007;77:418–422. [PubMed] [Google Scholar]
- 13.Roll Back Malaria . The African Summit on Roll Back Malaria. Abudja, Nigeria: World Health Organization; 2000. [Google Scholar]
- 14.Hill J, Kazembe P. Reaching the Abuja target for intermittent preventive treatment of malaria in pregnancy in African women: a review of progress and operational challenges. Trop Med Int Health. 2006;11:409–418. doi: 10.1111/j.1365-3156.2006.01585.x. [DOI] [PubMed] [Google Scholar]
- 15.Crawley J, Hill J, Yartey J, Robalo M, Serufilira A, Ba-Nguz A, Roman E, Palmer A, Asamoa K, Steketee R. From evidence to action? Challenges to policy change and programme delivery for malaria in pregnancy. Lancet Infect Dis. 2007;7:145–155. doi: 10.1016/S1473-3099(07)70026-9. [DOI] [PubMed] [Google Scholar]
- 16.Mbonye AK, Schultz Hansen K, Bygbjerg IC, Magnussen P. Effect of a community-based delivery of intermittent preventive treatment of malaria in pregnancy on treatment seeking for malaria at health units in Uganda. Public Health. 2008;122:516–525. doi: 10.1016/j.puhe.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 17.Brabin L, Stokes E, Dumbaya I, Owens S. Rural Gambian women's reliance on health workers to deliver sulphadoxine-pyrimethamine as recommended intermittent preventive treatment for malaria in pregnancy. Malar J. 2009;8:25. doi: 10.1186/1475-2875-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mubyazi GM, Bloch P, Magnussen P, Olsen OE, Byskov J, Hansen KS, Bygbjerg IC. Women's experiences and views about costs of seeking malaria chemoprevention and other antenatal services: a qualitative study from two districts in rural Tanzania. Malar J. 2010;9:54. doi: 10.1186/1475-2875-9-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sirima SB, Cotte AH, Konate A, Moran AC, Asamoa K, Bougouma EC, Diarra A, Ouedraogo A, Parise ME, Newman RD. Malaria prevention during pregnancy: assessing the disease burden one year after implementing a program of intermittent preventive treatment in Koupela District, Burkina Faso. Am J Trop Med Hyg. 2006;75:205–211. [PubMed] [Google Scholar]
- 20.Akinleye SO, Falade CO, Ajayi IO. Knowledge and utilization of intermittent preventive treatment for malaria among pregnant women attending antenatal clinics in primary health care centers in rural southwest, Nigeria: a cross-sectional study. BMC Pregnancy Childbirth. 2009;9:28. doi: 10.1186/1471-2393-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brabin BJ, Warsame M, Uddenfeldt-Wort U, Dellicour S, Hill J, Gies S. Monitoring and evaluation of malaria in pregnancy—developing a rational basis for control. Malar J. 2008;7((Suppl 1)):S6. doi: 10.1186/1475-2875-7-S1-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.ter Kuile FO, van Eijk AM, Filler SJ. Effect of sulfadoxine-pyrimethamine resistance on the efficacy of intermittent preventive therapy for malaria control during pregnancy: a systematic review. JAMA. 2007;297:2603–2616. doi: 10.1001/jama.297.23.2603. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization . Monitoring Antimalarial Drug Resistance. Report of WHO consultation. Geneva, Switzerland: World Health Organization; 2002. [Google Scholar]
- 24.Roll Back Malaria. Global Strategic Plan 2005–2015. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]


