Abstract
Exposure to Coxiella burnetii is a risk in the Hunter New England (HNE) region of New South Wales (NSW), Australia, based on yearly reported cases of Q fever. We assessed seroprevalence of phase II antibodies to C. burnetii by indirect immunofluorescence assay (IFA; screening at 1/50 dilution) of residents of 24 local government areas (LGA) of the HNE region of NSW. A total of 2,438 randomly selected sera sent to the Hunter Area Pathology Service for routine diagnostic purposes (not Q fever testing) during the period of 2006–2009 were tested. The overall seroprevalence in sample group was 7%. The proportion of males (59%) was higher than females (41%). In age distribution, the largest proportion (37%) of seropositives was in the > 60 years age group. Lower prevalence was observed in 0–9 years (1%) and 10–19 years (5%) age groups. The seroprevalence in different LGAs varied between 0.5% and 22%. It was highest in Guyra (22%), Gunnedah (21%), Tenterfield (18%), and Narrabri (16%), with Newcastle (0.5%), Port Stephens (2%), Lake Macquarie (3%), and Singleton (3%) being the lowest. In most of the LGAs, seroprevalence was between 6% and 12%. This report indicates a considerable exposure to C. burnetii of residents in rural areas of the HNE region and is consistent with the high notification rate for Q fever in this part of Australia.
Q fever is a worldwide endemic zoonotic disease first reported in Australia by Edward Derrick in 1937.1 It is caused by Coxiella burnetii, an obligate intracellular bacterium that humans generally acquire through the respiratory route by inhalation of infectious aerosol/dust produced by domestic livestock, especially sheep, goats, and cattle. However, Australian studies have revealed that domestic ruminants may not be the only significant reservoir of C. burnetii. Kangaroos2,3 and bandicoots4 may pose an important threat for zoonotic transfer of this pathogen. The clinical presentation of Q fever can be acute or chronic.5,6 Acute Q fever is difficult to diagnose, because influenza and other respiratory infectious diseases have similar symptoms, including fever, headache, myalgia, and pneumonia.7 Endocarditis and post-Q fever chronic fatigue are the most frequent clinical manifestations of the chronic form.8–11 Many doctors rarely consider Q fever as a differential diagnosis of an acute febrile illness unless a link with animal contact is established from the patient's history. Thus, many cases of Q fever may remain undiagnosed. After infection with C. burnetii, detectable antibodies appear in the blood within a few weeks and may last for years, even for life.12,13 The antibodies produced during a natural infection of humans react in vitro with phase I and phase II C. burnetii, with the acute serological response initially directed to phase II antigens, whereas the response in chronic infections becomes predominantly phase I. Serology is the current diagnostic modality for Q fever. Based on reported cases of Q fever, exposure to C. burnetii is considered to be a risk in the Hunter New England (HNE) region of New South Wales (NSW).14–16 The primary objective of this study was to determine the seroprevalence of Q fever antibodies in rural and urban residents, with particular attention to age groups, sex, and location (based on local government areas [LGAs]).
A total of 2,438 randomly selected serum samples sent to the Hunter Area Pathology Service and Pathology New England for routine hematology, immunology, and biochemistry, including infectious disease serology (not Q fever testing), during the period of 2006–2009 were tested. They were deidentified before use. These specimens came from residents of 24 LGAs of the HNE region of NSW (Figure 1). The specimen numbers selected were based on the population of each LGA so that the same percentage of population was tested in each LGA. Phase II antibody against C. burnetii in serum samples was detected by the indirect immunofluorescence (IF) test. Briefly, 40-well spot slides (Manzel-Glaser, Braunschweig, Germany) were coated with optimized phase II antigen obtained from a confluent culture of C. burnetii (clone 4 of 9-mile strain) grown in the XTC-2 cell line, air-dried, and fixed in acetone for 10 minutes. Sera were diluted to 1:50 in phosphate-buffered saline (PBS) with 2% casein (skim powder milk). The antigens, overlaid with sera, were incubated in a moist chamber for 30 minutes at 35°C and then washed three times in 1% PBS for 5 minutes each time. After air drying, the complex was overlaid with a mixture of fluorescein isothiocyanate (FITC)-conjugated goat anti-human immunoglobulin A (IgA), IgG, and IgM (KPL, Gaithersburg, MD). Incubation, washes, and drying were performed as before. The slides were mounted in buffered glycerol (Fronine; Laboratory Supplies, Taren Point, NSW) and read with a fluorescence microscope (Axioskop 40; Zeiss) at 400× magnification. Positive results were indicated by the presence of fluorescent C. burnetii. Q fever-positive and-negative human sera were used as controls on each slide. Individual antibody classes were not determined. The association between seroprevalence and Q fever notification rate in eight clusters of HNE region was also examined.
Figure 1.

Geographic distribution of the sampled population in the Hunter New England (HNE) region of New South Wales, Australia. The HNE region consists of 24 local government areas (LGAs). The population density of Newcastle and Lake Macquarie LGAs is much higher than the other LGAs; these areas are considered as urban populations (right map), and the rest are mostly rural areas.
The overall seroprevalence in the sample group was 7%. The distribution of Q fever-seropositive persons in different LGAs (Table 1) showed that seroprevalence varied between 0.5% and 22%. It was highest in Guyra (22%), Gunnedah (21%), Tenterfield (18%), and Narrabri (16%), with Newcastle (0.5%), Port Stephens (2%), Lake Macquarie (3%), and Singleton (3%) being the lowest. In most of the LGAs, seroprevalence was between 6% and 12%.
Table 1.
Local government area (LGA) and seroprevalence of Q fever (phase II antibody) in the HNE region of New South Wales, Australia
| LGA | Total sera tested | Q fever-positive sera | Seroprevalence (%) | |
|---|---|---|---|---|
| 1 | Guyra | 36 | 8 | 22 |
| 2 | Gunnedah | 81 | 17 | 21 |
| 3 | Tenterfield | 45 | 8 | 18 |
| 4 | Narrabri | 100 | 16 | 16 |
| 5 | Gwydir | 34 | 4 | 12 |
| 6 | Armidale | 82 | 9 | 11 |
| 7 | Tamworth | 185 | 19 | 10 |
| 8 | Muswellbrook | 100 | 10 | 10 |
| 9 | Gloucester | 31 | 3 | 10 |
| 10 | Walcha | 21 | 2 | 10 |
| 11 | Uralla | 41 | 4 | 10 |
| 12 | Great Lakes | 200 | 19 | 10 |
| 13 | Upper Hunter | 95 | 9 | 9 |
| 14 | Glen Innes | 58 | 5 | 9 |
| 15 | Inverell | 104 | 9 | 9 |
| 16 | Dungog | 57 | 4 | 7 |
| 17 | Liverpool | 32 | 2 | 6 |
| 18 | Maitland | 200 | 11 | 6 |
| 19 | Port Stephens | 200 | 4 | 2 |
| 20 | Cessnock | 160 | 6 | 4 |
| 21 | Lake Macquarie | 200 | 6 | 3 |
| 22 | Moree | 100 | 3 | 3 |
| 23 | Singleton | 76 | 2 | 3 |
| 24 | Newcastle | 200 | 1 | 0.5 |
| HNE region | 2,438 | 181 | 7 |
The proportion of males (59%) was higher than females (41%) (Figure 2).
Figure 2.

Seroprevalence to C. burnetii by sex among residents of the HNE region of New South Wales (N = 176).
In age distribution, the largest proportion (37%) of seropositives was in the > 60 years age group. Lower prevalence was observed in 0–9 years (1%) and 10–19 years (5%) age groups (Figure 3). Highest seroprevalence seemed to occur in the 20–39 years age group, which may correspond with the onset of risk because of new work practices.
Figure 3.
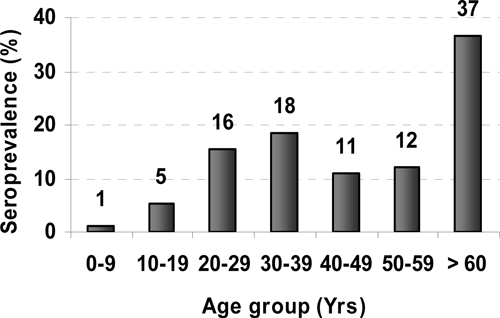
Seroprevalence to C. burnetii by age group of residents of the HNE region of New South Wales (N = 174).
This is the first seroprevalence report of Q fever among residents of the HNE region of NSW. Three features were evident: (1) there was a higher prevalence of Q fever antibody in males than females, (2) older people (> 60 years) had the highest seroprevalence, and (3) exposure was more prevalent in rural areas. Recent Q fever notification data revealed similar characteristics of the disease in the population of this region (7.4 cases per 100,000 population per annum between 2005 and 2007).15,16 However, this study indicates a higher exposure to C. burnetii than the notification system would indicate. It is unlikely that the difference in seropositivity between the older and younger age groups is a cohort effect related to the younger generation's more urbanized upbringing. Consistent with the age and sex distribution of notification data, which measures symptomatic disease, the markedly increased proportion of seropositives in males of working age and older in the seroprevalence data in this study probably reflects occupational exposure. There was no correlation between seroprevalence and notification rate in the different HNE clusters of LGA (R2 = 0.0014), which may reflect inadequate notifications of Q fever in this region. It is recognized that exposure to C. burnetii (and seroconversion) leads to only approximately 50% of patients developing symptoms.17,18 This may also partly explain the lack of correlation between seroprevalence and notification rates. In addition, there may well be underreporting of Q fever because of lack of proper laboratory diagnosis. This study reflects the seroprevalence of Q fever in a sample group of HNE residents that may or may not have been characteristic of the HNE population overall. Nevertheless, the comparative data between the LGAs are valid, because the random sampling was proportional to the population in each case.
Despite the availability of an effective vaccine, Q fever cases continue to be reported in this part of NSW, including a small outbreak in a shearing team in 2004.19 Q fever vaccinations seemed to be successful among people working in abattoirs, but many residents of rural NSW, who are potentially exposed to Q fever, remain susceptible to this disease.14 General practitioners should consider Q fever as a differential diagnosis of an acute febrile illness in rural patients. Further seroepidemiological studies in other parts of rural Australia are recommended to determine whether enhanced Q fever vaccination is appropriate.
ACKNOWLEDGMENTS
We acknowledge the technical assistance of Justine Allison, Department of Microbiology, Hunter Area Pathology Service, Newcastle, and Marion Mackintosh, Pathology New England, Tamworth.
Footnotes
Authors' addresses: Aminul Islam and Stephen Graves, Department of Microbiology, Hunter Area Pathology Service, Pathology North, John Hunter Hospital, New South Wales, Australia, and Australian Rickettsial Reference Laboratory, Barwon Health, Geelong, Victoria, Australia, E-mails: aminul.islam@hnehealth.nsw.gov.au and Stephen.Graves@hnehealth.nsw.gov.au. John Ferguson and Rod Givney, Department of Microbiology, Hunter Area Pathology Service, Pathology North, John Hunter Hospital, New South Wales, Australia. E-mails: John.Ferguson@hnehealth.nsw.gov.au and Rodney.Givney@hnehealth.nsw.gov.au.
References
- 1.Derrick EH. ‘Q' fever, a new fever entity: clinical features, diagnosis and laboratory investigation. Med J Aust. 1937;11:281–299. doi: 10.1093/clinids/5.4.790. [DOI] [PubMed] [Google Scholar]
- 2.Banazis MJ, Bestall AS, Reid SA, Fenwick SG. A survey of Western Australian sheep, cattle and kangaroos to determine the prevalence of Coxiella burnetii. Vet Microbiol. 2010;143:337–345. doi: 10.1016/j.vetmic.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Pope JH, Scott W, Dwyer R. Coxiella burnetii in kangaroos and kangaroo ticks in western Queensland. Aust J Exp Biol. 1960;38:17–28. doi: 10.1038/icb.1960.3. [DOI] [PubMed] [Google Scholar]
- 4.Derrick EH, Smith DJW. Studies in the epidemiology of Q fever. 2. The isolation of three strains of Rickettsia burnetii from the bandicoot Isoodon torosus. Aust J Exp Biol Med Sci. 1940;18:99–102. [Google Scholar]
- 5.Raoult D, Marrie T. Q fever. Clin Infect Dis. 1995;20:489–496. doi: 10.1093/clinids/20.3.489. [DOI] [PubMed] [Google Scholar]
- 6.Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12:518–553. doi: 10.1128/cmr.12.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marmion BP. A Guide to Q Fever and Q Fever Vaccination. Parkville, Victoria, Australia: CSL Biotherapies; 2009. [Google Scholar]
- 8.Botelho-Nevers E, Fournier PE, Richet H, Fenollar F, Lepidi H, Foucault C, Branchereau A, Piquet P, Maurin M, Raoult D. Coxiella burnetii infection of aortic aneurysms or vascular grafts: report of 30 new cases and evaluation of outcome. Eur J Clin Microbiol Infect Dis. 2007;26:635–640. doi: 10.1007/s10096-007-0357-6. [DOI] [PubMed] [Google Scholar]
- 9.Ellis ME, Smith CC, Moffat MAJ. Chronic or fatal Q fever infection; a review of 16 patients seen in north-east Scotland (1967–1980) Q J Med. 1983;205:54–66. [PubMed] [Google Scholar]
- 10.Fenollar F, Thuny F, Xeridat B, Lepidi H, Raoult D. Endocarditis after acute Q fever in patients with previously undiagnosed valvulopathies. Clin Infect Dis. 2006;42:818–821. doi: 10.1086/500402. [DOI] [PubMed] [Google Scholar]
- 11.Ayres JG, Flint N, Smith EG, Tunnicliffe WS, Fletcher TJ, Hammond K, Ward D, Marmion BP. Post-infection fatigue syndrome following Q fever. Q J Med. 1998;91:105–123. doi: 10.1093/qjmed/91.2.105. [DOI] [PubMed] [Google Scholar]
- 12.Dupuis G, Peter O, Peacock M, Burgdorfer W, Haller E. Immunoglobulin responses in acute Q fever. J Clin Microbiol. 1985;22:484–487. doi: 10.1128/jcm.22.4.484-487.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Worswick D, Marmion BP. Antibody responses in acute and chronic Q fever and in subjects vaccinated against Q fever. J Med Microbiol. 1985;19:281–296. doi: 10.1099/00222615-19-3-281. [DOI] [PubMed] [Google Scholar]
- 14.Massey PD, Irwin M, Durrheim DN. Enhanced Q fever risk exposure surveillance may permit better informed vaccination policy. Commun Dis Intell. 2009;33:41–45. [PubMed] [Google Scholar]
- 15.Population Health Division The Health of the People of New South Wales. Report of the Chief Health Officer. 2010. www.health.nsw.gov.au/publichealth/chorep/ Available at. Accessed February 28, 2010.
- 16.Hunter New England Population Health Health in Hunter New England HealtheResource. 2009. http://www1.hnehealth.nsw.gov.au/HNEPH/HHNE/com/comQfever.htm Available at. Accessed February 28, 2010.
- 17.Dupuis G, Petite J, Peter O, Vouilloz M. An important outbreak of human Q fever in a Swiss alpine valley. Int J Epidemiol. 1987;16:282–287. doi: 10.1093/ije/16.2.282. [DOI] [PubMed] [Google Scholar]
- 18.Tonge JI, Kennedy JM. An outbreak of Q fever in an abattoir near Brisbane. Med J Aust. 1963;50:340–343. doi: 10.5694/j.1326-5377.1963.tb23064.x. [DOI] [PubMed] [Google Scholar]
- 19.Massey P, Taylor K. Q fever cluster in a shearing team. N S W Public Health Bull. 2004;15:11–12. [Google Scholar]


