Abstract
Angiotensin-converting enzyme (ACE) inhibitor treatment was started in a 67-year-old woman with arterial hypertension. Two days later she complained of a hoarse, raspy voice and progressive abdominal pain. The laboratory investigation was within normal limits. However, CT scans of the abdomen revealed marked thickening of the proximal jejunum together with substantial fluid accumulation in the abdomen and pelvis. Due to the severity of the symptoms diagnostic laparatomy was considered as a surgical option. Several hours later the patient started to complain about a progressive inspiratory stridor, which resolved after treatment with epinephrine, antihistamines and corticosteroids. ACE inhibitor induced angioedema was suspected and ACE inhibitor treatment was stopped, after which the severe abdominal symptoms also resolved completely. ACE inhibitor induced angioedema is a rare and often unrecognised side effect of ACE inhibitor treatment that physicians need to be aware of in order to avoid unnecessary invasive procedures, including explorative laparatomy.
BACKGROUND
Angiotensin-converting enzyme (ACE) inhibitors are a common medication in arterial hypertension and congestive heart failure. The common side effects of this drug are well-known. However, less common side effects such as ACE inhibitor induced angioedema of the small intestine might be unrecognised due rare incidence. The patient described in this case report presented with an acute abdomen several days after ACE inhibitor therapy was started. Abdominal pain was progressing so rapidly that diagnostic laparatomy was considered as a surgical option. Fortunately, in this case, the patient also developed a swelling of the oropharynx that was successfully treated with epinephrine, antihistamines and corticoids. After prompt discontinuation of the ACE inhibitor, symptoms resolved completely within a couple of days. We believe that ACE inhibitor induced angioedema of the intestine is a rare but very important side effect of the drug that medical professionals need to be aware of during everyday practice.
CASE PRESENTATION
A 67-year-old woman was referred to our hospital for suspected coronary heart disease. Coronary angiography ruled out coronary heart disease but showed signs of hypertensive cardiomyopathy. The patient had been taking metoprolol to treat hypertension twice daily for the past 5 years. On admission ramipril 5 mg once a day was added. Two days after initiation of treatment the patient started complaining of a hoarse, raspy voice and progressive abdominal pain. On readmission to our emergency room, complete blood count and comprehensive metabolic tests were within normal range. To rule out a retroperitoneal haematoma after cardiac catheterisation, a CT scan of the abdomen was performed and revealed marked thickening of the proximal jejunum and ascites (fig 1A,B). Acute gastroenteritis was suspected and the patient was discharged. However, the next day the patient returned to the emergency room with worsening abdominal pain, rendering her almost unable to walk. Physical examination revealed a distended abdomen with dullness to percussion and diffuse tenderness on deep palpation. The vital signs were normal. Initial work-up included a complete blood count and comprehensive metabolic tests, all of which were within normal limits. Another CT scan of the abdomen and pelvis with both oral and intravenous contrast was performed. It demonstrated marked thickening of the proximal jejunum (fig 2A–C) along with massive fluid accumulation in the abdomen and pelvis. Due to the severity of the clinical symptoms the surgical service was consulted to discuss a diagnostic laparatomy. Since complete blood count and metabolic tests including lactate continued to be in normal range this option was dismissed and the patient was transferred to the intensive care unit for further monitoring. Approximately 6 h afterwards she started to complain about progressive hoarseness of her voice and difficulty breathing with a progressive inspiratory stridor. On physical examination she revealed a very large swelling in the oropharynx. ACE inhibitor angioedema was suspected and the patient was treated with epinephrine, antihistamines and corticosteroids. Her difficulty breathing resolved within 2 h. The ACE inhibitor was stopped and amlodipine was started.
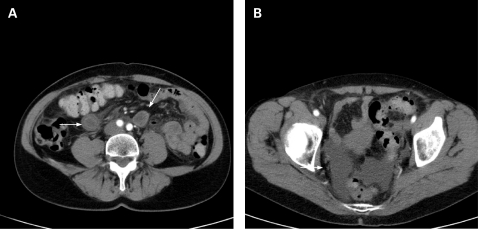
Figure 1.
CT scan of the abdomen revealing marked bowel wall enhancement with regular thickened mucosal folds (A) and ascites (B).
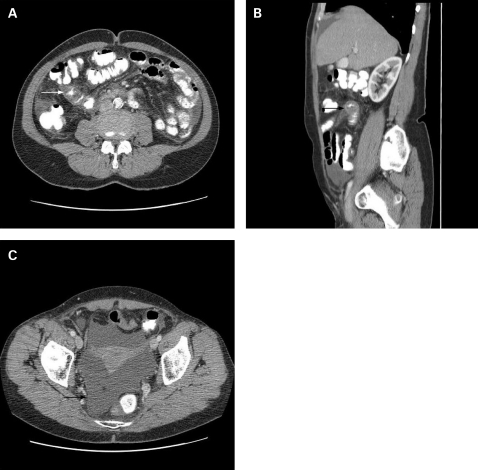
Figure 2.
CT scan of the abdomen revealing thickening of the small intestine (A, B) and progressive ascites (C).
OUTCOME AND FOLLOW-UP
Further diagnostic work-up revealed that complement and C1-esterase inhibitor levels were within normal ranges, while gastroscopy and coloscopy as well as analysis of an ascites puncture revealed no abnormal findings. The patient’s condition progressively improved. Abdomen ultrasound follow-up investigations showed marked improvement of small bowl wall thickening and decreasing ascites. The patient was sent home on amlodipine and metoprolol. At follow-up 3 weeks later her symptoms had completely resolved.
DISCUSSION
ACE inhibitors have been available since 1980. Dry cough, excessive hypotension, hyperkalaemia and angioedema have been described as adverse reactions.1,2 Angioedema has been associated with idiopathic, hereditary and acquired C1-esterase inhibitor deficiency, drugs and foods.3,4 It may be limited to the gastrointestinal tract, but cutaneous and respiratory findings are frequently concomitant.5 Angioedema occurs in 0.1–0.2% of patients after treatment initiation with ACE inhibitors.6,7 There is no dose–response relationship and it can be induced by different kinds of ACE inhibitors.7–11 A female predominance has been reported, which has been speculated to reflect an interaction with estradiol.12,13 Interestingly, results of the recently published ONTARGET study show that patients with combination therapy with ACE inhibitors and angiotensin-receptor blockers are more prone to diarrhoea, demonstrating that inhibition of the renin-angiotensin system is related to increasing adverse intestinal events.14 The angiotensin-converting enzyme releases the carboxyl terminal dipeptide phenylalanine-arginine and inactivates the monopeptide bradykinin, which is a potent activator of the L-arginine nitric oxide system, causing vasodilatation and increased vascular permeability. ACE inhibitors increase the concentration of bradykinin. A temporal relationship between the initiation of ACE inhibitor treatment and angioedema is often essential in establishing the diagnosis, because in most cases symptoms start within the first week of treatment. However, some cases have been reported after several months of treatment with ACE inhibitors.11,15 The levels of C1 and C4 are not altered and C1-esterase inhibitor functional activity is normal.
LEARNING POINTS
The diagnosis of ACE inhibitor induced intestinal angioedema is elusive, and frequently invasive procedures, including explorative laparatomy, are pursued.
Invasive procedures might be avoided if the treating physician recognises the association between angioedema and the ACE inhibitor, and withdraws the ACE inhibitor.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Gravas H, Gravas I. Angiotensin converting enzyme inhibitors: properties and side effects. Hypertension 1988; 11(Suppl II): 37. [DOI] [PubMed] [Google Scholar]
- 2.Weber MA. Safety issues during antihypertensive treatment with angiotensin converting enzyme inhibitors. Am J Med 1988; 84(Suppl 4 A): 16. [DOI] [PubMed] [Google Scholar]
- 3.Weinstock LB, Kothari T, Sharma RN, et al. Recurrent abdominal pain as the sole manifestation of hereditary angioedema in multiple family members. Gastroenterology 1987; 93: 1116–18 [DOI] [PubMed] [Google Scholar]
- 4.Poolger M, Kuhlman JE, Hanssen FC III, et al. Computed tomography of angioedema of the small bowel due to reaction to radiographic contrast medium. J Comput Assist Tomogr 1988; 12: 1044–6 [DOI] [PubMed] [Google Scholar]
- 5.Schmidt TD, McGrath KM. Angiotensin-converting enzyme inhibitor angioedema of the intestine: a case report and review of the literature. Am J Med Sci 2002; 324: 106–8 [DOI] [PubMed] [Google Scholar]
- 6.Israili ZH, Hall WD. Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy: a review of the literature and pathophysiology. Ann Intern Med 1992; 117: 234–42 [DOI] [PubMed] [Google Scholar]
- 7.Slater EE, Merrill DD, Guess HA, et al. Clinical profile of angioedema associated with angiotensin converting-enzyme inhibition. JAMA 1988; 260: 967–70 [PubMed] [Google Scholar]
- 8.Abdelmalek MF, Douglas DD. Lisinopril-induced isolated visceral angioedema: review of ACE-inhibitor-induced small bowel angioedema. Dig Dis Sci 1997; 42: 847–50 [DOI] [PubMed] [Google Scholar]
- 9.Jacobs RL, Hoberman LJ, Goldstein HM. Angioedema of the small bowel caused by an angiotensin-converting enzyme inhibitor. Am J Gastroenterol 1994; 89:127–8 [PubMed] [Google Scholar]
- 10.Farraye FA, Peppercorn MA, Steer ML, et al. Acute small bowel mucosal edema following enalopril use. JAMA 1988; 259: 3131. [PubMed] [Google Scholar]
- 11.Matsumura M, Haruki K, Kajinami K, et al. Angioedema likely related to angiotensin converting enzyme inhibitors. Intern Med 1993; 32: 424–6 [DOI] [PubMed] [Google Scholar]
- 12.Oudit G, Girgrah N, Allard J. ACE-inhibitor-induced angioedema of the intestine: case report, incidence, pathophysiology, diagnosis and management. Can J Gastroenterol 2001; 12: 827–32 [DOI] [PubMed] [Google Scholar]
- 13.Chiu AG, Newkirk KA, Davidson BJ, et al. Angiotensin-converting enzyme inhibitor-induced angioedema: a multicenter review and an algorithm for airway management. Ann Otol Rhinol Laryngol 2001; 110: 834–40 [DOI] [PubMed] [Google Scholar]
- 14.ONTARGET Investigators Telmisartan, ramipril, or both in patients at increased risk for vascular events. N Engl J Med 2008; 358: 1547–59 [DOI] [PubMed] [Google Scholar]
- 15.Chin HL, Buchan DA. Severe angioedema after long term use of an angiotensin-converting enzyme inhibitor. Ann Intern Med 1990; 112: 312. [DOI] [PubMed] [Google Scholar]