Abstract
Postoperative seroma is a common postoperative complication, particularly following surgery on massive weight loss patients. Within this patient population, seromas are often chronic, requiring multiple invasive procedures to adequately control. Here, the authors describe a unique dermal flap approach for the long-term treatment of postoperative seroma.
Background
Seromas are subcutaneous collections of serous fluid that arise at sites of previous surgeries and are common postoperative complications. The incidence of postoperative seroma varies widely in the literature depending on the site examined, and has been reported to be as high as 51% following breast and axillary surgery.1
Various theories have been proposed to account for the formation of seroma, from the disruption of lymphatic and vascular channels to an acute inflammatory process, although the exact mechanism is not completely understood. While most seromas usually resolve independently within a few weeks, chronic seromas can impair wound healing, lengthen recovery time, cause patient discomfort and may ultimately require subsequent re-operations. Here, we describe a unique surgical technique for addressing the challenge of chronic seroma.
Case presentation
A 57-year-old Caucasian female who had undergone laparoscopic Roux-en-Y gastric bypass for morbid obesity with subsequent bilateral medial thigh lifts 2 years later, had been referred for chronic seromas at both thigh lift incision sites. Previous non-operative approaches, including aspiration with drainage and injection of sclerosing agents had failed to control the seromas. She then underwent surgery 8 months after the original thigh lifts, with obliteration of bilateral seroma cavities. The linings of both seroma cavities were stripped and quilting sutures placed to minimize the dead space. Unfortunately, the seromas recurred and she was re-operated on 2 years later.
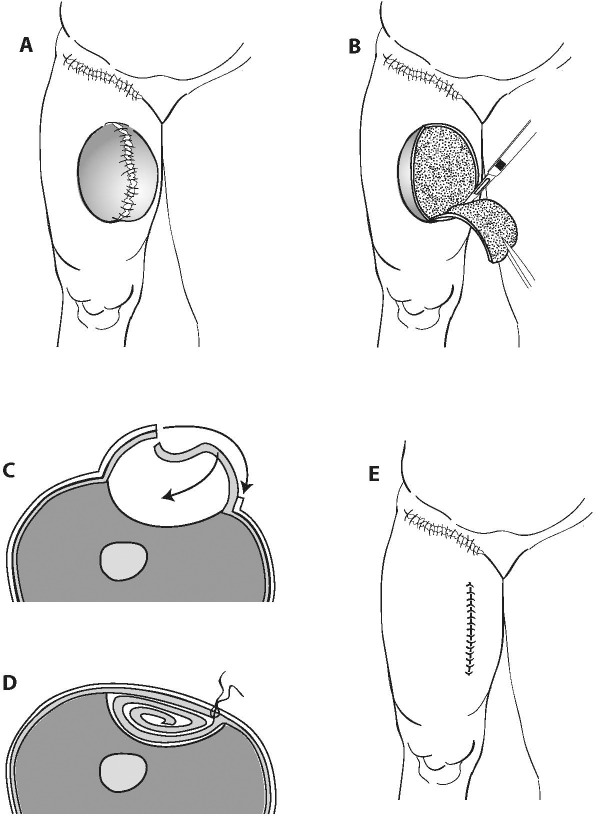
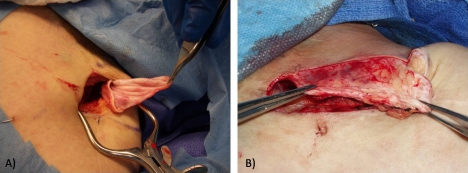
The seromas were excised bilaterally (figure 1A, B), however, this time dermal flaps were created measuring >30 cm on the left side and 20 cm on the right side (figures 1C and 2A). The flaps were de-epithelialised, tucked into the site of the seroma cavity, and sutured with Vicryl sutures (figures 1D, E and 2B). Complete haemostasis was obtained, and the incisions were closed using simple nylon sutures. The patient tolerated the procedure well. The rationale behind the surgery was that if the seroma recurred, the dermal flap would absorb the seroma fluid via dermal lymphatics. This technique has long been used in the treatment of severe lymphedema secondary to filiariasis and was first described by Thompson nearly 40 years ago.2
Figure 1.
Diagram of the procedure. The seroma was located at the incision site of a medial thigh lift (A). The seroma cavity was excised (B), and a de-epithelialised dermal flap created to obliterate dead space and increase lymphatic flow (C). The flap was tucked and sutured into the defect (D, E).
Figure 2.
Intraoperative photographs of the excised seroma cavity (A) and de-epithelialised dermal flap used to fill the defect (B).
A few months later, the patient re-presented for smaller re-accumulations of fluid, measuring ∼7 cm bilaterally. The seroma cavities, which were at the lower end of the thigh incisions, were excised in toto. Again, dermal flaps of tissue were created to both obliterate the defects as well as provide additional lymphatic flow. The flaps were de-epithelialised, placed into the wall of the seroma cavities, and secured with Vicryl sutures. The incisions were then closed in multiple layers without a drain, with pressure dressing applied.
Outcome and follow-up
Following this procedure, the patient's seromas have since been well-controlled at 24 months follow-up.
Discussion
Seromas have been most commonly studied in the literature on breast and axillary surgery, although the growing number of body contouring procedures following massive weight loss has shed light on the problem among this patient population. The incidence of seroma following body contouring for massive weight loss has been reported as high as 16.5%,3 and in our experience, seromas in this patient population tend to be chronic, requiring multiple procedures to adequately control. Shermak et al4 conducted a retrospective review of 222 patients who underwent body contouring surgery following massive weight loss and concluded that among patients with a body mass index of 30 or more, the greatest risk factor for seroma formation was the weight of excised skin, increasing risk by 9% for each additional pound, and that diabetes was the only significantly associated co-morbid medical condition.
The general treatment protocols for seromas stem from the literature on pleural effusions and include serial aspiration with drainage, injection of sclerosants and surgery.4 The most common sclerosants used to treat seromas are doxycycline and bleomycin,5 although case reports have described the use of a variety of antibiotics,6 alcohol and talc.7 Should the seroma recur after sclerotherapy, the mainstay of surgical treatment has been excision of the seroma cavity and minimizing the dead space through quilting sutures, which has also been found effective in reducing the incidence of seromas when performed prophylactically.4
Learning points.
Given the high rate of persistent seromas in massive weight loss patients, it may be useful to perform the dermal flap as a complementary technique when surgical excision is indicated.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Anand R, Skinner R, Dennison G, et al. A prospective randomised trial of two treatments for wound seroma after breast surgery. Eur J Surg Oncol 2002;28:620–2 [DOI] [PubMed] [Google Scholar]
- 2.Thompson N. Buried dermal flap operation for chronic lymphedema of the extremities. Ten-year survey of results in 79 cases. Plast Reconstr Surg 1970;45:541–8 [DOI] [PubMed] [Google Scholar]
- 3.Nemerofsky RB, Oliak DA, Capella JF. Body lift: an account of 200 consecutive cases in the massive weight loss patient. Plast Reconstr Surg 2006;117:414–30 [DOI] [PubMed] [Google Scholar]
- 4.Shermak MA, Rotellini-Coltvet LA, Chang D. Seroma development following body contouring surgery for massive weight loss: patient risk factors and treatment strategies. Plast Reconstr Surg 2008;122:280–8 [DOI] [PubMed] [Google Scholar]
- 5.Throckmorton AD, Askegard-Giesmann J, Hoskin TL, et al. Sclerotherapy for the treatment of postmastectomy seroma. Am J Surg 2008;196:541–4 [DOI] [PubMed] [Google Scholar]
- 6.Ali-Khan AS, Orlando A, Kenealy J. Erythromycin sclerotherapy in the management of seroma. J Plast Reconstr Aesthet Surg 2009;62:e55–8 [DOI] [PubMed] [Google Scholar]
- 7.Saeb-Parsy K, Athanassoglou V, Benson JR. Talc seromadesis: a novel technique for the treatment of chronic seromas following breast surgery. Breast J 2006;12:502–4 [DOI] [PubMed] [Google Scholar]