Abstract
Lacrimal sac tumours are rare entities. Patients often present with epiphora, recurrent dacryocystitis, and/or a lacrimal sac mass. Neoplasms of the lacrimal system may conveniently be grouped into epithelial and non-epithelial types: papillomas are the most common benign epithelial tumours, while oncocytic adenocarcinomas are extremely rare. Here we report a case of primary oncocytic adenocarcinoma of the lacrimal sac in a 56-year-old man.
CASE PRESENTATION
A 56-year-old man presented with a 4 year history of right sided inner canthal mass which was gradually enlarging, with incidental lacrimation. There was no history of diplopia, pain, redness, ulceration, or blurred vision. On ocular examination, a large swelling with an irregular outer surface measuring 1.6 cm × 2.0 cm was present in the right eye, which was attached to the medial canthus and the root of the nose. The mass was firm and non-tender. His visual acuity, intraocular pressure, and fundi examination were all within normal limits. Lacrimal syringing and probing revealed obstruction of the nasolacrimal duct. He had no other contributory non-ocular findings.
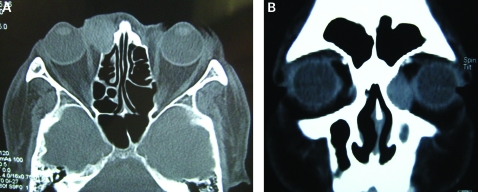
Computed tomography (CT) scanning revealed a soft tissue abnormality associated with the right sided lacrimal sac area (fig 1). There was bone destruction and invasion of the adjacent paranasal sinuses. The tumour invaded both the right side maxillary sinus and the left side sphenoid sinus. The patient underwent surgery for tumour resection. An en bloc resection of the medial maxilla with the nasolacrimal apparatus was performed. Intraoperatively, the mass was firm and fixed to the underlying structures. An incisional biopsy was taken from the tumour core.
Figure 1.
Computed tomography scan of the orbits: axial (A) and coronal (B) views. Note the large mass in the area of the lacrimal sac, extending into the right inferomedial orbit.
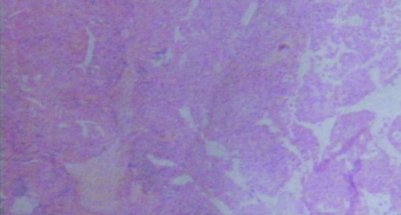
Biopsy pointed to a diagnosis of oncocytic adenocarcinoma. Histologically, the tumour was composed of cords, trabeculae, and nests of cells with abortive glandular structures. The tumour cells were polyhedral with central hyperchromatic nuclei, prominent nucleoli, and abundant granular eosinophilic cytoplasm. Mitotic figures were rare. Immunohistochemically, the tumour cells were positive for CK5/6, CK18, P63, partly positive for ki-67, and negative for P53, SMA (fig 2).
Figure 2.
Histopathologic evaluation of the excised tumour. Low power view of the tumour arising from the lacrimal sac (haematoxylin and eosin; original magnification ×5).
OUTCOME AND FOLLOW-UP
Based on the above mentioned features, a diagnosis of primary oncocytic adenocarcinoma of lacrimal sac was confirmed. Following surgery, the patient received a course of postoperative radiotherapy and general management.
The patient was followed up for 2 months postoperatively, by which time the wound had healed satisfactorily.
DISCUSSION
Primary tumours of the lacrimal sac are uncommon.1 The first description of lacrimal sac tumours, by Janin, appeared in 1772.2 They are characterised by a lacrimal sac mass, especially those presenting above the medial canthal tendon. Other common features include expressible blood from the punctum, lack of pain, and a history of chronic epiphora or intermittent dacryocystitis. Neoplasms of the lacrimal system are most commonly classified as either epithelial or non-epithelial. The epithelial type has been found in 75% of cases, with the remainder being non-epithelial.3 Many neoplasms are discovered inadvertently at the time of dacryocystorhinostomy for presumed dacryostenosis.
Oncocytoma can be found in some glands, such as the parotid and thyroid glands, and it is particularly prevalent in the elderly.4 Oncocytic adenocarcinoma, also known as malignant oncocytoma, is a rare oncocytic tumour that exhibits malignant histopathologic features. The tumour cells are characterised as large body, cytoplasm-rich, and fine granular eosinophilic cells, with electron microscopy revealing many abnormal mitochondria. Papillomas are the most common benign epithelial tumours, while oncocytic adenocarcinoma of the lacrimal sac are rare. Fewer than 10 cases of oncocytic adenocarcinoma of the lacrimal sac have been reported in the literature,4–9 and most of these recurred from an oncocytoma. Here we presented the evaluation and pathology of a primary oncocytic adenocarcinoma arising from the lacrimal sac.
Although rare, lacrimal sac tumours are potentially life threatening, so early diagnosis and treatment is particularly important. Ophthalmologists should be aware of the symptoms and signs: a painless mass above the medial canthal tendon, a prolonged history of intermittent epiphora, chronic dacryocystitis, and expressible blood from the punctum. Tissue biopsy is necessary to confirm the diagnosis,7 which can also be assisted by a dacryocystogram (DCG) and a CT scan. A DCG may demonstrate a mottled density or filling defect in the lacrimal sac. Orbital and sinus CT is imperative where a tumour is suspected, and will provide evidence of expansion or erosion of the lacrimal sac fossa, or invasion into neighbouring structures. Complete surgical resection is recommended while a confirmed diagnosis is made.
This case was presented to alert ophthalmologists to the occurrence of primary oncocytic adenocarcinoma of the lacrimal sac. Although rarely seen, these tumours should be taken into consideration in related cases.
LEARNING POINTS
Tissue biopsy and CT scan are necessary to confirm the diagnosis of lacrimal sac tumours.
Complete surgical resection is recommended while the diagnosis is confirmed.
Although rarely seen, primary oncocytic adenocarcinoma of the lacrimal sac should be taken into consideration in related cases.
Acknowledgments
The case report is presented in compliance with Beijing Tongren Hospital Ethics Committee guidelines
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication
REFERENCES
- 1.Hornblass A, Jakobiec FA, Bosniak S, et al. The diagnosis and management of epithelial tumours of the lacrimal sac. Ophthalmology 1980; 87: 476–90 [DOI] [PubMed] [Google Scholar]
- 2.Janin de Combe-Blance J. Cited in: The ocular adnexa, II: lacrimal, orbital and para-orbital diseases. : Duke-Elder S, ed. System of ophthalmology, vol 13 St Louis: CV Mosby, 1974: 733 [Google Scholar]
- 3.Ni C, D’Amico DJ, Fan CQ, et al. Tumors of the lacrimal sac: a clinicopathological analysis of 82 cases. Int Ophthalmol Clinics 1982; 22: 121–40 [DOI] [PubMed] [Google Scholar]
- 4.Tomic S, Warner T, Brandenburg J. Malignant oncocytoma of the lacrimal sac: ultrastructure and immunohistochemistry. Ear Nose Throat J 1995; 74: 717–20 [PubMed] [Google Scholar]
- 5.Peretz WL, Ettinghausen SE, Gray GF. Oncocytic adenocarcinoma of the lacrimal sac. Arch Ophthalmol 1978; 96: 303–4 [DOI] [PubMed] [Google Scholar]
- 6.Perlman J, Specht C, McLean I, et al. Oncocytic adenocarcinoma of the lacrimal sac; report of a case with paranasal sinus and orbital extension. Ophthalmic Surg 1995; 26: 377–9 [PubMed] [Google Scholar]
- 7.Brannan PA, Kersten RC, Schneider S, et al. A case of primary adenocarcinoma of the lacrimal sac. Orbit 2005; 24: 291–3 [DOI] [PubMed] [Google Scholar]
- 8.Yuen HK, Cheuk W, Cheng AC, et al. Malignant oncocytoma of the lacrimal sac as an unusual cause of epiphora. Ophathal Plast Reconstr Surg 2007; 23: 70–2 [DOI] [PubMed] [Google Scholar]
- 9.Stefanyszyn M, Hidayat A, Pe’er J, et al. Lacrimal sac tumors. Opthal Plast Reconstr Surg 1994; 10: 169–84 [DOI] [PubMed] [Google Scholar]