Abstract
Objective
To describe and test the feasibility of Asthma Self-Management for Adolescents with Undiagnosed Asthma (ASMA-Undx), an eight-week school-based intervention for urban adolescents comprised of three group and five individual coaching sessions, and academic detailing for their primary care providers (PCPs).
Methods
Thirty high school students (mean age 15.9; 92% female; 72% Latino/a) who reported symptoms of persistent asthma, but no diagnosis were randomized to ASMA-Undx or a no-treatment control group. Interviews were conducted pre- and post-intervention.
Results
All intervention students participated in the three group sessions; 64% received all five individual coaching sessions. Academic detailing telephone calls made by a pediatric pulmonologist reached 83% of the students’ PCPs. Relative to controls, a significantly greater proportion of ASMA-Undx students were diagnosed (79% versus 6%, respectively), and prescribed asthma medication (57% versus 6%, respectively). Barriers to diagnosis and treatment included students’ and parents’ lack of knowledge about asthma.
Conclusion
ASMA-Undx is a feasible and promising intervention to assist urban adolescents with undiagnosed asthma obtain a diagnosis and treatment.
Practice Implications
ASMA-Undx has the potential to reach many adolescents because it is school-based. It can serve as a model for interventions targeting other pediatric illnesses.
1. Introduction
Up to 50% of 7- to 18-year olds with asthma-like symptoms have not been diagnosed with asthma [1–7]. Undiagnosed asthma results in significant activity limitation [3, 6, 8], and when left untreated, the risk of adverse events, including exacerbations and death, increases [9]. Accurate recognition of asthma-like symptoms is a critical first step in enabling adolescents to be diagnosed and treated. School-based case detection efforts offer the advantage of identifying undiagnosed youth [11], and school-based interventions have been found to result in improved asthma control and quality of life in students [10, 12–18]. Two efficacious interventions targeting adolescents have included students with and without a diagnosis [16, 19]. However, because neither considered intervention effects by diagnosis, the efficacy of these interventions for youth with undiagnosed asthma remains unknown. Referral to physicians for elementary students with asthma symptoms was found to improve the diagnosis rate, but failed to change treatment or health status, suggesting that referral alone is insufficient [20].
To address this need, we undertook a program to identify and intervene with adolescents who report asthma symptoms, but no diagnosis. We describe Asthma Self-Management for Adolescents with Undiagnosed Asthma (ASMA-Undx), a comprehensive intervention to connect high school students to medical care to improve control of their asthma-like symptoms. To estimate its feasibility and potential utility, we conducted a pilot study hypothesizing that (1) it will be feasible to deliver ASMA-Undx, and (2) relative to controls, a greater proportion of intervention students will seek a medical evaluation, receive a diagnosis, and be prescribed asthma medication.
2. The Intervention
ASMA-Undx, an adaptation of our successful intervention for adolescents with diagnosed asthma [10, 17], expands the case-worker model [21, 22] by combining case detection, intervention for students, and academic detailing for students’ PCPs.
2.1. Case Detection
Students complete a brief case detection survey in class which combines two validated surveys [2, 23] with questions written by the investigators. Students indicate: (a) whether they were ever diagnosed with asthma, reactive airway disease, or wheezy bronchitis; and the frequency of (b) seven markers of uncontrolled asthma [23] and (c) asthma symptoms in the past 12 months [2]. Students who answered no to the diagnosis questions, and who endorsed at least three markers of uncontrolled asthma were categorized as having probable undiagnosed asthma [23]. Frequency of asthma symptoms permits classification into one of the four NHLBI categories of asthma severity (i.e., intermittent to severe persistent) [2]. To ensure we reached absent students who were potentially positive for undiagnosed asthma, we re-visited classes twice, and teachers distributed surveys on other days.
2.2. Student Intervention
Grounded in social cognitive theory [24], the student intervention is an intensive eight-week psycho-educational program comprised of three components: group workshops; individual coaching sessions; and instruction to see a PCP for a clinical evaluation. Each component teaches students about the importance and process of obtaining a diagnosis and treatment, and how to control symptoms. Table 1 lists session topics. Asthma self-regulation develops in four sequential phases (see Table 2) [25]; phase specific messages enhance movement through these phases [17, 26] and are incorporated into the intervention.
Table 1.
Content of ASMA-Undx Group Workshops and Individual Sessions
| Session | Topics |
|---|---|
| Group Workshop #1 |
|
| Group Workshop #2 |
|
| Group Workshop #3 |
|
| Individual sessions |
|
Table 2.
Patient and Family Characteristics by Phase of Asthma Self-Regulation [42]
| Phase 1 | Asthma symptom avoidance. The patient or family may perceive a periodic cough or wheeze, but they do not attribute these symptoms to an inherent physiological vulnerability with serious health-threatening outcomes if untreated. They try to avoid asthma symptoms nonmedically through activity restrictions and emotional calming |
| Phase 2 | Asthma acceptance. The patient or family accepts asthma as a serious health-threatening disease, but they respond to asthma only reactively (nonpreventively), primarily using bronchodilators. Their main pharmacological efforts are toward a rescue from acute episodes, and they are resigned to the recurrence of exacerbations. |
| Phase 3 | Asthma compliance. The patient or family seeks to prevent and control asthma symptoms by following the physician’s treatment recommendations and is therefore less likely to need emergency treatment. However, they lack the confidence to self-regulate asthma because they are unskilled at preventively altering medications. |
| Phase 4 | Asthma self-regulation. The patient or family develops an adoptable medical plan in consultation with the physician. They monitor lung functioning with peak flow meters or symptom recognition and can identify early warning signs of inflammation. They adjust their medical regimens on the basis of self-monitored signs, symptoms, or contact with triggers and are confident of their efficacy in implementing the plan and in contacting their doctor when modifications are needed. |
© Copyright 1999 Health Education and Behavior – reproduced with permission
Health educators deliver three group workshops, scheduled two to three weeks apart to allow time to practice skills. In individual coaching sessions held on off weeks, students set goals, identify barriers to diagnosis and treatment, and generate solutions to these barriers. Sessions focus on connecting students to appropriate medical care, and adhering to treatment. Students and the health educator review weekly homework assignments, including asthma checklists, where students record their symptoms, activity limitations and, if appropriate, medication use. Health educators also follow-up by telephone. All aspects of the intervention are manualized.
Students are instructed to see a PCP for a clinical evaluation and treatment. Students are coached on how to present information to PCPs to facilitate an accurate diagnosis. Health educators offer to accompany students to these visits to provide support and help students communicate adequately with their PCP. Referrals are made for students without a PCP or insurance.
2.3. Intervention with PCPs
Successful management of asthma requires collaboration with a PCP who accurately diagnoses and effectively treats asthma symptoms. To support PCPs, ASMA-Undx uses academic detailing, a technique whereby experts make in-person or telephone presentations to PCPs about a recommended change in therapy [27]. PCPs are mailed a packet including: (1) a letter explaining the study and informing them that we identified a patient who reports symptoms suggesting moderate or severe persistent asthma, but has not been diagnosed; (2) a blank asthma checklist; and (3) a written treatment plan (WTP) to complete for the student. A pediatric pulmonologist calls each PCP to answer questions about NHLBI criteria for diagnosing and treating asthma, and asks the PCP to review the student’s checklist, and in combination with their own history and examination, consider making a diagnosis of asthma, and if appropriate, prescribe medication and complete a WTP for the student.
3. The Pilot Study
3.1. Participants
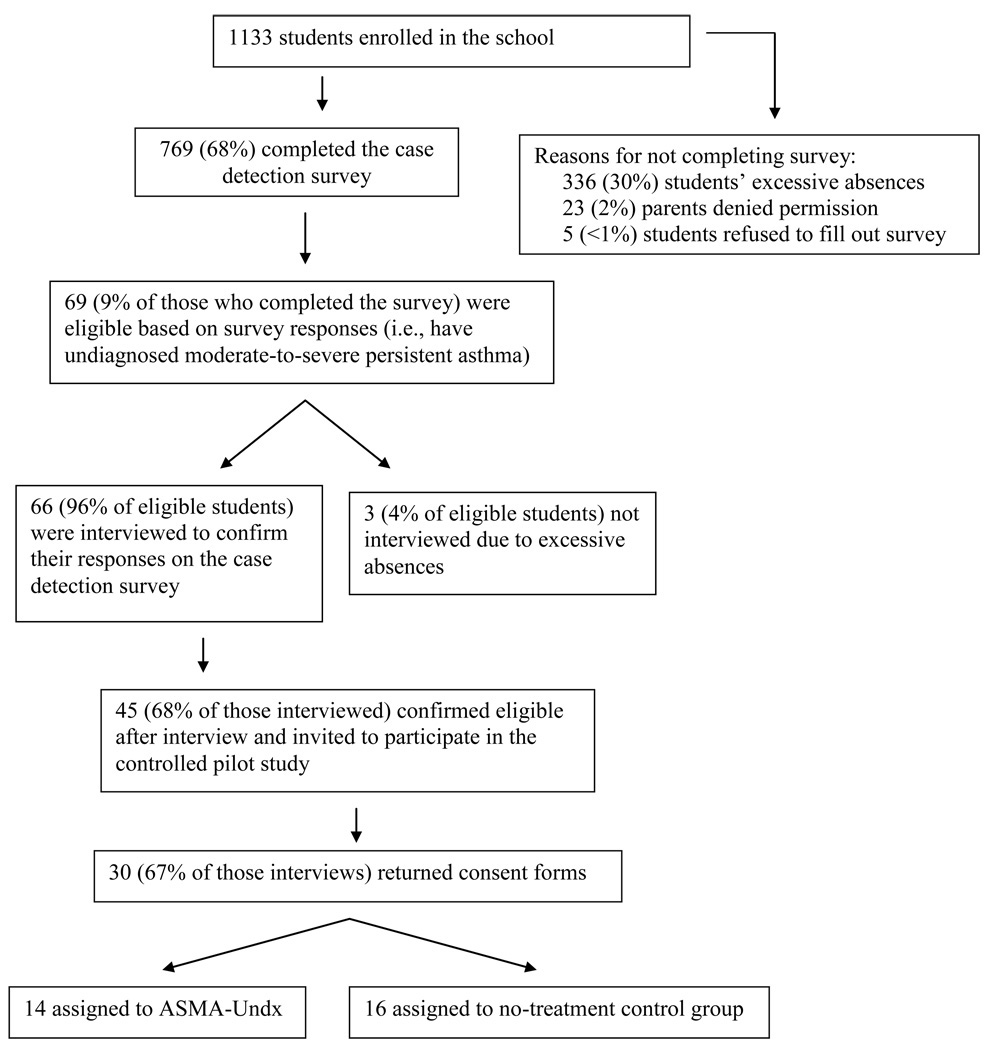
Thirty 9th through 11th graders, who reported symptoms consistent with probable undiagnosed moderate to severe persistent asthma [2, 9, 23], were recruited from one NYC public high school with a school-based health center (SBHC; Figure 1 details enrollment); 14 were randomized to ASMA-Undx and 16 to a no-treatment control group. There were no differences by group assignment for gender, ethnicity, or age. Table 3 lists demographic details.
Figure 1.
Flowchart of participants through the study.
Table 3.
Demographic Characteristics of Participants by Treatment Group
| ASMA-Undx (n=14) | Controls (n=16) | Total (N=30) | |
|---|---|---|---|
| Age, mean (SD) | 15.9 (1.06) | 15.7 (0.92) | 15.9 (0.98) |
| Female, % (n) | 100 (14) | 87.5 (14) | 93.3 (24) |
| Race | |||
| Latino/a, % (n) | 71.4 (10) | 56.4 (9) | 63.3 (19) |
| African American, % (n) | 14.3 (2) | 18.8 (3) | 16.7 (5) |
| Bi-racial, % (n) | 14.3 (2) | 25.0 (4) | 20.0 (6) |
3.2. Evaluation
Students were interviewed immediately following the intervention to determine whether they consulted a PCP for their breathing problems, received a diagnosis, and were prescribed asthma medication during the intervention. To identify barriers to diagnosis and treatment, we queried students regarding why they had not previously sought medical attention. Process evaluation data, including treatment fidelity, were collected.
3.3. Results
3.3.1. Process Evaluation
With make-up sessions, all students received the three group sessions; 64% (9/14) received all five individual coaching sessions and 29% (4/14) received 4 individual sessions. Twelve intervention students (86%; 12/14) had PCPs; only one used the SBHC for primary care. The two students without PCPs were referred to the SBHC. All PCPs were mailed intervention materials; academic detailing phone calls reached 83% (10/12) of PCPs. The pediatric pulmonologist indicated that academic detailing was well received by PCPs. Providers expressed appreciation for helping their patients come for care and adhere to their treatment regimes. Sample statements included, “If it gets the student back in the office for a check-up, that is a good thing,” and, “I’m glad someone will help the student because it is hard to get them to take medicine everyday.”
Treatment fidelity was high. On average, 98% of the content was taught in the three groups (range 96% to 99%). Students were engaged in the group and individual coaching sessions as evidenced by participation in discussions and asking appropriate questions.
3.3.2. Intervention Effects
Immediately post-intervention, relative to controls, a significantly greater proportion of intervention students reported being diagnosed (X2 (df=1)=16.27, P<.001) and prescribed asthma medication (X2 (df=1)=9.21, P<.01). The majority of intervention students obtained a clinical evaluation (86%; 12/14), were diagnosed with asthma (79%; 11/14), and prescribed medication (57%; 8/14). Only one control student had a clinical evaluation; she was diagnosed and obtained medication.
3.3.3. Diagnosis and Treatment Barriers
One common theme accounted for students not seeking treatment prior to the study: they did not realize their symptoms were serious, and left untreated might have significant health consequences. Students had not reported breathing problems during previous medical visits, an observation corroborated by PCPs. The SBHC nurse practitioner indicated that treatment was impeded because parents often failed to recognize their children’s symptoms as asthma. Few students (2/28; 7%) reported lack of insurance or cost influencing care-seeking behavior.
4. Discussion and Conclusions
ASMA-Undx is a novel school-based intervention with demonstrated feasibility and apparent treatment effects in adolescents with undiagnosed moderate to severe persistent asthma. Almost all treatment group adolescents sought medical evaluations for their symptoms, while only one control student did so. PCPs expressed openness to the academic detailing, which coupled with the adolescents’ new skill in presenting symptoms accurately, led to improved diagnosis and appropriate treatment for a group at high risk for asthma morbidity.
This study also informs on barriers to asthma care faced by urban African American and Latino/a adolescents. Students reported that they did not realize persistent symptoms were indicative of a serious health risk, and did not communicate them to their PCPs or parents. Once diagnosed, parents’ lack of awareness of their children’s symptoms sometimes impeded treatment.
Most study participants were female, which may be due to the fact that asthma rates are higher among females during adolescence and adulthood [28–30]. Research suggests that hormonal changes associated with puberty may account for this change [31]. Consequently, female adolescents may be experiencing symptoms for the first time, and have yet to receive a diagnosis.
Conclusions regarding the long-term clinical benefits and cost-effectiveness of ASMA-Undx are limited because this was a pilot study. A large-scale, longitudinal randomized control trial is currently addressing whether intervention students’ adhere to treatment and experience reductions in asthma morbidity, and whether students without intervention obtain a diagnosis over one year. If the intervention is efficacious, the cost-effectiveness of ASMA-Undx will be explored. We enhanced ASMA-Undx for the large-scale trial by adding a parent intervention and incorporating motivational interviewing techniques.
4.1. Practice Implications
Public health campaigns targeting asthma must incorporate well-designed, evidence-based interventions that identify cases of undiagnosed asthma and expend adequate efforts to: link youth to medical care; educate youth and their parents about the disease and the need to communicate symptoms to PCPs; and help youth overcome personal barriers to obtaining treatment. Preliminary evidence suggests that ASMA-Undx can accomplish these goals. ASMA-Undx has considerable practice relevance given the acute need for effective interventions for adolescents in low-income communities and the promise of school-based interventions. It can also serve as an intervention model for other chronic diseases.
Acknowledgement
We thank Rachel Klein, Ph.D. for her insightful comments and editorial assistance.
Funding Source: This study was supported by NHLBI (1R01HL089493; PI = Bruzzese).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jean-Marie Bruzzese, NYU School of Medicine
Sharon Kingston, Dickinson College
Beverley J. Sheares, Columbia University College of Physicians and Surgeons
Amarilis Cespedes, NYU School of Medicine
Hossein Sadeghi, Columbia University College of Physicians and Surgeons
David Evans, Columbia University College of Physicians and Surgeons
References
- 1.Lowe GL, Burr M. Undiagnosed and untreated wheezing in a cohort of adolescents with a family history of allergic disease. British Journal of General Practice. 2001;51(469):664–665. [PMC free article] [PubMed] [Google Scholar]
- 2.Clark NM, et al. Issues in identifying asthma and estimating prevalence in an urban school population. Journal of Clinical Epidemiology. 2002;55(9):870–881. doi: 10.1016/s0895-4356(02)00451-1. [DOI] [PubMed] [Google Scholar]
- 3.Yeatts K, et al. Health consequences for children with undiagnosed asthma-like symptoms. Archives of Pediatrics & Adolescent Medicine. 2003;157(6):540–544. doi: 10.1001/archpedi.157.6.540. [DOI] [PubMed] [Google Scholar]
- 4.Yeatts K, et al. Who gets diagnosed with asthma? Frequent wheeze among adolescents with and without a diagnosis of asthma. Pediatrics. 2003;111(5 Pt 1):1046–1054. doi: 10.1542/peds.111.5.1046. [DOI] [PubMed] [Google Scholar]
- 5.Lewis TC, et al. Identification of gaps in the diagnosis and treatment of childhood asthma using a community-based participatory research approach. Journal of Urban Health. 2004;81(3):472–488. doi: 10.1093/jurban/jth131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carter ER, Debley JS, Redding GJ. Changes in asthma prevalence and impact on health and function in Seattle middle-school children: 1995 vs 2003. Annals of Allergy, Asthma & Immunology. 2005;94(6):634–639. doi: 10.1016/S1081-1206(10)61320-8. [DOI] [PubMed] [Google Scholar]
- 7.Hetlevik O, et al. The wheezing schoolchild--an undiagnosed asthmatic: a follow-up of children with parentally reported episodes of wheeze without diagnosed asthma. Scandinavian Journal of Primary Health Care. 2000;18(2):122–126. doi: 10.1080/028134300750019034. [DOI] [PubMed] [Google Scholar]
- 8.Joseph CLM, et al. Effect of asthma intervention on children with undiagnosed asthma. Journal of Pediatrics. 2005;146:96–104. doi: 10.1016/j.jpeds.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 9.N.H.L.B.I . Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda: NIH; 2007. NIH Publication No. 07-4051. [DOI] [PubMed] [Google Scholar]
- 10.Bruzzese J-M, et al. Asthma education: the adolescent experience. Patient Education and Counseling. 2004;55(3):396–406. doi: 10.1016/j.pec.2003.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Bruzzese J-M, Evans D, Kattan M. School-based asthma programs. Journal of Allergy and Clinical Immunology. 2009;124(2):195–200. doi: 10.1016/j.jaci.2009.05.040. [DOI] [PubMed] [Google Scholar]
- 12.Butz A, et al. Rural children with asthma: impact of a parent and child asthma education program. Journal of Asthma. 2005;42(10):813–821. doi: 10.1080/02770900500369850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clark NM, et al. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades, and absenteeism. Chest. 2004;125(5):1674–1679. doi: 10.1378/chest.125.5.1674. [DOI] [PubMed] [Google Scholar]
- 14.Christiansen SC, Zuraw BL. Serving the underserved: school-based asthma intervention programs. Journal of Asthma. 2002;39(6):463–472. doi: 10.1081/jas-120004904. [DOI] [PubMed] [Google Scholar]
- 15.McGhan SL, et al. Evaluation of an education program for elementary school children with asthma. Journal of Asthma. 2003;40(5):523–533. doi: 10.1081/jas-120018785. [DOI] [PubMed] [Google Scholar]
- 16.Joseph CLM, et al. A web-based, tailored asthma management program for urban African-American high school students. American Journal of Respiratory & Critical Care Medicine. 2007;175(9):888–895. doi: 10.1164/rccm.200608-1244OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bruzzese J-M, et al. Effects a school-based intervention for urban adolescents with asthma: a controlled trial. American Journal of Respiratory and Critical Care Medicine. doi: 10.1164/rccm.201003-0429OC. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cicutto L, et al. Breaking the access barrier: evaluating an asthma center's efforts to provide education to children with asthma in schools. Chest. 2005;128(4):1928–1935. doi: 10.1378/chest.128.4.1928. [DOI] [PubMed] [Google Scholar]
- 19.Shah S, et al. Effect of peer led programme for asthma education in adolescents: cluster randomised controlled trial. British Medical Journal. 2001;322(7286):583–585. doi: 10.1136/bmj.322.7286.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hill R, et al. Can morbidity associated with untreated asthma in primary school children be reduced? A controlled intervention study. British Medical Journal. 1991;303(6811):1169–1174. doi: 10.1136/bmj.303.6811.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greineder DK, Loane KC, Parks P. A randomized controlled trial of a pediatric asthma outreach program. Journal of Allergy & Clinical Immunology. 1999;103(3 Pt 1):436–440. doi: 10.1016/s0091-6749(99)70468-9. [DOI] [PubMed] [Google Scholar]
- 22.Rosen CM, Rodriguez L. The Inner-City Asthma Intervention asthma counselor program: a collaborative model between physician and social worker to help empower families. Annals of Allergy, Asthma & Immunology. 2006;97(1) Suppl 1:S16–S19. doi: 10.1016/s1081-1206(10)60780-6. [DOI] [PubMed] [Google Scholar]
- 23.Redline S, et al. Development and validation of school-based asthma and allergy screening questionnaires in a 4-city study. Annals of Allergy, Asthma & Immunology. 2004;93(1):36–48. doi: 10.1016/S1081-1206(10)61445-7. [DOI] [PubMed] [Google Scholar]
- 24.Bandura A. Self-efficacy: the exercise of control. New York: W. H. Freeman Company; 1997. [Google Scholar]
- 25.Zimmerman BJ, et al. Self-regulating childhood asthma: a developmental model of family change. Health Education & Behavior. 1999;26(1):55–71. doi: 10.1177/109019819902600106. [DOI] [PubMed] [Google Scholar]
- 26.Bonner S, et al. An individualized intervention to improve asthma management among urban Latino and African-American families. Journal of Asthma. 2002;39(2):167–179. doi: 10.1081/jas-120002198. [DOI] [PubMed] [Google Scholar]
- 27.O'Brien MA, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews. 2007;(4) doi: 10.1002/14651858.CD000409.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osman M, et al. Gender-specific presentations for asthma, allergic rhinitis and eczema in primary care. Primary Care Respiratory Journal. 2007;16(1):28–35. doi: 10.3132/pcrj.2007.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Venn A, et al. Questionnaire study of effect of sex and age on the prevalence of wheeze and asthma in adolescence. BMJ. 1998;316(7149):1945–1946. doi: 10.1136/bmj.316.7149.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen Y, et al. Sex difference in hospitalization due to asthma in relation to age. Journal of Clinical Epidemiology. 2003;56(2):180–187. doi: 10.1016/s0895-4356(02)00593-0. [DOI] [PubMed] [Google Scholar]
- 31.Zannolli R, Morgese G. Does puberty interfere with asthma? Medical Hypotheses. 1997;48(1):27–32. doi: 10.1016/s0306-9877(97)90020-7. [DOI] [PubMed] [Google Scholar]