Abstract
A 16-year-old girl presented with primary amenorrhea and had had cyclical abdominal pain for almost a year. At examination we observed a painful mass in the lower abdomen and normal secondary sex characteristics. Perineal examination showed a bluish bulging hymen. Transabdominal ultrasonography revealed a dense mass in the pelvis measuring about 12×11 cm. We diagnosed an imperforate hymen with haematocolpos and haematometra. The hymen was opened surgically and a large quantity of menstrual blood was drained from the vagina and uterus. Postoperative recovery was normal without any pain. The patient now menstruates regularly. An imperforate hymen occurs in 0.05% of women. It is important to be aware of this while examining a female adolescent presenting with cyclical abdominal pain and primary amenorrhea. Late discovery of an imperforate hymen may lead to pain, infections, hydronephrosis and endometriosis with subfertility as a possible consequence.
BACKGROUND
Imperforate hymen is a rare cause of abdominal pain in female adolescents. It is seen in approximately 1 in 2000 females, although information on the true incidence is difficult to obtain.1,2 The lack of menses in an adolescent girl of (post-)menarcheal age with cyclical abdominal pain, urinary retention, constipation and/or a (symptomatic) lower abdominal mass suggests this condition should be considered.3 This case illustrates that there is quite often a considerable delay before a proper diagnosis is reached. The aim of this communication is to increase awareness of imperforate hymen among clinicians examining adolescent girls with lower abdominal pain.
CASE PRESENTATION
A 16-year-old girl was admitted with a history of lower abdominal pain. She was asymptomatic until a year previously. She then started developing cyclical crampy pain in the lower abdomen, which lasted for 7 days every month. The pain had become more severe during the previous 2 months and the size of her abdomen had increased over the past few months. There was no history of nausea, vomiting, fever, altered bowel habits or problems with urinating. She was 13 years old and had not yet had a menstrual period, but did have pubic hair and breast buds, confirming the onset of puberty. The patient denied any vaginal discharge and there was no history of sexual activity. No other members of her family had similar or other physical complaints. The medical history was unremarkable.
INVESTIGATIONS
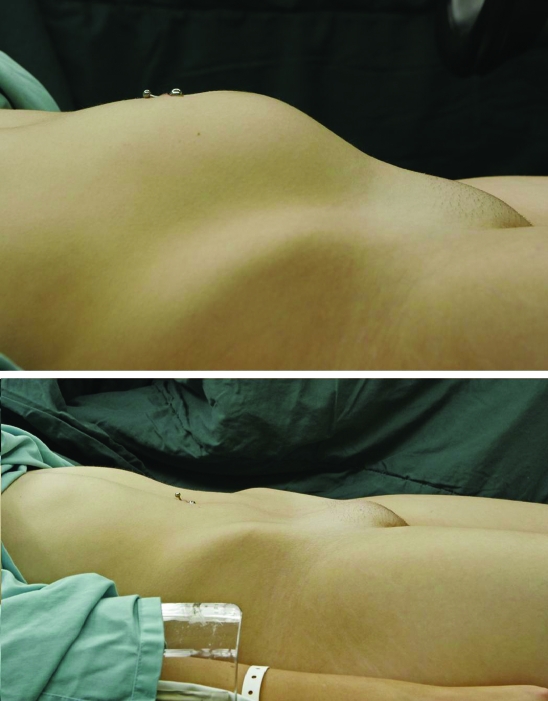
On physical examination, the secondary sex characteristics, such as pubic hair and breast buds, were well developed. A mobile, non-tender mass, arising from the pelvis to the belly button, was felt in the abdomen (fig 1, upper image). Gynaecologic examination revealed a bulging bluish hymen (fig 2). No other gross external abnormalities of the external genitalia were observed. A pelvic ultrasound showed a homogenous, hypoechoic mass in the vagina and uterus measuring about 12×11 cm. Both the ovaries were normal.
Figure 1.
Swollen abdomen with haematometra due to an imperforate hymen and the abdomen after hymenectomy.
Figure 2.
Imperforate hymen.
DIFFERENTIAL DIAGNOSIS
We diagnosed an imperforate hymen with consequent accumulation of blood in the vagina and uterus (haematocolpos and haematometra, respectively).
TREATMENT
Two days later the patient underwent a hymenectomy with a cruciate incision. Approximately 500 ml of viscous, chocolate coloured blood and clots were drained (fig 3).
Figure 3.
Surgical treatment of an imperforate hymen.
OUTCOME AND FOLLOW-UP
Immediately after the operation the size of the abdomen had regained normal proportions (fig 1, lower image).
During a 2-month follow-up, the patient was asymptomatic and started to have regular menstrual cycles.
DISCUSSION
Imperforate hymen is a rare though serious cause of abdominal pain in female adolescents. It is seen in approximately 1 in 2000 females.1,2,4 The hymen is an embryological remnant of mesodermal tissue that normally perforates during the later stages of embryo development. The hymen is called imperforate if there is no perforation of this membrane.
The reason for non-perforation of this membrane is unknown. Imperforate hymen occurs mostly in a sporadic manner, although some familial occurrences have been reported. Both the recessive and dominant modes of transmission have been suggested, but no genetic markers or mutations have been proven as aetiological factors.5,6 An imperforate hymen in younger children (<10 years) is discovered by chance in 90% of cases, while 100% of affected adolescents first present with symptoms.2
The most common symptoms of an imperforate hymen are cyclical abdominal pain and urinary retention, usually presenting between the ages of 13 and 15 years (when menarche occurs).7,8 There is primary amenorrhea but secondary sex characteristics are well developed. Because the vaginal outflow is obstructed by the non-perforated hymen, menstrual blood accumulates in the vagina (haematocolpos) and the uterus (haematometra). This may lead to mechanical effects on the urethra, bladder, intestines or pelvic blood vessels which can result in urinary retention, obstipation or oedema of the legs.7,9–14 Irritation of the sacral plexus or nerve roots can cause lower back pain.8 Problems with intercourse are rarely mentioned, probably because most of the patients are still sexually inactive.15
Some symptoms of appendicitis are similar to those of an imperforate hymen, and there are cases where groundless appendectomies have been performed.16 In addition, there is often an initial diagnosis of infection of the bladder, nephrolithiasis or abdominal tumour, which leads to unnecessary examinations and treatment. The history and physical examination are frequently incomplete.2 One should always consider an imperforate hymen if there is a discrepancy between the Tanner stage and menarcheal status.2
Gynaecological examination reveals a bluish bulging hymen and generally an abdominal mass. The diagnosis can be established with an abdominal ultrasound showing the pelvic cystic mass. Imperforate hymen should be differentiated from a low transverse vaginal septum using the Valsalva manoeuvre: an imperforate hymen should bulge and a transverse vaginal septum should not.4 Imperforate hymen is usually not associated with any other Müllerian abnormalities and extensive investigation for urogenital anomalies is unnecessary.4
Early diagnosis of an imperforate hymen is important, since it can lead to serious complications such as infections, hydronephrosis, kidney failure, endometriosis and subfertility.17–19 A retrospective study showed that eight of nine patients with haematocolpos or haematometra due to an outflow obstruction had endometriosis at the time of intra-abdominal operation.20
Treatment of haematocolpos or haematometra due to an imperforate hymen is to make cruciate incision in the hymen which allows the accumulated blood to drain away. This has to be done aseptically as a closed vagina lacks protective Doederlein’s bacilli and the pH is alkaline or weakly acidic; there is a poor natural resistance to bacteria entering from the lower genital tract and the blood and debris provide a good culture medium.4 The complications of a hymenectomy are bleeding, scarring and stenosis of the vaginal opening.21 Less invasive treatments for an imperforate hymen include the use of CO2 lasers or a Foley catheter.22,23
In a retrospective study of the long term results of surgical correction of imperforate hymen, nine of 15 patients had an irregular menstrual cycle and six of 15 patients had dysmenorrhea (over a follow-up of 8.5 years). Most patients had no sexual dysfunction. Pre-operative complaints of cryptomenorrhea (n=15), abdominal pain (n=11), palpable mass in the lower abdomen (n=9), urinary retention (n=6), dysuria (n=3) and problems defecating (n=4) almost all disappeared after surgery.15 Eight patients worried about their future fertility; two of them were attempting pregnancy and were successful. Another study showed that 86% of patients who attempted pregnancy succeeded after surgical correction of imperforate hymen.18
LEARNING POINTS
In adolescent girls with cyclical pain, it is very important to take a complete gynaecological history and perform a gynaecological examination as serious complications may follow an unnecessary delay in diagnosis.
Consider an imperforate hymen when there is a lack of menses in an adolescent girl with cyclical abdominal pain.
Consider an imperforate hymen if there is a discrepancy between the Tanner stage and menarcheal status.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Parazzini F, Cecchetti G. The frequency of imperforate hymen in Northern Italy. Int J Epidemiol 1990; 19: 763. [DOI] [PubMed] [Google Scholar]
- 2.Posner JC, Spandorfer PR. Early detection of imperforate hymen prevents morbidity from delays in diagnosis. Pediatrics 2005; 115: 1008. [DOI] [PubMed] [Google Scholar]
- 3.Doyle JC. Imperforate hymen: with and without hematocolpos. A review of the literature and a report of twenty cases. Cal West Med 1942; 56: 242–7 [PMC free article] [PubMed] [Google Scholar]
- 4.Dane C, Dane B, Erginbas M, et al. Imperforate hymen - a rare cause of abdominal pain: two cases and review of the literature. J Pediatr Adolesc Gynecol 2007; 20: 245–7 [DOI] [PubMed] [Google Scholar]
- 5.Sakalkale R, Samarakkody U. Familial occurrence of imperforate hymen. J Pediatr Adolesc Gynecol 2005; 18: 427–9 [DOI] [PubMed] [Google Scholar]
- 6.Usta IM, Awwad JT, Usta JA, et al. Imperforate hymen: report of an unusual familial occurrence. Obstet Gynecol 1993; 82: 655. [PubMed] [Google Scholar]
- 7.Hall DJ. An unusual case of urinary retention due to imperforate hymen. J Accid Emerg Med 1999; 16: 232–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Letts M, Haasbeek J. Hematocolpos as a cause of back pain in premenarchal adolescents. J Pediatr Orthop 1990; 10: 731. [DOI] [PubMed] [Google Scholar]
- 9.Dickson CA, Saad S, Tesar JD. Imperforate hymen with hematocolpos. Ann Emerg Med 1985; 14: 467–9 [DOI] [PubMed] [Google Scholar]
- 10.Isenhour JL, Hanley ML, Marx JA. Hematocolpometra manifesting as constipation in the young female. Acad Emerg Med 1999; 6: 752–3 [DOI] [PubMed] [Google Scholar]
- 11.Nisanian AC. Hematocolpometra presenting as urinary retention. J Reprod Med 1993; 38: 57–60 [PubMed] [Google Scholar]
- 12.Tuncer R, Tunali N. Imperforate hymen as a cause of bladder perforation and intestinal obstruction. Br J Urol 1997; 79: 993–4 [DOI] [PubMed] [Google Scholar]
- 13.Wort SJ, Heman-Ackah C, Davies A. Acute urinary retention in the young female. Br J Urol 1995; 76: 667–8 [DOI] [PubMed] [Google Scholar]
- 14.Yu TJ, Lin MC. Acute urinary retention in two patients with imperforate hymen. Scand J Urol Nephrol 1993; 27: 543–4 [DOI] [PubMed] [Google Scholar]
- 15.Liang CC, Chang SD, Soong YK. Long-term follow-up of women who underwent surgical correction for imperforate hymen. Arch Gynecol Obstet 2003; 269: 5–8 [DOI] [PubMed] [Google Scholar]
- 16.Nazir Z, Rizvi RM, Qureshi RN, et al. Congenital vaginal obstructions: varied presentation and outcome. Pediatr Surg Int 2006; 22: 749–53 [DOI] [PubMed] [Google Scholar]
- 17.Loscalzo IL, Catapano M, Loscalzo J, et al. Imperforate hymen with bilateral hydronephrosis: an unusual emergency department diagnosis. J Emerg Med 1995; 13: 337–9 [DOI] [PubMed] [Google Scholar]
- 18.Rock JA, Zacur HA, Dlugi AM, et al. Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstet Gynecol 1982; 59: 448–51 [PubMed] [Google Scholar]
- 19.Hijazeen R. Imperforate hymen with bilateral hydronephrosis in a neonate. Saudi J Kidney Dis Transpl 1995; 9: 33–5 [PubMed] [Google Scholar]
- 20.Olive DL, Henderson DY. Endometriosis and mullerian anomalies. Obstet Gynecol 1987; 69: 412–15 [PubMed] [Google Scholar]
- 21.Chang JW, Yang LY, Wang HH, et al. Acute urinary retention as the presentation of imperforate hymen. J Chin Med Assoc 2007; 70: 559–61 [DOI] [PubMed] [Google Scholar]
- 22.Friedman M, Gac D, Peretz B. Management of imperforate hymen with the carbon dioxide laser. Obstet Gynecol 1989; 74: 270–2 [PubMed] [Google Scholar]
- 23.Ali A, Cetin C, Nedim C, et al. Treatment of imperforate hymen by application of Foley catheter. Eur J Obstet Gynecol Reprod Biol 2003; 106: 3–4 [DOI] [PubMed] [Google Scholar]