Abstract
A case of undiagnosed congenital idiopathic megacolon in a 16-year-old boy who presented with toxic megacolon and cardiovascular instability with a background of longstanding constipation is presented. He underwent life-saving subtotal colectomy from which he made a full recovery.
Background
This case highlights the challenges of diagnosing and managing paediatric and adolescent patients with congenital idiopathic megacolon, especially when presenting as an emergency. As far as we are aware, this is the first case reporting life-saving surgery for toxic megacolon in an adolescent with undiagnosed congenital idiopathic megacolon.
Case presentation
A 16-year-old Caucasian boy was admitted as an emergency case with a history of abdominal distension, nausea, vomiting and constipation over the previous 3 days. From his medical history he had had constipation since he was a toddler, with faecal overflow incontinence. He also had bronchial asthma.
He was referred to paediatricians when he was 6 years old and subsequently to a colorectal surgeon. An examination under anaesthetic with sigmoidoscopy, manual evacuation of faeces and a rectal mucosal biopsy was performed at that time. The histology showed a mild chronic inflammatory infiltrate.
He was one of three siblings, the others being 23 and 19 years of age and in good health. Regular medications included movicol (polyethylene glycol 3350, sodium bicarbonate, sodium chloride and potassium chloride), senna and sodium docusate.
On clinical examination, he was cachectic, emaciated and dehydrated. His pulse rate (PR) was 129 beats/min. Blood pressure was 153/107 mm Hg. His respiratory rate was 22 breaths/min. His oxygen saturation (SaO2) was 95% on room air. He was drowsy at the time of presentation.
The abdomen was grossly distended with palpable faeces. Digital rectal examination revealed hard stools in the rectum with overflow of liquid faeces. The patient was resuscitated with intravenous fluids and catheterised. Phosphate enemas were given with no benefit. A decision was taken to perform a manual evacuation of faeces under a general anaesthetic. At 2 h after his admission, he became cardiovascularly compromised with SaO2 of 74%, PR of 158 beats/min and blood pressure of 160/105 mm Hg. Arterial blood gases showed a pH of 6.9, base excess of 13.1 mEq/litre, a lactate level of 8.0 μmol/litre, pO¼sub>2 11.51 kPa and pCO2 12.41 kPa.
He was taken urgently to the operating theatre for manual evacuation of faeces, to decompress the abdomen and relieve the pressure on his airways and mediastinum. After awake intubation in the sitting position, 3.8 kg of semisolid faeces were evacuated.
This resulted in some improvement of his airway pressures and improved oxygenation. He was ventilated overnight in the Intensive Therapy Unit (ITU). His vital signs improved.
The following morning he was feverish and a CT scan of the abdomen revealed free air in the peritoneal cavity. The patient was therefore prepared for a laparotomy. At surgery, there was huge megacolon and megarectum with impending caecal and transverse colonic perforations. There was turbid fluid in the peritoneal cavity. He underwent a subtotal colectomy and end ileostomy with a mucous fistula.
Investigations
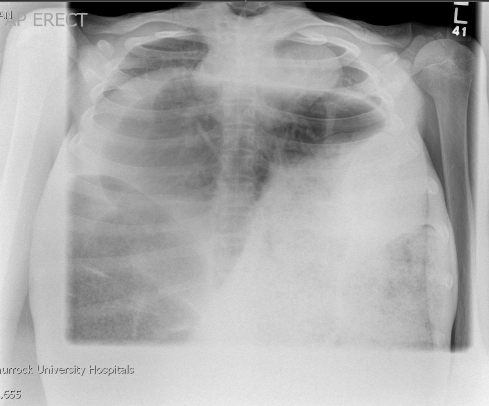
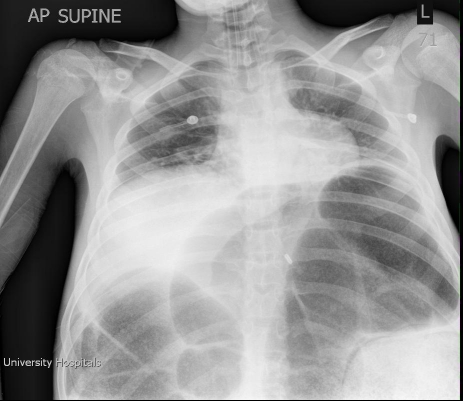
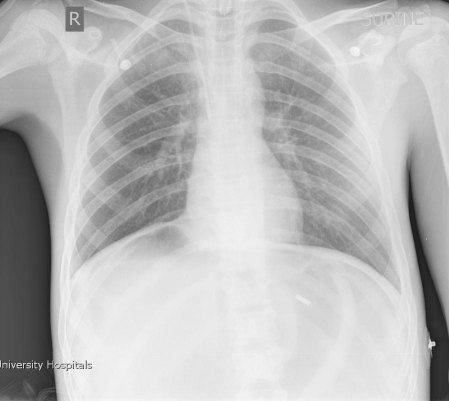
Abdominal x-ray and chest x-ray on admission revealed marked megacolon with severe displacement of the diaphragm, lungs and mediastinum cranially (figure 1). After manual evacuation of faeces and subsequent colectomy, there were marked improvements in chest x-ray appearance (figures 2 and 3)
Figure 1.
Chest x-ray on admission.
Figure 2.
Chest x-ray post manual evacuation of rectum.
Figure 3.
Chest x-ray post subtotal colectomy.
Outcome and follow-up
The postoperative period was complicated by ileus requiring total parenteral nutrition and an intra-abdominal collection, which was percutaneously drained.
The patient was discharged 17 days after his admission. He was followed-up in the outpatient clinic regularly and his weight was improving. The histology was reported as haemorrhagic infarction with transmural acute inflammation with cryptitis and occasional crypt abscesses. Immunohistochemistry showed the presence of ganglion cells in the submucosal and intramural plexuses. Definite features of Hirschsprung's disease were not seen.
The patient was referred to a specialist unit where anorectal physiological investigations revealed a morphologically normal rectum and a normal rectoanal inhibitory reflex. He has been diagnosed as having congenital idiopathic megacolon and is awaiting ileorectal anastomosis.
Discussion
Megacolon is a descriptive term that defines dilatation of the colon that is not caused by mechanical obstruction.1–2 The causes of megacolon can be broadly classified into congential or acquired. Patients with congenital megacolon experience onset of constipation in infancy and early childhood.
The differential diagnosis of congenital megacolon includes visceral myopathies and enteric neuropathies, for example, Hirschsprung's disease and Waardenburg–Shah syndrome. A large proportion of patients with non-Hirschsprung's congenital megacolon have the onset of symptoms in early childhood or adolescence and it seemed to occur more commonly in men.3–4 The true prevalence of this disorder is unknown.4–5 Idiopathic megacolon describes an abnormality of the colon characterised by a permanent distension of the bowel lumen in the absence of an identifiable cause. In contrast to the well defined histological abnormalities in Hirschsprung's disease, the pathological basis underlying idiopathic megacolon is unknown. Postulated mechanisms include abnormalities in the extrinsic nerves, the enteric nervous system, intestinal smooth muscle and neurotransmitters.6–8
Idiopathic megacolon is a diagnosis of exclusion made using a multimodal approach. Identification of electrolyte imbalances and thyroid dysfunction are important. Anorectal manometry may show lack of relaxation of the internal anal sphincter with balloon rectal distension. A normal rectoanal inhibitory reflex excludes the diagnosis of Hirschsprung's disease (HD). The diagnosis of HD must be established by a rectal suction biopsy showing the absence of ganglion cells in the distal colon.
Many patients with idiopathic megacolon can be managed successfully using long-term laxatives, although some require surgery.9 Surgical options include stoma formation, colectomy and anastomosis10 and a variety of pull-through procedures.11 Emergency surgery is indicated if there is evidence of toxic megacolon or volvulus.
The literature reports many cases of emergency surgery for toxic megacolon in association with ulcerative colitis, pseudomembranous colitis and HD. It is rare in cases of idiopathic megacolon. Leventhal et al12 reported a case of toxic idiopathic megacolon with a fatal outcome in a mentally retarded adolescent who also had pseudomembranous colitis.
The emergency management of idiopathic megacolon, such as in the case we have reported, revolves around aggressive resuscitation, followed by emergency decompression measures such as manual evacuation, formation of stoma or subtotal colectomy.
Learning points.
Paediatric patients with constipation should be thoroughly investigated, as establishing the correct diagnosis is important in order to achieve good long-term functional results.
Hirschsprung's disease should be excluded.
Toxic megacolon remains a life-threatening complication that should be recognised and treated aggressively.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Camilleri M. Acute and chronic pseudo-obstruction. In: Felman M, Friedman LS, Sleisenger MH, eds. Sleisenger & Fordtran's gastrointestinal and liver disease. 8th edn Philadelphia, USA: Saunders; 2007:2679–702 [Google Scholar]
- 2.Camilleri M. Dysmotility of the small intestine and colon. In: Yamada T, ed. Textbook of gastroenterology. 4th edn Vol 1 Philadelphia, USA: Lippincott Williams & Wilkins; 2003:1486–529 [Google Scholar]
- 3.Barnes PR, Lennard-Jones JE, Hawley PR, et al. Hirschsprung's disease and idiopathic megacolon in adults and adolescents. Gut 1986;27:534–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gattuso JM, Kamm MA. Clinical features of idiopathic megarectum and idiopathic megacolon. Gut 1997;41:93–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gladman MA, Scott SM, Lunniss PJ, et al. Systematic review of surgical options for idiopathic megarectum and megacolon. Ann Surg 2005;241:562–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gattuso JM, Kamm MA, Talbot JC. Pathology of idiopathic megarectum and megacolon. Gut 1997;41:252–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gattuso JM, Hoyle CH, Milner P, et al. Enteric innervation in idiopathic megarectum and megacolon. Int J Colorectal Dis 1996;11:264–71 [DOI] [PubMed] [Google Scholar]
- 8.Gattuso JM, Smith VV, Kamm MA. Altered contractile proteins and neural innervation in idiopathic megarectum and megacolon. Histopathology 1998;33:34–8 [DOI] [PubMed] [Google Scholar]
- 9.Kamm MA, Stabile G. Management of idiopathic megarectum and megacolon. Br J Surg 1991;78:899–900 [DOI] [PubMed] [Google Scholar]
- 10.Stabile G, Kamm MA, Hawley PR, et al. Colectomy for idiopathic megarectum and megacolon. Gut 1991;32:1538–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marquez TT, Acton RD, Hess DJ, et al. Comprehensive review of procedures for total colonic aganglionosis. J Pediatr Surg 2009;44:257–65; discussion 265 [DOI] [PubMed] [Google Scholar]
- 12.Leventhal A, Gimmon Z. Toxic idiopathic megacolon: fatal outcome in a mentally retarded adolescent. Dis Colon Rectum 1978;21:383–6 [DOI] [PubMed] [Google Scholar]