Abstract
We would like to report a case involving a 38-year-old woman who presented with knee and ankle swellings 2 weeks prior to admission. There were also multiple painful oral ulcers and a few skin sores on the wrist. She also had associated diarrhoea for 2 weeks. There was also marked loss of weight (6 kg in 2 weeks). Colonoscopy examination showed macroscopic and histopathological findings of Crohn’s disease; however, skin histology showed extensive neutrophilic infiltration in the dermis, predominantly in the perivascular region. Her final diagnosis was Sweet’s syndrome with Crohn’s disease.
BACKGROUND
The presence of Sweet’s syndrome and Crohn’s disease is a rare occurrence. Furthermore, it highlights the presenting symptoms of arthritis and gastrointestinal.
CASE PRESENTATION
A 38-year-old woman, who worked as a secretary, presented with bilateral knee and ankle swellings 2 weeks prior to admission. The pain was not associated with any morning stiffness. She also denied any other joint swellings, alopecia and photosensitivity rash. However, she had multiple painful oral ulcers and a few skin sores on the wrist.
She also had history of diarrhoea for 2 weeks. There was loose stool with mucous but no malaena and blood. There was no history of bloated abdomen, pain or vomiting. She also claimed that she had marked loss of weight (6 kg in 2 weeks).
These symptoms prevented her from doing her household chores and work.
There were no medical or surgical problems before. Clinically she was comfortable with a mild grade fever of 37.5°C.
On examination, she had mild pallor. There were bilateral episcleritis with multiple aphthous ulcer of the mouth. Cardiovascular and respiratory systems were normal. The abdomen was soft and not tender. There was no organomegaly. No lymph nodes were palpable.
There was also a blistering skin lesion on the right wrist measuring 2×3 cm.
There were bilateral knee and ankle swellings, with an effusion on the left knee swollen and tender to touch.
INVESTIGATIONS
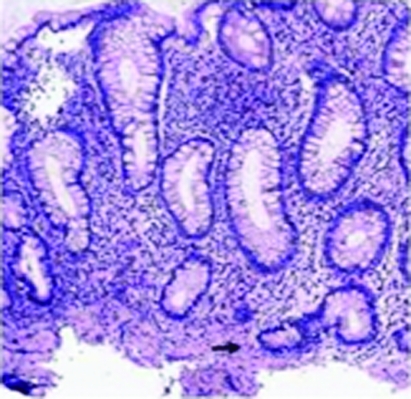
Colonoscopy examination showed multiple linear ulceration with “cobble stoning” appearance, starting from descending colon to caecum, sparing the rectum. Multiple biopsies were taken histologically showing sections of colonic mucosa with crypt branching and cryptitis in caecum, ascending, transverse colon (fig 1). There was no cryptitis in descending, sigmoid colon and rectum with some crypt branching and no granuloma in all sections.
Figure 1.
Colonoscopy examination showed multiple linear ulceration with “cobble stoning” appearance starting from descending colon to caecum sparing the rectum. Multiple biopsies were taken histologically showing sections of colonic mucosa with crypt branching and cryptitis in caecum, ascending, transverse colon. There was no cryptitis in descending, sigmoid colon and rectum with some crypt branching and no granuloma in all sections.
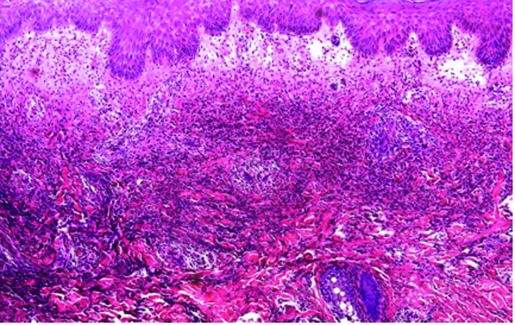
Skin biopsy revealed extensive neutrophilic infiltration in the dermis, predominantly in the perivascular region. There was no granuloma and immunofluorescence studies were negative— neutrophilic dermatoses (fig 2).
Figure 2.
Skin biopsy revealed extensive neutrophilic infiltration in the dermis predominantly in the perivascular region. There was no granuloma and immunofluorescence studies were negative— neutrophilic dermatose.
DIFFERENTIAL DIAGNOSIS
Ulcerative colitis, monoclonal gammopathy, rheumatoid arthritis, systemic lupus erythematosus, Sjogren’s syndrome and Behçet’s disease.
TREATMENT
She was transfused with 2 pints of pack cells. Subsequently she was started on oral prednisone (40 mg daily) with oral mesalazine (1 g four times a day) and oral antibiotic ciprofloxacin (500 mg three times a day) with oral metronidazole (400 mg three times a day) for her Crohn’s colitis.
OUTCOME AND FOLLOW-UP
Two weeks later, there was no more diarrhoea or oral ulcer and the skin lesion was well healed.
DISCUSSION
Sweet’s syndrome is an acute febrile neutrophilic dermatosis, which may be associated with inflammatory, infectious or neoplastic diseases. Its association with Crohn’s disease is very rare and when reported it has been mainly associated with Crohn’s colitis. Sweet’s syndrome may be considered as one of the extraintestinal manifestations of Crohn’s colitis. Early diagnosis of this dermatosis may be important because of the prompt response to treatment with corticosteroids.
It can also present with a broad spectrum of skin lesions, which include vesiculopustules, plaques, nodules and ulcerations. There is a strong predilection for women (87%), patients with colonic disease (100%) and those with other extra intestinal features (77%).1
Acute febrile neutrophilic dermatoses was first described in 1964 by Robert Douglas Sweet.2 The neutrophilic dermatoses are a group of non-infectious dermatoses with pathognomonic presence of an angiocentric, vessel-based neutrophilic infiltrate seen on histological examination.3
Sweet’s syndrome is an uncommon disorder consisting of rapidly evolving tender, red cutaneous plaques, fever and leucocytosis. It usually occurs in women 30–60 years of age with a 5:1 preponderance compared with males. The cutaneous findings of Sweet’s syndrome are distinctive. There is sudden onset of multiple bright to dusky red, sharply marginated, exquisitely tender, erythematous plaques. They are often mamillated (studded with closely set pseudovesicular papules) and are commonly located on the dorsal aspect of the upper extremities, neck and face regions4 The lesions usually heal in 5–12 weeks without scarring, but may recur in about a third of patients. Oral ulcers may sometimes be present.5 Lymphadenopathy is characteristically absent. Ninety per cent of patients have mild to moderate fever and 75% present with some form of prodromal illness, most commonly an upper respiratory infection. Twenty five per cent have arthralgias or an acute non-destructive pauciarticular arthritis. Conjunctivitis or episcleritis occurs with variable frequency. The most common laboratory abnormalities are a raised erythrocyte sedimentation rate and leucocytosis with neutrophilia.6
Sweet’s syndrome may represent a hypersensitivity or immunological phenomenon. There is increasing evidence that the disease is a T cell cytokine-mediated disease.7 On pathological examination of a plaque, a characteristic patchy, perivascular, or band-like infiltrate of mature neutrophils in the middle and upper dermis can be found.
The disease is also associated with ulcerative colitis and Crohn’s disease, monoclonal gammopathy, rheumatoid arthritis, systemic lupus erythematosus, Sjogren’s syndrome and Behçet’s disease. Sweet’s syndrome, when associated with Crohn’s disease or ulcerative colitis, shows a stronger predilection for women than men. There is also a higher incidence of colonic involvement and extraintestinal features like in this patient.8 The rash is associated with active disease in most patients, but may sometimes precede the onset of intestinal symptoms.
The natural history of untreated Sweet’s syndrome is resolution of the skin lesions within 6–8 weeks.8 The cutaneous and extracutaneous manifestations characteristically respond completely and immediately to systemically administered corticosteroids. Relapses are common if steroids are tapered too quickly. An initial dose of 40–60 mg of prednisone is recommended with tapering over 4–6 weeks. Our patient was started on prednisone (40 mg/day) with complete resolution of joint symptoms within 48 hours. The skin lesions resolved over the next few weeks and her prednisone was tapered gradually over the next few months to maintain quiescence of symptoms.
Other agents that have been reported to be effective include indomethacin, dapsone, potassium iodide, colchicine, clofazimine and isotretinoin.5
LEARNING POINTS
Sweet’s syndrome is an extra intestinal manifestation of Crohn’s disease.
Resolution of Sweet’s syndrome is prompt with corticosteroids.
The resolution of Sweet’s syndrome can parallel Crohn’s disease activity.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication.
REFERENCES
- 1.Travis S, Davies MG, Hughes S. Sweet’s syndrome: an unusual cutaneous feature of Crohn’s disease or ulcerative colitis. Eur J Gastroenterol Hepatol 1997; 9: 715–20 [DOI] [PubMed] [Google Scholar]
- 2.Sweet RD. An acute febrile neutrophilic dermatosis. Br J Dermatol 1964; 76: 349–56 [DOI] [PubMed] [Google Scholar]
- 3.Jorizzo JL, Solomon AR, Zanolli MD, et al. Neutrophilic vascular reaction. J Am Acad Dermatol 1998; 19: 983–1005 [DOI] [PubMed] [Google Scholar]
- 4.Storer JS, Nesbitt LT, Jr, Galen WK, et al. Sweet’s syndrome. Int J Dermatol 1983; 22: 8–12 [DOI] [PubMed] [Google Scholar]
- 5.von den Driesch P. Sweet’s syndrome (acute febrile neutrophilic dermatosis). J Am Acad Dermatol 1994; 31: 535–56 [DOI] [PubMed] [Google Scholar]
- 6.Cooper PH, Innes DJ, Jr, Greer KE. Acute febrile neutrophilic dermatosis (Sweet’s syndrome) and myeloproliferative disorders. Cancer 1983; 51: 1518–26 [DOI] [PubMed] [Google Scholar]
- 7.von den Driesch P, Gruschwitz M, Hornstein OP. Adhesion molecule modulation in Sweet’s syndrome compared to erythema multiforme. Eur J Dermatol 1993; 3: 393–7 [Google Scholar]
- 8.Travis S, Innes N, Davies MG, et al. Sweet’s syndrome: an unusual cutaneous feature of Crohn’s disease or ulcerative colitis. The Southwest Gastroenterology Group. Eur J Gastroenterol Hepatol 1997; 9: 715–20 [DOI] [PubMed] [Google Scholar]