Abstract
We report the application of quantitative mass spectrometry to identify plasma membrane proteins differentially expressed in melanoma cells with high vs. low metastatic abilities. Using stable isotope labeling with amino acids in culture (SILAC) coupled with nanospray tandem mass spectrometry, we identified CUB-domain–containing protein 1 (CDCP1) as one such differentially expressed transmembrane protein. CDCP1 is not only a surface marker for cells with higher metastatic potential, but also functionally involved in enhancing tumor metastasis. Overexpression of CDCP1 also correlates with activation of Src. Pharmacological reagents, PP2 and Dasatinib, which block Src family kinase activation, blocked scattered growth of CDCP1-overexpressing cells in 3D Matrigel culture, suggesting that CDCP1 might function through the activation of Src-family kinases (SFKs). This hypothesis was further supported by mutational studies of CDCP1. Whereas wild-type CDCP1 enhances Src activation, point mutation Y734F abolishes in vitro dispersive growth in 3D culture and in vivo metastasis-enhancing activities of CDCP1. In addition, the Y734F mutation also eliminated enhanced Src activation. Thus, this work provides molecular mechanisms for the metastasis-enhancing functions of CDCP1.
Despite significant improvement in treatments for cancer, most mortality is due to tumor metastasis to distant organs. Tumor metastasis is a complicated process, presumably involving tumor cell detachment and migration/invasion from the primary site (local invasion); intravasation, survival in the circulation, arrest, and extravasation from the circulation (systemic dissemination); and growth, survival, and angiogenesis at the distant organ sites (colonization) (1–4). It has become increasingly clear that tumor cells cooperate with environmental factors, including other cell types in the tumor, such as fibroblasts, macrophages, platelets, and endothelial cells, as well as extracellular matrix, to metastasize (5–7). On the other hand, many tumor-intrinsic factors have also been identified that promote (8–11) or inhibit (12–14) tumor metastasis, using expression microarrays and other large-scale profiling technologies such as copy-number variation and SNP arrays.
Plasma membrane proteins mediate communications between tumor cells and their microenvironment, acting in a sense as the “antennae” through which cells sense their microenvironment and determine cellular outcomes, such as cell proliferation, migration, or apoptosis, in response to the combined stimuli present in the microenvironment. Some plasma membrane proteins have been well studied, such as receptors for growth factors, cytokines, and chemokines, and a number have been shown to play important roles during various stages of tumor progression and metastasis. In addition, several cell–extracellular matrix and cell–cell adhesion molecules have been shown in different systems to contribute to tumor metastasis. Examples include up-regulation of integrin αV and CD44 and reduction of E-cadherin. However, our insights into changes in many other plasma membrane proteins are still limited. For example, CD82 (or KAI1), a metastasis suppressor identified >10 y ago (12), has only recently been shown to exert its function through interaction with DARC on endothelial cells (15). Plasma membrane proteins, such as CD133 and CD44 are often used as markers to define tumor-initiating cells and cells with higher propensity to metastasize (16). We are particularly interested in cell-surface membrane proteins, and we wish to identify new markers and/or players in melanoma metastasis and to elucidate the mechanisms by which these proteins function.
In this article, we report application of quantitative proteomics approaches to investigate differences in protein levels, particularly those in plasma membrane proteins, between closely related poorly and highly metastatic melanoma cells. Using such approaches, we identified CUB-domain–containing protein 1 (CDCP1) as a membrane protein that is up-regulated in highly metastatic melanomas. We find that CDCP1 contributes to the enhancement of melanoma metastasis, without affecting tumor growth at primary s.c. sites. In vitro, CDCP1 causes detachment of melanoma cells in 2D culture and dispersive growth in 3D Matrigel cultures. Mechanistically, CDCP1 activates Src family kinases to exert these biological functions both in vitro and in vivo.
Results
Stable Isotope Labeling with Amino Acids in Culture (SILAC) Coupled with Tandem Mass Spectrometry Identifies Plasma Membrane Proteins Differentially Expressed Between Highly and Poorly Metastatic Melanoma Cells.
A colloidal silica protocol was used for plasma membrane enrichment and removal of intracellular membrane [endoplasmic reticulum (ER) or Golgi] contamination (see Fig. S1A for details). When the final enriched membrane fraction was separated by SDS/PAGE and blotted with antibodies against different subcellular markers, significant amounts of cytoplasmic, ER, Golgi, and nuclear proteins were removed using this method, whereas plasma membrane proteins were retained (Fig. S1B). We then labeled highly metastatic MA2 cells and poorly metastatic A375 cells with stable isotope-enriched arginine and lysine in culture using SILAC (Fig. S1C). Following plasma membrane enrichment, quantitative mass spectrometry was applied to determine the differentially expressed membrane proteins (Fig. S1D). Among plasma membrane proteins showing differences in protein levels, EphA2 was found to have lower expression levels in MA2 cells, and integrins αV and β3 and CD44 exhibited higher levels. These data conform with earlier work (17–21). We also observed that CDCP1 was up-regulated in MA2 cells (Fig. S1D). For details, see SI Materials and Methods and Fig. S1).
CDCP1 Is Up-Regulated in Highly Metastatic Melanoma Cell Lines.
CDCP1, also known as SIMA135 or Trask, is a transmembrane glycoprotein that contains three putative extracellular CUB domains. CUB domains are believed to function in protein–protein (22, 23) and protein/carbohydrate (24) interactions. We initially focused on CDCP1 for several reasons: i) CDCP1 was previously reported to be overexpressed in human colorectal and lung cancers (25, 26) and up-regulated in highly metastatic human carcinoma cells (27). ii) Tyrosine phosphorylation of CDCP1 correlates with cell detachment from extracellular matrix, and overexpression of CDCP1 leads to cell rounding and cell detachment, suggesting potential roles in cell adhesion and migration (28–30), processes that have been linked to tumor cell metastasis. iii) In addition to its expression on epithelial cells, CDCP1 has limited expression on hematopoietic and mesenchymal stem cells (31, 32).
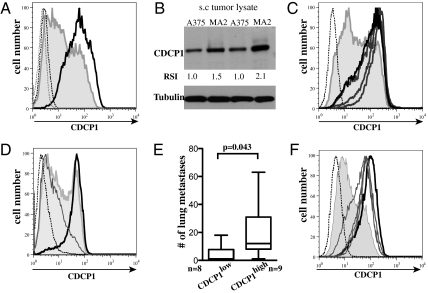
We first confirmed the mass spectrometry results by other means. When cultured cells were analyzed for surface CDCP1 expression levels using flow cytometry, MA2 cells showed higher expression levels relative to A375 cells (Fig. 1A). In line with the in vitro flow cytometric data, increased CDCP1 total protein levels were observed in the s.c. tumors generated from MA2 cells compared with those from A375 cells using Western analysis (Fig. 1B). Using flow cytometry we investigated the surface expression levels of CDCP1 on other highly metastatic melanoma cells derived independently by in vivo selection of parental A375 cells (14). All highly metastatic cells (MA1, MA2, MC1, and MC2) expressed higher cell surface levels of CDCP1 compared with A375 cells (Fig. 1C).
Fig. 1.
CDCP1 expression is up-regulated in highly metastatic melanoma cells and correlates with metastatic potential. (A) Flow-cytometric analysis of poorly metastatic A375 cells (shaded curve) and highly metastatic MA2 cells (thick line) shows enhanced CDCP1 expression in MA2 cells in vitro. (B) Western blotting reveals that total in vivo CDCP1 expression was enhanced in s.c. tumors derived from MA2 cells relative to those from A375 cells. Relative signal intensity (RSI) for CDCP1 is shown under the Western blot. (C) Flow-cytometric analysis shows CDCP1 surface levels are increased in all highly metastatic cells (MA1, MA2, MC1, and MC2) (thick lines) compared with poorly metastatic parental A375 (shaded curve). (D) Surface expression of CDCP1 on A375 cells reveals two peaks (shaded line), which can be sorted into two subpopulations: CDCP1high and CDCP1low. (E) A total of 1 × 106 cells were i.v. injected into NOD/SCID mice, CDCP1high cells formed more lung metastases than did CDCP1low cells. Box plots show numbers of lung surface tumors 5 wk after tail-vein injection. (F) Four different cell lines isolated from lung metastases from mice injected with CDCP1high (thin lines) maintain higher CDCP1 expression levels equivalent to those of MA2 cells (thick line). Dotted lines: isotype controls.
Flow cytometric analysis of the parental A375 cells revealed two subpopulations (Fig. 1 A, C, and D). However, all cells derived from the rare lung metastases obtained after i.v. injection of A375 cells in NOD/SCID mice exhibited higher surface CDCP1 expression (Fig. S2), suggesting that CDCP1 might be a surface marker for cells with higher metastatic potential. Parental A375 cells were sorted on the basis of CDCP1 expression levels into CDCP1high and CDCP1low populations (Fig. 1D) and separately injected into NOD/SCID mice via the tail vein. Mice injected with CDCP1high cells harbor more lung metastases than do those injected with CDCP1low cells, supporting our hypothesis (Fig. 1E). Furthermore, cell lines were derived from lung tumor nodules from mice injected with CDCP1high cells and selected with neomycin to remove nontumor cells, and all those cell lines retained high surface CDCP1 expression (Fig. 1F). Our results are consistent with recent clinical data where expression levels of CDCP1 in renal cell carcinoma and lung adenocarcinoma were found to be significant predictors of disease-free survival in patients (33, 34).
CDCP1 Plays a Causal Role During Melanoma Metastasis but Has No Significant Effect on s.c. Tumor Growth.
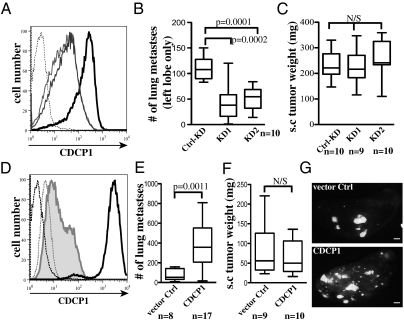
To test the functionality of CDCP1 in melanoma metastasis, we used reciprocal approaches. First, we generated two stable CDCP1-knockdown cell lines from highly metastatic MA2 cells (MA2-KD1 and MA2-KD2), using a miR30-based shRNA knockdown system (Fig. 2A). Down-regulation of CDCP1 had no effect on tumor cell proliferation in vitro (Fig. S3A). However, we found that MA2-KD1 and -KD2 formed significantly fewer lung metastases (mean = 42.8 ± 10.7 and 51.4 ± 7.3, and P = 0.0002 and 0.0001, respectively) compared with MA2-Ctrl-KD cells (mean = 110.8 ± 7.8) when tested by tail-vein injection assays (Fig. 2B). s.c. tumors derived from MA2-KD1 and MA2-KD2 cells reached the same size as those from MA2-Ctrl-KD cells (Fig. 2C), although these cells maintained lower CDCP1 expression levels at the time of tumor dissection (Fig. S3B). These results show that reduction of CDCP1 expression suppresses melanoma metastasis, without significant effects on primary tumor growth.
Fig. 2.
CDCP1 plays a functional role in melanoma metastasis without affecting primary tumor growth. (A) Flow-cytometric analysis shows down-regulation of surface CDCP1 in two cell lines (thin lines) relative to MA2 cells expressing control knockdown constructs (thick line). The dotted line represents isotype control of MA2 cells. (B) Box plots show that reduction of CDCP1 results in decreased numbers of metastases in NOD/SCID mice. Surface lung metastases on the left lobe were counted 5 wk after i.v. injection of 1 × 106 cells. (C) Box plots show that reduction of CDCP1 has no effect on tumor growth at a s.c. site 33 d after injecting 0.5 × 106 cells. (D) Flow-cytometric analysis shows overexpression of CDCP1 in A375 cells (thick line). The shaded curve shows A375 cells expressing a vector control. (E) Box plots show that overexpression of CDCP1 significantly enhanced lung metastases in NOD/SCID mice. Total numbers of surface lung metastases were counted 5 wk after i.v. injection. (F) Overexpression of CDCP1 in A375 cells does not affect s.c. tumor growth as shown by box plots. (G) Representative images of lungs from mice injected with control cells (Upper) or A375-CDCP1 cells (Lower). (Scale bar: 1 mm.)
Second, we overexpressed CDCP1 in poorly metastatic parental A375 cells (A375-CDCP1) (Fig. 2D) and tested the ability of these cells to form lung tumors in tail-vein injection assays relative to A375 cells expressing vector control (A375-Vector-Ctrl). A375-CDCP1 cells generated significantly more lung tumor nodules (mean = 375 ± 48.7) than did A375-Vector-Ctrl cells (mean = 74.9 ± 28.4, P = 0.0011; Fig. 2E) (representative images are shown in Fig. 2G). s.c. tumors derived from both cell types reached similar weights (Fig. 2F), although A375-CDCP1 cells do proliferate somewhat more slowly in vitro (Fig. S3C). Thus, both loss-of-function and gain-of-function experiments implicate CDCP1 as a causal agent in metastasis.
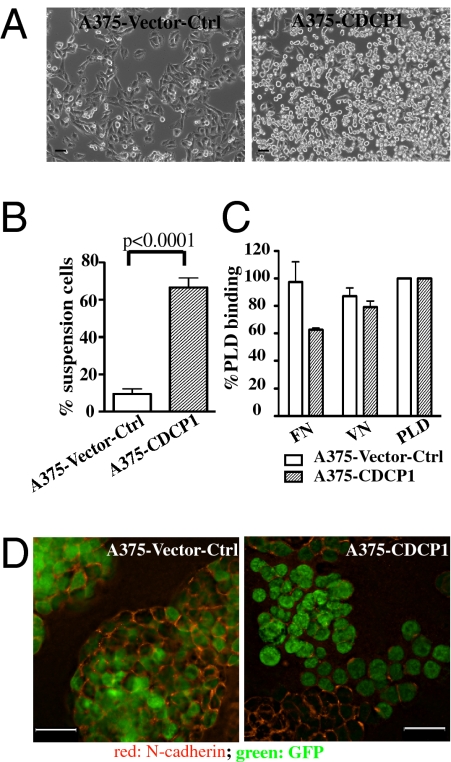
Overexpression of CDCP1 in Vitro Causes Reductions in Cell–Extracellular Matrix Adhesion and in Cell–Cell Adhesion.
When analyzing the in vitro phenotypes of A375-CDCP1 cells, we observed profound changes in cell morphology; whereas A375-Vector-Ctrl cells are adherent cells in culture (Fig. 3A, Left), overexpression of CDCP1 causes these cells to round up, detach, and proliferate as suspension cells (Fig. 3 A, Right and B for quantification). In agreement with this result, A375-CDCP1 cells showed significantly less adhesion to fibronectin compared with A375-Vector-Ctrl cells, although adhesion to vitronectin was not affected (Fig. 3C). In addition, when these cells were allowed to adhere to fibronectin or vitronectin for 1.5 h, most A375-CDCP1 cells completely failed to spread, showing no or minimum numbers of focal adhesions (Fig. S4A). Together, these results suggest that CDCP1 overexpression caused a reduction in cell–extracellular matrix adhesion and prevented cell spreading.
Fig. 3.
Overexpression of CDCP1 in A375 cells causes reduction of cell–substrate interactions and cell–cell interactions in vitro. (A) Images of A375-vector-Ctrl cells (Left) and A375-CDCP1 cells (Right) reveal loss of adherent phenotype when CDCP1 is overexpressed. (Scale bar: 30 μm.) (B) Quantification of the percentage of cells growing in suspension. Error bars represent SEM. (C) Adhesion to fibronectin is reduced, whereas adhesion to vitronectin is not significantly affected. Ninety-six-well plates were coated overnight with 10 μg/mL of fibronectin or vitronectin or with 20 μg/mL poly-d-lysine as positive control. Bars show cells adherent to the indicated substrate as percentage of the number adherent to poly-d-lysine. (D) A375-CDCP1 cells lose N-cadherin (red), whereas A375-vector-Ctrl cells retain strong N-cadherin staining at cell–cell junctions in 3D Matrigel assay. (Scale bar: 21 μm.)
Next, three-dimensional culture in Matrigel was applied to investigate the behavior of A375-Vector-Ctrl and A375-CDCP1 cells. Whereas A375-Vector-Ctrl cells formed “ball”-like structures with strong signal for N-cadherin (Fig. 3D, Left, red) and β-catenin (Fig. S4B, Left) at cell–cell junctions, A375-CDCP1 cells grew in a scattered manner, forming “clusters-of-grapes” with reduced N-cadherin staining at cell–cell junctions (Fig. 3D, Right, red) and mislocalized β-catenin (Fig. S4B, Right). Total expression levels of N-cadherin and β-catenin remained the same (Fig. S4A). Our data indicate that overexpression of CDCP1 resulted in mislocalization of cell–cell junction molecules and reduction of cell–cell adhesion in vitro.
To understand further the mechanisms by which CDCP1 functions to enhance metastasis, we used various in vitro assays to test its potential involvement in cell proliferation, apoptosis, migration, and invasion. We did not observe significant differences in cell migration when comparing MA2-Ctrl-KD to MA2-KD1 or KD2 cells using either scratch assay (Fig. S4D) or Boyden chamber migration assay, nor did we observe differences in Matrigel invasion assays using these cells. Using a soft-agar colony formation assay, we observed a slight reduction in the number of colonies formed by MA2-KD2 cells relative to MA2-Ctrl-KD cells (Fig. S4E), perhaps hinting that CDCP1 might be involved in anoikis resistance. This in vitro result was supported by investigating in vivo proliferation and apoptosis within the lung metastases. We performed immunohistological staining using anti-Ki67 antibody and ApopTag, respectively, and found a statistically significant but small reduction in the proliferation index between MA2-KD2 and MA2-Ctrl-KD (Fig. S5A) and a small increase in the percentage of cells undergoing apoptosis within the metastases when comparing MA2-KD1 and MA2-KD2 to MA2-Ctrl-KD (Fig. S5B). Consistent with these data, we observed a small reduction in the size of the lung metastases (Fig. S5C). We also analyzed apoptosis under adhesion-free conditions by coating tissue-culture plates with poly 2-hydroxyethyl methacrylate (polyHEMA). However, we did not observe significant differences in percentages of cells undergoing apoptosis under the conditions we tested.
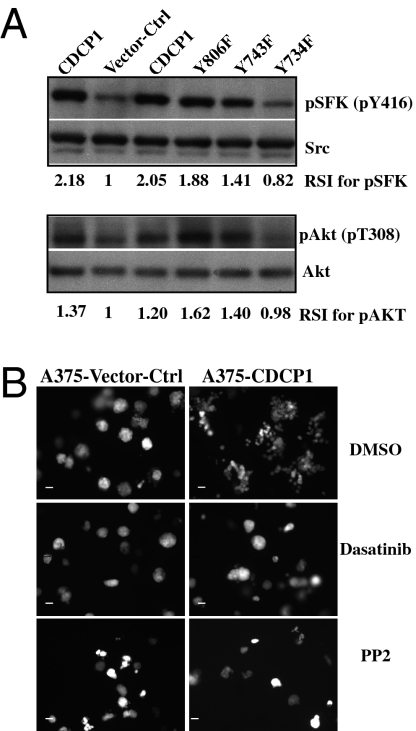
CDCP1 Functions Through Activation of Src Family Kinases to Exert Its Biological Effects.
Next, we wished to elucidate the signaling pathway(s) activated by CDCP1 that might contribute to enhancement of tumor metastasis. Western blotting using a series of activation status-specific antibodies revealed that overexpression of CDCP1 in A375 cells enhanced the activation of Src-family kinases (SFKs) relative to A375-Vector-Ctrl cells (Fig. 4A). Next we examined the subcellular localization of Src and activated SFKs. In control cells, both Src and activated SFKs are located both in the cytoplasm and at the cell membrane. However, for CDCP1-overexpressing cells, although Src is localized both in the cytosol and in the membrane, pSFK is almost exclusively localized at the cell membrane, particularly at cell–cell junctions (Fig. S6). We also found that Akt activation was enhanced in A375-CDCP1 cells compared with Vector-Ctrl cells (Fig. 4A), although the activation status of p44/p42 MAPK (ERK1/2) and FAK was not affected (Fig. S7B). Neither the PI3K inhibitor wortmannin nor an Akt inhibitor treatment affected the growth pattern of A375-CDCP1 cells (Fig. S7C), suggesting that enhanced activation of Akt may not be directly involved in the dispersive growth observed in these cells. However, when inhibitors against SFK activation were used in 3D Matrigel culture, we found that both PP2 (at 2 μM) and Dasatinib (at 2 μM) inhibited the dispersive growth of A375-CDCP1 cells, whereas PP3 (at 2 μM) or DMSO had no effect on the growth pattern of these cells (Fig. 4B). These results suggested that activation of SFKs may function downstream of CDCP1, to promote scattered growth of tumor cells in 3D Matrigel.
Fig. 4.
Overexpression of CDCP1 enhances Src family kinase activity. (A) Western blotting using antibodies specific for activated forms of SFKs or Akt shows that CDCP1 overexpression in A375 cells enhances activation of SFKs and Akt. A point mutation at Y734F in CDCP1 abolished this enhancement, whereas mutations at Y743F and Y806F had no effect. Relative signal intensities (RSI) for pSFK and pAKT are indicated. (B) Treatment with Src-family kinase inhibitor, Dasatinib, abolished scattered growth of A375-CDCP1 cells in 3D Matrigel and was imaged 6 d later. (Scale bar: 30 μm.)
We further tested the hypothesis that CDCP1 functions through activation of SFKs. The cytoplasmic domain of CDCP1 contains five tyrosines, which have been reported to be phosphorylated by SFKs. In particular, Y734 has been reported to serve as a docking site for SFKs (29, 35). Therefore, we performed site-directed mutagenesis to obtain tyrosine-to-phenylalanine mutant forms of CDCP1 and generated stable A375 cell lines expressing each of these mutants (A375-Y734F, A375-Y743F, A375-Y762F, and A375-Y806F). Surface expression levels of these mutants and wild-type CDCP1 were similar (Fig. S8). Cells overexpressing the Y743F or Y806F mutant forms of CDCP1 have strong activation of SFKs and Akt, similar to the activation levels in cells overexpressing wild-type CDCP1 (Fig. 4A). However, cells overexpressing the Y734F mutant CDCP1 failed to elicit strong SFK and Akt activation (Fig. 4A). Therefore, this tyrosine residue appears to play a key role in the signaling functions of CDCP1.
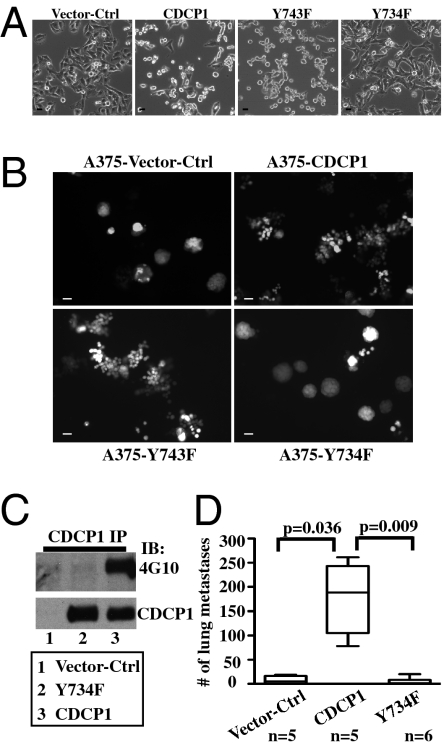
Mutants causing strong activation of SFKs and Akt (Y743F, Y762F, and Y806F) retained the functions of CDCP1 in vitro, inducing both cell–substrate detachment in 2D culture (Fig. 5A and Fig. S8B) and dispersive growth in 3D Matrigel (Fig. 5B and Fig. S8C). However, the Y734F mutant of CDCP1 that failed to activate SFKs and Akt completely lacked the functions of CDCP1 in these in vitro assays. A375 cells overexpressing Y734F-CDCP1 were adherent in 2D culture (Fig. 5A) and remained as balls in 3D Matrigel (Fig. 5B). Mutation of Y734F also abolished tyrosine phosphorylation of CDCP1 (Fig. 5C and Fig. S7A). When tested for tail-vein metastasis, A375-Y734F cells failed to promote metastasis in the lungs (Fig. 5D). Together, these data indicate that many of the functions of CDCP1 depend on Y734, possibly functioning through activation of SFKs to exert its biological functions both in vitro and in vivo.
Fig. 5.
Point mutation in CDCP1 (Y734F) abolishes the effects of CDCP1 both in vitro and in vivo. (A) In 2D culture, overexpression of CDCP1, Y743F, or Y806F mutant forms causes cell detachment, but the Y734F mutant form does not. A375 cells were plated on six-well plates and infected with virus containing various CDCP1 cDNAs and imaged 48 h later. (Scale bar: 30 μm.) (B) Whereas A375-vector-Ctrl cells grow as ball-like structures in 3D Matrigel assay, overexpression of CDCP1 (A375-CDCP1) induced scattered growth. Mutation of CDCP1(Y734F) abolished this scattered growth pattern; however, other point mutations (shown here for Y743F and also true for Y806F and Y762F) had no effect. (Scale bar: 30 μm.) (C) CDCP1(Y734F) was not phosphorylated on tyrosines. Equal numbers of cells from each cell line were lysed in 1% Triton lysis buffer and immunoprecipitated with 1 μg of rabbit IgG or anti-CDCP1 antibody followed by agarose-conjugated anti-rabbit IgG. Membranes were blotted with either 4G10 antityrosine phosphate antibody (Upper) or anti-CDCP1 antibody (Lower). (D) Box plots show that the Y734F point mutation abolished the metastasis-enhancing activity of CDCP1 in vivo in an experimental metastasis assay.
Discussion
Using a quantitative proteomics approach, we showed that the expression level of a transmembrane protein, CDCP1, is elevated in a series of highly metastatic human melanoma cells relative to their poorly metastatic counterparts. We also investigated the functional involvement of CDCP1 during melanoma metastasis, using both shRNA-mediated down-regulation and overexpression of CDCP1. We find that CDCP1 plays important roles in enhancing tumor metastasis in our experimental model, without affecting tumor growth at s.c. sites. Furthermore, we show that a single tyrosine residue, Y734, known to bind Src and other SFKs, is essential for the prometastatic effects of CDCP1, as well as for a variety of in vitro phenotypes induced by overexpression of CDCP1. Y734 is essential for activation of Src and Akt and additional experiments showed that inhibition of SFKs blocks the phenotypic consequences of overexpression of CDCP1, suggesting that CDCP1 functions via activation of Src and possibly other SFKs. Using antibodies specific for Src, Fyn, and Yes we found that Src is the major SFK in A375 cells; Fyn and Yes were barely detectable.
CDCP1 has been reported to be overexpressed in other metastatic cell lines (27) and in hematopoietic and mesenchymal stem cells (31, 32). Elevated expression of CDCP1 correlates with poor prognosis in renal cell carcinoma (33) and adenocarcinoma of the lung (34). These results and ours suggest broad implications of CDCP1 overexpression for malignancy. In agreement with our results, it has been shown that shRNA suppression of CDCP1 can inhibit experimental metastasis of A549 lung adenocarcinoma cells and i.p. dissemination of scirrhous gastric carcinoma cell lines (36, 37). It was recently reported that overexpression of CDCP1 in HeLa or PC3 cells enhanced metastasis and that antibodies to CDCP1 suppress metastasis in mouse and chicken models, again in agreement with our data (38).
There is fairly general agreement that overexpression of CDCP1 correlates with reduced cell adhesion (28–30, 36–39). However, there is divergence of results concerning the effects of CDCP1 on anoikis resistance. Uekita et al. (36) report that overexpression of CDCP1 and its association with Src protects lung adenocarcinoma cells against apoptosis and anchorage dependence of growth. However, both we and Deryugina et al. (38) found relatively small effects on anoikis and growth in soft agar. In melanoma cells, this might be due to formation of large spheroidal cell aggregates, which has been shown to enhance cell survival via cell–cell contacts and localized secretion of ECM proteins (40–42). Nevertheless, on the basis of several hints from our results including i) a small reduction in soft agar formation ability when CDCP1 expression is reduced (Fig. S4D) without affecting proliferation (Fig. S3A) and ii) an adhesion-to-suspension transition when cells overexpress CDCP1 (Fig. 3A), we speculate that this aspect of CDCP1 function may play some role in enhancing metastasis. In addition, it was reported that CDCP1 could protect from apoptosis in HeLa cells doubly challenged by loss of adhesion and by doxorubicin but not those challenged by either one alone; and there was some evidence for apoptosis of metastatic cells inhibited by anti-CDCP1, suggesting that CDCP1 may confer some level of apoptosis resistance in stress conditions (38). Uekita et al. reported strong enhancement of migration of gastric scirrhous carcinoma cells in vitro by CDCP1 (37) but we saw little effect on migration of melanoma cells in standard migration assays (Boyden chamber with or without Matrigel, scratch wounds). However, we did observe dispersive growth in 3D cultures in Matrigel, accompanied by markedly reduced cell–cell adhesion and enhanced migration of the dissociated cells. This pattern of dispersion showed some similarities with the pattern of extravasation in vivo observed by Deryugina et al. and shown to be inhibited by anti-CDCP1 antibodies (38). These data suggest that effects of CDCP1 on cellular dispersion may play important roles in its ability to enhance metastasis. We speculate that the subtle effect on apoptosis resistance and this dispersive growth together contribute to the enhancement of metastases by CDCP1-overexpressing cells.
These phenotypic consequences of overexpression of CDCP1 in cell culture correlate well with the ability of CDCP1 and various mutant forms to enhance metastasis. Importantly, they also correlate well with the activation of Src (Fig. 4A) and the phosphorylation of CDCP1 and all these effects are abolished by mutation of Y734. Together with the inhibition of the dispersive growth phenotype by SFK family inhibitors (Fig. 4B), these results indicate that activation of Src (and possibly other SFKs) by CDCP1 is essential for its ability to enhance metastasis. The Y734F mutant form of CDCP1 also failed to confer anoikis resistance in lung adenocarcinoma cells and failed to promote gastric cancer cell migration (36, 37). However, in direct conflict with our data, Deryugina et al. (38) reported that the Y734F mutation somewhat enhanced metastasis, even though it was not phosphorylated on tyrosines. Deryugina et al. concluded that phosphorylation of this tyrosine is not required for CDCP-enhanced metastasis (38). We cannot at this point explain this discrepancy, although it appears that HeLa cells do not express endogenous CDCP1 whereas other cell types do, and Y734F has been suggested to have a dominant-negative effect (36). It is also possible that CDCP1 may have differing effects in different cell types and, indeed, there are clear differences among reports on the effects of CDCP1 on cellular phenotypes in vitro.
Y734 was previously identified as a critical residue mediating interaction of SFKs with CDCP1 (35) and other studies have shown that CDCP1 is tyrosine phosphorylated by SFKs (28, 29, 36). Phosphorylation of CDCP1 is required for the formation of CDCP1-SFK-PKCδ signaling complexes (35). We find that, although wild-type CDCP1 is tyrosine phosphorylated, the Y734F mutant has no detectable tyrosine phosphorylation (Fig. 5C) as also reported by others (36, 38). We propose a “feed-forward” loop between SFKs and CDCP1, where initial activity by SFKs is important for phosphorylation of CDCP1, which in turn further enhances activation of SFKs. However, the mechanism by which CDCP1 activates SFKs is not clear. Phosphorylation-dependent interaction between CDCP1 and SFKs has been reported (35), suggesting that CDCP1 may act as an adaptor protein to recruit SFKs and to modulate their activity. However, we could not reproducibly detect decreased interaction between CDCP1 and Src in cells expressing Y734F mutants compared with those expressing wild-type CDCP1, suggesting perhaps an indirect mechanism of CDCP1-induced Src activation.
PKCδ has been reported to interact with CDCP1 via Y762 in a phosphotyrosine-dependent manner (35) and to be important for anoikis resistance (36). However, in A375 cells, the Y762F mutation showed no altered effects on the behavior of the cells either in 2D or in 3D cultures (Fig. S8). Furthermore, knocking down PKCδ in A375-CDCP1 cells did not affect scattered growth of these cells relative to A375-CDCP1 cells harboring control shRNA. Therefore, in our system, we do not have evidence that PKCδ is critical for the functions of CDCP1 that we observed. We also report that overexpression of CDCP1 enhances Akt activation. However, direct tests of Akt function using inhibitors of PI3K and Akt (Fig. 4B) suggest that enhanced activation of Akt may not be involved in scattered growth of A375-CDCP1 cells in Matrigel. Because of the strong correlation between the cellular behaviors in 3D culture in vitro and metastasis potential in vivo in our system, we think that Akt is less likely to contribute to CDCP1-mediated metastasis-enhancing function, although an in vivo metastasis assay using A375-CDCP1 cells harboring shRNA targeting Akt is required for conclusive assessment of this possibility.
Thus, although the involvement of PKCδ and Akt in the functions of CDCP1 remains somewhat unclear, our data demonstrate a key requirement for CDCP1-mediated activation of Src (and perhaps other SFKs) in the functions of CDCP1 in altered cell–cell and cell–substratum adhesion in vitro and in metastasis in vivo. Numerous studies have shown important and diverse contributions of SFKs to tumor formation, progression, and metastasis (43–45). SFK activation is known to reduce cell–cell and cell–extracellular matrix adhesion and enhance cell migration (46–48) and activate anoikis-resistance pathways (49), among other mechanisms. These effects are all consistent with the effects of CDCP1, reinforcing the hypothesis that it functions through activation of SFKs.
Materials and Methods
For details, see SI Materials and Methods.
s.c. Tumor Growth.
A375-CDCP1 or A375-Vector-Ctrl cells were harvested, washed, and treated with PBS/EDTA and resuspended in HBSS. Eight- to 10-wk-old nonobese diabetic severe combined immunodeficient (NOD/SCID) mice (Jackson Laboratories) were anesthetized with isoflurane/O2 mixture (Abbott Laboratories). A total of 0.5 × 106 cells were injected s.c. using a 26G needle. Thirty-three days later, mice were killed and tumors dissected and weighed.
Experimental Metastasis Assay.
Six- to 8-wk-old NOD/SCID mice were injected via the lateral tail veins with 1 × 106 cells, using a 30G needle. Thirty-five days later, mice were killed and lungs were inflated with 4% formalin in PBS, tied, and fixed for 5 min. Lungs were dissected and placed in ice-cold PBS and green fluorescent tumors were counted under a UV dissection microscope. All animal experiments were approved by the MIT Department of Comparative Medicine.
Graphs and Statistical Analysis.
P values were calculated using Student's t test (http://www.physics.csbsju.edu/stats/). Box plots were generated by Prizm software (GraphPad Software). The box plots show the interquartile range (middle 50% of data), with the median marked by a line, and the whiskers represent the full range of the data.
Supplementary Material
Acknowledgments
We thank Lei Xu, Arjan van der Flier, Kaan Cartel, Richard Cook, Alla Leshinsky, Shahin Begum, and Denise Crowley for experimental advice and assistance and Drs. Stolz, Stern, Sakai, and Benes for reagents. We thank Drs. Lamar, Labelle, and van der Flier for critical reading of the manuscript. This work was supported by the National Institutes of Health (U54-CA112967 and U54-CA126515), the Ludwig Center at MIT, a National Institute of General Medical Sciences Training grant to the MIT Biology Department, a fellowship from the David H. Koch Fund, and the Howard Hughes Medical Institute.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1017228108/-/DCSupplemental.
References
- 1.Gupta GP, Massagué J. Cancer metastasis: Building a framework. Cell. 2006;127:679–695. doi: 10.1016/j.cell.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Hynes RO. Metastatic potential: Generic predisposition of the primary tumor or rare, metastatic variants-or both? Cell. 2003;113:821–823. doi: 10.1016/s0092-8674(03)00468-9. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen DX, Bos PD, Massagué J. Metastasis: From dissemination to organ-specific colonization. Nat Rev Cancer. 2009;9:274–284. doi: 10.1038/nrc2622. [DOI] [PubMed] [Google Scholar]
- 4.Weiss L. Metastasis of cancer: A conceptual history from antiquity to the 1990s. Cancer Metastasis Rev. 2000;19:I–XI, 193–383. [PubMed] [Google Scholar]
- 5.Bissell MJ, Radisky D. Putting tumours in context. Nat Rev Cancer. 2001;1:46–54. doi: 10.1038/35094059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Condeelis J, Pollard JW. Macrophages: Obligate partners for tumor cell migration, invasion, and metastasis. Cell. 2006;124:263–266. doi: 10.1016/j.cell.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Joyce JA, Pollard JW. Microenvironmental regulation of metastasis. Nat Rev Cancer. 2009;9:239–252. doi: 10.1038/nrc2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clark EA, Golub TR, Lander ES, Hynes RO. Genomic analysis of metastasis reveals an essential role for RhoC. Nature. 2000;406:532–535. doi: 10.1038/35020106. [DOI] [PubMed] [Google Scholar]
- 9.Kang Y, et al. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell. 2003;3:537–549. doi: 10.1016/s1535-6108(03)00132-6. [DOI] [PubMed] [Google Scholar]
- 10.Müller A, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- 11.Yang J, et al. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell. 2004;117:927–939. doi: 10.1016/j.cell.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Dong JT, et al. KAI1, a metastasis suppressor gene for prostate cancer on human chromosome 11p11.2. Science. 1995;268:884–886. doi: 10.1126/science.7754374. [DOI] [PubMed] [Google Scholar]
- 13.Wong SY, et al. Protein 4.1B suppresses prostate cancer progression and metastasis. Proc Natl Acad Sci USA. 2007;104:12784–12789. doi: 10.1073/pnas.0705499104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu L, Begum S, Hearn JD, Hynes RO. GPR56, an atypical G protein-coupled receptor, binds tissue transglutaminase, TG2, and inhibits melanoma tumor growth and metastasis. Proc Natl Acad Sci USA. 2006;103:9023–9028. doi: 10.1073/pnas.0602681103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bandyopadhyay S, et al. Interaction of KAI1 on tumor cells with DARC on vascular endothelium leads to metastasis suppression. Nat Med. 2006;12:933–938. doi: 10.1038/nm1444. [DOI] [PubMed] [Google Scholar]
- 16.Visvader JE, Lindeman GJ. Cancer stem cells in solid tumours: Accumulating evidence and unresolved questions. Nat Rev Cancer. 2008;8:755–768. doi: 10.1038/nrc2499. [DOI] [PubMed] [Google Scholar]
- 17.Vaught D, Brantley-Sieders DM, Chen J. Eph receptors in breast cancer: Roles in tumor promotion and tumor suppression. Breast Cancer Res. 2008;10:217. doi: 10.1186/bcr2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Felding-Habermann B, et al. Integrin activation controls metastasis in human breast cancer. Proc Natl Acad Sci USA. 2001;98:1853–1858. doi: 10.1073/pnas.98.4.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li X, et al. Integrin alphavbeta3 mediates K1735 murine melanoma cell motility in vivo and in vitro. J Cell Sci. 2001;114:2665–2672. doi: 10.1242/jcs.114.14.2665. [DOI] [PubMed] [Google Scholar]
- 20.Pécheur I, et al. Integrin alpha(v)beta3 expression confers on tumor cells a greater propensity to metastasize to bone. FASEB J. 2002;16:1266–1268. doi: 10.1096/fj.01-0911fje. [DOI] [PubMed] [Google Scholar]
- 21.Hill A, McFarlane S, Johnston PG, Waugh DJ. The emerging role of CD44 in regulating skeletal micrometastasis. Cancer Lett. 2006;237:1–9. doi: 10.1016/j.canlet.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 22.Kozyraki R, et al. The intrinsic factor-vitamin B12 receptor, cubilin, is a high-affinity apolipoprotein A-I receptor facilitating endocytosis of high-density lipoprotein. Nat Med. 1999;5:656–661. doi: 10.1038/9504. [DOI] [PubMed] [Google Scholar]
- 23.Tu CF, et al. Domain and functional analysis of a novel platelet-endothelial cell surface protein, SCUBE1. J Biol Chem. 2008;283:12478–12488. doi: 10.1074/jbc.M705872200. [DOI] [PubMed] [Google Scholar]
- 24.Töpfer-Petersen E, Ekhlasi-Hundrieser M, Tsolova M. Glycobiology of fertilization in the pig. Int J Dev Biol. 2008;52:717–736. doi: 10.1387/ijdb.072536et. [DOI] [PubMed] [Google Scholar]
- 25.Perry SE, et al. Expression of the CUB domain containing protein 1 (CDCP1) gene in colorectal tumour cells. FEBS Lett. 2007;581:1137–1142. doi: 10.1016/j.febslet.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 26.Scherl-Mostageer M, et al. Identification of a novel gene, CDCP1, overexpressed in human colorectal cancer. Oncogene. 2001;20:4402–4408. doi: 10.1038/sj.onc.1204566. [DOI] [PubMed] [Google Scholar]
- 27.Hooper JD, et al. Subtractive immunization using highly metastatic human tumor cells identifies SIMA135/CDCP1, a 135 kDa cell surface phosphorylated glycoprotein antigen. Oncogene. 2003;22:1783–1794. doi: 10.1038/sj.onc.1206220. [DOI] [PubMed] [Google Scholar]
- 28.Brown TA, et al. Adhesion or plasmin regulates tyrosine phosphorylation of a novel membrane glycoprotein p80/gp140/CUB domain-containing protein 1 in epithelia. J Biol Chem. 2004;279:14772–14783. doi: 10.1074/jbc.M309678200. [DOI] [PubMed] [Google Scholar]
- 29.Bhatt AS, Erdjument-Bromage H, Tempst P, Craik CS, Moasser MM. Adhesion signaling by a novel mitotic substrate of src kinases. Oncogene. 2005;24:5333–5343. doi: 10.1038/sj.onc.1208582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xia Y, Gil SG, Carter WG. Anchorage mediated by integrin alpha6beta4 to laminin 5 (epiligrin) regulates tyrosine phosphorylation of a membrane-associated 80-kD protein. J Cell Biol. 1996;132:727–740. doi: 10.1083/jcb.132.4.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bühring HJ, et al. CDCP1 identifies a broad spectrum of normal and malignant stem/progenitor cell subsets of hematopoietic and nonhematopoietic origin. Stem Cells. 2004;22:334–343. doi: 10.1634/stemcells.22-3-334. [DOI] [PubMed] [Google Scholar]
- 32.Conze T, et al. CDCP1 is a novel marker for hematopoietic stem cells. Ann N Y Acad Sci. 2003;996:222–226. doi: 10.1111/j.1749-6632.2003.tb03249.x. [DOI] [PubMed] [Google Scholar]
- 33.Awakura Y, et al. Microarray-based identification of CUB-domain containing protein 1 as a potential prognostic marker in conventional renal cell carcinoma. J Cancer Res Clin Oncol. 2008;134:1363–1369. doi: 10.1007/s00432-008-0412-4. [DOI] [PubMed] [Google Scholar]
- 34.Ikeda J, et al. Expression of CUB domain containing protein (CDCP1) is correlated with prognosis and survival of patients with adenocarcinoma of lung. Cancer Sci. 2009;100:429–433. doi: 10.1111/j.1349-7006.2008.01066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benes CH, et al. The C2 domain of PKCdelta is a phosphotyrosine binding domain. Cell. 2005;121:271–280. doi: 10.1016/j.cell.2005.02.019. [DOI] [PubMed] [Google Scholar]
- 36.Uekita T, et al. CUB domain-containing protein 1 is a novel regulator of anoikis resistance in lung adenocarcinoma. Mol Cell Biol. 2007;27:7649–7660. doi: 10.1128/MCB.01246-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uekita T, et al. CUB-domain-containing protein 1 regulates peritoneal dissemination of gastric scirrhous carcinoma. Am J Pathol. 2008;172:1729–1739. doi: 10.2353/ajpath.2008.070981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deryugina EI, et al. Functional role of cell surface CUB domain-containing protein 1 in tumor cell dissemination. Mol Cancer Res. 2009;7:1197–1211. doi: 10.1158/1541-7786.MCR-09-0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spassov DS, Baehner FL, Wong CH, McDonough S, Moasser MM. The transmembrane src substrate Trask is an epithelial protein that signals during anchorage deprivation. Am J Pathol. 2009;174:1756–1765. doi: 10.2353/ajpath.2009.080890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tzukert K, et al. A novel dynamic matrix detachment model reveals a shift from apoptosis to necrosis in melanoma cells. Cancer Lett. 2008;272:345–354. doi: 10.1016/j.canlet.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 41.Zhang Y, Lu H, Dazin P, Kapila Y. Squamous cell carcinoma cell aggregates escape suspension-induced, p53-mediated anoikis: Fibronectin and integrin alphav mediate survival signals through focal adhesion kinase. J Biol Chem. 2004;279:48342–48349. doi: 10.1074/jbc.M407953200. [DOI] [PubMed] [Google Scholar]
- 42.Shimony N, et al. A 3D rotary renal and mesenchymal stem cell culture model unveils cell death mechanisms induced by matrix deficiency and low shear stress. Nephrol Dial Transplant. 2008;23:2071–2080. doi: 10.1093/ndt/gfn062. [DOI] [PubMed] [Google Scholar]
- 43.Ishizawar R, Parsons SJ. c-Src and cooperating partners in human cancer. Cancer Cell. 2004;6:209–214. doi: 10.1016/j.ccr.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 44.Summy JM, Gallick GE. Src family kinases in tumor progression and metastasis. Cancer Metastasis Rev. 2003;22:337–358. doi: 10.1023/a:1023772912750. [DOI] [PubMed] [Google Scholar]
- 45.Yeatman TJ. A renaissance for SRC. Nat Rev Cancer. 2004;4:470–480. doi: 10.1038/nrc1366. [DOI] [PubMed] [Google Scholar]
- 46.Abram CL, Courtneidge SA. Src family tyrosine kinases and growth factor signaling. Exp Cell Res. 2000;254:1–13. doi: 10.1006/excr.1999.4732. [DOI] [PubMed] [Google Scholar]
- 47.Hynes RO. Integrins: Versatility, modulation, and signaling in cell adhesion. Cell. 1992;69:11–25. doi: 10.1016/0092-8674(92)90115-s. [DOI] [PubMed] [Google Scholar]
- 48.Thomas SM, Brugge JS. Cellular functions regulated by Src family kinases. Annu Rev Cell Dev Biol. 1997;13:513–609. doi: 10.1146/annurev.cellbio.13.1.513. [DOI] [PubMed] [Google Scholar]
- 49.Windham TC, et al. Src activation regulates anoikis in human colon tumor cell lines. Oncogene. 2002;21:7797–7807. doi: 10.1038/sj.onc.1205989. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.