Abstract
Chronic graft-versus-host disease (cGVHD) may mimic clinical and serological features of various autoimmune diseases. We present a case of a 23-year-old man who developed vitiligo, symmetric polyarthritis, high titre rheumatoid factor, antinuclear antibodies and anti-double stranded DNA antibodies after allogenic peripheral blood stem cell transplantation for severe aplastic anaemia. He was treated with low dose oral steroids, non-steroid anti-inflammatory drugs and azathioprine and clinical improvement of polyarthritis were observed initially. However, atlantoaxial subluxation (C1-C2) and rapid progression of symmetrical joint space narrowing in knees and wrists developed within 1 year. cGVHD mimicking rheumatoid arthritis with unusual presentations was observed in this patient.
BACKGROUND
Chronic graft-versus-host disease (cGVHD) is a multisystem alloimmune disorder mimicking autoimmune diseases such as scleroderma, Sjögren’s syndrome (SjS), polymyositis, primary biliary cirrhosis, rheumatoid arthritis (RA), and systemic lupus erythematosus (SLE).1–3 It represents a major cause of morbidity and mortality after allogenic haematopoietic stem cell transplantation (allo-HSCT).
CASE PRESENTATION
This case involves a 23-year-old man with severe aplastic anaemia (SAA) and diffuse toxic goitre. The initial presentations included pallor, exertional dyspnoea, leucopenia (white blood cell count 2,600/mm3) and anaemia (haemoglobin 4.6g/d). He had no family history of similar diseases, hereditary diseases or other autoimmune diseases. There were no thymoma, myasthenia gravis, Grave’s disease, virus infections or other autoimmune diseases. A bone marrow biopsy disclosed generalised hypocellularity. The hyperthyroidism was treated with methimazole. Prednisolone, cyclosporine A (CsA) and azathioprine were prescribed for SAA but were ineffective. Several months later, he received allogenic peripheral blood stem cell transplantation (allo-PBSCT) from a healthy HLA identical sibling donor, his 10-year-old younger sister, after undergoing conditioning chemotherapy with cyclophosphamide. GVHD prophylaxis was performed with methotrexate and CsA. A follow-up bone marrow biopsy revealed SAA in complete remission with full donor engraftment. However, persistent elevation of liver enzymes without evidence of concomitant drug induced hepatitis or infection occurred 4 months after allo-PBSCT. Thus, cGVHD with liver involvement was diagnosed. Add-on prednisolone and CsA resulted in gradual normalisation of the liver enzymes. There were no further events except for an episode of herpes zoster infection in the following year. Two years after PBSCT, generalised vitiligo (fig 1) appeared on the face, trunk and extremities, for which the patient was reluctant to undergo ultraviolet phototherapy, although topical steroid treatment prescribed later was also ineffective. Arthritis of the bilateral wrist, proximal interphalangeal, metacarpophalangeal, knee and ankle joints developed and were sustained for more than 6 weeks until late into the fourth year following allo-PBSCT. Laboratory investigations showed normal haemograms and serum biochemistry, elevated IgG (2500 mg/dl), high erythrocyte sedimentation rate (ESR, 136 mm/h) and C reactive protein (CRP, 20.0 mg/dl). Autoantibody profile showed high rheumatoid factor (RF) (2200 IU/ml), antinuclear antibodies (Abs) (ANA, 1:320, homogenous) and anti-dsDNA Abs (84 IU/ml). Abs to Sm/RNP, SS-A/SS-B, Scl-70, cyclic citrullinated peptide (CCP), mitochondrion (AMA), smooth muscle (ASMA), thyroid stimulating hormone receptor, thyroglobulin, and thyroxin peroxidase were not detected. Complement components C3/C4 levels were normal and thyroid function tests showed euthyroidism. A magnetic resonance (MR) scan of the hands revealed marrow oedema in the carpal bones and active synovitis in the wrists and hands, but not bony erosions. A plain film failed to show joint space narrowing or bony erosion in the knees. Arthrocentesis from the knees yielded yellowish non-purulent inflammatory effusion. Microbial investigations failed to show hepatitis B virus, hepatitis C virus, cytomegalovirus or other traceable infectious foci. Hence, low dose prednisolone, azathioprine and non-steroidal anti-inflammatory drugs (NSAIDs) were given for suspected cGVHD resembling autoimmune diseases. These were very effective, and rapid clinical remission with a dramatic decrease in acute phase reactants as well as RF titre were soon observed.
Figure 1.
Generalised vitiligo developed 2 years after allogenic peripheral blood stem cell transplantation.
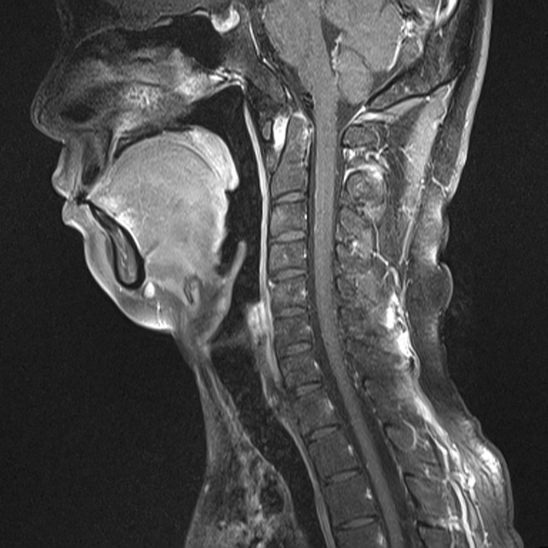
In the subsequent year, rapid progressive knee soreness and spastic gait developed. Another MR scan disclosed pannus formation in cervical spines associated with C1-C2 subluxation (fig 2). Radiographs showed symmetrical joint space narrowing in the wrists and knees, and avascular necrosis of the hip joints. With these features, a diagnosis of cGVHD resembling rapidly progressive RA was made.
Figure 2.
Sagittal contrast enhanced T1 weighted magnetic resonance image of the C spine revealing pannus formation with C1-C2 subluxation.
DISCUSSION
Autoimmunity following haematopoietic stem cell transplantation (HSCT) is protean, including appearance of autoantibodies (autoAbs), homeostatic expansion of T cells with acquired lymphopenia, transference of autoimmunity from donor to recipient, and altered immunity associated with GVHD. The actual pathophysiological mechanism has not been fully elucidated. Alloreactive T cells, regulatory T cells, B cells, autoAbs and cytokines are implicated. Conditioning chemotherapy and host factors also influence its occurrence.2–4 The most frequent autoAbs appearing in cGVHD are ANA (up to 63%)5,6 and AMA.7 Anti-dsDNA and anti-cardiolipin Abs as detected in our patient are much less common. However, these autoAbs or their titres may not correlate with the clinically observed autoimmune symptoms and severity of cGVHD.6,8 In this patient, despite persistent ANA and anti-dsDNA Abs suggestive of lupus, there were no clinical symptoms or signs specific for SLE. He presented initially with typical clinical and early radiological evidence of RA as well as high titre RF in the absence of anti-CCP Ab. Rapid development of C1-C2 subluxation with bilateral wrist and knee joint destruction were unusual and rarely seen in early RA. When polyarthritis develops in allo-HSCT patients, infection, connective tissue disease, RA or GVHD should be differentiated.2 In view of the chronological appearance of symptoms including previous cGVHD with liver damage, newly developed vitiligo, and epiphenomenal serological features of SLE, we think cGVHD mimicking rapid progressive RA is more likely than a de novo development of autoimmune diseases. In contrast to other rheumatic diseases such as SjS, polymyositis or scleroderma, cGVHD simulating RA is less frequently reported.9–11 Interestingly, pre-PBSCT human leucocyte antigen (HLA) typing of the donor and the patient revealed the presence of HLA-DRβ1*04, which was well recognised as a genetic risk of RA. However, there was no evidence for autoimmunity transference from the donor to the recipient.
Among the skin lesions developing after HSCT, lichenoid and sclerodermoid changes are most frequently encountered in cGVHD.11 Vitiligo is uncommon after HSCT. Immune derangement in cGVHD might be a contributing factor to initiate the depigmentation, in which cytotoxic T cells recognise and destroy melanocytes.12 A similar mechanism might have driven polyarthritis development in this patient. Vitiligo is well known to accompany a variety of autoimmune diseases, including Grave’s disease and Hashimoto’s thyroiditis. The patient has a history of hyperthyroidism led by diffuse toxic goitre, which remitted completely after short term methimazole treatment. Therefore, vitiligo as a unique presentation after allo-PBSCT in this particular patient might have been another autoimmune manifestation of cGVHD.
In conclusion, a constellation of vitiligo, polyarthritis with C1-C2 subluxation, high RF and lupus specific autoAbs occurring after allo-PBSCT in a young man was attributed to cGVHD with autoimmune mimics. These unique features may highlight the importance of careful differential diagnosis and proper immunosuppressant therapy in this kind of patient.
LEARNING POINTS
Chronic graft-versus-host disease (cGVHD) may mimic various autoimmune diseases, in which rheumatoid arthritis with complicated C1-C2 subluxation is unusual.
When this occurs, careful differential diagnosis and proper immunosuppressant therapy are necessary.
Vitiligo, though uncommon, is an autoimmune phenomenon after haematopoietic stem cell transplantation.
Long term observation to see if full blown lupus or any major organ involvement of the lupus disease is necessary in cGVHD mimicking lupus.
Footnotes
Competing interests: none.
Patient consent: Patient/guardian consent was obtained for publication
REFERENCES
- 1.Baird K, Pavletic SZ. Chronic graft versus host disease. Curr Opin Hematol 2006; 13: 426–35 [DOI] [PubMed] [Google Scholar]
- 2.Daikeler T, Tyndall A. Autoimmunity following haematopoietic stem-cell transplantation. Best Pract Res Clin Haematol 2007; 20: 349–60 [DOI] [PubMed] [Google Scholar]
- 3.Tyndall A, Dazzi F. Chronic GVHD as an autoimmune disease. Best Pract Res Clin Haematol 2008; 21: 281–9 [DOI] [PubMed] [Google Scholar]
- 4.Snowden JA, Atkinson K, Kearney P, et al. Allogeneic bone marrow transplantation from a donor with severe active rheumatoid arthritis not resulting in adoptive transfer of disease to recipient. Bone Marrow Transplant 1997; 20: 71–3 [DOI] [PubMed] [Google Scholar]
- 5.Kier P, Penner E, Bakos S, et al. Autoantibodies in chronic GVHD: High prevalence of antinucleolar antibodies. Bone Marrow Transplant 1990; 6: 93–6 [PubMed] [Google Scholar]
- 6.Patriarca F, Skert C, Sperotto A, et al. The development of autoantibodies after allogeneic stem cell transplantation is related with chronic graft-vs-host disease and immune recovery. Exp Hematol 2006; 34: 389–96 [DOI] [PubMed] [Google Scholar]
- 7.Siegert W, Stemerowicz R, Hopf U. Antimitochondrial antibodies in patients with chronic graft-versus-host disease. Bone Marrow Transplant 1992; 10: 221–7 [PubMed] [Google Scholar]
- 8.Trendelenburg M, Gregor M, Passweg J, et al. ‘Altered immunity syndrome’, a distinct entity in long-term bone marrow transplantation survivors? Bone Marrow Transplant 2001; 28: 1175–6 [DOI] [PubMed] [Google Scholar]
- 9.Lamey PJ, Lundy FT, Al-Hashimi I. Sjögren’s syndrome: a condition with features of chronic graft-versus-host disease: does duct cell adhesion or permeability play a role in pathogenesis? Med Hypotheses 2004; 62: 825–9 [DOI] [PubMed] [Google Scholar]
- 10.Couriel DR, Beguelin GZ, Giralt S, et al. Chronic graft-versus-host disease manifesting as polymyositis: an uncommon presentation. Bone Marrow Transplant 2002; 30: 543–6 [DOI] [PubMed] [Google Scholar]
- 11.Canninga-van Dijk MR, Sanders CJ, Verdonck LF, et al. Differential diagnosis of skin lesions after allogeneic haematopoietic stem cell transplantation. Histopathology 2003; 42: 313–30 [DOI] [PubMed] [Google Scholar]
- 12.Sanli H, Akay BN, Arat M, et al. Vitiligo after hematopoietic cell transplantation: six cases and review of the literature. Dermatology 2008; 216: 349–54 [DOI] [PubMed] [Google Scholar]