Abstract
Background:
Mexican Americans and non-Hispanic blacks have higher stroke recurrence rates and lower rates of secondary stroke prevention than non-Hispanic whites. As a potential explanation for this disparity, we assessed racial/ethnic differences in access to physician care and medications in a national sample of US stroke survivors.
Methods:
Among all 4,864 stroke survivors aged ≥45 years who responded to the National Health Interview Survey years 2000–2006, we compared access to care within the last 12 months by race/ethnicity before and after stratification by age (45–64 years vs ≥65 years). With logistic regression, we adjusted associations between access measures and race/ethnicity for sex, comorbidity, neurologic disability, health status, year, income, and health insurance.
Results:
Among stroke survivors aged 45–64 years, Mexican Americans, non-Hispanic blacks, and non-Hispanic whites reported similar rates of no generalist physician visit (approximately 15%) and inability to afford medications (approximately 20%). However, among stroke survivors aged ≥65 years, Mexican Americans and blacks, compared with whites, reported greater frequency of no generalist visit (15%, 12%, 8%; p = 0.02) and inability to afford medications (20%, 11%, 6%; p < 0.001). Mexican Americans and blacks more frequently reported no medical specialist visit (54%, 49%, 40%; p < 0.001) than did whites and rates did not differ by age. Full covariate adjustment did not fully explain these racial/ethnic differences.
Conclusions:
Among US stroke survivors at least 65 years old, Mexican Americans and blacks reported worse access to physician care and medications than whites. This reduced access may lead to inadequate risk factor modification and recurrent stroke in these high-risk minority groups.
Racial/ethnic disparities in stroke and its secondary prevention constitute substantial health and economic concerns for medical and public health systems.1 Non-Hispanic blacks and Hispanics, particularly Mexican Americans, have markedly higher incidence and prevalence of stroke than non-Hispanic whites, a difference that continues until age 75–85 years.2,3 Moreover, blacks and Mexican Americans have increased risk of recurrent stroke4,5 (which is more disabling and costly compared with first stroke6). Despite greater recurrent stroke risk, minority stroke survivors have lower rates of secondary stroke prevention.7–10
Reduced access to physicians and medications may prevent minority stroke survivors from receiving adequate secondary stroke prevention. Secondary stroke prevention requires access to care, often both generalist and specialist physician care, and to medications, to treat modifiable risk factors, such as hypertension and diabetes mellitus. Among US stroke survivors, blacks and Hispanics may have reduced access to stroke preventive care because they have lower median household income, have less access to high-quality health care, and are more frequently uninsured.11 Few studies have assessed racial/ethnic differences in access to ambulatory physician care or medication affordability among stroke survivors. Little is known regarding racial/ethnic differences in access to care for stroke survivors across the United States.
We examined racial/ethnic differences in access to physician care and medications, as well as other barriers to care, among non-Hispanic black, Mexican American, and non-Hispanic white community-dwelling stroke survivors using data from a recent nationally representative, population-based survey. We focus on Mexican Americans because they are the largest subgroup of Hispanics, in turn the largest minority population in the United States, they have been shown to have higher recurrent stroke rates, and the remaining surveyed Hispanic subgroups were small and heterogeneous.
METHODS
In this cross-sectional study, we compared access to care by race/ethnicity before and after stratification by age (45–64 years vs ≥65 years) among stroke survivors who responded to the National Health Interview Survey (NHIS) from years 2000 to 2006.
Study population.
The NHIS is a continuing, in-person household survey of the civilian, noninstitutionalized US population conducted annually by the National Center for Health Statistics.12 NHIS adult survey years 2000 to 2006 used similar survey designs and data collection methods and had final response rates of 70%–80%.12
Stroke survivors were identified as respondents who answered yes to the question, “Have you ever been told by a doctor or other health professional that you had a stroke?” The 2000 to 2006 NHIS samples from all US states and the District of Columbia and was designed to produce population-based estimates for the entire United States.12 NHIS oversamples black and Hispanic persons at approximate rates of 1.5:1 for blacks and 2:1 for Hispanics.12 To increase the proportion of elderly adults who are black or Hispanic, any black or Hispanic adult aged 65+ years was given twice the chance of being selected as any other adult in the family starting with the 2006 NHIS.12 We combined self-reported race and ethnicity to create 3 racial/ethnic groups: non-Hispanic whites (whites), non-Hispanic blacks (blacks), and Hispanic Mexican Americans (Mexican Americans). Data were obtained from the Minnesota Population Center and State Health Access Data Assistance Center (Integrated Health Interview Survey: Version 1.0; Minneapolis: University of Minnesota, 2006; http://ihis.us).
Outcome measures.
The 3 outcomes, measured within the past 12 months, were report of a visit to a generalist (general practice, family medicine, or internal medicine) physician, report of a visit to a medical specialist (other than obstetrician/gynecologist, psychiatrist, or ophthalmologist), and the inability to afford medications (“Was there any time when you needed prescription medicines but didn't get [them] because you couldn't afford [them]?”).
Statistical analysis.
Health care access variables and outcome measures were compared between racial/ethnic groups using χ2 test or t test, and US population estimates were calculated. Covariates were selected using clinical observation, literature review, and the Andersen Behavioral Model framework,13 which defines key factors (predisposing, enabling, and need-based) that impact health behaviors (i.e., having physician visits or purchasing medications) and outcomes. Predisposing factors relate to demographics and social structure and included age, sex, and education. Enabling factors refer to personal/family resources or health care access and included having a usual place for medical care, annual household income, lack of transportation delaying care, and health insurance. Need-based factors relate to perceived and evaluated health and included self-reported health status, neurologic disability due to stroke, and comorbidity. A comorbidity score was calculated by assigning 1 point for the presence of each of 6 major health conditions (hypertension, coronary heart disease, diabetes mellitus, emphysema, chronic kidney disease, and heart condition or disease) resulting in a maximum score of 6.14 Neurologic disability attributable to stroke was defined as stroke causing the adult respondent to have difficulty with ≥1 specific functional activities (e.g., walk a quarter mile, lift/carry 10 pounds). Given general qualification for Medicare health insurance at age 65 and our previous research showing that age modifies access to physician care and medications among stroke survivors,15 we examined frequencies of health insurance and access measures by race/ethnicity among younger (aged 45–64 years) and older (aged ≥65 years) stroke survivors.
Multivariable logistic regression analyses, stratified by the two age groups, examined the adjusted associations between racial/ethnic groups and the 3 outcome measures. We performed incremental regression models to examine the effect of sequential addition (i.e., forced entry) of predisposing factors, followed by enabling factors and then need-based factors. Annual household income and educational attainment were highly correlated so we included income and omitted education from the final models. Two covariates, usual place of care and lack of transportation, were excluded due to a lack of statistical contribution to the models. All of the analyses used SAS-callable SUDAAN version 9.01 (Research Triangle Institute, Research Triangle Park, NC) to obtain proper variance estimations that accounted for the complex NHIS sampling design and results that were weighted to reflect national population estimates.
Standard protocol approvals, registrations, and patient consents.
The Ohio State University institutional review board approved the project.
RESULTS
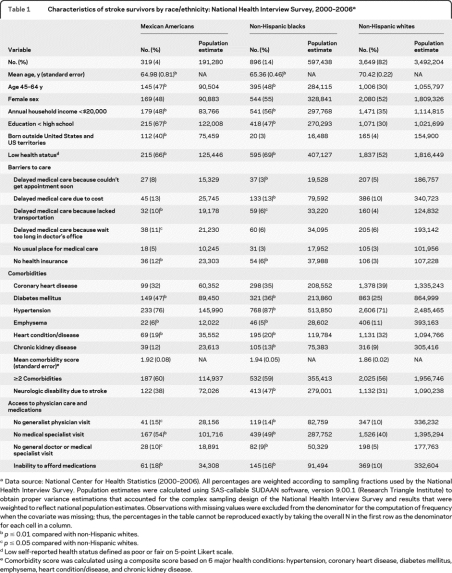
We identified 4,864 stroke survivors aged ≥45 years representing an estimated 4.3 million US stroke survivors (191,000 Mexican Americans [4%], 597,000 blacks [14%], 3.5 million whites [82%]). Mexican Americans (n = 319) and blacks (n = 896) were more likely than whites (n = 3649) to report < high school education and annual household income <$20,000 (table 1). Mexican Americans were more likely to be born outside the United States than blacks or whites. Mexican Americans and blacks reported similar but higher than whites' rates of low health status. The prevalence of diabetes was highest in Mexican Americans and of hypertension highest in blacks. The comorbidity score (mean 1.9) was similar across racial/ethnic groups.
Table 1.
Characteristics of stroke survivors by race/ethnicity: National Health Interview Survey, 2000–2006a
Data source: National Center for Health Statistics (2000–2006). All percentages are weighted according to sampling fractions used by the National Health Interview Survey. Population estimates were calculated using SAS-callable SUDAAN software, version 9.00.1 (Research Triangle Institute) to obtain proper variance estimations that accounted for the complex sampling design of the National Health Interview Survey and results that were weighted to reflect national population estimates. Observations with missing values were excluded from the denominator for the computation of frequency when the covariate was missing; thus, the percentages in the table cannot be reproduced exactly by taking the overall N in the first row as the denominator for each cell in a column.
p ≤ 0.01 compared with non-Hispanic whites.
p ≤ 0.05 compared with non-Hispanic whites.
Low self-reported health status defined as poor or fair on 5-point Likert scale.
Comorbidity score was calculated using a composite score based on 6 major health conditions: hypertension, coronary heart disease, diabetes mellitus, emphysema, heart condition/disease, and chronic kidney disease.
Racial/ethnic differences in barriers to medical care among US stroke survivors.
Overall, Mexican Americans and blacks were significantly more likely than whites to have lack of transportation delaying medical care and no health insurance (table 1). Among those aged 45–64 years, rates of no health insurance were 17% for Mexican Americans (pvs whites = 0.03), 12% for blacks (pvs whites = 0.15), and 9% for whites; however, among those aged ≥65 years, rates of no health insurance were 8% for Mexican Americans (pvs whites = 0.05), 2% for blacks (pvs whites = 0.19), and 0.6% for whites. Among uninsured stroke survivors, 60% of Mexican Americans were foreign-born compared with 2% of blacks and 11% of whites (p = 0.001). Blacks more frequently reported delaying medical care due to cost than whites, whereas Mexican Americans more commonly reported delaying medical care because of long wait in the doctor's office.
Racial/ethnic differences in access to physician care and medications among US stroke survivors.
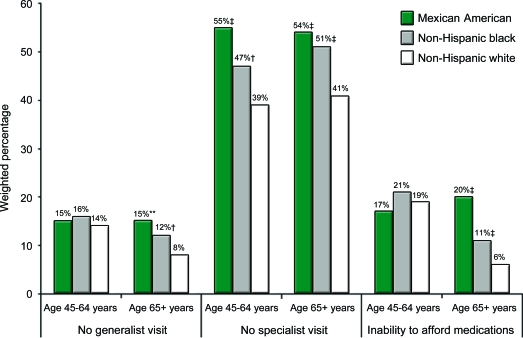
Mexican Americans and blacks, compared with whites, more often reported no generalist visit, no medical specialist visit, no generalist or medical specialist visit, and the inability to afford medications in the past 12 months (table 1). Stratification by age revealed that racial/ethnic differences in no generalist visit and the inability to afford medications were present among those ≥65 years old but absent in those 45–64 years old; conversely, racial/ethnic differences in no specialist visit did not differ by age (figure). Compared with younger stroke survivors, older stroke survivors had lower frequency of no generalist visit for whites only (14% vs 8%; p < 0.01) and less difficulty affording medications for whites (19% vs 6%; p < 0.01) and blacks (21% vs 11%; p < 0.01) but not Mexican Americans (17% vs 20%; p = 0.61).
Figure. Access to physician care and medications by race/ethnicity and age: National Health Interview Survey, 2000–2006*.
*Data source: National Center for Health Statistics (2000–2006). †p ≤ 0.05 compared with non-Hispanic whites. ‡p ≤ 0.01 compared with non-Hispanic whites. **p ≤ 0.07.
Effect of adjustment for demographic, socioeconomic, and clinical characteristics.
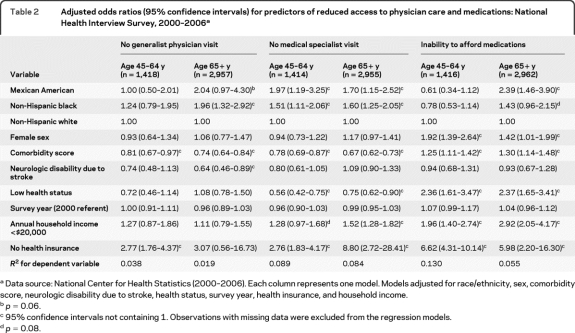
Among older stroke survivors, greater odds of no generalist visit were seen for blacks and there was a trend toward statistical significance for Mexican Americans after full adjustment. Greater odds of inability to afford medications were seen for Mexican Americans and there was a trend toward statistical significance for blacks (table 2). For both age groups, Mexican Americans and blacks had significantly greater odds of no specialist visit after adjustment. Regression models were not constructed for the combined outcome of no generalist physician or medical specialist visit because of insufficient sample size.
Table 2.
Adjusted odds ratios (95% confidence intervals) for predictors of reduced access to physician care and medications: National Health Interview Survey, 2000–2006a
Data source: National Center for Health Statistics (2000–2006). Each column represents one model. Models adjusted for race/ethnicity, sex, comorbidity score, neurologic disability due to stroke, health status, survey year, health insurance, and household income.
p = 0.06.
95% confidence intervals not containing 1. Observations with missing data were excluded from the regression models.
p = 0.08.
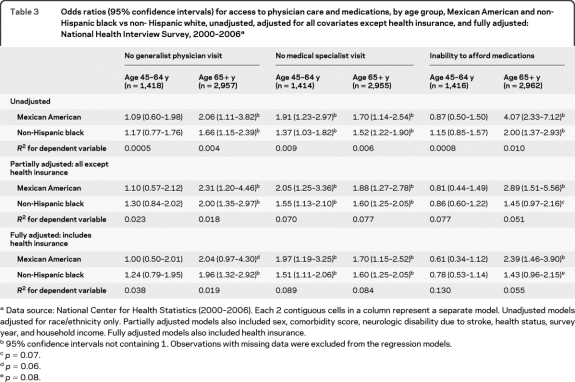
Given the magnitude of the odds ratios for no health insurance predicting lack of physician visits or inability to afford medications (point estimates of the odds ratios ranged from 2.7 to 8.8 in table 2) and the unexpectedly higher disparities in health insurance for the older group, we also compared unadjusted odds ratios, fully adjusted odds ratios (full models in table 2), and models adjusted for all covariates in table 2 except health insurance (table 3). We found that adjustment for demographics and comorbidity reduced racial/ethnic differences in inability to afford medications. Further adjustment for health insurance attenuated the odds of no generalist visit and inability to afford medications for Mexican Americans but not blacks.
Table 3.
Odds ratios (95% confidence intervals) for access to physician care and medications, by age group, Mexican American and non-Hispanic black vs non- Hispanic white, unadjusted, adjusted for all covariates except health insurance, and fully adjusted: National Health Interview Survey, 2000–2006a
Data source: National Center for Health Statistics (2000–2006). Each 2 contiguous cells in a column represent a separate model. Unadjusted models adjusted for race/ethnicity only. Partially adjusted models also included sex, comorbidity score, neurologic disability due to stroke, health status, survey year, and household income. Fully adjusted models also included health insurance.
95% confidence intervals not containing 1. Observations with missing data were excluded from the regression models.
p = 0.07.
p = 0.06.
p = 0.08.
DISCUSSION
In this recent nationally representative sample of stroke survivors, non-Hispanic blacks and Mexican Americans aged 65 years or older reported less access to generalist and specialist physician care and to medications than similarly aged non-Hispanic whites. Among those 45–64 years old, these differences were present only for specialist care. Comorbidity, health insurance, or income did not fully explain observed racial/ethnic differences in access to physician care and medications. Despite equal or greater need for medical care with higher prevalence rates of stroke risk factors, such as hypertension or diabetes, minority stroke survivors also had increased frequency of additional barriers to care including lack of transportation delaying care, income <$20,000, and, particularly for Mexican Americans, no health insurance. Strikingly, although prevalence of insurance was higher for each racial/ethnic group in the Medicare age range than for the younger group, racial/ethnic differences in health insurance were more pronounced in those above age 65. Among all covariates, lack of health insurance conferred the highest adjusted odds for reduced access in both age groups.
Although some16,17 but not all studies18 have shown less access to specialist (neurologist) care for minority stroke patients in the emergency department or hospital setting, few studies have assessed racial/ethnic differences in more general access measures and in a population-based fashion. Among US veterans hospitalized with ischemic stroke, outpatient utilization of both general medicine and neurology in the VA health system was lower for whites compared with blacks, although non-VA Medicare health care utilization was not captured and may have been higher among the older whites.19 In the Brain Attack Surveillance in Corpus Christi project, Mexican American stroke patients (mean age, 70 years) more frequently lacked a primary care physician compared with non-Hispanic whites (mean age, 75 years); however, the ethnic differences in access to primary care were attenuated after adjustment for age, sex, education, and insurance.20 We found that black and Mexican American stroke survivors had greater odds of no medical specialist visit and, among blacks aged 65 years or older, no generalist physician visit, after adjusting for comorbidity, socioeconomic factors, and health insurance. Our finding of a nonsignificant 2.04 greater odds in fully adjusted no generalist visit between Mexican Americans and whites may be due to small sample size of Mexican Americans or may reflect a true attenuation of the association between Hispanic ethnicity and no generalist visit by health insurance. In our earlier study assessing age-related differences in access to care of US stroke survivors in NHIS years 1998–2002, we found that black race was associated with lack of medical specialist visit but not with lack of generalist visit, perhaps owing to smaller sample size, reduced power to detect racial differences, and confounding by ethnicity and time.15
Potential causes of racial/ethnic disparities in access to or use of physician care include differences in socioeconomic status, health care access and utilization, and community resources, differences that may not be fully captured by income and insurance.11,21 Previous US research has found that differences in insurance, income, and available safety net services explain most differences (>80%) in access to physician care between Hispanics and whites but explain less of the access disparities between blacks and whites.21 Lower incomes and education levels of minority stroke survivors may be associated with broader health care access problems. Even in a system of universal health coverage, higher incomes and education levels are associated with significantly greater likelihood of referral to a cardiologist following discharge from acute myocardial infarction (AMI) hospitalization.22 In addition, physician practices and health care systems serving minority populations in the United States may have greater problems accessing specialist care and delivering high-quality care.23,24
Our findings are consistent with previous research in older US adults with chronic health conditions showing greater odds of cost-related nonadherence to medication among blacks and Hispanics compared with whites even after adjusting for demographic factors, comorbidity, or prescription drug coverage.25 In previous studies of US stroke survivors, we obtained conflicting results for the association of being black with inability to afford medications. The study of age-related differences in medication access found an absence of association possibly due to insufficient power and confounding by Hispanic ethnicity.15 In the study of regional differences in medication access, black women but not black men were more likely to be unable to afford medications after adjustment for income and insurance, possibly due to effect modification by gender and age.14 Our finding of a nonsignificant 1.45 greater odds in adjusted inability to afford medications for blacks vs whites, in the present study, may be due to decreased power or may reflect a true attenuation of the association between being black and inability to afford medications by demographics and comorbidity. Demographics and comorbidity and also health insurance explained some but not all of the difference in inability to afford medications between Mexican Americans and whites.
The reasons for greater difficulty affording medications among older minority stroke survivors are uncertain but may include unmeasured racial/ethnic differences in socioeconomic status.25 Given the need for secondary stroke prevention and the frequency of stroke-related conditions and comorbidities, stroke survivors have a high burden and cost of medication. In the observational CAReS study, stroke survivors aged 50 years or older were discharged home from rehabilitation with an average of 11.3 medications (range 3–27).26 In the same cohort, the monthly cost of the 10 most common medications prescribed at discharge was $800 (monthly average wholesale price, 2008).26 In this 2000–2006 study, we found that, among US stroke survivors aged 45 years or older, about 1 in 5 Mexican Americans, 1 in 6 blacks, and 1 in 10 whites had cost-related nonadherence (CRN) to medication within the last 12 months. Although the NHIS asks only about CRN to any medication, a survey of middle-aged and elderly adults that specifically assessed CRN to stroke medication found that 13% of US stroke survivors reported CRN to stroke medication ever in the past year and 8% reported CRN to stroke medication at least monthly, numbers consistent with our findings.27
Reduced access to ambulatory physician care and medications following stroke potentially leads to poor quality of care and adverse health outcomes. Lack of physician follow-up after stroke has been associated with lower rates of secondary stroke preventive therapy28 and higher risk of death, even after adjusting for demographics and comorbidity.19 Although there is not information regarding the impact of CRN to medication on health outcomes in cohorts of stroke patients only, studies in middle-aged and elderly adults with preexisting cardiovascular disease including stroke found that CRN to medication was associated with greater odds of nonfatal stroke or AMI,29 angina,29 and hospitalization.30 In a study of a related cardiovascular disease, AMI, financial barriers to health care services or medications were associated with suboptimal recovery including more angina, higher risk of rehospitalization, and poorer quality of life.31 The provision of affordable or immediate Medicare insurance to uninsured stroke survivors would be expected to improve access to medical care, including physician visits32 and medications,33 and may result in substantial health gains and subsequent reductions in health care costs.34 Full prescription drug coverage of secondary preventive therapies for poststroke patients after hospital discharge, currently under study for post-AMI patients,35 may prove cost-effective.36 In addition to health insurance and prescription drug coverage, increased resources and insurance reimbursements for primary care providers in high-minority practices are needed to improve the quality of care, including care coordination and ability to obtain specialty care, for complex ambulatory poststroke patients.24
Our study has several limitations. Given the observational study design, we cannot infer causation from observed associations. Several factors, including provider characteristics, metropolitan status, and stroke features (type, severity, or timing), could not be assessed adequately. These NHIS data, including stroke history, are self-reported and subject to recall bias and reporting error. However, recent reports suggest high self-reported stroke accuracy, even in the disabled elderly, with sensitivity rates ranging from 80% to 98%37,38 and substantial reliability in minorities.39 We were unable to assess the effect of acculturation or English proficiency among Hispanics but decreased acculturation and limited English proficiency are associated with lower rates of receipt of recommended health care services.40 Because the NHIS does not have measures of disease severity, the comorbidity score did not incorporate disease severity. The NHIS includes only community-dwelling, noninstitutionalized stroke survivors, and results may only be generalized to this population. Selection bias may occur if minority stroke survivors with reduced access to care are less frequently sampled compared to minority stroke survivors with adequate access. This potential selection bias would reduce the ability to detect the differences we observed. Further research is needed to assess whether disparities in these processes of care are associated with racial/ethnic differences in poststroke outcomes such as recurrent stroke.
Footnotes
- AMI
- acute myocardial infarction
- CRN
- cost-related nonadherence
- NHIS
- National Health Interview Survey
AUTHOR CONTRIBUTIONS
Statistical analysis was conducted by Dr. Deborah A. Levine and Dr. Sudeep Karve.
DISCLOSURE
Dr. Levine receives research support from the NIH (P30 AG024824-07 [Sub-project PI]). Dr. Neidecker serves as a consultant for Ortho-McNeil-Janssen Pharmaceuticals, Inc. and her spouse owns stock in Thoratec Corporation. Dr. Kiefe serves as Co-Editor-in-Chief of Medical Care and receives/has received research support from the NIH (R01 HL70786 [PI], U01 HL079171 [PI], HC-93-01 [Associate Director, Coordinating Center], U01 CA 93329 [investigator], U54 RR024376 [Co-PI], P60 DK0769626 [Associate Director for Prevention and Control], and U18 HS016956 [investigator]). Dr. Karve reports no disclosures. Dr. Williams serves as Section co-chair for Health Policy and Outcomes, Stroke; is Research Coordinator for the VA HSR&D Stroke QUERI; and receives/has received research support from the NIH (R01 NS 3957 [PI]) and the US Veterans Administration (IIR 05-297-2 [Co-PI], SDP 09-158 [PI], SDP-06-004 [coinvestigator], IIR-06-233-2 [coinvestigator]. Dr. Allison serves as Co-Editor-in-Chief of Medical Care and receives/has received research support from the NIH (1R01CA1290911 [investigator] and R21 DK081887 [investigator]), the Agency for Healthcare Research and Quality, and the American Cancer Society.
REFERENCES
- 1. Brown DL, Boden-Albala B, Langa KM, et al. Projected costs of ischemic stroke in the United States. Neurology 2006;67:1390–1395 [DOI] [PubMed] [Google Scholar]
- 2. Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics: 2010 update: a report from the American Heart Association. Circulation Epub 2009 Dec 17 [DOI] [PubMed] [Google Scholar]
- 3. Morgenstern LB, Smith MA, Lisabeth LD, et al. Excess stroke in Mexican Americans compared with non-Hispanic whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol 2004;160:376–383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sheinart KF, Tuhrim S, Horowitz DR, Weinberger J, Goldman M, Godbold JH. Stroke recurrence is more frequent in blacks and Hispanics. Neuroepidemiology 1998;17:188–198 [DOI] [PubMed] [Google Scholar]
- 5. Lisabeth LD, Smith MA, Brown DL, Moye LA, Risser JM, Morgenstern LB. Ethnic differences in stroke recurrence. Ann Neurol 2006;60:469–475 [DOI] [PubMed] [Google Scholar]
- 6. Samsa GP, Bian J, Lipscomb J, Matchar DB. Epidemiology of recurrent cerebral infarction: a medicare claims-based comparison of first and recurrent strokes on 2-year survival and cost. Stroke 1999;30:338–349 [DOI] [PubMed] [Google Scholar]
- 7. Brenner DA, Zweifler RM, Gomez CR, et al. Awareness, treatment, and control of vascular risk factors among stroke survivors. J Stroke Cerebrovasc Dis 2010;19:311–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Christian JB, Lapane KL, Toppa RS. Racial disparities in receipt of secondary stroke prevention agents among US nursing home residents. Stroke 2003;34:2693–2697 [DOI] [PubMed] [Google Scholar]
- 9. Birman-Deych E, Radford MJ, Nilasena DS, Gage BF. Use and effectiveness of warfarin in Medicare beneficiaries with atrial fibrillation. Stroke 2006;37:1070–1074 [DOI] [PubMed] [Google Scholar]
- 10. Hughes CM, Lapane KL. Factors associated with the initiation and discontinuation of secondary stroke prevention agents in nursing homes. J Stroke Cerebrovasc Dis 2004;13:164–170 [DOI] [PubMed] [Google Scholar]
- 11. US Department of Health and Human Services National Healthcare Disparities Report 2008: AHRQ Publication No. 09-0002. Rockville, MD: Agency for Healthcare Research and Quality; March 2009. Available at: http://www.ahrq.gov/qual/qrdr08.htm Accessed March 18, 2010 [Google Scholar]
- 12. National Health Interview Survey. Available at: http://www.cdc.gov/nchs/nhis.htm Accessed March 18, 2010
- 13. Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res 2000;34:1273–1302 [PMC free article] [PubMed] [Google Scholar]
- 14. Levine DA, Kiefe CI, Howard G, Howard VJ, Williams OD, Allison JJ. Reduced medication access: a marker for vulnerability in US stroke survivors. Stroke 2007;38:1557–1564 [DOI] [PubMed] [Google Scholar]
- 15. Levine DA, Kiefe CI, Houston TK, Allison JJ, McCarthy EP, Ayanian JZ. Younger stroke survivors have reduced access to physician care and medications: National Health Interview Survey from years 1998 to 2002. Arch Neurol 2007;64:37–42 [DOI] [PubMed] [Google Scholar]
- 16. Brown DL, Lisabeth LD, Garcia NM, Smith MA, Morgenstern LB. Emergency department evaluation of ischemic stroke and TIA: the BASIC Project. Neurology 2004;63:2250–2254 [DOI] [PubMed] [Google Scholar]
- 17. Mitchell JB, Ballard DJ, Matchar DB, Whisnant JP, Samsa GP. Racial variation in treatment for transient ischemic attacks: impact of participation by neurologists. Health Serv Res 2000;34:1413–1428 [PMC free article] [PubMed] [Google Scholar]
- 18. Jacobs BS, Birbeck G, Mullard AJ, et al. Quality of hospital care in African American and white patients with ischemic stroke and TIA. Neurology 2006;66:809–814 [DOI] [PubMed] [Google Scholar]
- 19. Kamalesh M, Shen J, Tierney WM. Stroke mortality and race: does access to care influence outcomes? Am J Med Sci 2007;333:327–332 [DOI] [PubMed] [Google Scholar]
- 20. Smith MA, Risser JM, Lisabeth LD, Moye LA, Morgenstern LB. Access to care, acculturation, and risk factors for stroke in Mexican Americans: the Brain Attack Surveillance in Corpus Christi (BASIC) project. Stroke 2003;34:2671–2675 [DOI] [PubMed] [Google Scholar]
- 21. Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res 2003;38:809–829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alter DA, Iron K, Austin PC, Naylor CD. Socioeconomic status, service patterns, and perceptions of care among survivors of acute myocardial infarction in Canada. JAMA 2004;291:1100–1107 [DOI] [PubMed] [Google Scholar]
- 23. Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med 2007;167:1177–1182 [DOI] [PubMed] [Google Scholar]
- 24. Reschovsky JD, O'Malley AS. Do primary care physicians treating minority patients report problems delivering high-quality care? Health Aff 2008;27:222–231 [DOI] [PubMed] [Google Scholar]
- 25. Gellad WF, Haas JS, Safran DG. Race/ethnicity and nonadherence to prescription medications among seniors: results of a national study. J Gen Intern Med 2007;22:1572–1578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ostwald SK, Wasserman J, Davis S. Medications, comorbidities, and medical complications in stroke survivors: the CAReS study. Rehabil Nurs 2006;31:10–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health 2004;94:1782–1787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Redfern J, McKevitt C, Rudd AG, Wolfe CD. Health care follow-up after stroke: opportunities for secondary prevention. Fam Pract 2002;19:378–382 [DOI] [PubMed] [Google Scholar]
- 29. Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care 2004;42:626–634 [DOI] [PubMed] [Google Scholar]
- 30. Heisler M, Choi H, Rosen AB, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: a longitudinal analysis. Med Care 2010;48:87–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA 2007;297:1063–1072 [DOI] [PubMed] [Google Scholar]
- 32. McWilliams JM, Zaslavsky AM, Meara E, Ayanian JZ. Impact of Medicare coverage on basic clinical services for previously uninsured adults. JAMA 2003;290:757–764 [DOI] [PubMed] [Google Scholar]
- 33. Evans-Molina C, Regan S, Henault LE, Hylek EM, Schwartz GR. The new Medicare Part D prescription drug benefit: an estimation of its effect on prescription drug costs in a Medicare population with atrial fibrillation. J Am Geriatr Soc 2007;55:1038–1043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Medicare spending for previously uninsured adults. Ann Intern Med 2009;151:757–766 [DOI] [PubMed] [Google Scholar]
- 35. Choudhry NK, Brennan T, Toscano M, et al. Rationale and design of the Post-MI FREEE trial: a randomized evaluation of first-dollar drug coverage for post-myocardial infarction secondary preventive therapies. Am Heart J 2008;156:31–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Choudhry NK, Patrick AR, Antman EM, Avorn J, Shrank WH. Cost-effectiveness of providing full drug coverage to increase medication adherence in post-myocardial infarction Medicare beneficiaries. Circulation 2008;117:1261–1268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Simpson CF, Boyd CM, Carlson MC, Griswold ME, Guralnik JM, Fried LP. Agreement between self-report of disease diagnoses and medical record validation in disabled older women: factors that modify agreement. J Am Geriatr Soc 2004;52:123–127 [DOI] [PubMed] [Google Scholar]
- 38. Heckbert SR, Kooperberg C, Safford MM, et al. Comparison of self-report, hospital discharge codes, and adjudication of cardiovascular events in the Women's Health Initiative. Am J Epidemiol 2004;160:1152–1158 [DOI] [PubMed] [Google Scholar]
- 39. Andresen EM, Malmstrom TK, Miller DK, Miller JP, Wolinsky FD. Retest reliability of self-reported function, self-care, and disease history. Med Care 2005;43:93–97 [PubMed] [Google Scholar]
- 40. Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med 2007;22(suppl 2):283–288 [DOI] [PMC free article] [PubMed] [Google Scholar]