Abstract
A 64-year-old woman presented with shortness of breath, right-sided pleuritic chest pain and dry cough. She was systemically anticoagulated with warfarin for a pulmonary embolism diagnosed 3 months previously, with an international normalised ratio (INR) of 3.0 on presentation. Chest radiograph demonstrated a new right paratracheal abnormality, and CT scan showed a large mediastinal mass not present 3 weeks earlier. MRI demonstrated an ovoid mass with a fluid/fluid level with high T2 and dark T1 signal consistent with a mediastinal haematoma. The patient's anticoagulation was emergently reversed and a temporary inferior vena cava filter was placed. The haematoma slowly resolved on serial follow-up with no additional intervention. Spontaneous mediastinal haematoma is a rare but life-threatening diagnosis that frequently presents with chest pain, dry cough and dysphagia. It is frequently associated with therapeutic anticoagulation and may potentially be caused by sudden, atraumatic rise in intrathoracic pressure (ie, cough or emesis).
Background
Spontaneous mediastinal haematoma is a rare but life-threatening diagnosis that must be seriously considered in anticoagulated patients presenting with chest pain, dyspnoea and/or dysphagia and new radiographic abnormalities.
Case presentation
A 64-year-old white female non-smoker presented with a 2-day history of shortness of breath, non-productive cough and right-sided pleuritic chest pain. She denied infectious symptoms or dysphagia, and there was no family history of clotting or bleeding disorders. Review of systems was positive only for mild nausea and chronic myalgias.
Past medical history was significant only for a right popliteal vein thrombosis (deep vein thrombosis) 3 months previously, complicated by multiple bilateral segmental and subsegmental pulmonary emboli. This event was attributed to an extended car trip in the setting of concurrent hormone replacement therapy for severe post-menopausal symptoms. Hormone therapy was discontinued at that time, and anticoagulation was initiated with weight-based enoxaparin and transitioned to oral warfarin. Her compliance with anticoagulation was excellent, with consistently therapeutic international normalised ratios (INRs) on serial close monitoring.
Approximately 3 weeks before her current presentation the patient presented with similar symptoms of non-productive cough and shortness of breath. CT pulmonary angiogram (CTPA) excluded recurrent venous thromboembolism and demonstrated new right middle lobe infiltrate and reactive mediastinal lymphadenopathy. The patient was treated with azithromycin for presumptive community-acquired pneumonia with subsequent resolution of her symptoms.
Physical examination demonstrated normal vital signs and oxygenation saturation of 94% on room air. Physical examination was normal.
Investigations
Initial laboratory evaluation was remarkable for a mild, stable anaemia and an INR of 3.01 (goal 2.0–3.0). Chest radiograph demonstrated a new significant right paratracheal abnormality (figure 1).
Figure 1.

Initial posteroanterior view of the chest showing a large paratracheal mass.
A contrast-enhanced chest CT revealed a 3.6×4.2 cm right paratracheal mass that was not present on CTPA performed 3 weeks previously (figure 2).
Figure 2.
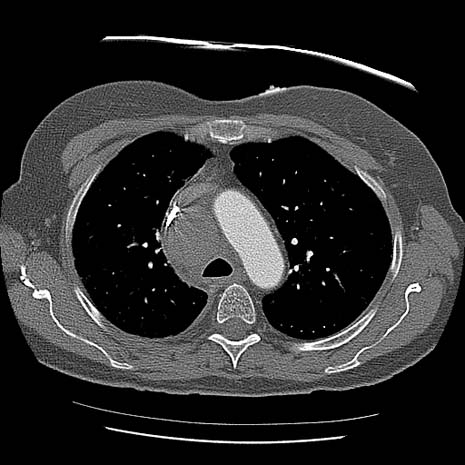
CT of the chest demonstrating a 3.6×4.2 cm ovoid-shaped right paratracheal mass.
The patient was admitted for observation and expedited evaluation. Follow-up MRI with and without gadolinium revealed a heterogeneous 5.9×4.6×3.2 cm ovoid-shaped right paratracheal mass. There was a fluid/fluid level within the mass, with the more dependent component demonstrating high T2 and dark T1 signal precontrast consistent with blood (figure 3).
Figure 3.
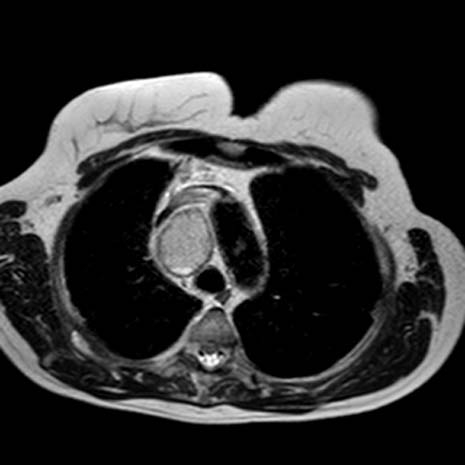
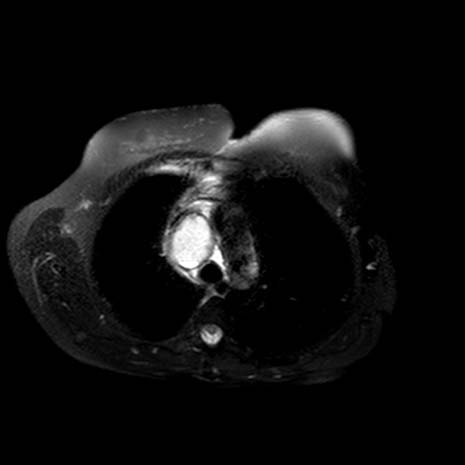
(A, B) Axial fast-recovery fast spin-echo T2 images with and without fat saturation images showing heterogeneous signal within the mass and a dark peripheral rim.
Differential diagnosis
The differential diagnosis of the middle mediastinal mass identified in this patient requires careful consideration of the normal structures found in this vicinity. Lymphadenopathy in this area is common, and can be due to involvement from primary lung or metastatic tumours, lymphoma or Kaposi's sarcoma (in AIDS patients). A wide variety of inflammatory and infectious aetiologies may also result in lymphadenopathy in this area, including granulomatous inflammation from mycobacterial or fungal infection, plague, sarcoidosis, drug reaction and Castleman's disease. Congenital abnormalities including bronchogenic cysts and bronchopulmonary sequestration may also present with an isolated mediastinal mass in this manner. Primary tracheal or bronchogenic tumours may also cause similar radiographic findings. Associated vascular abnormalities include significant distension of the superior vena cava, right-sided aortic arch and haematoma.
Treatment
The rapid development of a large mediastinal mass over 3 weeks in the setting of supra-therapeutic anticoagulation in this patient was strongly suggestive of a spontaneous mediastinal haematoma, which was confirmed on short interval follow-up MRI. Due to the interval increase in the size of her haematoma between her CT and MRI images, the patient was emergently reversed with vitamin K and fresh frozen plasma and monitored closely with serial radiographs and complete blood cell counts for the next 48 h. Despite her progressive radiographic changes and the suggestion of venous compression on her cross-sectional imaging, the patient remained largely asymptomatic and never exhibited signs or symptoms to suggest superior vena cava syndrome. As it was not quite 3 months since she had experienced a significant episode of venous thromboembolism, a removable inferior vena cava filter was placed.
Outcome and follow-up
Serial observation and radiographic imaging over the next 10 months demonstrated complete resolution of her mediastinal haematoma with no residual radiographic abnormalities (figure 4).
Figure 4.

Posteroanterior chest radiograph 10 months after initial presentation demonstrating complete radiographic resolution of the patient's mediastinal haematoma.
Discussion
Spontaneous (atraumatic) mediastinal haematoma is a rarely reported entity, with fewer than 50 cases documented in the literature.1–5 The majority of these cases were attributed to anticoagulation or other bleeding diathesis; other documented aetiologies include haemorrhage into a mediastinal organ or abnormal cystic structure, and several others were idiopathic. The most common postulated mechanism is spontaneous vessel rupture in the setting of anticoagulation, which in some cases appears to be preceded by a rapid, atraumatic increase in intrathoracic pressure such as with repeated vomiting or violent coughing.
Presenting symptoms described in previous case reports include chest pain, dyspnoea and/or dysphagia. Appropriate diagnostic modalities include both invasive and non-invasive imaging modalities, with the selection largely based on the acuity of the patient's clinical condition and the suspicion for the presence of a haematoma. Although the patient in this case report remained clinically stable throughout her course, the presentation of spontaneous mediastinal haematoma is highly variable and underlines the seriousness of this condition. Twenty-one of the 39 patients reported in the largest case series by Gomelsky et al required surgical intervention, and five of these 39 patients died from complications related to the haematoma and its management. Patient acuity and evidence of ongoing bleeding prompted emergent surgical exploration and haematoma removal or embolisation of a suspected vessel in most reported cases, while other patients needed no emergent intervention or treatment other than discontinuation of anticoagulation.
Our patient provides a classic example of the clinical presentation and risk factors for spontaneous mediastinal haematoma, with symptoms of chest pain and dyspnoea following a series of coughing episodes in the setting of therapeutic anticoagulation for recent pulmonary emboli. With our patient's supratherapeutic anticoagulation and rapidly expanding mediastinal mass with haemorrhagic component and fluid/fluid level, she most likely spontaneously ruptured a small vein or venule in her superior mediastinum. The resulting haematoma likely created a tamponade to further flow, as the patient remained haemodynamically stable and required neither urgent surgical intervention nor blood replacement.
A thickened right paratracheal stripe can indicate disease affecting the trachea, mediastinum or pleura, including findings associated with adenopathy or other masses. On CT scan, the differential considerations for the rapidly developing ovoid-shaped 3.6×4.2 cm soft tissue density mass seen in this patient are a focal haematoma or marked interval enlargement of a node in a patient with history of infection. The MRI findings of fluid/fluid levels and a dark rim confirm the suspicion of haematoma in a patient with a history of anticoagulation. Interval decrease in chest radiograph findings corroborates a decrease in size of the haematoma. Chest CT should be the next appropriate step in evaluation for paratracheal stripe thickening or evaluation for a clinical suspicion of mediastinal haematoma.
Spontaneous mediastinal haematoma needs to be carefully considered in the differential diagnosis of a patient presenting with chest pain and dyspnoea who is taking anticoagulation and has a new or rapidly enlarging mediastinal mass. Stable patients should receive non-invasive thoracic imaging with CT or MRI, and treatment includes reversal of anticoagulation and serial monitoring for evidence of ongoing active bleeding. Close follow-up is necessary to ensure complete resolution of radiographic abnormalities and to exclude underlying mediastinal pathology that may predispose to haematoma formation in patients with risk factors for malignancy.
Learning points.
-
▶
Spontaneous mediastinal haematoma is a rare condition with a variable clinical course, and can be associated with serious complications and death.
-
▶
The most common postulated mechanism for this condition is spontaneous vessel rupture in the setting of anticoagulation, preceded by a rapid, atraumatic increase in intrathoracic pressure such as with repeated vomiting or violent coughing.
-
▶
Presenting symptoms include chest pain, dyspnoea and dysphagia with a new mediastinal mass on radiographic imaging.
-
▶
Chest CT should be the next step after plain radiographs to evaluate patients with a clinical suspicion of mediastinal haematoma, with angiography and emergent surgical exploration reserved for unstable patients with evidence of significant, ongoing bleeding.
-
▶
Close serial follow-up to ensure resolution of radiographic changes is essential in patients with risk factors for malignancy.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Gomelsky A, Barry MJ, Wagner RB. Spontaneous mediastinal hemorrhage: a case report with a review of the literature. Md Med J 1997;46:83–7 [PubMed] [Google Scholar]
- 2.Song J, Hindawi R, Deshpande A, et al. Spontaneous atraumatic mediastinal hematoma. Hosp Physician 2002;38:37–9 [Google Scholar]
- 3.Tanaka T, Ueda K, Hayashi M, et al. Minimally invasive treatment for spontaneous mediastinal hematoma. Surgery 2009;145:248–9 [DOI] [PubMed] [Google Scholar]
- 4.Bageacu S, Prades JM, Kaczmarek D, et al. Images in cardiothoracic surgery. Spontaneous rupture of the inferior thyroid artery leading to life-threatening mediastinal hematoma. Ann Thorac Surg 2005;80:e20–1 [DOI] [PubMed] [Google Scholar]
- 5.Shih SY, Hu SY, Tsan YT, et al. Spontaneous hemomediastinum and hemothorax caused by ruptured bronchial artery aneurysm. Eur J Cardiothorac Surg 2009;35:1076–9 [DOI] [PubMed] [Google Scholar]


