Abstract
Reasons for inconsistent associations between overeating styles and adiposity among youth may include differences in effects by age, gender, or ethnicity; failure to control for social desirability of response; or adiposity measurement limitations. This study examined the relationship between overeating styles and multiple measures of adiposity, after controlling for social desirability and testing for moderation by ethnicity, age, and gender. Data from 304 9–10 year old children and 264 17–18 year old adolescents equally representing African American, Hispanic, and White ethnic groups were extracted from a larger cross-sectional study. Measures included the Dutch Eating Behavior Questionnaire (restrained, external, and emotional overeating subscales), the “Lie Scale” from the Revised Children’s Manifest Anxiety Scale, and measured weight, height, waist circumference, and triceps skinfold. BMI z-score and a global adiposity index were calculated. Mixed model linear regression showed restraint was positively and external eating was negatively related to measures of adiposity. African American youth had a stronger inverse association between emotional eating and adiposity than White or Hispanic youth. Relationships were not influenced by social desirability nor moderated by age or gender. Overeating styles are related to adiposity in nearly all youth but the nature of these associations are moderated by ethnicity.
Keywords: overeating styles, restraint, external eating, emotional eating, adiposity, children, adolescents
Introduction
Positive energy balance is in part the result of overeating, and thus involved in the pathogenesis of obesity (Braet & Van Strien, 1997; Hervey, 1969; Das, 2010). Three theories have addressed how eating style may lead to obesity (Braet & Van Strien, 1997). Psychosomatic theory (Bruch, 1964) posited normal weight individuals experience reductions in hunger and eating, as a normal fight or flight response to strong negative emotions (Gold & Chrousos, 2002), but some overweight individuals have learned through early rearing experiences to maladaptively respond to these emotions with an upregulation in energy intake (Bohon, Stice, & Spoor, 2009; Snoek, Engels, Janssens, & van Strien, 2007; van Strien, Snoek, van der Zwaluw, & Engels, 2010). Externality theory (Schachter & Rodin, 1974) posited normal weight individuals ate in response to internal hunger signals while obese individuals ate in response to food cravings triggered by cues environmental cues (Burton, Smit, & Lightowler, 2007). These environmentally influenced overeating behaviors may be automatic, and occur without conscious awareness (Wansink, 2004; Wansink, Payne, & Chandon, 2007). Restraint theory (Herman & Polivy, 1980) posited obese individuals overate as a rebound response to chronic dieting and food restriction; however, recent longitudinal research among adolescents indicated the reverse: overweight individuals more likely restricted intake in response to weight problems (Snoek, Van Strien, Janssens, & Engels, 2008).
The Dutch Eating Behavior Questionnaire (DEBQ) validly measured restrained, external, and emotional eating styles (Van Strien, Frijters, Bergers, & Defares, 1986) among obese and non-obese adults (Van Strien, Herman, & Verheijden, 2009), adolescents (Braet, Claus, Goossens, Moens, Van Vlierberghe, & Soetens, 2008; van Strien, et al., 2010), and children (Van Strien & Oosterveld, 2008). Studies involving the DEBQ among European adults consistently found a relationship between weight and overeating styles (Van Strien, et al., 1986; Van Strien, et al., 2009), but the associations between overeating styles and adiposity among children have been less consistent (Braet, et al., 2008; Braet & Van Strien, 1997; Lluch, Herbeth, Mejean, & Siest, 2000; Snoek, Van Strien, Janssens, & Engels, 2007). Compared to normal weight European children, obese European children scored higher on emotional, restrained, and external eating when overeating style was measured by parent report, (Braet & Van Strien, 1997). Although child and adolescent self-reported restraint has repeatedly been positively related to adiposity among youth regardless of age and gender (Braet, et al., 2008; Lluch, et al., 2000; Snoek, et al., 2007), inverse relationships between self-reported emotional and external eating scores and adiposity were detected among male (Snoek, et al., 2007) and female adolescents (Lluch, et al., 2000), and male and female children (Braet, et al., 2008). Age and gender differences have been detected in the associations between eating style and adiposity; however, no studies have statistically tested for moderation effects.
Obesity/overweight prevalence in the United States differed by ethnic group with ethnic minority youth being at greatest risk of overweight and obesity (Flegal, Ogden, Yanovski, Freedman, Shepherd, Graubard, et al. 2010; Ogden, Carroll, Curtin, Lamb, & Flegal, 2010). Weight misperception was more prevalent among obese non-Hispanic adults and obese Mexican American females compared to White obese adults (Ogden et al., 2010), and ethnic groups differed in body satisfaction, dieting, and eating disorder behaviors (Gluck & Geliebter, 2002; Lynch, Heil, Wagner, & Havens, 2007; Neumark-Sztainer, Croll, Story, Hannan, French, & Perry, 2002; Pernick, Nichols, Rauh, Kern, Ji, Lawson et al., 2006; Ricciardelli, McCabe, Williams, & Thompson, 2007; White & Grilo, 2005). Ethnic groups differed in overeating behaviors in the Netherlands (Dutch children scored lower on restraint than Moroccan, Surinamese, and Turkish children) (Snoek, et al., 2007).
Youth overeating style (Snoek, et al., 2007; van Strien, et al., 2010) and child eating behavior (Faith, Heshka, Keller, Sherry, Matz, Pietrobelli, et al., 2003; Faith, Scanlon, Birch, Francis, & Sherry, 2004) were influenced by parent and care provider behaviors, which varied by ethnic group (Hughes, Patrick, Power, Fisher, Anderson, & Nicklas, 2007). African American parents used direct commands and reasoning during meals to influence child eating (Iannotti, O’Brien, & Spillman, 1994), while Hispanic parents reported using bribery (Kaiser, Martinez, Harwood, & Garcia, 1999), and were permissive and encouraging with desired foods, authoritarian in response to food refusal, but authoritative when discouraging eating undesirable foods (Kaiser, et al., 1999; Olvera-Ezzell, Power, & Cousins, 1990). Non-Hispanic and non-African American mothers provided greater choice at meals to their toddlers than Hispanic or African American mothers (Faith, et al., 2003). Ethnic group differences in obesity rates, parental feeding practices, and eating behaviors, suggests ethnicity may be a moderator of the association between overeating style and adiposity among youth.
Social desirability biased children’s accurate report of their own thoughts, feelings, and behaviors related to their eating (Braet, et al., 2008), and social desirability influenced children’s reporting of eating and physical activity behaviors related to weight status (Klesges, Baranwoski, Beech, Cullen, Murray, Rochon, et al., 2004). Failure to control for this potential confounder may explain inconsistencies in the association between overeating styles and adiposity (Braet, et al., 2008; Braet & Van Strien, 1997; Lluch, et al., 2000; Snoek, et al., 2007).
Studies examining the relationships between eating behavior and adiposity among youth have measured adiposity with age and gender corrected BMI (Braet, et al., 2008; Snoek, et al., 2007), or relative weight, which is a percentage of ideal body weight accounting for height and gender (Lluch, et al., 2000). Limitations of BMI and relative weight are they fail to account for fat distribution (Stevens, 2008; Stevens, McClain, & Truesdale, 2008), and BMI percentile missed the detection of excess adiposity in some children (Bedogni, Iughetti, Ferrari, Malavolti, Poli, Bernasconi et al., 2003; Freedman, Wang, Ogden, Thornton, Mei, Pierson, et al., 2007; Mei, Grummer-Strawn, Wang, Thornton, Freedman, Pierson, et al., 2007), but the addition of other measures of adiposity (i.e., triceps skinfold) increased BMI percentile sensitivity (Bedogni, et al., 2003; Freedman, et al., 2007; Mei, et al., 2007). Triceps skinfold provides a representation of subcutaneous body fat (Fogelholm & Lichtenbelt, 1997), and waist circumference (WC) is an indicator of central or visceral adiposity (Ness-Abramof & Apovian, 2008; Stevens, 2008; Stevens, et al., 2008). Recent longitudinal data showed childhood WC was a better predictor of young adult metabolic syndrome development than BMI (Schmidt, Dwyer, Magnussen, & Venn, 2010). Limitations to WC and triceps skinfold, however, are neither are age nor gender adjusted; they represent only localized fatness; and they are subject to substantial measurement error. WC, triceps skinfold, and BMI z-score are all adiposity indicators, and each are associated with some degree of measurement error. Combining these measures into a composite index (similar to a latent variable), results in one variable consisting of the shared variance of these measures which represents the underlying construct of global adiposity (Bollen, 1989; Chavance, Escolano, Romon, Basdevant, de Lauzon-Guillain, & Charles, 2010; Marshall, Hazlett, Spady, & Quinney, 1990). The global adiposity index has less error but is represented by one variable, thereby allowing for more parsimonious analysis (Bollen, 1989; Chavance, et al., 2010). There is growing epidemiology interest in composite measures of adiposity given the limitations of single measures (Chavance, et al., 2010). No research among youth has examined eating styles in relation to WC, triceps skinfold, or a composite indicator of adiposity.
The current study examined the relationship between eating styles (restrained, external, and emotional) and adiposity (as indicated by global adiposity index, BMI z-score, WC, and triceps skinfold) after controlling for social desirability (potential confounder) and testing for the possible moderation effects of ethnicity, age, and gender. It is hypothesized that ethnicity, age, and gender will significantly moderate the association between eating behavior and adiposity thereby explaining the inconsistent findings in previous studies of this relationship among youth (Braet, et al., 2008; Lluch, et al., 2000; Snoek, et al., 2007). Understanding the relationships between overeating styles and adiposity has implications for developing interventions to address the obesity epidemic among youth.
Methods
Participants
Data for this study were extracted from a larger study testing the relationship of taste sensitivity for a bitter compound found in some foods (6-n-Propylthiouracil; PROP) to adiposity (Baranowski et al., 2010). In the larger study sample, a two stage sampling method was used. The second stage sample was balanced on gender, ethnicity, age, adiposity status, and PROP sensitivity to enable a cost efficient test of the extent to which diet, PA, and related variables mediated or moderated that relationship (Baranowski, Baranowski, Beltran, Watson, Jago, Callie, et al., 2010). Children or adolescents were excluded from participating with medical conditions or medications that interfered with taste, diet, or physical activity, or with developmental limitations that affected their ability to understand or provide age appropriate responses to the questions posed during testing.
The design in the current analyses, which was an exploratory secondary analysis of the original data, was cross sectional with a sample of 568. Of the 304 9–10 year old children, 49 were White girls, 56 were Black girls, 52 were Hispanic girls, 48 were White boys, 52 were Black boys, and 47 were Hispanic boys. Of the 264 17–18 year old adolescents, 42 were White females, 51 were Black females, 55 were Hispanic females, 41 were White males, 43 were Black males, and 32 were Hispanic males. Upon approval by the school district, and in turn the principals (n=9) of the elementary and high schools with greater than 30% ethnic minority representation from the Houston Independent School District (HISD) and the classroom teachers, research assistants visited classrooms with large concentrations of 9, 10, 17, or 18 year olds and provided information packets to those who expressed an interest in participating. Packets included information about the study, contact information for study staff, consent forms, and screening questionnaires regarding inclusion/exclusion criteria for parents to review. Eligible youth who returned signed consent forms from their parents (n=1690) enrolled in the first stage sample (Baranowski et al., 2010). A second stage sample (n = 843) was enrolled to efficiently collect detailed data on diet and PA.
Recruitment and data collection were conducted over three years to efficiently use skilled staff. Thus, recruitment in some schools occurred up to six times (twice per year). All staff were trained annually. Although 843 participants were accepted for the larger study, 100 considered themselves as part of “other” ethnic groups and 175 were missing data on two or more variables and therefore not included in this sample. The study was approved by the Baylor College of Medicine Institutional Review Board; the parents of all children completed informed consent and all children provided assent.
Procedure
Parents completed a family demographic questionnaire, which included their child’s medical history and household income. Child anthropometry and self-report questionnaires were conducted at school at times arranged with administrators (during non-academic class time for elementary school children; before school hours for high school students).
Measurements
Weight (kg) was measured using a SECA Alpha 882 scale from SECA Corporation (Hamburg, Germany). Height (cm) was measured using a PE-AIM-101 Stadiometer from Perspective Enterprises (Olney, Maryland). BMI for age z-score was calculated with the CDC computerized program using the averaged height and weight measurements (Kuczmarski, Ogden, Guo, Grummer-Strawn, Flegal, Mei, et al., 2002). WC (cm) was measured using a tape with tensioning device (a Gulick Measuring Tape from Fitness Wholesale; Park Twinsburg, OH). Triceps skinfold (mm) was measured using a Lange skinfold caliper from Body Trends (West Palm Beach, FL). All measurements were collected twice and averaged. Trained and certified research staff collected all measurements using standard protocols (Lohman, Roche, & Martorell, 1988; NHANES, 2000). The three adiposity indicator variables were highly inter-correlated (≥ .690). A principle components analysis revealed one component (i.e., factor or latent variable) represented 87% of the shared variance, representing global adiposity. As a result, a composite index was computed averaging the normalized values of BMI z-score, WC, and triceps skinfolds. Higher scores indicated greater adiposity.
The Dutch Eating Behavior Questionnaire (DEBQ) (Van Strien, et al., 1986) provides self-reported continuous scale scores for three types of overeating: external, emotional, and restrained. At the start of data collection a children’s version of the DEBQ was not available; thus, modifications were made to the existing adolescent and adult version. While the original version of the DEBQ was appropriate to use with the adolescents in this sample (17–18 year olds), it was desired to use the same measure of overeating among all youth (9–10 year olds and 17–18 year olds) in this sample. Because measures designed for children are often simpler and easier to understand by adults (Resnicow, Davis, Smith, Baranowski, Lin et al., 1998) yet maintain good psychometric characteristics, it was believed a simplified measure the younger children could understand would be understood by the adolescents, rather than the reverse. For the current study, the wording was simplified, the response options were restricted from five-point Likert scale (“never” to “very often”) to “yes” or “no,” as children used mostly two response categories (Watson, Baranowski, & Thompson, 2006; Watson, Baranowski, Thompson, Jago, Baranowski, Klesges, et al., 2006). Since the data from this study were collected, a 20-item version of the DEBQ (DEBQ-C) was published for children ages 7–12 (Van Strien & Oosterveld, 2008). In the current study, only those items consistent with the 20 DEBQ-C items were retained. A confirmatory factor analysis was completed to determine whether the items fit the three dimensional structure. The model included 20-items consistent with the DEBQ-C items and demonstrated adequate fit X2(79, N=568) = 309.45, TLI=.94, and RMSEA=.07. All item standardized coefficients were significant (p<.001) and ranged from .57 to .85 except for one item from the External Eating subscale (“Can you stop yourself from eating tasty food?”) which had a standardized coefficient of −.18 and one item from the Restrained Eating subscale (“Do you try to eat less than normal when you gain weight?”) which had a standardized coefficient of .17. Thus, these items were removed leaving an 18-item model which continued to demonstrate adequate fit, X2(65, N=586) = 261.28, TLI=.95, and RMSEA=.07, with standardized coefficients (all p<.001) ranging from .57–.85. Cronbach’s alphas were .77 (emotional eating; 7-items), .84 (restrained eating; 6-items), and .74 (external eating; 5-items) indicating acceptable internal consistency. Thus, an 18-item version of the DEBQ for children (9–10 years of age) and adolescents (17–18 years of age) demonstrated satisfactory dimensional stability and good internal consistency to measure external, restrained, and emotional eating styles.
Social Desirability of Response was measured with the “Lie Scale” from the Revised Children’s Manifest Anxiety Scale (Reynolds & Paget, 1983). This 9-item measure of the degree to which responses may be biased by a desire to present oneself in a socially desirable manner was normed on a large sample of diverse children aged 6–19 from 13 states in the United States (Reynolds & Paget, 1983). Social Desirability as measured by the Lie Scale has confounded associations between BMI and self-reported dietary intake, physical activity behaviors, weight concerns, and dieting behaviors among children (Klesges, et al., 2004); therefore it was used in this study to control for the effect of social desirability on the hypothesized associations.
Statistical Analyses
Preliminary data inspection assured no violation of the assumptions of normality, linearity, multicollinearity, and homoscedascticity. Pearson correlations were conducted between dependent (BMI, triceps skinfold, waist circumference, and adiposity composite index) and independent variables (restrained, emotional, and external eating). Four mixed model linear regression analyses predicted adiposity (BMI z-score, Triceps Skinfold, Waist Circumference, and global adiposity index) from demographics, type of eating style (adjusted for social desirability) and interaction effects (eating style by each demographic variable) with backward deletion of non-significant two-way interactions. Because race in this study was a 3-group categorical variable (African American, Hispanic, and White) and a regression approach, which requires numerical variables, was used, it was necessary to create two dummy variables to represent race with Whites serving as the referent group. The models were adjusted for the clustering effect of nine schools. Standardized betas (std beta) were presented to assess the magnitude of the association between the independent and dependent variables. Analyses were performed using SAS version 9.2 (2008, SAS Institute Inc., Cary, NC). The level of significance was set at p<0.05.
Results
There were no significant differences between those included and those who were not on age, gender, income, or any of the adiposity measures. The sample was composed of 304 multiethnic elementary age children (ages 9–10) and 264 high school adolescents (ages 17–18). Social desirability was significantly correlated with the emotional eating (r = .21, p < .001) and restrained eating (r = .09, p = .03) subscales of the 18-item version of the DEBQ used in this study. As a result, the residuals resulting from regressing the emotional and restrained eating subscale scores on the Social Desirability score were used in the multivariate analyses.
Relationships among eating styles and adiposity measures
All four adiposity indicators were highly and significantly inter-correlated (r’s >.78; Tables 1 & 2). All three overeating styles were significantly and positively inter-correlated, although correlations were weak (r’s <.22). Among 9–10 year old girls, restrained eating was not significantly correlated with any measures of adiposity; and emotional eating and external eating were significantly inversely related to all measures of adiposity. Among 9–10 year old boys, restrained eating was significantly and positively related to all measures of adiposity; external eating was significantly and inversely related to all measures of adiposity; but emotional eating was not significantly related to any measures of adiposity. Among 17–18 year old females, emotional eating was not significantly correlated with any measures of adiposity; external eating was significantly and inversely correlated with all measures of adiposity; and restrained eating was only significantly correlated in a positive direction with BMI z-score but not other measures of adiposity. Among 17–18 year old boys, restrained eating was significantly and positively correlated with all measures of adiposity emotional eating was not significantly correlated with any measures of adiposity; and external eating was significantly inversely correlated with all measures of adiposity except BMI z-score.
Table 1.
Correlations between independent and dependent variables among 9–10 years old.
| Global Adiposity Index | BMI z score | Triceps skinfold | WC | Restraint | Emotional Eating | External Eating | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | M | F | M | F | M | F | M | F | |
| Global Adiposity Index |
1 | 1 | ||||||||||||
| BMI z score |
.90*** | .92*** | 1 | 1 | ||||||||||
| Triceps skinfold (mm) |
.97*** | .94*** | .84*** | .82*** | 1 | 1 | ||||||||
| WC (cm) |
.97*** | .96*** | .86*** | .87*** | .90*** | .82*** | 1 | 1 | ||||||
| Restraint (a = .84) |
.29*** | .13 | .31** | .16 | .27** | .10 | .27** | .12 | 1 | 1 | ||||
| Emotional Eating (a = .77) |
−.03 | −.25** | .02 | −.19* | −.03 | −.26** | −.06 | −.24*** | .17* | −.02 | 1 | 1 | ||
| External Eating (a = .74) | −.31*** | −.30*** | −.29*** | −.30*** | −.30*** | −.27** | −.31*** | −.28*** | .09 | .22** | .17* | .22** | 1 | 1 |
p<.05,
p<.01,
p<.001, a indicates Cronbach’s alpha of internal consistency reliability; these analyses did not control for social desirability of response.
Table 2.
Correlations between independent and dependent variables among 17–18 years old.
| Global Adiposity Index | BMI z score | Triceps skinfold | WC | Restraint | Emotional Eating | External Eating | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | M | F | M | F | M | F | M | F | |
| Global Adiposity Index |
1 | 1 | ||||||||||||
| BMI z score |
.86*** | .90*** | 1 | 1 | ||||||||||
| Triceps skinfold (mm) |
.95*** | .92*** | .78*** | .80*** | 1 | 1 | ||||||||
| WC (cm) |
.99*** | .95*** | .85*** | .86*** | .91*** | .80*** | 1 | 1 | ||||||
| Restraint (a = .84) |
.23* | .13 | .24* | .27** | .21* | .15 | .24** | .10 | 1 | 1 | ||||
| Emotional Eating (a = .77) |
<.01 | −.01 | .09 | −.02 | −.03 | .01 | −.01 | .01 | −.15 | .13 | 1 | 1 | ||
| External Eating (a = .74) | −.21* | −.24 | −.09 | −.28 | −.26** | −.22** | −.19* | −.19* | .09 | .11 | −.04 | .19* | 1 | 1 |
p<.05,
p<.01,
p<.001, a indicates Cronbach’s alpha of internal consistency reliability; these analyses did not control for social desirability of response.
Relationships between eating styles and adiposity controlling for demographics
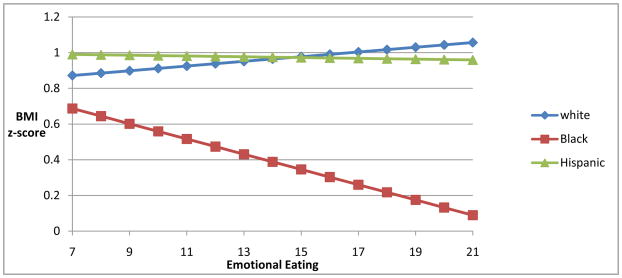
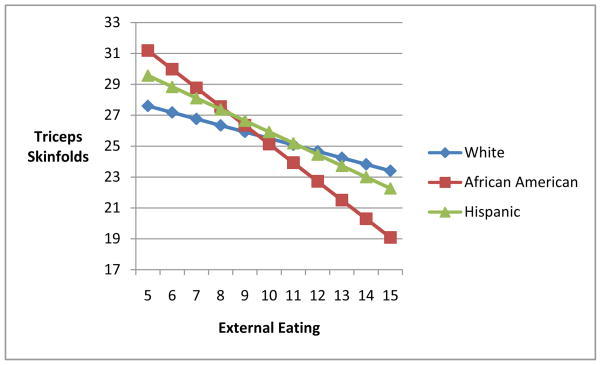
Results for the relationships between external and restrained eating with all adiposity indicators, except triceps skinfold, were similar. External eating was inversely related and restrained eating was positively related to global adiposity index, BMI z-score, and WC after controlling for demographic variables and social desirability (Table 3). Restrained eating was positively related to triceps skinfold after controlling for demographic variables and social desirability. There was a significant ethnic group by emotional eating interaction effect for the global adiposity index, BMI z-score (figure 1), and WC after controlling for demographics and social desirability. After controlling for demographics and social desirability, among Hispanic and White youth adiposity (BMI z-score, WC, and global adiposity) did not change as emotional eating increased, but among African American youth, adiposity (BMI z-score, WC, and composite adiposity index) decreased as emotional eating increased. There was also an ethnic group by external eating interaction effect showing a significantly stronger inverse relationship between external eating and triceps skinfold among African American youth than Hispanic or White youth (figure 2). African American ethnicity contributed significantly to triceps skinfold variance (Std. Beta=.44; p<.05; mixed model linear regression data not shown). White or Hispanic ethnicity did not contribute significantly to the variance in any of the adiposity measures (mixed model linear regression data not shown).
Table 3.
Impact on adiposity by demographic variables, eating styles, and interaction effects.
| Adiposity Indicators (Dependent Variables) | ||||
|---|---|---|---|---|
| Independent Variables | Adiposity Composite | BMI z-score | Triceps Skinfold | Waist Circumference |
| Adj R2 = .34 | Psuedo R2 = .12 | Adj R2 = .21 | Adj R2 = .43 | |
| Standardized Beta | Standardized Beta | Standardized Beta | Standardized Beta | |
| Eating Styles |
||||
| Restrained Eating | .21*** | .27*** | .25*** | .17*** |
| External Eating | −.24*** | −.26*** | −.13 | −.20*** |
| Emotional Eating |
.05 | .05 | −.04 | .02 |
| Interactions |
||||
| Afr. Amer.X EmEat (referent group: White) | −.13* | −.12* | - | −.11* |
| Afr. Amer. X ExterEat (referent group: White) | - | - | −.47** | - |
Models adjusted for social desirability, gender, age, race, and income.
p<.05,
p<.01,
p<.001
Figure 1.
Race by emotional eating interaction on BMI z-score.
Slope for Black youth (referent group: White): −.12 (p<.05)
Slope for White and Hispanic youth (referent group: White): Non Significant
Figure 2.
Race by external eating interaction on triceps skinfold.
Slope for African American youth (referent group: White): −.47 (p<.01)
Slope for White and Hispanic (referent group: White): Non Significant
Discussion
Restrained eating was positively related to adiposity without moderation effects of gender, age, or ethnicity, and has been consistently positively related to adiposity in samples of European male and female children and adolescents (Braet, et al., 2008; Lluch, et al., 2000; Snoek, et al., 2007). While restraint theory posits that overeating occurs as a rebound response to chronic dieting (Herman & Polivy, 1980), recent longitudinal research among adolescents (Snoek, et al., 2008) and adults (Chavance et al., 2010) showed that over time adiposity predicted restrained eating rather than restrained eating predicting adiposity. Weight gain or self-perception of excess adiposity likely prompts food restriction or at least restraint from overeating (Stice, Sysko, Roberto, & Allison, 2009).
Gender and age did not moderate the relationship between external eating and adiposity in this sample, but African American youth demonstrated a stronger inverse relationship between external eating and triceps skinfold than White or Hispanic youth. Because the interaction effect did not appear for global adiposity, the ethnic group interaction effect for triceps skinfold represented differences on some unique variance in triceps skinfold not related to global adiposity. Among children and adolescents, body composition and fat distribution varied across ethnic groups after controlling for BMI (Sisson, Katzmaryzyk, Srinivasan, Chen, Freedman, Bouchard, et al, 2009). Because triceps skinfold reflects subcutaneous fat distribution, the moderation effect found here may reflect ethnic group differences on fat distribution more so than differences on external eating.
Contrary to Externality theory predictions (Schachter & Rodin, 1974), external eating was significantly inversely related to global adiposity, BMI, and WC regardless of demographic variables or social desirability. Some have suggested that positive relationships between external eating and adiposity do not emerge until adulthood (Snoek, et al., 2007); however the fact that age was not a moderator in this study with the oldest youth in the 17–18 year age range (cusp of early adulthood) diminishes the strength of this argument. It has been suggested social desirability may bias children’s accurate report of their own thoughts and feelings related to their eating behaviors, thereby leading to inverse associations between external eating and adiposity (Braet, et al., 2008). However, social desirability of response on eating style self report was statistically controlled in the current study. Others suggest children may not be able to provide insightful self-report data (Braet, et al., 2008), and experimental research showed that overeating in response to environmental cues was automatic and occurred without conscious awareness of the impact of environmental cues on intake (Wansink, 2004; Wansink, et al., 2007). It’s possible that youth may be less aware than adults of the impact of the environment on their intake. Another possibility is related to habituation. In food habituation the desire for food decreases with repeated exposure during the course of a meal (Epstein, Temple, Roemmich, & Bouton, 2009). It is possible that if children are repeatedly served highly palatable energy dense foods, not only may these children be more likely to gain weight and become obese, but their sensitivity to environmental food cues to these foods may decrease as well. Conflicting results have been reported on the relationship of externality to adiposity among youth with differences by gender (Braet, et al., 2008; Lluch, et al., 2000; Snoek, et al., 2007) and age (Braet, et al., 2008). One recent study showed no association between adiposity and external eating even among adults in the Netherlands (Van Strien, et al., 2009). More research is needed to explore the construct of external eating and its association with adiposity. Self-report may not be a valid way of measuring this construct.
The relationship between emotional eating and most adiposity indicators was moderated by race when controlling for demographic characteristics and social desirability. More specifically, African American youth demonstrated an inverse relationship, while White youth and Hispanic youth showed no relationship between emotional eating and adiposity. Neither age nor gender was significant moderators of the relationships between any adiposity indicators and emotional overeating. The normal response to emotional distress is a reduction in energy intake (Gold & Chrousos, 2002). African American youth in this sample with higher adiposity were more likely to experience normal healthy downregulation of energy intake during times of distress. Prevalence of overweight and obesity is higher among African American youth than White youth (Ogden, et al., 2010), but research has also shown disinhibited overeating patterns are not as prevalent among African American youth as other ethnic groups (Gluck & Geliebter, 2002). In addition, minority adults have less awareness of their own status as overweight or obese than non-Hispanic Whites (Dorsey, Eberhardt, & Ogden, 2009). Thus, while overweight/obese may be misperceived it is generally accepted within the African American community and not reflective of eating patterns associated with loss of control and disinhibition.
In other studies, one showed no relationship between emotional eating and adiposity among male and female adolescents, but there was a significant positive relationship among women (Lluch, et al., 2000); another showed there were gender and age differences (Braet, et al., 2008); and a third study showed no association for adolescent girls, but an inverse association for adolescent boys (Snoek, et al., 2007). Inconsistent findings between and within these prior studies may have occurred because ethnicity was not accounted for and it appears to moderate this relationship (Braet, et al., 2008; Lluch, et al., 2000; Snoek, et al., 2007).
Because BMI z-score, triceps skinfold, and WC are all indicators of adiposity and there is measurement error associated with each. All three were combined into a composite index of the shared variance representing global adiposity (Bollen, 1989; Chavance, et al., 2010; Marshall, et al., 1990). The global adiposity index was useful in studying the associations between overeating styles and adiposity. BMI z-score performed similarly to the global adiposity index in this sample suggesting it remains the best choice if only one measure of adiposity is used. Despite the fact that WC was not age or gender adjusted and is prone to measurement error, it too performed similarly to the composite index, in that the same significant relationships were seen, but they were weaker. Variations in significant relationships for triceps skinfold with overeating styles and demographic variables suggest this measure of adiposity among youth should be used with caution or at least not in isolation. Triceps skinfold is subject to substantial measurement error, represents only a localized point of fat distribution (Krebs, Himes, Jacobson, Nicklas, Guilday, & Styne, 2007), and is not age or gender adjusted. Future research should emphasize composite indicators.
Limitations
The data were cross-sectional which does not permit conclusions about causality. Self-report data assumes adequate cognitive abilities; self-awareness of thoughts, feelings, and behaviors; appropriate interpretation of items; and accurate self perceptions and memory of behaviors, which may not be true of all children. The DEBQ was adapted for the current study (i.e., changed response options, simplified wording of items, and removed items that were not adding meaningfully to the overall latent variable model), but it demonstrated adequate reliability and confirmatory factor analysis showed the items to strongly fit the underlying latent variables. While the sample was large and evenly distributed across racial, gender, and age groups, it is possible some moderation effects (i.e., age and gender) were not detected because they may be very weak and require a larger sample to detect. This sample consisted of a multiethnic group of children and adolescents, they were primarily lower income and urban, which may limit generalizability. While adiposity was measured with multiple indicators obtained by trained technicians, the current gold standard for body composition measurement is full body DXA scanning, which was not feasible for data collected in schools.
Conclusion
No relationships were moderated by age or gender, after controlling for demographics and social desirability. Among youth from several ethnic groups common in the US, restrained eating was positively related to adiposity. Ethnicity moderated the effects of emotional eating on most measures of adiposity and the effects of external eating on triceps skinfolds only. Some of the results regarding external eating were opposite Externality Theory predictions; future research should examine potential reasons for this. The moderating effect of ethnicity for external and emotional eating suggests potential ethnic group differences in fat distribution and eating behaviors; future research should explore these cultural differences. After adjusting for demographics and social desirability, overeating styles appeared to have a role in adiposity in nearly all youth.
Acknowledgments
This research was funded by the National Institute of Health, grant R01 CA 116766. In addition, this work is a publication of the USDA/ARS Children’s Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine and Texas Children’s Hospital, Houston, Texas. This project has been funded in part by federal funds from the USDA/ARS under Cooperative Agreement 58-6250-6001. The contents of this publication do not necessarily reflect the views or policies of the USDA nor mention of trade names, commercial products or organizations imply endorsement by the U.S. Government. In addition, this work is a publication of the USDA/ARS Children’s Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine and Texas Children’s Hospital, Houston, Texas. This project has been funded in part by federal funds from the USDA/ARS under Cooperative Agreement 58-6250-6001. The contents of this publication do not necessarily reflect the views or policies of the USDA nor mention of trade names, commercial products or organizations imply endorsement by the U.S. Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tracey Ledoux, Email: TALedoux@uh.edu.
Kathy Watson, Email: kwatson@bcm.edu.
Janice Baranowski, Email: jbaranow@bcm.edu.
Beverly J. Tepper, Email: Tepper@aesop.rutgers.edu.
Tom Baranowski, Email: tbaranow@bcm.edu.
References
- Baranowski JC, Baranowski T, Beltran A, Watson KB, Jago R, Callie M, et al. 6-n-Propylthiouracil sensitivity and obesity status among ethnically diverse children. Public Health Nutr. 2010;13(10):1587–1592. doi: 10.1017/S1368980009993004. [DOI] [PubMed] [Google Scholar]
- Bedogni G, Iughetti L, Ferrari M, Malavolti M, Poli M, Bernasconi S, et al. Sensitivity and specificity of body mass index and skinfold thicknesses in detecting excess adiposity in children aged 8–12 years. Annals of Human Biology. 2003;30(2):132–139. doi: 10.1080/0301446021000033409. [DOI] [PubMed] [Google Scholar]
- Bohon C, Stice E, Spoor S. Female emotional eaters show abnormalities in consummatory and anticipatory food reward: a functional magnetic resonance imaging study. International Journal of Eating Disorders. 2009;42(3):210–221. doi: 10.1002/eat.20615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York, NY: Wiley; 1989. [Google Scholar]
- Braet C, Claus L, Goossens L, Moens E, Van Vlierberghe L, Soetens B. Differences in eating style between overweight and normal-weight youngsters. Journal of Health Psychology. 2008;13(6):733–743. doi: 10.1177/1359105308093850. [DOI] [PubMed] [Google Scholar]
- Braet C, Van Strien T. Assessment of emotional, externally induced and restrained eating behaviour in nint to twelve-year old obese and non-obese children. Behavior Research Theory. 1997;35:863–873. doi: 10.1016/s0005-7967(97)00045-4. [DOI] [PubMed] [Google Scholar]
- Bruch H. Psychological Aspects of Overeating and Obesity. Psychosomatics. 1964;5:269–274. doi: 10.1016/s0033-3182(64)72385-7. [DOI] [PubMed] [Google Scholar]
- Burton P, Smit HJ, Lightowler HJ. The influence of restrained and external eating patterns on overeating. Appetite. 2007;49:191–197. doi: 10.1016/j.appet.2007.01.007. [DOI] [PubMed] [Google Scholar]
- Chavance M, Escolano S, Romon M, Basdevant A, de Lauzon-Guillain B, Charles MA. Latent variables and structural equation models for longitudinal relationships: an illustration in nutritional epidemiology. BMC Medical Research Methodology. 2010;10:37. doi: 10.1186/1471-2288-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das UN. Obesity: Genes, brain, gut, and environment. Nutrition. 2010:1–15. doi: 10.1016/j.nut.2009.09.020. [DOI] [PubMed] [Google Scholar]
- Dorsey RR, Eberhardt MS, Ogden CL. Racial/ethnic differences in weight perception. Obesity (Silver Spring) 2009;17(4):790–795. doi: 10.1038/oby.2008.603. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Temple JL, Roemmich JN, Bouton ME. Habituation as a determinant of human food intake. Psychological Reviews. 2009;116(2):384–407. doi: 10.1037/a0015074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faith MS, Heshka S, Keller KL, Sherry B, Matz PE, Pietrobelli A, et al. Maternal-child feeding patterns and child body weight: findings from a population-based sample. Archives of Pediatric Adolescent Medicine. 2003;157(9):926–932. doi: 10.1001/archpedi.157.9.926. [DOI] [PubMed] [Google Scholar]
- Faith MS, Scanlon KS, Birch LL, Francis LA, Sherry B. Parent-child feeding strategies and their relationships to child eating and weight status. Obesity Research. 2004;12(11):1711–1722. doi: 10.1038/oby.2004.212. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Ogden CL, Yanovski JA, Freedman DS, Shepherd JA, Graubard BI, et al. High adiposity and high body mass index-for-age in US children and adolescents overall and by race-ethnic group. American Journal of Clinical Nutritrition. 2010;91(4):1020–1026. doi: 10.3945/ajcn.2009.28589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fogelholm M, Lichtenbelt WvM. Comparison of body composition methods: a literature analysis. European Journal of Clinical Nutrition. 1997;51:495–503. doi: 10.1038/sj.ejcn.1600448. [DOI] [PubMed] [Google Scholar]
- Freedman DS, Wang J, Ogden CL, Thornton JC, Mei Z, Pierson RN, et al. The prediction of body fatness by BMI and skinfold thicknesses among children and adolescents. Annals of Human Biology. 2007;34(2):183–194. doi: 10.1080/03014460601116860. [DOI] [PubMed] [Google Scholar]
- Gluck ME, Geliebter A. Racial/ethnic differences in body image and eating behaviors. Eating Behaviors. 2002;3:143–151. doi: 10.1016/s1471-0153(01)00052-6. [DOI] [PubMed] [Google Scholar]
- Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs low CRH/NE states. Molecular Psychiatry. 2002;7(3):254–275. doi: 10.1038/sj.mp.4001032. [DOI] [PubMed] [Google Scholar]
- Herman CP, Polivy J. Restrained Eating. Philadelphia, PA: Saunders; 1980. [Google Scholar]
- Hervey GR. Regulation of energy balance. Nature. 1969;222(5194):629–631. doi: 10.1038/222629a0. [DOI] [PubMed] [Google Scholar]
- Hughes SO, Patrick H, Power TG, Fisher JO, Anderson CB, Nicklas T. The impact of child care providers’ feeding on children’s food consumption. Journal of Developmental and Behavioral Pediatrics. 2007;28:100–107. doi: 10.1097/01.DBP.0000267561.34199.a9. [DOI] [PubMed] [Google Scholar]
- Iannotti RJ, O’Brien RW, Spillman DM. Parental and peer influences on food consumption of preschool African-American children. Perceptual Motor Skills. 1994;79(2):747–752. doi: 10.2466/pms.1994.79.2.747. [DOI] [PubMed] [Google Scholar]
- Kaiser LL, Martinez NA, Harwood JO, Garcia LC. Child feeding strategies in low-income Latino households: focus group observations. Journal of American Dietetic Association. 1999;99(5):601–603. doi: 10.1016/S0002-8223(99)00148-0. [DOI] [PubMed] [Google Scholar]
- Klesges LM, Baranowski T, Beech B, Cullen K, Murray DM, Rochon J, et al. Social desirability bias in self-reported dietary, physical activity and weight concerns measures in 8- to 10-year-old African-American girls: results from the Girls Health Enrichment Multisite Studies (GEMS) Preventive Medicine. 2004;38(Suppl):S78–87. doi: 10.1016/j.ypmed.2003.07.003. [DOI] [PubMed] [Google Scholar]
- Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S193–228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital & Health Statistics-Series II: Data from the National Health Survey. 2002;246:1–190. [PubMed] [Google Scholar]
- Lluch A, Herbeth B, Mejean L, Siest G. Dietary intakes, eating style and overweight in the Stanislas Family Study. International Journal of Obesity and Related Metabolic Disorders. 2000;24(11):1493–1499. doi: 10.1038/sj.ijo.0801425. [DOI] [PubMed] [Google Scholar]
- Lohman TG, Roche AF, Martorell R. Anthropometric Standardizatin Reference Manual. Champaign, IL: Human Kinetics Books; 1988. [Google Scholar]
- Lynch WC, Heil DP, Wagner E, Havens MD. Ethnic differences in BMI, weight concerns, and eating behaviors: comparison of Native American, White, and Hispanic adolescents. Body Image. 2007;4(2):179–190. doi: 10.1016/j.bodyim.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall JD, Hazlett CB, Spady DW, Quinney HA. Comparison of convenient indicators of obesity. American Journal of Clinical Nutrition. 1990;51(1):22–28. doi: 10.1093/ajcn/51.1.22. [DOI] [PubMed] [Google Scholar]
- Mei Z, Grummer-Strawn LM, Wang J, Thornton JC, Freedman DS, Pierson RN, Jr, et al. Do skinfold measurements provide additional information to body mass index in the assessment of body fatness among children and adolescents? Pediatrics. 2007;119(6):e1306–1313. doi: 10.1542/peds.2006-2546. [DOI] [PubMed] [Google Scholar]
- National Health and Nutrition Examination Survey. Anthropometry Procedures Manual. Atlanta, GA: Centers for Disease Control; 2001. [Google Scholar]
- Ness-Abramof R, Apovian CM. Waist circumference measurement in clinical practice. Nutrition in Clinical Practice. 2008;23(4):397–404. doi: 10.1177/0884533608321700. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Croll J, Story M, Hannan PJ, French SA, Perry C. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: findings from Project EAT. Journal of Psychosomatic Research. 2002;53(5):963–974. doi: 10.1016/s0022-3999(02)00486-5. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. Journal of the American Medical Association. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- Olvera-Ezzell N, Power TG, Cousins JH. Maternal socialization of children’s eating habits: strategies used by obese Mexican-American mothers. Child Development. 1990;61(2):395–400. doi: 10.1111/j.1467-8624.1990.tb02785.x. [DOI] [PubMed] [Google Scholar]
- Pernick Y, Nichols JF, Rauh MJ, Kern M, Ji M, Lawson M, et al. Disordered eating among a multi-racial/ethnic sample of female high-school athletes. Journal of Adolescent Health. 2006;38:689–695. doi: 10.1016/j.jadohealth.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Davis M, Smith M, Baranowski T, Lin LS, Baranowski J, et al. Results of the TeachWell worksite wellness program. American Journal of Public Health. 1998;88:250–257. doi: 10.2105/ajph.88.2.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds C, Paget K. National normative and reliability data for the revised children’s manifest anxiety scale. Social Psychological Review. 1983;12:324–336. [Google Scholar]
- Ricciardelli LA, McCabe MP, Williams RJ, Thompson JK. The role of ethnicity and culture in body image and disordered eating among males. Clinical Psychological Reviews. 2007;27(5):582–606. doi: 10.1016/j.cpr.2007.01.016. [DOI] [PubMed] [Google Scholar]
- Schachter S, Rodin J. Obese humans and rats. Washington DC: Erlbaum/Halstead; 1974. [Google Scholar]
- Schmidt MD, Dwyer T, Magnussen CG, Venn AJ. Predictive associations between alternative measures of childhood adiposity and adult cardio-metabolic health. International Journal of Obesity. 2010 doi: 10.1038/ijo.2010.205. [DOI] [PubMed] [Google Scholar]
- Sisson SB, Katzmarzyk PT, Srinivasan SR, Chen W, Freedman DS, Bouchard C, et al. Ethnic differences in subcutaneous adiposity and waist girth in children and adolescents. Obesity (Silver Spring) 2009;17(11):2075–2081. doi: 10.1038/oby.2009.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snoek HL, Van Strien T, Janssens JM, Engels RC. Emotional, external, restrained eating and overweight in Dutch adolescents. Scandinavian Jouranl of Psychology. 2007;48(1):23–32. doi: 10.1111/j.1467-9450.2006.00568.x. [DOI] [PubMed] [Google Scholar]
- Snoek HL, Van Strien T, Janssens JMAM, Engels RCME. Restrained eating and BMI: A longitudinal study among adolescents. Health Psychology. 2008;27:753–759. doi: 10.1037/0278-6133.27.6.753. [DOI] [PubMed] [Google Scholar]
- Snoek HM, Engels RC, Janssens JM, van Strien T. Parental behaviour and adolescents’ emotional eating. Appetite. 2007;49(1):223–230. doi: 10.1016/j.appet.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Stevens J. BMI and mortality: sorting through the data to find the public health message. International Journal of Obesity (Lond) 2008;32(5):727–729. doi: 10.1038/ijo.2008.35. [DOI] [PubMed] [Google Scholar]
- Stevens J, McClain JE, Truesdale KP. Selection of measures in epidemiologic studies of the consequences of obesity. International Journal of Obesity (Lond) 2008;32(Suppl 3):S60–66. doi: 10.1038/ijo.2008.88. [DOI] [PubMed] [Google Scholar]
- Stice E, Sysko R, Roberto CA, Allison S. Are dietary restraint scales valid measures of dietary restriction? Additional objective behavioral and biological data suggest not. Appetite. 2009;54(2):331–339. doi: 10.1016/j.appet.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Strien T, Frijters JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. International Journal of Eating Disorders. 1986;5:295–315. [Google Scholar]
- Van Strien T, Herman CP, Verheijden MW. Eating style, overeating, and overweight in a representative Dutch sample. Does external eating play a role? Appetite. 2009;52(2):380–387. doi: 10.1016/j.appet.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Van Strien T, Oosterveld P. The Children’s DEBQ for assessment of restrained, emotional, and external eating in 7- to 12-year-old children. International Journal of Eating Disorders. 2008;41:72–81. doi: 10.1002/eat.20424. [DOI] [PubMed] [Google Scholar]
- Van Strien T, Snoek HM, van der Zwaluw CS, Engels RC. Parental control and the dopamine D2 receptor gene (DRD2) interaction on emotional eating in adolescence. Appetite. 2010;54(2):255–261. doi: 10.1016/j.appet.2009.11.006. [DOI] [PubMed] [Google Scholar]
- Wansink B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annual Reviews Nutrition. 2004;24:455–479. doi: 10.1146/annurev.nutr.24.012003.132140. [DOI] [PubMed] [Google Scholar]
- Wansink B, Payne CR, Chandon P. Internal and external cues of meal cessation: the French paradox redux? Obesity (Silver Spring) 2007;15(12):2920–2924. doi: 10.1038/oby.2007.348. [DOI] [PubMed] [Google Scholar]
- Watson K, Baranowski T, Thompson D. Item response modeling: an evaluation of the children’s fruit and vegetable self-efficacy questionnaire. Health Educ Res. 2006;21(Suppl 1):i47–57. doi: 10.1093/her/cyl136. [DOI] [PubMed] [Google Scholar]
- Watson K, Baranowski T, Thompson D, Jago R, Baranowski J, Klesges LM. Innovative application of a multidimensional item response model in assessing the influence of social desirability on the pseudo-relationship between self-efficacy and behavior. Health Educ Res. 2006;21(Suppl 1):i85–97. doi: 10.1093/her/cyl137. [DOI] [PubMed] [Google Scholar]
- White MA, Grilo CM. Ethnic differences in the prediction of eating and body image disturbances among female adolescent psychiatric inpatients. International Journal of Eating Disorders. 2005;38:78–84. doi: 10.1002/eat.20142. [DOI] [PubMed] [Google Scholar]