Abstract
Considerable controversy exists regarding the optimal management of elderly patients with type II odontoid fractures. There is uncertainty regarding the consequences of non-union. The best treatment remains unclear because of the morbidity associated with prolonged cervical immobilisation versus the risks of surgical intervention. The objective of the study was to evaluate the published literature and determine the current evidence for the management of type II odontoid fractures in elderly. A search of the English language literature from January 1970 to date was performed using Medline and the following keywords: odontoid, fractures, cervical spine and elderly. The search was supplemented by cross-referencing between articles. Case reports and review articles were excluded although some were referred to in the discussion. Studies in patients aged 65 years with a minimum follow-up of 12 months were selected. One-hundred twenty-six articles were reviewed. No class I study was identified. There were two class II studies and the remaining were class III. Significant variability was found in the literature regarding mortality and morbidity rates in patients treated with and without halo vest immobilisation. In recent years several authors have claimed satisfactory results with anterior odontoid screw fixation while others have argued that this may lead to increased complications in this age group. Lately, the posterior cervical (Goel–Harms) construct has also gained popularity amongst surgeons. There is insufficient evidence to establish a standard or guideline for odontoid fracture management in elderly. While most authors agree that cervical immobilisation yields satisfactory results for type I and III fractures in the elderly, the optimal management for type II fractures remain unsolved. A prospective randomised controlled trial is recommended.
Keywords: Odontoid, Fracture, Cervical spine, Elderly
Introduction
In most countries, the elderly are the most rapidly growing segment of society, and it is estimated that by 2025, almost a fifth of the population will be over the age of 65 [33]. In this review, we have arbitrarily considered patients above 65 years as elderly. Patients in this age group are vulnerable to cervical spine injuries with the upper cervical (C0–C2) spine being involved in more than 50% of the time [34, 49, 60, 61, 63, 67, 80]. Fracture of the odontoid process of the axis is commonest with majority being Anderson and D’Alonzo type II fractures. Cervical spine fractures in the elderly are potentially life threatening, and it has been reported that following traumatic spinal cord injury, the in-hospital as well as 1-year mortality rates in patients above 65 years is up to eightfold higher [16, 22, 40, 41]. In spite of the relative frequency of odontoid fractures (OF) in the elderly, there is lack of agreement regarding the optimal management especially with type II fractures with no published standards or guidelines to date. A Medline search of the English language literature for all published articles on odontoid fractures in the elderly after 1970 was performed. Studies in patients aged greater than 65 years and with follow-up of at least 12 months were included. Case reports and review articles were excluded although some were referred to in the discussion. The aim of this article was to review the literature and summarise the evidence for and against each treatment option for the management of OFs in patients above 65 years.
Aetiology and classification
Although fractures of the odontoid occur in all age groups, younger patients often sustain these injuries after motor vehicle accidents while older patients present after low-energy falls and are less likely to have severe neurological deficits [10, 32, 60, 63, 68]. The mechanism responsible for odontoid fractures is generally agreed to be hyperflexion or hyperextension of the cervical spine [60]. Moradian [58] and Doherty [18] demonstrated in biomechanical studies that type II OFs result from lateral bending and extension forces. Neurological injury is averted by the relatively larger diameter of the cervical spinal canal at this level [10, 36, 80]. However, when present, it can be fatal due to the high level of spinal cord injury.
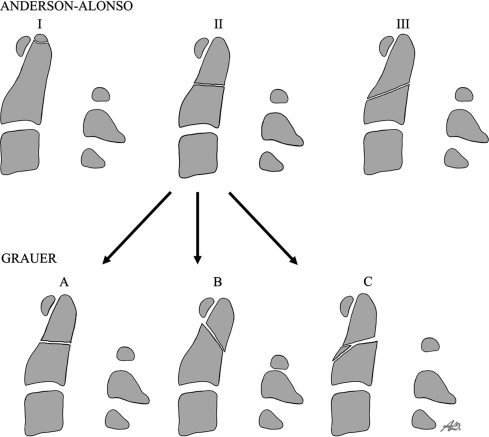
In 1974, Anderson and D’Alonzo [2] proposed a classification system of odontoid fractures based on fracture pattern. Type I fractures were described to be near the tip of the odontoid process, above the transverse ligament and were considered stable. Type II fractures occur at the base of the odontoid, between the level of the transverse ligament and the body of the axis. They are the commonest type and are considered unstable. Type III fractures extend into the vertebral body and are relatively stable unless significantly displaced. Although this is the most widely accepted classification, two limitations of this classification have been highlighted. First is the difficulty in precise differentiation between a low type II and a high type III fractures; the second is the lack of distinction between fractures in terms of fracture line obliquity, displacement and comminution which has an impact on subsequent management. To address the first limitation, Hadley et al. [31] introduced a type IIA fracture subclass to the classification, defined as a type II fracture complicated by an additional chip-fracture fragment at the anterior or posterior aspect of the base of the odontoid. In order to address the second limitation of the Anderson and D’Alonzo classification, Grauer et al. [28] further classified type II fractures into three subtypes (Fig. 1) based on fracture line obliquity, displacement and comminution into IIA, B and C to guide treatment options. Type IIA was defined as a minimally or non-displaced fracture with no comminution which could be treated with external immobilisation. Type IIB was a displaced fracture extending from anterior–superior to posterior-inferior, or a transverse fracture which are amenable to anterior screw fixation if reducible assuming adequate bone density. Type IIC was a fracture extending from anterior–inferior to posterior superior or a fracture with significant comminution which are generally treated with posterior stabilisation. Prospective application of this classification system is yet to be performed.
Fig. 1.
Schematic diagram for type II odontoid fractures
Fracture classification systems fulfil many roles, prediction of outcome and categorisation for research being but two. A generic critique of classifications is that they do not consider clinically relevant factors such as bone mineral density, physiological age rather than chronological age and co-morbidity that might influence treatment selection. All systems should be subject to inter and intra observer error studies to validate the reliability of a classification system.
Management options
When considering the optimal treatment for a type II OF in the elderly, several factors need to be taken into consideration including associated injuries, medical co-morbidities [American Society of Anaesthesiologists (ASA) grade], healing potential of fracture, anticipated tolerance of the halo vest (HV) or surgery and patients wishes [3, 6, 34, 37, 46, 63, 70]. Treatment options remain controversial because of the risks of operative intervention versus the morbidity associated with prolonged cervical immobilisation. In the literature, four separate treatment options are described including rigid and non-rigid immobilisation, anterior screw fixation of the odontoid and posterior fusion of the C1/2 complex. However, in most studies, the number of patients is limited, and often more than one treatment option has often been used. The presence of radiological osseous union has been used as a standard to determine the optimal treatment outcome [59]. However, some authors have argued that a stable fibrous union in an asymptomatic patient above 65 years may well be acceptable [34, 49, 59, 68]. The various treatment options in the elderly and the pros and cons of each as mentioned in the published English literature are discussed below.
Non-rigid external immobilisation
The use of non-rigid external immobilisation using a hard cervical collar is a recognised form of treatment for type II odontoid fractures in the elderly. In an earlier study from our institution on ‘Cervical spine injuries in the elderly’ in 1994 [49], we mentioned that the ‘aims of treatment are very different in the young and elderly’. We also stated that bony union is not always necessary in the elderly, and that stable fibrous union may be an acceptable result. In this study, majority of the 11 patients with type II OF were treated with a rigid collar, and all achieved stable union. Although the number of patients in this study was too low to make any conclusion, we believe it raised an important point which has also been addressed by other authors [34, 49, 59, 63, 68]. Hanigan et al. [34] concluded that in the elderly, fibrous union of the odontoid is an adequate goal, and that a rigid collar provides sufficient immobilisation. Ryan et al. [68] reported on 29 patients with type II OFs treated with external immobilisation ranging from collar to HV (rigid immobilisation). Although there was a 77% non-union rate, no evidence of late neurological deterioration was evident on follow-up. They mentioned that “vigorous attempts to secure both primary union and a sound arthrodesis for non-union were questionable in the elderly except in unusual circumstances”. They concluded that myelopathy was a rare consequence of non-union, and that a good functional outcome in this age group was less dependent on radiographic criteria for union and more dependent on return to pain-free, independent living, regardless of union rate. Pepin et al. [63] described 19 elderly patients with OF, and supported the use of a rigid collar. Muller et al. [59] treated 19 stable type II OF with a mean age of 59.1 years in a hard cervical collar, and reported a 77% osseous union. When stable, asymptomatic fibrous union was included as a favourable outcome, the success rate increased to 92%. He could not find any correlation between radiological findings and clinical outcome, and concluded that non-union of the odontoid could be stable, without clinical symptoms, and therefore, do not necessarily imply a poor clinical outcome.
Rigid external immobilisation
The HV was first developed by Perry and Nickel [64] for stabilisation of patients with poliomyelitis. Over the last few decades it has undergone several modifications in design and materials with consequent expansion of its indications. Presently it offers an advantage over all other cervical orthosis in terms of limitation of movement in the upper cervical spine. Johnson et al. [44] estimated that without restriction, in flexion and extension at the C1–C2 level, there was movement of 13.4° compared to 8.5° in the Philadelphia collar and 3.4° with the HV. Several authors have proposed immobilisation by HV as the treatment of choice for type II OFs in the elderly [19, 21, 51, 52, 69, 71, 73] while others have suggested a more cautious approach for its use in this age group quoting morbidity and mortality figures of up to 51 and 40%, respectively [25, 34, 39, 49, 50, 55, 60, 63, 77, 80]. There is considerable variability in the literature with acceptable fusion rate ranging from less than 50 to 90% [6, 12, 31, 45, 47, 48, 59, 68, 79].
In the first published series of complications of the use of HV in the patients aged 70 years or more, Horn et al. [39] reported a combined morbidity of 52% and mortality of 19%. Amongst the 42 patients in their series, there were 23 patients with OFs (Anderson and D’Alonzo classification of the fractures not specified), and halo brace was applied in a total of 21 patients. Tashijan et al. [77] reviewed 78 patients greater than 65 years (mean age 80.7 years) with odontoid fractures. There were 50 type II OFs in their study. Thirty-eight patients were treated with HV while 27 had collar and 13 were operated. There was no difference in injury severity score (ISS) or baseline medical conditions within the HV and non-HV patients. The mortality and morbidity rates in HV patients were 42 and 66% while that in the non-HV patients were 20 and 36%, respectively. Majercik et al. [55] claimed that the use of HV in the elderly was similar to a ‘death sentence’. They retrospectively reviewed the use of the HV in elderly patients with cervical spine injuries. In this study, the fracture types were not described. They divided patients into two groups with similar ISS and co-morbidities within the subgroups: old (>66 years, n = 129) and young (18–65 years, n = 289). They found that following cervical spine trauma, older patients died at nearly four times the rate of their younger counterparts (21 vs. 5%). In addition, old patients with HV had a much higher mortality than young patients with HV (40 vs. 2%, p < 0.001) as well as compared to old patients treated with surgery or collar (6 and 12%). However, in a recent prospective cohort study of complications associated with HV immobilisation for cervical spine injuries, Van Middendorp et al. [78] claimed lower rates of mortality (8%) and pneumonia (4%) amongst elderly patients. It is difficult to identify reasons for this large difference in mortality and morbidity in comparison to other published studies. The ASA grades were not stated precisely making direct comparison with other published papers impossible.
Amongst the 239 patients in this study, there were 79 patients aged more than 65 years. Isolated HV was offered to 61% and the remaining had HV supplemented with surgery. Although the total number of minor complications were substantial, the authors claimed that ‘awareness of and responsiveness to minor complications can prevent the subsequent development of serious morbidities and perhaps reduce mortality’.
Surgical fixation
As a result of the unacceptably high mortality and morbidity rates of HV immobilisation, several authors have recommended early surgical stabilisation in elderly patients with type II OFs [1, 6, 7, 13, 23, 46, 48]. Over the last few decades, there has been an evolution of posterior arthrodesis techniques ranging from C1/2 wiring described by Gallie [24] to transarticular screws described by Magerl [53] and to the more recent C1 lateral mass and C2 pars interarticularis screw introduced by Goel [26, 27] and modified by Harms and Melcher [33]. Amongst the surgical options, posterior fixation techniques of the C1/2 complex had been previously suggested as the most effective option. The posterior wiring technique for OFs has been shown to achieve fusion rates of 80–100% [5, 54] as compared to 23–82% for non-operative treatment of type II fractures [2, 12, 59, 63, 68, 73]. Most studies have used HV concurrently. The transarticular screw fixation offers a much more stable construct than wiring with fusion rates approaching 100% [4, 13, 17, 18, 42]. The procedure is technically demanding and carries the risk of vertebral artery injury [75, 80]. Goel [26] in 1994 described the use of C1 lateral mass and C2 pedicle screw for posterior atlanto-axial fixation. Subsequently, Harms and Melcher [35] in 2001 reported a modification of this technique using polyaxial screws and rod. This Goel/Harms C1/2 fixation is comparable to the transarticular screw fixation in terms of fusion but with lower vascular and neurological risks [35, 75, 81]. The superior and medial placement of the C2 pars screw involves less risk to the vertebral artery. Regarding C1 lateral mass screw placement, there is a risk of damaging the internal carotid artery and the hypoglossal nerve, if anterior surface of C1 lateral mass is penetrated as reported by Currier [15] and Ebraheim et al. [20]. Tan et al. [76] suggested screw insertion through the posterior arch of C1 avoiding injury to the venous plexus by Goel’s insertion technique through the caudal base of C1 posterior arch.
Unfortunately, posterior arthrodesis eliminates approximately 50% of cervical rotation [4] which led to the development of an alternative stabilisation technique for type II odontoid fractures, namely, direct stabilisation with anterior screw fixation which was first described by Bohler [8, 9]. This procedure offers immediate spinal stability, preserves normal C1/2 rotation and is associated with a high fusion rate without the need for concurrent HV immobilisation. It also offers rapid patient mobilisation and what many authors believe, the best anatomical and functional results for the treatment of OFs in the elderly. The use of one or two screws has been debated [29]. However, no significant differences between the two techniques have been found either in biomechanical stability [56] or in fusion rates [43]. However, concerns have been raised regarding the feasibility of this technique in elderly patients with osteoporosis. Diminished bone quantity, poor bony healing from osteoporosis, advanced patient’s age and increased anaesthetic risks leading to a higher failure rate with this technique in the elderly has been claimed [3, 30, 70]. Other authors believe that as osteoporosis is mainly a cancellous disease and since the technique of anterior odontoid screw fixation is dependent on the distal tip of screw purchasing the dense cortical bone, it may not significantly affect the manner of screw purchase [8]. Wolfgang et al. [11] performed a case–control study of 27 patients with type II OFs to determine whether patients above 70 years have less favourable outcome than younger patients with this technique. They demonstrated that the procedure can be successfully performed in the elderly and with low mortality and morbidity.
Discussion
Due to lack of class I studies, no definitive conclusions can be drawn regarding the optimal treatment of type II OFs in the elderly. Table 1 lists some of the recent published studies on the management of type II odontoid fractures in elderly. The majority of the data is class III evidence, and unfortunately due to the heterogeneous nature of these studies with regard to patient selection, co-morbidities, lack of clear definition of fracture subtype with age as well as combinations of treatment offered in different studies; a systematic analysis of the each treatment outcome is difficult. Treatment remains controversial due to the high rate of non-union. Anderson and D’Alonzo [2] suggested that when fractures were treated non-surgically, type II produced late non-union more often than type III fractures. Several theories exist to explain this [45]. The presence of a watershed zone (between two vascular arcades) as well as a synovial capsule within the dens that does not receive periosteal blood, the relative predominance of cortical over cancellous bone at the base of the dens and the distraction provided by the apical ligaments that create a physical gap are factors that retard bone healing. Other specific factors that have been debated to contribute to non-union include patients age, degree and direction of dens displacement (>4–6 mm), dens angulation greater than 10°, fracture malalignment during follow-up and delayed treatment [20, 30, 31, 48, 51, 68]. Most authors have noted a significant difference in fracture healing when analysing the effect of age on outcome while some have found this not to be the case [22, 70].
Table 1.
Some of the published studies in the last 15 years on type II odontoid fractures in elderly
| Author & year | Level of evidence | Description of study | Outcome |
|---|---|---|---|
| [72] | III | A retrospective cohort study of operative versus non-operative treatment of isolated type II OF in the octogenarian population. 72 patients with mean age of 85 years without neurologic deficits were included. 32 patients received operative (10 anterior and 22 posterior) and 40 patients received nonsurgical treatment. The acute in-hospital outcome was determined. | Mortality (15%) in the non-operative & operative groups were 15% & 12.5% respectively. This was not statistically significant (P>0.05). The percentage of patients experiencing at least one significant complication was higher in the operative group than the non-operative group (62% vs. 35%, respectively, P<0.05). Type II OF in the octogenarian population are associated with substantial morbidity/mortality, irrespective of management method. |
| Koech 2008 | III | One of the largest studies to date. To investigate the functional outcome after non-operative management of type II OF in elderly. Retrospective analysis from a prospective database. 42 patients with median age 80 years–10(collar) & 32(HV) followed up for mean 24 months. | Osseous union- 50%(collar) & 37.5%(HV). Fracture stability- 90%(collar) & 100%(HV). No difference in outcome between osseous & stable fibrous union. The latter may be an adequate aim in the elderly. |
| [72] | III | This study examined trends in surgical management of acute type II OF in the past 20 years at a regional spinal cord injury centre. 75 patients with a mean age of 82 years were included. Among other analyses, the type of surgical procedure and distribution of surgical technique over time were determined. | Logistic fit of surgical technique by year indicated a significant increase (P<.05) in the use of C1 lateral mass and C2 isthmus/pedicle constructs, no significant change in the use of transarticular (Magerl) fixation and a decline in the use of odontoid screws. Patients undergoing the latter procedure were significantly more likely to develop swallowing or vocal cord problems compared to the other surgical procedures (P<.01) |
| [65] | III | A case-control study analysing retrospective data from a prospective database examining 90 patients with a mean age of 69 years who had undergone non-operative treatment for OF. To determine the long-term results after rigid immobilization using a HV and to identify specific risk factors for failure of halo immobilization. The followup was for at least 2 years. | Overall fusion rate noted was 84%. 83% returned to preinjury level within 1 year. The Smiley-Webster scale showed an overall functional outcome score of 1.64. Therefore satisfactory outcome with HV. Nonunion was found significantly more often in older patients and in those with displaced OF. Secondary loss of reduction & delay of treatment were further risk factors for nonfusion. |
| [23] | III | Retrospective analysis of posterior transarticular C1/2 fixation of OF in elderly in 27 patients with mean age of 85 years. Comparison of outcome with that reported for HV in published literature. | 95% fusion rate within 3 months. Combined and perioperative mortality of 21% and 11% which was much lower than that reported for HV (42-52%) |
| Platzer 2006 | III | Retrospective analysis of functional and radiographic results after anterior screw fixation for type II OF between young (< 65 years) and elderly patients with a follow up of at least 2 years. | Morbidity 22% in elderly and 8% in young. Mortality 9% in elderly and 1% in young. Nonunion rate of 12% & 4% in elderly and young. |
| [77] | III | Review of a series of OF in elderly patients and evaluation of in-hospital morbidity/mortality between those treated with and without HV with similar injury severity scores and medical condition in either group. | Mortality- HV(42%); non HV(20%). Morbidity- HV(66%); non HV(36%) |
| [55] | III | To evaluate the outcome in young and elderly with cervical spine fractures treated with HV, collar & surgery. 129 old(> 79 years) & 289 young(< 38 years) recruited. Study period of 80 months. | Very poor outcome of HV in elderly Mortality with HV- elderly(40%); young(2%) Mortality within the elderly subgroup: surgery(6%); collar(12%) |
| [59] | III | Retrospective analysis of the outcome of non-rigid immobilization for stable OF treated over a 15 year period. 19 type II & 7 type III fractures included. The mean age of the patients was 59 years. | The overall fusion rate was 73.7% (type II) & 85.7% (type III). Clinical outcome did not correlate with the radiological findings. Stable type II and type III fractures of the odontoid can be successfully treated with non-rigid immobilisation |
| [11] | III | To determine whether patients aged 70 years or older with Type II OF have a less favorable outcome than younger patients with anterior odontoid screw(AOS) fixation. Case-control study of 27 patients —15 patients > 70 years (Group 1) and 12 patients < 70 years (Group 2). Mean follow-up was 16.6 months. | Fusion rates : 73% in Group 1 & 75% in Group 2. Additional dorsal stabilization was performed in 13% of cases in Group 1 & 17% of cases in Group 2. Complications occurred in 20% of cases in Group 1 and 8% of cases in Group 2. Outcome after AOS fixation is not affected by patient age. Slightly higher rates of medical complications did not reach statistical significance. |
| [48] | II | Case controlled study to evaluate age as a risk factor for failure of HV in treatment of type II OF. 33 patients selected- 11 cases and 22 controls. | Odds ratio of data indicated that risk of HV immobilization was 21 times greater in patients aged 50 years or more |
| [37] | III | A retrospective review of 10 patients with a mean age of 80 years withtype II OF who underwent anterior odontoid screw fixation were reviewed. All patients were placed in a rigid external orthosis (five halos and five collars) after surgery. | Nine patients were alive at a mean of 10 months post surgery. Dynamic radiographs demonstrated stable fusion in 8/9 patients. Peri-operative morbidity and mortality was 20% & 10% respectively. Authors commented that odontoid screw fixation is safe in elderly patients |
| [46] | III | A retrospective review to investigate the role of surgical & nonsurgical treatment in elderly patients with Type II OF who were consecutively admitted to a single medical center over a 5-year period. 20 patients included with mean age of 80 years. 8 offered surgery and 12 nonsurg. 3 patients crossed over to the surgical group later. The mean follow up was 14 months. | Nonsurgical treatment with a HV(7), Minerva brace (3) or collar (2) resulted in a 50% early failure rate (six of 12 patients) with 10% morbidity & 10% mortality, whereas surgery was well tolerated, resulting in a 9% early failure rate with 9% morbidity & mortality respectively.. |
| [60] | III | Retrospective analysis of fractures of the odontoid in patients over 70 years of age with regard to the aetiology, natural history and the treatment of fractures of the dens in this age group. This data was then compared to those of a contemporary series of patients less than 70 years of age. 23 patients with a mean age of 80 years and 54 patients with a mean age of 47 years were included. Followup was for 44 months. | Treatment offered in elderly was operative in 21.7% (5 ant screw)& non-opearative in 78.3% (15 collar and 3 HV). In younger group 31.5% were operated and 78.5% managed conservatively. The overall complication rate was significantly higher in elderly (52.2% vs. 32.7%), with an in-hospital mortality of 34.8%. Elderly patients with a fracture of the odontoid are a high-risk group with a high morbidity /mortality. |
| [70] | III | To determine by age and fracture type which treatment regimen provided the best functional outcome in young and old patients with dens fractures. 37 Type II and 20 Type III fractures. 29 patients were under & 28 over 60 years age. Treatment offered were post C1-2 fixation(6); HV(46) & collar(5). The follow up duration was 2.4 years. | Older patients treated surgically did not have a statistically better functional outcome score than those treated non-operatively (P < 0.8). The surgical group did not have a statistically improved outcome than the non-operative group. |
| [66] | III | Retrospective analysis of Philadelphia collar vs. HV for management of OF. 57 patients included–36 type II(20 HV, 16 collar) & 18 type III(18 HV, 5 collar). For type II OF, median age : collar(69 yrs), HV(44 yrs). Mean follow up was 8 months. | No statistical advantage shown by either treatment in terms of stability, fracture healing or need for late surgical repair. Suggested that either treatment could be used equivalently |
| [68] | III | Retrospective review of the outcome of 30 patients > 60 years age with type II OF. 29 were managed conservatively with collar or HV and 1 underwent surgery. The mean follow-up was 21 months. | The non-union rate was 77%. Myelopathy as a late complication of non-union was not observed. The data suggested that vigorous attempts to secure both primary union and a sound arthrodesis for non-union are questionable in the elderly except in unusual circumstances. |
One of the controversies regarding the treatment of type II OFs is whether a stable non-union is an acceptable outcome in the elderly patients. Osseous union is an easily defined measurable outcome and arguably the ideal goal of treatment. It is defined by evidence of bony trabeculae crossing the fracture site, absence of motion on dynamic flexion/extension views and absence of sclerotic borders adjacent to the fracture site [67]. Fine-cut CT scans with helical reconstruction can be obtained if the adequacy of bony fusion is unclear on standard X-rays. In contrast, a stable non-union or fibrous union is described when clinically the patient is asymptomatic, and in the absence of osseous union, dynamic X-rays show no instability at the site of fracture [38, 49, 59, 65, 68]. The views of several authors that stable fibrous union may be an adequate functional aim of treatment in the elderly has to be seriously considered in the light of the published results [34, 49, 59, 68]. One of the arguments against this is the development of delayed myelopathy in patients with established non-union of the odontoid [2, 14]. Although this is a recognised risk, the actual risk of progression is unknown and may take several years [57, 74]. Even in younger, more active patients, myelopathy may not occur till 13.5 years of post-injury [62]. Thus, a fibrous non-union in the elderly population is probably acceptable in functional terms and not associated with significant risk of myelopathy.
Bohler [8] emphasised that non-union of the odontoid is an absolute indication for surgery. However, successful non-operative management of stable non-union in the elderly has also been described. Hart et al. [38] followed a series of elderly patients with chronic, mobile odontoid non-union without myelopathy with non-operative treatment. None of the patients developed myelopathic symptoms during the follow-up period (4 years and 7 months). Unless gross instability is present, many authors have favoured the role of external immobilisation either with a collar or HV. In a recent biomechanical in vivo analysis of atlanto-axial motion in a group of 20 young normal adults immobilised with the HV or Philadelphia collar, the authors demonstrated that under extremes of flexion and extension, there was no significant difference in restriction of sagittal motion at C1–C2 when using the collar instead of the HV [47]. They concluded that the use of the Philadelphia collar is sufficient for the treatment of stable odontoid fractures. The reported fracture union rates after conservative treatment of type II OFs vary between 23 and 82% [2, 12, 59, 63, 73]. In the only study directly comparing the outcomes of OFs treated with HV and collar by Polin et al. [66], no statistically significant difference was found between the two treatment modalities although a trend towards higher fusion rate was found with HV (47 vs. 26%). The authors emphasised that this difference was probably as a result of the significant age difference between the two groups (44 years with the HV and 68 years in the collar subgroup).
In the last two decades, the problems with HV in the elderly have been increasingly highlighted by several authors with complication rates of up to 51%. The risks of pneumonia (up to 34%) as well as cardiac arrest (up to 26%) have been especially worrying. In one of the few class II studies on OFs, Lennarson et al. [48] evaluated age as a risk factor for failure of halo immobilisation in patients with type II OF. The odds ratio of their data indicated that the risk of failure of halo immobilisation was 21 times higher in patients aged 50 years or more. However, in their recent study, Van Middendorp et al. claimed much lower rates of mortality (8%) and pneumonia (4%) during HV immobilisation. At the same time, one cannot ignore the complications associated with the HV in the long lists of published studies from several institutions to date. In summary, HV remains an alternative treatment option in selected patients, but may be associated with higher risk of complications compared with hard collar in the elderly.
The association of elevated non-union rates with conservative treatment and the morbidity and mortality associated with HV in the elderly led to a trend towards operative fixation of type II OFs, especially unstable fractures based on evidence that early surgery in neurologically intact elderly patients leads to decreased morbidity and mortality [6, 48]. The technique of anterior odontoid screw has gained wide acceptance over the years with osseous union rates of 88–100% [1, 7, 11], and has been claimed by several authors to be the procedure of choice for treatment of type II OFs. Apart from immediate stabilisation of the fracture site, its principal advantage is the near preserved range of neck motion due to the sparing of the C1–C2 joint. Nevertheless, some authors have reported complication rates using this technique in the elderly [3, 28, 70]. Smith, Vaccaro and colleagues [72] recently reviewed the trends in the surgical management for type II OFs at a regional spinal cord injury centre. The mean age of their cohort was 82.3 years. Over a 20-year period, they noted an evolution of surgical technique from posterior cervical wiring to posterior transarticular fixation and more recently C1 lateral mass and C2 pedicle/isthmus screw (Goel–Harms) constructs. The increase in the use of the Goel–Harms technique relative to other posterior fixation methods was statistically significant. In their cohort, posterior methods for fixation were used much more frequently than anterior odontoid screw fixation. The latter was associated with a significantly higher rate of postoperative pneumonia and swallowing dysfunction compared with posterior instrumentations. In a retrospective cohort study of operative versus non-operative treatment of isolated type II odontoid fractures in patients aged 80 years or more, Smith et al. [71] noted a similar overall mortality rate between the surgical and conservatively managed patients (12.5 vs. 15%). However, the morbidity rate was much higher in the surgical group (62 vs. 42%) although this was not statistically significant. They concluded that the management of type II odontoid fractures in the octogenarian population are associated with substantial morbidity and mortality, irrespective of the management method.
Caution has to be exercised in the interpretation of the literature regarding surgery for OF. There is inherently a publication bias towards reported good outcomes, with a relative paucity of patients in the 65–80+ years group. If the latter are included, an uniform adjuvant description of the performance index, ASA status and co-morbidities are lacking. These factors are potentially more important in determining outcome from OF treatment than the surgical procedure per se. This lack of detail makes comparison between studies very difficult. Notwithstanding the above, interpretation of the data suggests that surgery for the grossly unstable type II OF is probably worthwhile provided that the patient is fit and has few co-morbidities.
Conclusion
Several articles have addressed the treatment of odontoid fractures in elderly. The definition of elderly has been different, and the separation of type II OFs according to age groups have not been uniform in most studies. In this article, we have tried to summarise the views of various authors on this controversial subject focussing on the pros and cons of each treatment option. The ideal treatment for type II OFs in the elderly is that which would provide the best possible functional outcome with least associated risk and not simply the best radiological outcome alone. While it is true that osseous union is a measurable absolute outcome measure, the views of several authors that stable fibrous union may be an adequate aim of treatment in the elderly cannot be ignored. It is evident that each treatment option has a role, and that management has to be individualised. Non-rigid hard collar is a low risk option for the conservative treatment in the elderly, particularly if there is significant co-morbidity that might preclude operative treatment. HV immobilisation in the elderly does have a significant potential complication rate. Its use should be carefully considered in this group with significant co-morbidities and prior poor performance index. Surgery is indicated in a limited group of patients with unstable fractures. There are no comparative studies prospectively comparing surgical options. A multicentre prospective randomised controlled trial would clarify some of the uncertainty to better inform treatment options. Until better evidence is available, practical wisdom and judgement in the treatment of individuals with this injury permits a variety of acceptable treatment options.
References
- 1.Aebi M, Etter C, Coscia M. Fractures of the odontoid process. Treatment with anterior screw fixation. Spine. 1989;14:1065–1070. doi: 10.1097/00007632-198910000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 3.Andersson S, Rodrigues M, Olerud C. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9:56–59. doi: 10.1007/s005860050009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93:227–236. doi: 10.3171/spi.2000.93.2.0227. [DOI] [PubMed] [Google Scholar]
- 5.Appuzo ML, Heiden JS, Weiss MH, Ackerson TT, Harvey JP, Kurze T. Acute fractures of the odontoid process. An analysis of 45 cases. J Neurosurg. 1978;48(1):85–91. doi: 10.3171/jns.1978.48.1.0085. [DOI] [PubMed] [Google Scholar]
- 6.Bednar DA, Parikh J, Hummel J. Management of type II odontoid process fractures in geriatric patients: a prospective study of sequential cohorts with attention to survivorship. J Spinal Disord. 1995;8:166–169. [PubMed] [Google Scholar]
- 7.Berlemann U, Schwarzenbach O. Dens fractures in the elderly: results of anterior screw fixation in 19 elderly patients. Acta Orthop Scand. 1997;68:319–324. doi: 10.3109/17453679708996169. [DOI] [PubMed] [Google Scholar]
- 8.Bohler J. Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am. 1982;64:18–27. [PubMed] [Google Scholar]
- 9.Bohler J. Operative treatment of injuries to cervical spine. Orthop Rev. 1986;15(1):58–59. [PubMed] [Google Scholar]
- 10.Bohlmann HH. Acute fractures and dislocations of the cervical spine: an analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg. 1979;61:1119–1142. [PubMed] [Google Scholar]
- 11.Börm W, Kast E, Richter HP, et al. Anterior screw fixation in Type II odontoid fractures: is there a difference in outcome between age groups. Neurosurgery. 2003;52:1089–1094. [PubMed] [Google Scholar]
- 12.Clark CR, White AA., III Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67:1340–1348. [PubMed] [Google Scholar]
- 13.Coyne TJ, Fehlings MG, Wallace MC, et al. C1–C2 posterior cervical fusion: long-term evaluation of results and efficacy. Neurosurgery. 1995;37:688–793. doi: 10.1227/00006123-199510000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Crockard A, Heilman A, Stevens J. Progressive myelopathy secondary to odontoid fractures: clinical, radiographic and surgical features. Neurosurgery. 1993;78:579–586. doi: 10.3171/jns.1993.78.4.0579. [DOI] [PubMed] [Google Scholar]
- 15.Currier BL, Todd LT, Maus TP, Fisher DR, Yamzemski MJ. Anatomic relationship of the internal carotid artery to the C1 vertebra: a case report of cervical reconstruction for chordoma and pilot study to assess the risk of screw fixation of the atlas. Spine. 2003;28:E461–E467. doi: 10.1097/01.BRS.0000092385.19307.9E. [DOI] [PubMed] [Google Scholar]
- 16.DeVivo MJ, Kartus PL, Stover SL, Rutt RD, Fine PR. Seven-year survival following spinal cord injury. Arch Neurol. 1987;44:872–875. doi: 10.1001/archneur.1987.00520200074023. [DOI] [PubMed] [Google Scholar]
- 17.Dickman CA, Sontagg VK. Posterior C1-C2 Transarticular screw fixation for atlantoaxial arthrodesis. Neurosurgery. 1998;43(2):275–280. doi: 10.1097/00006123-199808000-00056. [DOI] [PubMed] [Google Scholar]
- 18.Doherty BJ, Heggeness MH, Esses SI. A biomechanical study of odontoid fractures and fracture fixation. Spine. 1993;18:178–184. doi: 10.1097/00007632-199302000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Dunn ME, Seljeskog EL. Experience in the management of odontoid process injuries: an analysis of 128 cases. Neurosurgery. 1986;18:306–310. doi: 10.1227/00006123-198603000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Ebraheim NA, Misson JR, Xu R, Yeasting RA. The optimal transarticular c1–2 screw length and the location of the hypoglossal nerve? Surg Neurol. 2000;53(3):208–210. doi: 10.1016/s0090-3019(00)00160-9. [DOI] [PubMed] [Google Scholar]
- 21.Ekong CE, Schwartz ML, Tator CH, et al. Odontoid fracture: management with early mobilization using the halo device. Neurosurgery. 1981;9:631–637. doi: 10.1227/00006123-198112000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Fassett DR, Harrop JS, Maltenfort M, et al. Mortality rates in geriatric patients with spinal cord injuries. J Neurosurg Spine. 2007;7(3):277–281. doi: 10.3171/SPI-07/09/277. [DOI] [PubMed] [Google Scholar]
- 23.Frangen TM, Zilkens C, Muhr G, Schinkel C. Odontoid fractures in the elderly: dorsal C1/C2 fusion is superior to halo-vest immobilization. J Trauma. 2007;63:83–89. doi: 10.1097/TA.0b013e318060d2b9. [DOI] [PubMed] [Google Scholar]
- 24.Gallie WE. Fractures and dislocations of the cervical spine. Am J Surg. 1939;3:495–499. [Google Scholar]
- 25.Glaser JA, Whitehill R, Stamp WG, Jane JA. Complications associated with the halo-vest. A review of 245 cases. J Neurosurg. 1986;65:762–769. doi: 10.3171/jns.1986.65.6.0762. [DOI] [PubMed] [Google Scholar]
- 26.Goel A, Leheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir. 1994;129:47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 27.Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery. 2002;51:1351–1357. [PubMed] [Google Scholar]
- 28.Grauer JN, Shafi B, Hilibrand AS, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5:123–129. doi: 10.1016/j.spinee.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 29.Graziano G, Jaggers C, Lee M, et al. A comparative study of fixation techniques for Type II fractures of the odontoid process. Spine. 1993;18:2383–2387. doi: 10.1097/00007632-199312000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Greene KA, Dickman CA, Marciano FF, Drabier J, Drayer BP, Sonntag VK. Transverse atlantal ligament disruption associated with odontoid fractures. Spine. 1994;19:2307–2314. doi: 10.1097/00007632-199410150-00010. [DOI] [PubMed] [Google Scholar]
- 31.Hadley MN, Browner CM, Liu SS, et al. New subtype of acute odontoid fractures (type IIA) Neurosurgery. 1988;22:67–71. doi: 10.1227/00006123-198801010-00010. [DOI] [PubMed] [Google Scholar]
- 32.Hadley MN, Dickman CA, Browner CM, et al. Acute axis fractures: a review of 229 cases. J Neurosurg. 1989;71:642–647. doi: 10.3171/jns.1989.71.5.0642. [DOI] [PubMed] [Google Scholar]
- 33.Hagen S (1999) CBO memorandum: projections of expenditures for long-term care services for the elderly. Congressional Budget Office, Washington, DC
- 34.Hanigan WC, Powell FC, Elwood PW, et al. Odontoid fractures in elderly patients. J Neurosurg. 1993;78:32–35. doi: 10.3171/jns.1993.78.1.0032. [DOI] [PubMed] [Google Scholar]
- 35.Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 36.Harrop JS, Sharan AD, Przybylski GJ. Epidemiology of spinal cord injury after acute odontoid fractures. Neurosurg Focus. 2000;8(6):e4. [PubMed] [Google Scholar]
- 37.Harrop JS, Przybylski GJ, Vaccaro AR, et al. Efficacy of anterior odontoid screw fixation in elderly patients with Type II odontoid fractures. Neurosurg Focus. 2000;8(6):e6. [PubMed] [Google Scholar]
- 38.Hart R, Saterbak A, Rapp T, Clark C. Nonoperative management of dens fracture nonunion in elderly patients without myelopathy. Spine. 2000;25(11):1339–1343. doi: 10.1097/00007632-200006010-00004. [DOI] [PubMed] [Google Scholar]
- 39.Horn E, Theodore N, Feiz-Erfan I, Lekovic GP, Dickman C, Sonntag VKH. Complications of halo fixation in the elderly. J Neurosurg Spine. 2006;5:46–49. doi: 10.3171/spi.2006.5.1.46. [DOI] [PubMed] [Google Scholar]
- 40.Irwin AN, Arthur M, Mullins RJ, Hart RA. Variations in injury patterns, treatment and outcome for spinal fractures and paralysis in adult versus geriatric patients. Spine. 2004;29:796–802. doi: 10.1097/01.brs.0000119400.92204.b5. [DOI] [PubMed] [Google Scholar]
- 41.Jackson AP, Haak MH, Khan N, Meyer PR. Cervical spine injuries in the elderly: acute postoperative mortality. Spine. 2005;30:1524–1527. doi: 10.1097/01.brs.0000167822.75063.8c. [DOI] [PubMed] [Google Scholar]
- 42.Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992;5:464–475. doi: 10.1097/00002517-199212000-00012. [DOI] [PubMed] [Google Scholar]
- 43.Jenkins JD, Coric D, Branch CL. A clinical comparison of one- and two-screw odontoid fixation. J Neurosurg. 1998;89:366–370. doi: 10.3171/jns.1998.89.3.0366. [DOI] [PubMed] [Google Scholar]
- 44.Johnson R, Hart D, Simmons E. Cervical orthoses: a study comparing their effectiveness in restricting cervical motion in normal subjects. J Bone Joint Surg Am. 1977;59:332–339. [PubMed] [Google Scholar]
- 45.Koivikko MP, Kiuru MJ, Koskinen SK, Myllynen P, Santavirta S, Kivisaari L. Factors associated with non-union in conservatively-treated type-II fractures of the odontoid process. J Bone Joint Surg Br. 2004;86:1146–1151. doi: 10.1302/0301-620x.86b8.14839. [DOI] [PubMed] [Google Scholar]
- 46.Kuntz C, 4th, Mirza SK, Jarell AD, Chapman JR, Shaffrey CL, Newell DW. Type II odontoid fractures in the elderly: early failure of nonsurgical treatment. Neurosurg Focus. 2000;8:E7. doi: 10.3171/foc.2000.8.6.8. [DOI] [PubMed] [Google Scholar]
- 47.Koller H, Zenner J, Hitzl W, Ferraris L, Resch H, Tauber M, Auffarth A, Lederer S, Mayer M. In vivo analysis of atlantoaxial motion in individuals immobilised with the halo thoracic vest or Philadelphia collar. Spine. 2009;34(7):670–679. doi: 10.1097/BRS.0b013e31819c40f5. [DOI] [PubMed] [Google Scholar]
- 48.Lennarson PJ, Mostafavi H, Traynelis VC, Walters BC. Management of type II dens fractures: a case-control study. Spine. 2000;25:1234–1237. doi: 10.1097/00007632-200005150-00006. [DOI] [PubMed] [Google Scholar]
- 49.Lieberman IH, Webb JK. Cervical spine injuries in the elderly. J Bone Joint Surg Br. 1994;76:877–881. [PubMed] [Google Scholar]
- 50.Lind B, Bake B, Lundqvist C, Nordwall A. Influence of halo vest treatment on vital capacity. Spine. 1987;12:449–452. doi: 10.1097/00007632-198706000-00005. [DOI] [PubMed] [Google Scholar]
- 51.Lind B, Nordwall A, Sihlbom H. Odontoid fractures treated with halo-vest. Spine. 1987;12:173–177. doi: 10.1097/00007632-198703000-00014. [DOI] [PubMed] [Google Scholar]
- 52.Maak, Travis G, Grauer, Jonathan N (2006) The contemporary treatment of odontoid injuries. Spine 31(11S):S53–S60 [DOI] [PubMed]
- 53.Magerl F, Seeman PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A, editors. Cervical spine. Wien: Springer; 1986. pp. 267–278. [Google Scholar]
- 54.Maiman DJ, Larson SJ. Management of odontoid fractures. Neurosurgery. 1982;11:471–476. [PubMed] [Google Scholar]
- 55.Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59(2):350–357. doi: 10.1097/01.ta.0000174671.07664.7c. [DOI] [PubMed] [Google Scholar]
- 56.McBride AD, Mukherjee DP, Kruse RN, Albright JA. Anterior screw fixation of type II odontoid fractures: a biomechanical study. Spine. 1995;20:1855–1860. doi: 10.1097/00007632-199509000-00001. [DOI] [PubMed] [Google Scholar]
- 57.Moscovich R, Crockard H. Myelopathy due to a hypertrophic non-union of the dens: case report. J Trauma. 1990;30:222–225. doi: 10.1097/00005373-199002000-00017. [DOI] [PubMed] [Google Scholar]
- 58.Mouradian WH, Fietti VG, Chochran GVB, Fielding JW, Young J. Fractures of the odontoid: a laboratory and clinical study of mechanism. Orthop Clin North Am. 1978;9:985–1001. [PubMed] [Google Scholar]
- 59.Muller EJ, Schwinnen I, Fischer K, et al. Non-rigid immobilisation of odontoid fractures. Eur Spine J. 2003;12:522–525. doi: 10.1007/s00586-003-0531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Muller EJ, Wick M, Russe O, et al. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8:360–365. doi: 10.1007/s005860050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Olerud C, Andersson S, Svensson B, Bring J. Cervical spine fractures in the elderly: factors influencing survival in 65 cases. Acta Orthop Scand. 1999;70:509–513. doi: 10.3109/17453679909000990. [DOI] [PubMed] [Google Scholar]
- 62.Paradis G, Janes J. Posttraumatic atlantoaxial instability: the fate of the odontoid process fracture in 46 cases. J Trauma. 1973;13:359–366. [PubMed] [Google Scholar]
- 63.Pepin JW, Bourne RB, Hawkins RJ. Odontoid fractures, with special reference to the elderly patient. Clin Orthop Relat Res. 1985;193:178–183. [PubMed] [Google Scholar]
- 64.Perry J, Nickel VL. Total cervical-spine fusion for neck paralysis. J Bone Joint Surg Am. 1959;41:37–60. [PubMed] [Google Scholar]
- 65.Platzer P, Thalhammer G, Sarahrudi K, Kovar F, Vekszler G, MD, Vécsei V, Gaebler C (2007) Nonoperative management of odontoid fractures using a halothoracic brace. Neurosurgery 61(3):522–530 [DOI] [PubMed]
- 66.Polin RS, Szabo T, Bogaev CA, et al. Nonoperative management of types II and III odontoid fractures: the Philadelphia collar versus the halo vest. Neurosurgery. 1996;38:450–456. doi: 10.1097/00006123-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 67.Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23:38–40. doi: 10.1016/0020-1383(92)90123-a. [DOI] [PubMed] [Google Scholar]
- 68.Ryan MD, Taylor TFK. Odontoid fractures in the elderly. J Spinal Dis. 1993;6:397–401. doi: 10.1097/00002517-199306050-00005. [DOI] [PubMed] [Google Scholar]
- 69.Schweigel JF. Management of the fractured odontoid with halo-thoracic bracing. Spine. 1987;12:838–839. doi: 10.1097/00007632-198711000-00002. [DOI] [PubMed] [Google Scholar]
- 70.Seybold EA, Bayley JC. Functional outcome of surgically and conservatively managed dens fractures. Spine. 1998;23:1837–1845. doi: 10.1097/00007632-199809010-00006. [DOI] [PubMed] [Google Scholar]
- 71.Smith HE, Kerr SM, Maltenfort M, Chaudhry S, Norton R, Albert TJ, Harrop J, Hilibrand AS, et al. Early complications of surgical versus conservative treatment of isolated type ii odontoid fractures in octogenarians: a retrospective cohort study. J Spinal Disord Tech. 2008;21(8):535–539. doi: 10.1097/BSD.0b013e318163570b. [DOI] [PubMed] [Google Scholar]
- 72.Smith HE, Vaccaro AR, Maltenfort M, Albert TJ, Hilibrand AS, et al. Trends in surgical management for type ii odontoid fracture: 20 years of experience at a regional spinal cord injury center. Orthopedics. 2008;31(7):650. [PubMed] [Google Scholar]
- 73.Stoney J, O’Brien J, Wilde P. Treatment of type-two odontoid fractures in halothoracic vests. J Bone Joint Surg Br. 1998;80:452–455. [PubMed] [Google Scholar]
- 74.Stratford J. Myelopathy caused by atlantoaxial dislocation. J Neurosurg. 1957;14:97–104. doi: 10.3171/jns.1957.14.1.0097. [DOI] [PubMed] [Google Scholar]
- 75.Stulik J, Vyskocil T, Sebesta P, Kryl J. Atlantoaxial fixation using the polyaxial screw-rod system. Eur Spine J. 2007;16:479–484. doi: 10.1007/s00586-006-0241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tan MS, et al. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine. 2003;28:888–895. doi: 10.1097/01.BRS.0000058719.48596.CC. [DOI] [PubMed] [Google Scholar]
- 77.Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60(1):199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 78.van Middendorp JJ, Slooff WB, Nellestein WR, Oner FC (2009) Incidence of and risk factors for complications associated with halo-vest immobilization: a prospective, descriptive cohort study of 239 patients. J Bone Joint Surg Am 91(1):71–79 [DOI] [PubMed]
- 79.Vieweg U, Schultheiss R. A review of halo vest treatment of upper cervical spine injuries. Arch Orthop Trauma Surg. 2001;121:50–55. doi: 10.1007/s004020000182. [DOI] [PubMed] [Google Scholar]
- 80.Weller SJ, Malek AM, Rossitch E. Cervical spine fractures in the elderly. Surg Neurol. 1997;47:274–281. doi: 10.1016/s0090-3019(96)00362-x. [DOI] [PubMed] [Google Scholar]
- 81.Wright NM, Lauryssen C. Vertebral artery injury in C1–2 transarticular screw fixation: results of a surgery of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg. 1998;88:634–640. doi: 10.3171/jns.1998.88.4.0634. [DOI] [PubMed] [Google Scholar]