Abstract
Background
Little research has examined how chronic stress in different domains relates to allostatic load (AL).
Purpose
We examined the relationship between multiple chronic stressors with AL, and evaluated lifestyle factors as possible mediating factors.
Methods
Three hundred one middle-aged Mexican-American women underwent a physical exam and completed measures of lifestyle factors and chronic stress in eight domains. A composite of 12 neuroendocrine, metabolic, cardiovascular, and inflammatory markers represented AL.
Results
Chronic work, financial, and caregiving domains related to higher AL scores after adjusting for covariates and other stressors. Lifestyle factors made little contribution to the association between stressors and AL.
Conclusions
Chronic work, financial, and caregiving stressors are associated with physiological dysregulation in Mexican-American women. This study is among the first to examine multiple domains of chronic stress in relation to AL, in a population that has been understudied in research concerning stress and health.
Keywords: Allostatic load, Health behaviors, Hispanic, Latino, Stress
Introduction
Allostatic load (AL) is a potentially useful conceptual framework through which to capture physiological dysregulation related to chronic stress [1]. However, relatively few studies have directly assessed the association between subjective experiences of chronic stress in different domains and AL. The current study examined (1) the relationship between chronic stress in health, work, relationship, caregiving, and financial domains with AL scores in a community sample of Mexican-American women and (2) evaluated the contribution of lifestyle factors to the association between chronic stress and AL.
Allostatic Load and its Measurement
AL is an increasingly prominent model in research concerning the physiological and health consequences of chronic stress [2, 3]. The framework asserts that the cumulative burden of stress manifests as physiological dysregulation across multiple, interrelated systems involved in restoring allostasis and maintaining healthy functioning in the presence of internal or environmental demands. This “load” is typically indicated by elevated (or reduced) levels across neuroendocrine markers of the sympathetic–adrenal–medullary (SAM; i.e., epinephrine and norepinephrine) and hypothalamic–pituitary–adrenal (HPA) systems (i.e., cortisol) and indicators of cardiovascular and metabolic functioning. SAM and HPA functioning are considered the primary mediators of AL, whereas the latter are viewed as secondary indicators of the primary neuroendocrine pathways. Recent conceptualizations of AL have also incorporated markers of inflammation as primary mediators [4–7]. AL scores have been shown to predict cardiovascular disease (CVD), all-cause mortality, cognitive dysfunction, and disability [8–11]. Moreover, there is evidence that AL has a stronger relationship with physical health than its individual components [8, 10] or the metabolic syndrome, which overlaps with secondary manifestations of AL [8]. Although additional research is needed to determine optimal measurement, and to test certain aspects of the model, AL appears to have conceptual utility in capturing the physical toll of chronic stress.
Chronic Stress and Allostatic Load
The AL model postulates that cumulative exposure to stress across the lifespan is a catalyst in physiological dysregulation. Accordingly, stressors that are enduring or frequent should demonstrate marked relationships with AL and with health [12]. Consistent with this view, chronic stress in life domains including work [13], marriage [14, 15], and caregiving [16, 17] predicts health outcomes such as CVD and all-cause mortality. Studies have related these chronic stressors to regulatory function in single physiological systems, but research examining chronic stress and multi-systemic functioning is critically lacking. Indeed, many studies of AL have inferred stress based on social conditions such as low socioeconomic status [5, 18, 19] or low social support [20, 21].
Additional research has shown that individuals reporting greater work stress (e.g., job demands, effort–reward imbalance; 22, 23) evidence higher AL scores. Perceived stress among dementia caregivers has also been related to primary mediators, but not other facets, of AL [24]. Caregivers also evidenced increases in primary mediators from baseline to 1-year follow-up in this study, suggesting an escalation in physiological burden over time. Finally, several reports concerning stress and AL derive from the Social Environment and Biomarkers of Aging Study (SEBAS), which examines a nationally representative sample of older Taiwanese residents. In this cohort, individuals who reported more stressful life events in the preceding 4 years evidenced higher AL scores than those with fewer events [25]. Perceived stress also related to higher AL, with a stronger association in women than in men [26]. Duration of life stress, and several presumed indicators of stress (e.g., low education, widowhood) were unrelated to the primary mediators of AL in the SEBAS cohort. However, women (but not men) reporting more current familial stressors showed higher scores on the primary AL mediators [27].
Notably, the degree of dysregulation associated with chronic stress could depend markedly on subjective distress. For example, studies of caregivers suggest that only those who feel “strained” experience deleterious health outcomes [16]. Stress appraisals and reactions stem from many factors including individual differences, such as personality and coping resources, and the social context in which stress occurs [28]. Thus, seemingly stressful social circumstances, such as low socioeconomic status, or social isolation, might not translate into the same physical, emotional, and behavioral consequences for all individuals. Research that incorporates personal perceptions of stress may provide a more complete picture of how stress relates to AL and health [29].
Allostatic Load in the Latino Population
To date, only limited research has examined AL specifically within Latinos. However, studies of Latinos suggest that discrimination [30, 31] and caregiving stress [32] relate to responses in individual physiological systems. In addition, several recent studies have examined predictors of AL in the National Health and Nutrition Examination Survey (NHANES) III, a US population-based study including a large, multi-ethnic, representative sample. Analyses have shown that (1) socioeconomic status (SES) predicted AL in Latinos and other ethnic groups [33], (2) neighborhood SES related inversely to AL in Mexican-American and Black but not White participants [19], and (3) poverty related to higher aggregate biological risk among all participants after controlling for race/ethnicity [34]. Additional research in an earlier NHANES cohort revealed that Latinos had higher levels of biological risk than Whites, but lower levels than Blacks [35]. Other studies suggest that US-born Mexican-Americans display greater biological risk than Mexican immigrants [7, 35], and that longer duration of US residence predicts higher AL scores in immigrants [7]. To our knowledge, no prior research has examined the association between chronic stress and AL in Latinos.
The Current Study
The current study expanded on the extant literature in several ways. First, we examined chronic stress in several domains, including personal health problems, health and substance problems in loved ones, work, close relationships, housing, finances, and caregiving, in relation to AL. Second, we considered the implications of stress appraisals, by asking participants not only whether they experienced a chronic stressor, but also how stressful they found the situation to be. Third, we examined these relationships in a well-defined social–cultural group—i.e., middle-aged Mexican-American women with diverse SES, living in a border region of the US—that has been underrepresented in research concerning stress, physiological responses, and health.
We hypothesized that women who were exposed to chronic stress in a given domain would demonstrate elevated levels of AL, particularly if they perceived the exposure to be more subjectively distressing. Prior studies of women provide evidence for effects of caregiver [32, 36], relationship (particularly marital) [37–39], work [22, 40], and financial stress [41] in association with physiological dysregulation, and it might be predicted that these stressors would be associated with AL in the current study. However, because it is unclear what the relative predictive utility of these domains might be when examined simultaneously, and other stressors examined in the current study have not been well researched, we did not form hypotheses about the relative impact of the different stressor domains.
Finally, the current study examined lifestyle factors as a possible intervening mechanism connecting chronic stress with AL. Health-damaging behaviors have been associated with stress and affect physiological functioning. However, to date, few studies have explored health behaviors in analyses of AL [7, 34, 42, 43], and most have included them as covariates, rather than explicitly examining their contributions to stress–AL associations. We predicted that women experiencing chronic stress would report more health-damaging behaviors, which would relate directly to AL and contribute to (but not fully explain) the association between chronic stress and AL.
Methods
Participants and Recruitment
The current analyses are based in a study of CVD risk in healthy, middle-aged Mexican-American women living near the (San Diego) California–Mexico border. Participants were randomly recruited via targeted telephone and mail procedures. Women were invited to participate if they were aged 40–65 years, Mexican-American, literate in English or Spanish, and free of major health conditions and medications with autonomic effects. Six hundred and fifty-six women were screened, 365 (55.6%) were eligible, and 323 (88%) participated in some or all portions of the study. The current study includes 301 women who completed the psychosocial and physical exams and had all AL datapoints.
Procedures
Participants were scheduled for two consecutive weekday home visits. During the first visit, a bilingual research assistant obtained informed consent and administered a battery of measures (in Spanish or English) assessing sociodemographic characteristics, behavioral risk factors, health history, and psychosocial variables. Participants were also given materials and instructions for a 12-h, overnight urine collection and fasting. The second visit included a fasting blood draw and physical measurements (blood pressure, height, weight, waist circumference). Participants were instructed to refrain from taking anti-inflammatory medications for at least 48 h, to avoid strenuous exercise and alcohol consumption for at least 24 h, and to avoid consuming caffeine and tobacco for at least 30 min prior to the physical exam. All research staff was thoroughly trained in study procedures, and regular quality control checks were conducted. The San Diego State University and University of California, San Diego institutional review boards approved all study procedures.
Allostatic Load: Parameter Assessment and Operationalization
There is controversy about measurement of AL, including which parameters should be included, how they should be combined, whether they should be represented as continuous or categorical variables, and whether cutoffs should be sample-based or established by clinical criteria (e.g., 44, 45). However, studies comparing distinct measurement approaches have found only modest differences in their predictive utility [4, 8, 29, 46], and a recent analysis supported the existence of an overarching AL factor comprising physiological dysregulation across six sub-parameters and 18 specific neuroendocrine, metabolic, cardiovascular, and inflammatory indicators [6]. The current study included all parameters used in the MacArthur Study of Successful Aging [10, 11], with the exception of dehydroepiandrosterone sulfate, which is less clearly related to health outcomes in women than in men [47, 48]. Thus, we examined neuroendocrine markers of SAM and HPA activity [12-h, overnight urinary norepinephrine, epinephrine, and cortisol excretion], metabolic system functioning [serum high-density lipoprotein cholesterol (HDL-c); the ratio of HDL-c to total serum cholesterol; glycosolated hemoglobin (HbA1c); waist circumference], and cardiovascular system functioning [systolic and diastolic blood pressure (SBP and DBP)]. In addition, consistent with other recent conceptualizations [6, 23, 49, 50], we included markers of inflammation [i.e., high sensitivity C-reactive protein (hsCRP); interleukin-6 (IL-6) and tumor necrosis factor alpha (TNF-α)], given considerable research suggesting that inflammation is an important component of many disease processes [51–53] and physiological adjustment to stress [54]. We adopted the MacArthur Studies of Successful Aging algorithm [10, 11], such that each of the 12 biological parameters was divided into quartiles based on the distribution of scores in the sample, and AL was measured by summing the number of parameters for which the subject fell into the highest risk quartile. The one exception was cortisol, for which individuals with scores in either the upper or lower 12.5% of the distribution were counted as high risk. This approach is consistent with research suggesting that both hypo- and hyper-cortisolism represent states of physiological dysregulation related to psychological stress and health problems [55, 56], and has been used in other AL studies [22, 57]. AL scores ranged from 0 to 12, with higher scores indicating greater dysregulation. Table 1 shows the cut-points used for each AL component.
Table 1.
Sample cutoffs for each parameter of allostatic load
| Biological parameters | Highest risk |
|---|---|
| Systolic blood pressure (mm Hg) | ≥124.50 |
| Diastolic blood pressure (mm Hg) | ≥78.00 |
| Waist circumference (cm) | ≥94.50 |
| Total cholesterol/high-density lipoprotein (HDL) cholesterol | ≥4.40 |
| HDL cholesterol (mg/dl)a | ≤45.00 |
| Hemoglobin A1c (%) | ≥5.80 |
| Cortisol μg/g creatinineb | 0.00, ≥43.54 |
| Norepinephrine μg/g creatinine | ≥7.75 |
| Epinephrine μg/g creatinine | ≥3.66 |
| C-reactive Protein (ng/mL) | ≥4.42 |
| Interleukin-6 (pg/mL) | ≥0.94 |
| Tumor Necrosis Factor-α (pg/mL) | ≥3.81 |
aHigh risk for HDL cholesterol corresponds to those individuals who fall in lowest quartile of the sample distribution
bHigh risk for cortisol μg/g creatinine corresponds to those individuals who fall in highest and lowest 12.5% of the sample distribution. Low readings were at undetectable levels according to the assay applied
SBP and DBP were calculated as the average of the second and third of three readings taken while the participant was in a seated position, with arm elevated to heart level, following 30 min of rest, using an automatic sphygmomanometer shown to be valid and reliable (i.e., Omron HEM 705-CP, Omron Corporation, Kyoto Japan). Waist circumference was calculated as the average of the second and third measurements, assessed by tape measure in centimeters at the narrowest point between the ribs and iliac crest. Urine samples were collected by the participant and refrigerated. Blood for the inflammatory biomarkers and lipids was obtained from a venous draw using either ethylenediaminetetraacetic acid as a preservative or serum. Samples were immediately put on ice and centrifuged and the plasma stored at −70°C until assay.
Inflammatory biomarker and neuroendocrine assays were performed at the University of California San Diego (UCSD) General Clinical Research Center Core Laboratory and the UCSD Clinical Biomarker Laboratory. Circulating levels of CRP, IL-6 and TNF-α were determined in non-freeze thawed samples by commercial enzyme-linked immunosorbent assay (MSD, Gaithersburg, Maryland). The intra-assay and inter-assay coefficients of variation are less than 5% and 8%, respectively [58]. Urinary cortisol levels were determined by a commercial radioimmunoassay (Diagnostic Products Corporation, Los Angeles, CA), with intra- and inter-assay CVs of <4% and <7%, respectively. Urinary epinephrine and norepinephrine were measured using a catechol-O-methyltransferase-based radioenzymatic assay that concentrates catecholamines with 81% efficiency and has inter- and intra-assay CVs <10% [59]. Results for norepinephrine, epinephrine, and cortisol were reported in micrograms per gram of creatinine to adjust for body size. Blood specimens used to derive lipids and HbA1c were processed by Quest Diagnostics Laboratories. Serum total cholesterol and HDL-c were measured using enzymatic procedures, following standards set by the Lipid Standardization Program of the Centers for Disease Control and Prevention [60]. HbA1c was assayed using a Biorad Diomat high-pressure liquid chromatography analyzer.
Chronic Stress Domains
Participants completed a measure asking if they had experienced eight chronic stressors for at least 12 months duration [61]. The response format was on a four-point scale with 0 indicating that the stressor did not occur, 1 indicating occurrence of the stressor but with little or no subjective stress (“not upsetting”), and 2 and 3 indicating occurrence of the stressor with moderate or severe subjective stress (“somewhat upsetting” and “very upsetting”), respectively. The domains queried were: personal health stress, health problems in a family member; drug or alcohol problems in a family member; financial strain; work stress; housing problems; relationship stress; and caregiving stress (i.e., helping a sick, disabled, or frail family member or friend on a regular basis). The measure was translated into Spanish for the current study (forward and back translation with reconciliation by committee).
Lifestyle Factors
Participants reported whether or not they currently smoked and frequency and quantity of alcohol intake (used to estimate alcoholic beverages consumed per month). Dietary behaviors were assessed with two brief screeners that have been shown to be highly correlated with the full length Block Food Frequency Questionnaire in a validation study with a large, multi-ethnic sample [62]. For the current study, we examined total fat (grams) and fiber (grams). Spanish translations of these scales were developed for a prior study of Mexican-Americans with minor modifications to include examples of foods specific to the population [e.g., tortillas, lard; 63]. Exercise levels were assessed with the Leisure Time Exercise Questionnaire [64], which asks respondents to state the number of times during a typical week they participated in strenuous or moderate exercise for at least 15 min and provides an estimate of total Metabolic Equivalent of Task Units (i.e., METs) per week. METs provide an estimate of the intensity and energy expenditure of physical activity that is comparable across people of differing body sizes. The measure was translated for the current study as described above. Prior research concerning the English version has demonstrated high 2-month test–retest reliability for vigorous exercise (r = 0.84), acceptable test–retest reliability for moderate exercise (r = 0.36), and adequate criterion-related validity with accelerometer assessments [r = 0.36; 64, 65].
Covariates
Analyses controlled for several factors that could be related to chronic stress, AL, or both, including age, menopausal status, (with those reporting no menstruation for at least 12 months considered post-menopausal), SES (education/income composite, defined below), employment status (employed for wages, or not), marital status (married or living with a partner, or not), and insurance status (any coverage or none). In addition, we controlled for language of survey, a commonly used proxy for acculturation [66], which also accounted for the influence of Spanish versus English versions of the measures. For SES, participants indicated the highest level of education they achieved, from no education to a doctoral or professional degree, recoded into six categories for analysis. Total monthly family income was assessed on an ordinal scale in $500 increments, ranging from less than $500/month to more than $8,000 per month. An education/income composite was created by standardizing and summing the variables. For four participants with missing income data, education only was used to represent SES.
Statistical Analyses
Descriptive statistics were calculated and all variables were examined for normality. Exercise and alcohol were extremely positively skewed, with a large proportion of women reporting no leisure time physical activity (25.7%) or no alcohol consumption (45.5%). Based on the sample distributions, exercise was categorized into quintile groups, and alcohol was coded into 4 groups, representing those who reported 0–1 drinks, 2–5 drinks, 6–19 drinks, and 20 or more drinks per month.
The primary hypotheses of interest were tested in multiple linear regression analyses. Preliminary diagnostic analyses confirmed that assumptions of ordinary least squares regression were met (results not reported). Two regression models were conducted. In the first model, covariates (age, menopausal status, SES, employment status, marital status, health insurance status, and language of assessment) were entered at step 1, followed by the chronic stress variables at step 2. All chronic stress domains were examined in a single analysis, to determine the association between a given stressor with AL after accounting for the influence of all other stressors. A second model examined if lifestyle factors contributed to the association between chronic stress and AL, with covariates entered at step 1, behavioral factors at step 2, and chronic stressors at step 3. Missing data were excluded on a pairwise basis to maximize power. Given the exploratory nature of the research, and relatively small sample size, we also noted cases where relationships approached significance (i.e., 0.05 < p < 0.10).
Results
As shown in Table 2, the mean age of the sample was approximately 49.8 years (SD = 6.61). The majority completed the questionnaires in Spanish (59.5%), and SES was widely varied. Mean AL score was 3.04 (SD = 2.06). Frequency and severity of chronic stressors varied, with only 10.29% reporting moderate to severe personal health stress and 34.21% reporting moderate to severe financial strain.
Table 2.
Sample descriptive statistics (N = 301)
| Variables | Mean (SD) or n (%) |
|---|---|
| Age (years), M (SD) | 49.80 (6.61) |
| Post-menopausal, n (%) | 144 (47.8%) |
| Married or living with partner, n (%) | 218 (72.4%) |
| Completed interview in Spanish, n (%) | 179 (59.5%) |
| Educational attainment, n (%) | |
| ≤8th grade | 52 (17.3%) |
| Some high school | 53 (17.6%) |
| GED or high school diploma | 35 (11.6%) |
| Some college | 94 (31.2%) |
| 4 year college degree | 48 (16.0%) |
| Graduate education | 19 (6.3%) |
| Monthly income, n (%) | |
| ≤$2499 | 94 (32.0%) |
| $2500–$4999 | 115 (39.0%) |
| ≥$5000 | 87 (29.4%) |
| Employed for wages, n (%) | 155 (51.7%) |
| Uninsured, n (%) | 79 (26.2%) |
| Allostatic load, M (SD) | 3.04 (2.06) |
| Personal health stress, n (%) | |
| No stressor | 256 (85.0%) |
| Yes, not upsetting | 14 (4.7%) |
| Yes, somewhat upsetting | 22 (7.3%) |
| Yes, very upsetting | 9 (3.0%) |
| Health problem in family member, n (%) | |
| No stressor | 185 (61.5%) |
| Yes, not upsetting | 22 (7.3%) |
| Yes, somewhat upsetting | 61 (20.3%) |
| Yes, very upsetting | 33 (11.0%) |
| Drug/alcohol problem in family member, n (%) | |
| No stressor | 230 (76.7%) |
| Yes, not upsetting | 8 (2.7%) |
| Yes, somewhat upsetting | 30 (10.0%) |
| Yes, very upsetting | 32 (10.7%) |
| Work stress, n (%) | |
| No stressor | 235 (78.1%) |
| Yes, not upsetting | 16 (5.3%) |
| Yes, somewhat upsetting | 40 (13.3%) |
| Yes, very upsetting | 10 (3.3%) |
| Financial strain, n (%) | |
| No stressor | 163 (54.2%) |
| Yes, not upsetting | 35 (11.6%) |
| Yes, somewhat upsetting | 73 (24.3%) |
| Yes, very upsetting | 30 (10.0%) |
| Housing problems, n (%) | |
| No stressor | 255 (84.7%) |
| Yes, not upsetting | 7 (2.3%) |
| Yes, somewhat upsetting | 26 (8.6%) |
| Yes, very upsetting | 13 (4.3%) |
| Caregiving stress, n (%) | |
| No stressor | 174 (58.0%) |
| Yes, not upsetting | 63 (21.0%) |
| Yes, somewhat upsetting | 47 (15.7%) |
| Yes, very upsetting | 16 (5.3%) |
| Relationship stress, n (%) | |
| No stressor | 213 (70.8%) |
| Yes, not upsetting | 20 (6.6%) |
| Yes, somewhat upsetting | 40 (13.3%) |
| Yes, very upsetting | 28 (9.3%) |
| Total fiber (grams per day), M (SD) | 25.38 (5.46) |
| Total fat (grams per day), M (SD) | 129.87 (21.90) |
| Exercise (METs per week), n (%) | |
| 0 | 76 (25.7%) |
| 1–9 | 43 (14.5%) |
| 9.1–19.9 | 63 (21.3%) |
| 20–34.9 | 55 (18.6%) |
| ≥35 | 59 (19.9%) |
| Alcohol consumption (drinks per month), n (%) | |
| 0–1 | 193 (65.4%) |
| 2–5 | 77 (26.1%) |
| 6–19 | 15 (5.1%) |
| ≥20 | 10 (3.4%) |
| Current smoker, n (%) | 27 (9.0%) |
Income is shown in three categories that correspond approximately to low, medium, and high socioeconomic status for the targeted sampling frame
The full continuum of responses was used in analyses
As shown in Table 3, Pearson Product Moment and Point-Biserial correlation coefficients showed that women reporting lower alcohol consumption (p < 0.01) and exercise (p < 0.05) evidenced higher AL scores, whereas smoking and dietary factors did not relate to AL. Women with work stress consumed more alcohol (p < 0.05), and tended to consume more fat (p < 0.10). Women reporting relationship stress showed a trend toward higher alcohol consumption (p < 0.10), and significantly higher fat intake (p < 0.01)
Table 3.
Bivariate associations between AL and domains of chronic stress with lifestyle factors
| Variables | Current smoker | Alcohol consumption (drinks/month) | Fiber (grams/day) | Fat (grams/day) | Exercise (METs/week) |
|---|---|---|---|---|---|
| Allostatic load | −0.017 | −0.216*** | −0.009 | 0.033 | −0.127** |
| Personal health problems | −0.058 | −0.044 | 0.020 | −0.020 | 0.001 |
| Health problems—family member | 0.013 | 0.004 | −0.022 | 0.009 | 0.035 |
| Drug/alcohol problems—family member | −0.064 | 0.011 | 0.008 | 0.030 | 0.022 |
| Work stress | 0.023 | 0.139** | −0.020 | 0.097* | 0.012 |
| Financial strain | −0.014 | −0.085 | −0.083 | 0.057 | −0.075 |
| Housing problems | −0.055 | 0.003 | 0.035 | −0.013 | 0.052 |
| Caregiving stress | −0.069 | −0.045 | 0.006 | 0.042 | 0.059 |
| Relationship stress | −0.017 | 0.108* | −0.037 | 0.148*** | 0.032 |
*p < 0.10; **p < 0.05; ***p < 0.01
Regressing Allostatic Load on Chronic Stress Domains
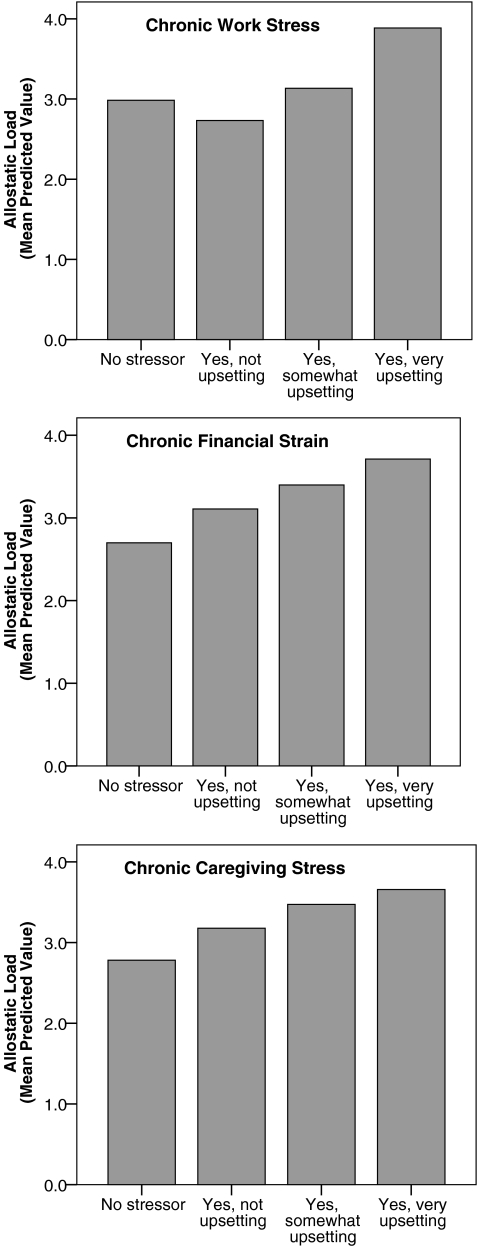
Table 4 shows the results of analyses regressing AL scores simultaneously on all chronic stress domains. In model 1, the chronic stressors in aggregate accounted for approximately 7% of the variance in AL scores, after accounting for covariates. Work stress (p < 0.05), financial strain (p < 0.01), and caregiving stress (p < 0.01) were independently associated with higher AL scores. Mean predicted AL scores (controlling for covariates) across responses for these domains are shown in Fig. 1. Women without chronic financial or caregiving stress had mean predicted AL scores that were 1.01 and 0.88 points lower, respectively, than did women with severe stress in those domains. Women with chronic work stress but no subjective distress had mean predicted AL scores 1.15 points lower than those with severe chronic work stress.
Table 4.
Results of multiple linear regression analyses regressing allostatic load on chronic stress domains, without (model 1) and with (model 2) control for lifestyle factors
| B | SE B | β | ΔR 2 | ΔF | |
|---|---|---|---|---|---|
| Model 1: Association between allostatic load and chronic stress domains, after adjusting for covariates (n = 298) | |||||
| Covariates | 12.1% | F 7,290 = 5.72*** | |||
| Chronic stress domains | 7.1% | F 8,282 = 3.09*** | |||
| Personal health problems | 0.079 | 0.167 | 0.027 | ||
| Health problems—family member | −0.075 | 0.119 | −0.040 | ||
| Drug/alcohol problems—family | −0.050 | 0.117 | −0.026 | ||
| Work stress | 0.290 | 0.140 | 0.120** | ||
| Financial strain | 0.336 | 0.119 | 0.178*** | ||
| Housing problems | −0.031 | 0.155 | −0.012 | ||
| Relationship stress | −0.218 | 0.137 | −0.109 | ||
| Caregiving stress | 0.315 | 0.127 | 0.142*** | ||
| Model 2: Model 1 plus lifestyle factors (n = 287) | |||||
| Covariates | 12.0% | F 7,279 = 5.42*** | |||
| Lifestyle Factors | 3.5% | F 5,274 = 2.26** | |||
| Current smoker | 0.009 | 0.115 | 0.004 | ||
| Alcohol consumption | −0.272 | 0.122 | −0.130** | ||
| Fiber | 0.006 | 0.124 | 0.003 | ||
| Fat | 0.192 | 0.122 | 0.093 | ||
| Exercise | −0.118 | 0.125 | −0.057 | ||
| Chronic stress domains | 6.4% | F 8,266 = 2.72*** | |||
| Personal health problems | 0.087 | 0.170 | 0.030 | ||
| Health problems—family member | −0.094 | 0.121 | −0.051 | ||
| Drug/alcohol problems -family | −0.047 | 0.119 | −0.024 | ||
| Work stress | 0.320 | 0.146 | 0.130** | ||
| Financial strain | 0.284 | 0.121 | 0.151** | ||
| Housing problems | −0.006 | 0.158 | −0.002 | ||
| Relationship stress | −0.235 | 0.140 | −0.118* | ||
| Caregiving stress | 0.279 | 0.129 | 0.127** | ||
Covariates are age, menopausal status, SES, employment status, marital status, health insurance status, and language of assessment. R 2 and F change are for model step. All coefficients are from final model step
*p < 0.10; **p < 0.05; ***p < 0.01
Fig. 1.
Predicted values for allostatic load, controlling for covariates, across chronic stressor response categories for work stress, financial strain, and caregiving stress
In model 2, lifestyle factors accounted for a significant amount of the variance in AL scores, p < 0.05, after controlling for covariates (Table 4). Higher alcohol consumption related to lower AL scores (p < 0.05). The aggregate influence of chronic stress domains remained statistically significant, and work stress, financial strain, and caregiving stress were again observed to be independent predictors of AL scores (p < 0.05). Interestingly, there was a marginally significant trend for higher relationship stress to be associated with lower AL scores in this analysis. In all cases, the reduction in the weight of the regression coefficients for previously significant chronic stress effects was negligible, indicating that lifestyle factors played a minimal role in explaining the association between chronic stress and AL.
Discussion
The current study examined associations between chronic stress experienced in different domains and AL scores in middle-aged Mexican-American women, and evaluated the contribution of lifestyle factors to these associations. Although prior studies have shown that AL relates to social circumstances presumed to foster stress, only limited research has examined stress perceptions, and no study has, to our knowledge, assessed the association of multiple types of chronic stress with AL in a single study.
In support of the AL framework, we found that greater stress in the domains of work, finances, and caregiving related to higher AL scores. These findings are consistent with prior studies that have shown an association between work stress and AL [22, 23] and between perceived stress and the primary mediators of AL in dementia caregivers [24]. To our knowledge, no prior study has examined the specific relationship of chronic financial stress with AL. Notably, health problems in self or loved ones and relationship stress did not relate significantly to AL in the current sample. These stressors have not previously been studied as individual predictors of AL, although relationship (particularly marital) stress has been associated with specific indicators of physiological dysregulation in prior research (e.g., elevated blood pressure; metabolic dysregulation; 37–39).
Given research demonstrating that AL predicts health outcomes including CVD and mortality [8–11], the current findings suggest that chronic stress, particularly in the areas of work, caregiving, and finances may be relevant to understanding Mexican-American women’s health risks. For example, in a study of older adults [67], each 1 unit increment in a similar measure of AL was associated with more than double the mortality risk after adjusting for age and gender. In the current study, the difference in predicted AL scores (controlling for covariates) between women who experienced severe stress and those who reported no stress was more than 1 unit difference for chronic financial strain and 0.85 unit difference for caregiving stress. A greater than 1 point difference was also observed between women who experienced work stress but did not find it upsetting and those with work stress they found to be severely upsetting. Thus, the findings suggest clinically meaningful increases in health risks associated with severe chronic stress in these domains. However, future research is needed to examine how AL relates to objective health outcomes such as mortality specifically in Latino populations.
It is interesting to note that only certain types of chronic stress were independently associated with AL scores in the current study. This supports the utility of considering and discriminating among multiple domains of stress instead of simply examining overall perceived stress, or counting the number of stressful events. In addition, several factors may help explain why certain stressors did not emerge as AL predictors. First, some participants may have been reluctant to disclose problems in areas that are highly valued (i.e., relationship stress) or that carry social stigma (i.e., family substance abuse), especially given the general trend for Latinos to respond in a socially desirable manner (e.g., relative to non-Latino whites; 68). These tendencies may have led to errors in quantifying exposure to chronic stress. Second, lack of precision in assessment could be a contributing factor. For example, participants might have endorsed “ongoing work stress” because of interpersonal problems with colleagues, low levels of control at work, or failure to advance in their profession. Thus, this domain could conceivably represent either a social or achievement related stressor. As another example, “ongoing problems in a close relationship” might describe conflict with a spouse, child, or friend, and could refer to a relationship with someone seen daily or someone with whom the participant interacts only rarely. Given this range, the physiological consequences of close relationship stress could be expected to vary considerably. Comparatively, items assessing caregiving and financial stress are relatively more straightforward in their interpretations. Moreover, both caregiving and financial stress are likely to have an insidious influence across all aspects of a person’s life. Overall, additional research using more refined assessments of each stress domain is needed to explore the stability of the current findings, and whether they generalize to other social–cultural groups.
A second goal of the current study was to examine the contribution of lifestyle factors to associations between chronic stress and AL [43]. In a prior study of middle-aged Hawaiian residents [69], health behaviors (specifically, less alcohol use, more smoking, and less physical activity) were related to physiological dysregulation in multivariate analyses for men but not women. In SEBAS, greater physiological dysregulation was observed in alcohol abstainers versus non-abstainers, whereas smoking did not relate to AL [43]. Analyses performed in the NHANES III cohort found that heavy drinking was unassociated with AL; whereas smokers had higher AL scores [34]. Lifestyle factors explained a significant amount of variance in AL scores after controlling for covariates in the current study. However, only alcohol consumption emerged as a significant predictor, with greater alcohol consumption predicting lesser AL. It is notable that alcohol consumption was quite moderate in our sample, with only 8.5% of women consuming six or more drinks per month. Prior research indicates that the association between alcohol and health is J-shaped, so that low to moderate levels of consumption are salubrious, whereas heavier drinking predicts increased health risks [e.g., higher cardiovascular and all-cause mortality rates; 70, 71]. The mechanisms explaining these effects are believed to include enhanced HDL-c and insulin sensitivity, and reduced inflammation [72], all of which are reflected in our AL construct. Notably, chronic stressors did not relate consistently to lifestyle factors in our study and consequently, these variables had a negligible role in connecting chronic stress with AL. This suggests a more salient direct relationship between chronic stress and AL. Measurement limitations (e.g., self-report assessments of activity and diet; lack of validation information on Spanish versions) and the fact that few women in our study evidenced high-risk lifestyles may also be relevant to understanding these findings.
The current study adds to the literature by comparing multiple domains of chronic stress in relation to AL, considering subjective stress appraisals, and focusing on an understudied, well-defined sociocultural group. However, the study also must be interpreted in light of its limitations. The cross-sectional nature of the design prohibits conclusions regarding directionality of the observed associations. Although conceptually unlikely, AL might influence chronic stress perceptions. A longitudinal study involving multiple assessments of chronic stress domains and AL over time would provide stronger evidence for the hypothesized relationships. In addition, to minimize participant burden, comprehensive assessments of each chronic stress domain were not administered. The use of a single item to assess each stressor could create interpretive differences that might have diminished our ability to identify chronic stress effects in certain domains. Finally, although there are advantages to focusing on a specific demographic group, given that the impact or relevance of different types of stress may be influenced by social–cultural context among other factors, this approach also limits generalizability. We focused on a relatively small sample of a specific segment of US female Latino residents, and the findings cannot be assumed to generalize beyond this sociodemographic group. Likewise, given that we excluded women with health problems, and endeavored to represent the full range of SES (consistent with target communities’ SES distribution according to census data), it is possible that levels of chronic stress or AL were different (e.g., lower) in the current sample relative to what might have been observed in other samples of Mexican-American women. Indeed, certain stress categories were endorsed infrequently, and this may have attenuated statistical power. Future research addressing each of these limitations is recommended to further explore how specific domains of chronic stress relate to AL in diverse populations.
Acknowledgments
This study was supported by grant number 1R01HL081604-01from the National Heart Lung and Blood Institute, National Institutes of Health (NHLBI/NIH). Authors Jessica Jiménez and Smriti Shivpuri were supported by 1T32HL079891-01A2 (NHLBI/NIH) and Karla Espinosa de los Monteros by F31HL087732-02(NHLBI/NIH) during their work on the study. This research was also supported in part by grant number 1P20MD002293-01, San Diego Partnership to reduce CVD Disparities, National Center of Minority Health and Health Disparities, NIH. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of the NIH. We thank Dr. Scott Roesch for his assistance with statistical analyses, Dr. Wendy Davila-Fraga, project manager, and all other research staff and students who assisted with this project. Finally, we thank the participants of “Nuestra Salud” for their invaluable contributions.
Conflict of interest statement
The authors have no conflict of interest to disclose.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.McEwen B, Lasley EN. Allostatic load: When protection gives way to damage. Adv Mind Body Med. 2003;19:28–33. [PubMed] [Google Scholar]
- 2.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 3.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 4.Gruenewald TL, Seeman TE, Ryff CD, Karlamangla AS, Singer BH. Combinations of biomarkers predictive of later life mortality. Proc Nat Acad Scie. 2006;103:14158–14163. doi: 10.1073/pnas.0606215103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seeman TE, Crimmins E, Huang MH, et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc Sci Med. 2004;58:1985–1997. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- 6.Seeman T, Gruenewald T, Karlamangla A et al. Modeling multisystem biological risk in young adults: The Coronary Artery Risk Development in Young Adults Study. Am J Hum Biol 2009, EPUB. [DOI] [PMC free article] [PubMed]
- 7.Peek MK, Cutchin MP, Salinas JJ et al. Allostatic load among Non-Hispanic Whites, Non-Hispanic Blacks, and People of Mexican Origin: Effects of ethnicity, nativity, and acculturation. Am J Public Health 2009, EPUB. [DOI] [PMC free article] [PubMed]
- 8.Karlamangla AS, Singer BH, McEwen BS, Rowe JW, Seeman TE. Allostatic load as a predictor of functional decline. MacArthur studies of successful aging. J Clin Epidemiol. 2002;55:696–710. doi: 10.1016/S0895-4356(02)00399-2. [DOI] [PubMed] [Google Scholar]
- 9.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. Am J Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation–allostatic load and its health consequences. MacArthur studies of successful aging. Arch Intern Med. 1997;157:2259–2268. doi: 10.1001/archinte.157.19.2259. [DOI] [PubMed] [Google Scholar]
- 11.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci U S A. 2001;98:4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: Some conceptual perspectives. J Health Soc Behav. 2005;46:205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- 13.Kivimaki M, Virtanen M, Elovainio M, Kouvonen A, Vaananen A, Vahtera J. Work stress in the etiology of coronary heart disease—a meta-analysis. Scand J Work Environ Health. 2006;32:431–442. doi: 10.5271/sjweh.1049. [DOI] [PubMed] [Google Scholar]
- 14.Matthews KA, Gump BB. Chronic work stress and marital dissolution increase risk of posttrial mortality in men from the Multiple Risk Factor Intervention Trial. Arch Intern Med. 2002;162:309–315. doi: 10.1001/archinte.162.3.309. [DOI] [PubMed] [Google Scholar]
- 15.Orth-Gomer K, Wamala SP, Horsten M, Schenck-Gustafsson K, Schneiderman N, Mittleman MA. Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. JAMA. 2000;284:3008–3014. doi: 10.1001/jama.284.23.3008. [DOI] [PubMed] [Google Scholar]
- 16.Schulz R, Newsom J, Mittelmark M, Burton L, Hirsch C, Jackson S. Health effects of caregiving: The caregiver health effects study: An ancillary study of the cardiovascular health study. Ann Behav Med. 1997;19:110–116. doi: 10.1007/BF02883327. [DOI] [PubMed] [Google Scholar]
- 17.Schulz R, Beach SR. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 18.Kubzansky LD, Kawachi I, Sparrow D. Socioeconomic status, hostility, and risk factor clustering in the Normative Aging Study: Any help from the concept of allostatic load? Ann Behav Med. 1999;21:330–338. doi: 10.1007/BF02895966. [DOI] [PubMed] [Google Scholar]
- 19.Merkin SS, Basurto-Davila R, Karlamangla A, et al. Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of U.S. adults: NHANES III. Ann Epidemiol. 2009;19:194–201. doi: 10.1016/j.annepidem.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seeman TE, Singer BH, Ryff CD, Dienberg LG, LevyStorms L. Social relationships, gender, and allostatic load across two age cohorts. Psychosom Med. 2002;64:395–406. doi: 10.1097/00006842-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Singer B, Ryff CD. Hierarchies of life histories and associated health risks. Ann N Y Acad Sci. 1999;896:96–115. doi: 10.1111/j.1749-6632.1999.tb08108.x. [DOI] [PubMed] [Google Scholar]
- 22.Bellingrath S, Weigl T, Kudielka BM. Chronic work stress and exhaustion is associated with higher allostastic load in female school teachers. Stress. 2009;12:37–48. doi: 10.1080/10253890802042041. [DOI] [PubMed] [Google Scholar]
- 23.Schnorpfeil P, Noll A, Schulze R, Ehlert U, Frey K, Fischer JE. Allostatic load and work conditions. Soc Sci Med. 2003;57:647–656. doi: 10.1016/S0277-9536(02)00407-0. [DOI] [PubMed] [Google Scholar]
- 24.Clark MS, Bond MJ, Hecker JR. Environmental stress, psychological stress and allostatic load. Psychol Health Med. 2007;12:18–30. doi: 10.1080/13548500500429338. [DOI] [PubMed] [Google Scholar]
- 25.Glei DA, Goldman N, Chuang YL, Weinstein M. Do chronic stressors lead to physiological dysregulation? Testing the theory of Allostatic Load. Psychosom Med. 2007;69:769–776. doi: 10.1097/PSY.0b013e318157cba6. [DOI] [PubMed] [Google Scholar]
- 26.Goldman N, Glei DA, Seplaki C, Liu IW, Weinstein M. Perceived stress and physiological dysregulation in older adults. Stress. 2005;8:95–105. doi: 10.1080/10253890500141905. [DOI] [PubMed] [Google Scholar]
- 27.Gersten O. Neuroendocrine biomarkers, social relations, and the cumulative costs of stress in Taiwan. Soc Sci Med. 2008;66:507–519. doi: 10.1016/j.socscimed.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chun CA, Moos RH, Cronkite RC. Culture: A fundamental context for the stress and coping paradigm. In: Wong PTP, Wong LCJ, Lonner WJ, editors. Handbook of Multicultural Perspectives on Stress and Coping. New York: Springer; 2006. [Google Scholar]
- 29.Seeman TE, Epel E, Gruenewald T, Karlamangla A, McEwan BS. Socio-economic differentials in peripheral biology: Cumulative allostatic load. Ann N Y Acad Sci. 2010;1186:223–239. doi: 10.1111/j.1749-6632.2009.05341.x. [DOI] [PubMed] [Google Scholar]
- 30.Salomon K, Jagusztyn NE. Resting cardiovascular levels and reactivity to interpersonal incivility among Black, Latina/o, and White individuals: The moderating role of ethnic discrimination. Health Psychol. 2008;27:473–481. doi: 10.1037/0278-6133.27.4.473. [DOI] [PubMed] [Google Scholar]
- 31.Brondolo E, Libby DJ, Denton Eg, et al. Racism and ambulatory blood pressure in a community sample. Psychosom Med. 2008;70:49–56. doi: 10.1097/PSY.0b013e31815ff3bd. [DOI] [PubMed] [Google Scholar]
- 32.Gallagher-Thompson D, Shurgot GR, Rider K, et al. Ethnicity, stress, and cortisol function in Hispanic and non-Hispanic white women: A preliminary study of family dementia caregivers and noncaregivers. Am J Geriatr Psychiatry. 2006;14:334–342. doi: 10.1097/01.JGP.0000206485.73618.87. [DOI] [PubMed] [Google Scholar]
- 33.Seeman T, Merkin SS, Crimmins E, Koretz B, Charette S, Karlamangla A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994) Soc Sci Med. 2008;66:72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crimmins EM, Kim JK, Seeman TE. Poverty and biological risk: The earlier “aging” of the poor. J Gerontol A Biol Sci Med Sci. 2009;64A:286–292. doi: 10.1093/gerona/gln010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97:1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lutgendorf SK, Garand L, Buckwalter KC, Reimer TT, Hong SY, Lubaroff DM. Life stress, mood disturbance, and elevated interleukin-6 in healthy older women. J Gerontol A Biol Sci Med Sci. 1999;54:M434–M439. doi: 10.1093/gerona/54.9.m434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carels RA, Sherwood A, Szczepanski R, Blumenthal JA. Ambulatory blood pressure and marital distress in employed women. Behav Med. 2000;26:80–85. doi: 10.1080/08964280009595755. [DOI] [PubMed] [Google Scholar]
- 38.Gallo LC, Troxel WM, Matthews KA, Kuller L. Marital status and quality in middle aged women: Association with levels and trajectories of cardiovascular risk factors. Health Psychol. 2003;22:463. doi: 10.1037/0278-6133.22.5.453. [DOI] [PubMed] [Google Scholar]
- 39.Troxel WM, Matthews KA, Gallo LC, Kuller LH. Marital quality and occurrence of the metabolic syndrome in women. Arch Intern Med. 2005;165:1022–1027. doi: 10.1001/archinte.165.9.1022. [DOI] [PubMed] [Google Scholar]
- 40.Gallo LC, Bogart LM, Vranceanu AM, Walt LC. Job characteristics, occupational status, and ambulatory cardiovascular activity in women. Ann Behav Med. 2004;28:62–73. doi: 10.1207/s15324796abm2801_8. [DOI] [PubMed] [Google Scholar]
- 41.Steptoe A, Brydon L, Kunz-Ebrecht S. Changes in financial strain over three years, ambulatory blood pressure, and cortisol responses to awakening. Psychosom Med. 2005;67:281–287. doi: 10.1097/01.psy.0000156932.96261.d2. [DOI] [PubMed] [Google Scholar]
- 42.Szanton SL, Gill JM, Allen JK. Allostatic load: A mechanism of socioeconomic health disparities? Biol Res Nurs. 2005;7:7–15. doi: 10.1177/1099800405278216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hu PF, Wagle N, Goldman N, Weinstein M, Seeman TE. The associations between socioeconomic status, allostatic load and measures of health in older Taiwanese persons: Taiwan social environment and biomarkers of aging study. J Biosoc Sci. 2007;39:545–556. doi: 10.1017/S0021932006001556. [DOI] [PubMed] [Google Scholar]
- 44.Loucks EB, Juster RP, Pruessner JC. Neuroendocrine biomarkers, allostatic load, and the challenge of measurement: A commentary on Gersten. Soc Sci Med. 2008;66:525–530. doi: 10.1016/j.socscimed.2007.09.006. [DOI] [Google Scholar]
- 45.McDade TW. Challenges and opportunities for integrative health research in the context of culture: A commentary on Gersten. Soc Sci Med. 2008;66:520–524. doi: 10.1016/j.socscimed.2007.09.005. [DOI] [Google Scholar]
- 46.Seplaki CL, Goldman N, Glei D, Weinstein M. A comparative analysis of measurement approaches for physiological dysregulation in an older population. Exp Gerontol. 2005;40:438–449. doi: 10.1016/j.exger.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 47.Mazat L, Lafont S, Berr C, et al. Prospective measurements of dehydroepiandrosterone sulfate in a cohort of elderly subjects: Relationship to gender, subjective health, smoking habits, and 10-year mortality. Proc Natl Acad Sci U S A. 2001;98:8145–8150. doi: 10.1073/pnas.121177998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Trivedi DP, Khaw KT. Dehydroepiandrosterone sulfate and mortality in elderly men and women. J Clin Endocrinol Metab. 2001;86:4171–4177. doi: 10.1210/jc.86.9.4171. [DOI] [PubMed] [Google Scholar]
- 49.Seplaki CL, Goldman N, Weinstein M, Lin YH. How are biomarkers related to physical and mental well-being? J Gerontol A Biol Sci Med Sci. 2004;59:B201–B217. doi: 10.1093/gerona/59.3.b201. [DOI] [PubMed] [Google Scholar]
- 50.Seeman T, Glei D, Goldman N, Weinstein M, Singer B, Lin YH. Social relationships and allostatic load in Taiwanese elderly and near elderly. Soc Sci Med. 2004;59:2245–2257. doi: 10.1016/j.socscimed.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 51.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 52.Danesh J, Wheeler JG, Hirschfield GM, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med. 2004;350:1387–1397. doi: 10.1056/NEJMoa032804. [DOI] [PubMed] [Google Scholar]
- 53.Gan WQ, Man SFP, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: A systematic review and a meta-analysis. Thorax. 2004;59:574–580. doi: 10.1136/thx.2003.019588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Black PH. Stress and the inflammatory response: A review of neurogenic inflammation. Brain Behav Immun. 2002;16:622–653. doi: 10.1016/S0889-1591(02)00021-1. [DOI] [PubMed] [Google Scholar]
- 55.Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology. 2000;25:1–35. doi: 10.1016/S0306-4530(99)00035-9. [DOI] [PubMed] [Google Scholar]
- 56.Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol Bull. 2007;133:24–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- 57.Glover DA, Stuber M, Poland RE. Allostatic load in women with and without PTSD symptoms. Psychiatry. 2006;69:191–203. doi: 10.1521/psyc.2006.69.3.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mills PJ, Shapiro D, Goldstein IB, et al. Metabolic predictors of inflammation, adhesion, and coagulability in healthy younger-aged adults. Obesity. 2008;16:2702–2706. doi: 10.1038/oby.2008.420. [DOI] [PubMed] [Google Scholar]
- 59.Kennedy B, Ziegler MG. A more sensitive and specific radioenzymatic assay for catecholamines. Life Sci. 1990;47:2143–2153. doi: 10.1016/0024-3205(90)90314-H. [DOI] [PubMed] [Google Scholar]
- 60.Warnick GR. Measurement of cholesterol and other lipoprotein constituents in the clinical laboratory. Clin Chem Lab Med. 2000;38:287–300. doi: 10.1515/CCLM.2000.041. [DOI] [PubMed] [Google Scholar]
- 61.Bromberger JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychol Aging. 1996;11:207–213. doi: 10.1037/0882-7974.11.2.207. [DOI] [PubMed] [Google Scholar]
- 62.Block G, Gillespie C, Rosenbaum EH, Jenson C. A rapid food screener to assess fat and fruit and vegetable intake. Am J Prev Med. 2000;18:284–288. doi: 10.1016/S0749-3797(00)00119-7. [DOI] [PubMed] [Google Scholar]
- 63.Elder JP, Ayala GX, Campbell NR, et al. Interpersonal and print nutrition communication for a Spanish-dominant Latino population: Secretos de la buena vida. Health Psychol. 2005;24:49–57. doi: 10.1037/0278-6133.24.1.49. [DOI] [PubMed] [Google Scholar]
- 64.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–146. [PubMed] [Google Scholar]
- 65.Sallis JF, Saelens BE. Assessment of physical activity by self-report: Status, limitations, and future directions. Res Q Exerc Sport. 2000;71:S1–14. [PubMed] [Google Scholar]
- 66.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: A systematic review of public health studies with Hispanic populations in the United States. Soc Sci Med. 2009;69:983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 67.Karlamangla AS, Singer BH, Seeman TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom Med. 2006;68:500–507. doi: 10.1097/01.psy.0000221270.93985.82. [DOI] [PubMed] [Google Scholar]
- 68.Hopwood CJ, Flato CG, Ambwani S, Garland BH, Morey LC. A comparison of Latino and Anglo socially desirable responding. J Clin Psychol. 2009;65:769–780. doi: 10.1002/jclp.20584. [DOI] [PubMed] [Google Scholar]
- 69.Hampson SE, Goldberg LR, Vogt TM, Hillier TA, Dubanoski JP. Using physiological dysregulation to assess global health status: Associations with self-rated health and health behaviors. J Health Psychol. 2009;14:232–241. doi: 10.1177/1359105308100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002. J Am Coll Cardiol. 2010;55:1328–1335. doi: 10.1016/j.jacc.2009.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006;166:2437–2445. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- 72.O’Keefe JH, Bybee KA, Lavie CJ. Alcohol and cardiovascular health: The razor-sharp double-edged sword. J Am Coll Cardiol. 2007;50:1009–1014. doi: 10.1016/j.jacc.2007.04.089. [DOI] [PubMed] [Google Scholar]