Abstract
We investigated reasons for clinical follow-up and treatment discontinuation among HIV-infected individuals receiving antiretroviral therapy (ART) in a public-sector clinic and in a workplace clinic in South Africa. Participants in a larger cohort study who had discontinued clinical care by the seventh month of treatment were traced using previously provided locator information. Those located were administered a semistructured questionnaire regarding reasons for discontinuing clinical follow-up. Participants who had discontinued antiretroviral therapy were invited to participate in further in-depth qualitative interviews. Fifty-one of 144 (35.4%) in the workplace cohort had discontinued clinical follow-up by the seventh month of treatment. The median age of those who discontinued follow-up was 46 years and median educational level was five years. By contrast, only 16.5% (44/267) of the public-sector cohort had discontinued follow-up. Among them the median age was 37.5 years and median education was 11 years. Qualitative interviews were conducted with 17 workplace participants and 10 public-sector participants. The main reasons for attrition in the workplace were uncertainty about own HIV status and above the value of ART, poor patient–provider relationships and workplace discrimination. In the public sector, these were moving away and having no money for clinic transport. In the workplace, efforts to minimize the time between testing and treatment initiation should be balanced with the need to provide adequate baseline counseling taking into account existing concepts about HIV and ART. In the public sector, earlier diagnosis and ART initiation may help to reduce early mortality, while links to government grants may reduce attrition.
Introduction
The number of HIV-infected persons receiving antiretroviral therapy (ART) in sub-Saharan Africa, where the disease burden is highest, has grown in recent years.1 This expansion has been across a range of settings in the public and private sectors delivering ART within a diverse set of financial and organisational contexts. In all settings, complete discontinuation of antiretroviral therapy (ART), subsequent to attrition from HIV clinical follow-up, is the main challenge to maximizing the benefits of treatment to individual patients and to the community at large. A systematic review by Rosen et al.2 showed that attrition in 13 sub-Saharan countries averaged 22% after 10 months of follow up and 40% after 2 years of follow-up.
Because of logistical and financial constraints early ART research focused on understanding reasons for poor adherence only among patients who remained within clinical care. Published attrition studies rarely traced patients to investigate reasons for discontinuation of care, relying instead on patients (if still alive) and/or family members returning to the clinic to explain the reasons for discontinuation of care. Studies therefore often classified patients, for whom attrition outcomes were unknown, as lost to follow-up. In the review by Rosen et al.,2 among the 22% of patients who discontinued care after 10 months, 56% were classified as lost to follow-up. The dearth of information regarding the reasons for treatment discontinuation once patients stop accessing clinical care leads to an underestimation of mortality,3 poor adherence and poor treatment outcomes,4 and in turn limits the understanding of how best to support patients to remain within clinical care and on ART for as long as possible.
In this study, we set out to investigate patients' reported reasons for attrition. Given the diversity of settings within which ART is delivered, we were particularly interested in the possible influence of the context of service delivery on treatment discontinuation. To this end, we investigated the reasons for discontinuation of clinical follow-up and treatment among participants enrolled in two ART clinics in South Africa: a public-sector clinic based in a tertiary hospital in Gauteng Province and a workplace clinic-based in a tertiary hospital for employees of a mining company in the Northwest Province.
Methods
Study setting and population
Participants for this study were drawn from a larger observational cohort study of adherence predictors conducted in a workplace clinic and a public-sector clinic between May 2005 and September 2007.5 In the cohort study, all treatment-naïve individuals 18 years or older and starting ART during the study period were eligible for enrolment. At enrolment, participants were asked to provide locator information and permission to be traced if they missed their 6-month clinic visit by 1 month or more. Once enrolled, cohort participants were followed up for 6 months to assess baseline determinants of adherence.5 Those who missed their 6-month ART clinic visit by 1 month or more were classified as having discontinued clinical follow-up and enrolled in the attrition study described in this article.
Recruitment of study participants
Up to three attempts were made to trace participants who had discontinued clinical follow-up using locator information collected at ART initiation. If after three attempts, neither the patient nor their secondary contact could be traced, no further attempts were made and the patient was classified as untraceable. If the patient or their secondary contact was located, information to confirm general reasons for attrition (e.g., death, moving away, or treatment discontinuation) was collected using a cross-sectional questionnaire. Of 95 patients traced through this method, 40 were alive and asked if they were willing to participate in the qualitative study. Twenty-seven agreed, comprising 17 individuals who had discontinued ART in the workplace clinic and 10 individuals who had discontinued ART in the public-sector clinic.
Data collection
Semistructured qualitative interviews were conducted by a trained research assistant, using a topic guide that focused on the reasons for testing for HIV and experiences on ART. Participants were also asked about barriers to adherence, including personal circumstances, belief in the existence of HIV and personal HIV status, the value of ART, interactions with ART providers and quality of care at the clinic. Whenever possible, face-to-face interviews were conducted and recorded. Otherwise, interviews were conducted by telephone and detailed notes were recorded. Face-to-face interviews were conducted in the research office located within the ART clinic premises in both sites. Of the 27 in-depth interviews, only 4 were conducted by phone. The average duration of face-to-face interviews was 25 min and that of phone interviews was 20 min. Participants were interviewed in their preferred language, English or one of the four main local languages.
Data processing and analysis
Cross-sectional questionnaire data were analyzed descriptively using Stata 10 software (Stata Corp., College Station, TX). Semistructured interviews were transcribed, translated into English, and entered into the qualitative data analysis software NVivo 8 (QSR International, Doncaster, Victoria, Australia) to organize the data and facilitate the analysis. All transcripts were perused on a line-by-line basis and key themes emerging in the data were grouped together and used to develop a coding scheme. Relevant thematic areas included: personal economic circumstances, reasons for testing, belief in HIV, patient/provider interactions, and system of care. The data were coded and the retrieved data were examined in relation to the original questions, and with respect to differences between the public-sector and the workplace clinic environments.
Ethical approval
The study was approved by the Research Ethics Committee of the University of KwaZulu-Natal; the Human Ethics Research Committee of the University of Witwatersrand; and the Ethics Committee of the London School of Hygiene and Tropical Medicine, UK. Individuals willing to participate in the study provided written informed consent for participation.
Results
The context of service delivery
During the study, both clinics provided ART free of charge. However, the workplace clinic had better financial and human resources, with a patient-to-doctor ratio of 142:1 and a patient-to-nurse ratio of 214:1, compared to the public-sector clinic's ratios of 366:1 and 1219:1, respectively. This difference was reflected in the environment of the two clinics. The workplace clinic, operating within an outpatient department of a tertiary hospital, had treatment rooms and a waiting area that were spacious, organized, airy, and well maintained.
In contrast, the public-sector clinic was set up in a small single-storey annex of a large tertiary hospital. There were few treatment rooms and the patient waiting area was small, overcrowded, and poorly ventilated. Many waiting patients had to sit or lie on the pavement outside the clinic until they were called in for their appointments.
There were important differences in the pathways to HIV testing and treatment initiation. In the public-sector clinic, most patients self-presented for treatment after undergoing voluntary counseling and testing (VCT) in a primary health center. Because of the high demand for ART and low human resource capacity, once individuals presented to the HIV clinic, and were confirmed to be eligible for ART, they were placed on a 6-week waiting list to start treatment. In contrast, most patients in the workplace clinic were actively referred for ART after receiving provider initiated testing and counseling (PITC) offered to individuals with HIV-associated disease or as part of yearly employment health check-ups. Once eligibility was confirmed, there was no waiting list to start ART and eligible individuals were encouraged to start ART promptly. This proactive approach to testing and treatment meant that the time between the first HIV test and starting ART was on average much shorter in the workplace than in the public-sector clinic (1.4 months compared to 11.7 months, respectively). Active counseling and testing, along with the provision of free treatment, clinical follow-up and transport ultimately contributed to the initiation of more than 95% of the estimated total eligible for ART onto treatment as of September 2006 (C. Innes, personal communication). In the first 6 months, the follow-up schedule in the two clinics was similar. For the first 8 weeks patients were followed up bimonthly, then every 4–6 weeks until their 6-month visit. After 6 months, workplace patients returned to the clinic monthly for prescription refills and every 3 months for clinical follow-up. In the public-sector clinic, between 6 months and 2 years, patients returned to the clinic every 2 months for prescription refills and every 3–4 months for clinical follow-up. At each visit in both sites, a review of adherence and counseling took place.
Profile of patients who discontinued follow-up visits
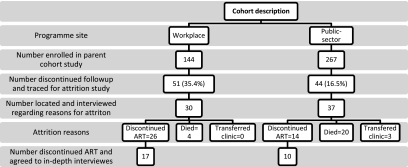
Figure 1 shows the overall sample description and reported attrition reasons in both programs. In the predominately male workplace setting, 137 (95.1%) of the 144 participants enrolled in the larger cohort study were male, and aside from only 2 female dependents all were employed by the mining company. The median age was 46 years and the median educational level was 6 years. Just over a third of the cohort participants in the workplace (51/144; 35.4%) stopped coming to the clinic for follow-up visits by the seventh month of treatment. For those who discontinued follow-up, 98% were male, the median age was 46 years, the median education level was 5 years, and the average CD4 count was 173 cells per microliter at treatment initiation. We were able to trace two thirds of these patients successfully (30/51; 60%). Among the 30 traced, 26 (86.7%) were found to be alive but to have discontinued ART use (despite remaining in employment) and four (13.3%) had died. Seventeen of these individuals agreed to an interview regarding their reasons for discontinuation of ART. Among those not interviewed the main reasons for refusal was not wanting to return to the clinic and/or being too busy.
FIG. 1.
Sample description and reasons for attrition by program.
In contrast, among the 267 individuals enrolled in the public-sector cohort at baseline 64.3% were female, 36.3% were unemployed, the median age was 37 years and the median education level was 11 years. By the seventh month of treatment only 16.5% (44/267) of the study cohort had discontinued follow-up. Of these patients, 23 (52%) were women. Less than half (42%) of the women who discontinued follow-up were unemployed, while 30% of men who discontinued follow-up were unemployed. The baseline median age was 37.5 years, median level of education was 11 years and the average CD4 count at baseline was 104 cells per microliter. Thirty-seven of these participants (37/44; 84%) were traced successfully. Of the 37 traced successfully, 14 (38%) were alive and had discontinued ART use, 20 (54%) had died, and 3 (8%) had transferred to another ART clinic to receive ART. Of the 14 traced alive, 11 (78.5%) were female and of the 20 who had died 14 (66.7%) were male. Of the 14 traced alive, 10 agreed to take part in further interviews. Of those not interviewed, the main reason for refusal was being too busy, hence not having time for an interview.
The main self-reported reasons for treatment discontinuation among the 27 patients interviewed are organized respectively under the two distinct contexts of ART delivery—workplace versus public sector—within which study participants were first initiated onto ART.
Reasons for discontinuation of ART in the workplace clinic
Disbelief in HIV and ART
Many workplace clinic participants were uncertain about the existence of HIV and/or their own HIV-infected status. Most were unsure about their HIV diagnosis because they felt that they were sick with something else, namely witchcraft:
After checking with my traditional doctor and realizing that I was bewitched, I decided not to continue with treatment [ART]. What is the point of taking ART if this was witchcraft? … my HIV is man-made and needs traditional medicine … I am very well [now] because the traditional doctor took out a small frog that has been in my stomach since I started working so I believe as a result I will be fine. I don't need ART again, it will complicate things. (Male workplace participant)
Some were ambivalent about their HIV status because they did not “know” or could not “see” HIV in themselves, either because they felt or looked healthy or because they did not feel at risk of the disease. One participant described how he “sees” HIV as a disease of thinness and sickness:
I see it [HIV] but I don't know if I have it or not and where is it from and how it works … I see it in people who are said to be HIV positive, I see when a person is getting thinner and is sick, then they say a person has HIV but I really don't know how it works. (Male workplace participant)
He continued by questioning how he could have a sexually transmitted disease when he had always been faithful to his wife:
… with me I am still wondering [how I got HIV] because I only sleep with my wife, I don't go sleeping around … I left home coming to the mines to work and I married my wife, until now I am not naughty at all, I just can't figure out how I got that. (Male workplace participant)
Poor patient–provider interaction and communication
Some participants also displayed mistrust of ART providers, whom they believed diagnosed all patients with HIV regardless of their symptoms:
I hear that we are sick, we are sick, but we don't see what we are suffering from. I mean [I don't see] that all of us might be suffering from one illness (HIV). (Male workplace participant)
I thought there was a mistake somewhere [HIV diagnosis] and I thought everyone was said to be HIV positive as long as they were sick, that is why I opted for a second opinion from my traditional healer. (Male workplace participant)
Workplace participants also described a paternalistic patient/provider relationship that contributed to a fear of contradicting providers' medical advice regarding testing for HIV and ART initiation. One participant described being uncertain about his HIV diagnosis, yet being unable to contradict the doctor's HIV diagnosis:
Participant: No, I don't know it well [HIV], because I only hear people talking about HIV and AIDS. I don't know much. I really don't know how it goes …
Interviewer: Do you believe you have HIV?
Participant: If they [doctors] say so I can't argue with them. (Male workplace participant)
Several participants reported that they were “told” to test for HIV and then prescribed ART, all without being informed of the HIV test results. This was despite the fact that the clinic's counseling protocol included the provision of at least three counseling sessions before starting patients on ART. None of the participants reported questioning their doctor on why they were being put on HIV treatment without an HIV diagnosis.
I don't know if I have it [HIV] or not … they only collected blood, saying they wanted to check if I have it or not but they never told me [the results] … if I have it or not, I don't know. (Male workplace participant)
Fear of workplace discrimination
Workplace participants were not only poorly convinced of the need for treatment, but also felt that the follow-up visits required by the ART clinic created problems for them with their employers. The most frequently cited reason for treatment discontinuation among the workplace program participants was harassment and discrimination by line managers who refused to grant time off work for clinic attendance. Managers in the workplace reportedly queried the need for clinic attendance if the employee “look[ed] fine” and considered repeated absences for clinical follow-up as a way of “abusing sick leave”. In such circumstances, participants often decided to stop attending clinic rather than disclose their status and risk further confrontations, or at worst termination of employment:
I had to choose between losing my job and coming here [clinic] … if your senior wants to know the reason why you go to hospital every month how am I going to tell him the truth? We fought with words … he told me that I am abusing sick leave because I look fine to him … I tried to come forcefully, believe me, that is when he told me that he will recommend medical board and he started treating me differently. (Male workplace participant)
Workplace participants who reported experiencing side effects leading to impairment or loss of functional work capacity also reported discontinuing treatment for fear of making mistakes on the job:
The pills … they make me feel like sleeping … at work I feel like sleeping … at times I skip pills for two days and take them during weekend … I could lose my job if my seniors find me asleep at work or get injured while asleep … that is the reason I decided to stop them [ART] for a while. (Male workplace participant)
Use of nonbiomedical therapies
A number of participants interviewed reported that mistrust and uncertainty about HIV and ART contributed to their decision to use traditional medicines. One participant described how traditional medicines were superior to ART in alleviating his symptoms, which he believed to be caused by witchcraft:
No ways, I was not going to live like this. Let me try the other way round. I then found someone … he said you have been bewitched. He tried … [silence] and he took out something from this leg. Eh … an imbumbuli … it's sort of a bullet from a gun … I've never been shot at, it is just manmade things … they [imbumbuli] created this problem for me, because after the removal of that thing [imbumbuli] I started feeling much better. (Male workplace participant)
Among those who used traditional medicines, most felt that ART and traditional medicines should not be taken together, and therefore stopped taking ART:
I used them [ART] for three months only and I skipped some visits but the pills I took every day, until my traditional doctor ordered me to stop, because the two don't go together. I think it didn't work [ART] because I am not HIV positive. (Male workplace participant)
Reasons for discontinuation of ART use in the public-sector clinic
Financial and travel constraints
In contrast to the workplace clinic participants, who had direct access to the ART clinic through their employment, public-sector clinic participants cited lack of money for transport and/or moving away to be closer to family as the main reasons for discontinuing treatment:
In my family, my father was not working. There was no money. We were borrowing some money from my aunts … I was unable to find money to come to the hospital for my treatment for the last 8 months. (Female public-sector participant)
Among those who moved away, some thought that they could not seek care at another ART clinic without having their original ART clinic file:
I have moved to my home in X [new town] to be with my family … I cannot return to the clinic as I am staying with my mother, my brothers and children. There is no one to look after me in Y [old town]. I didn't bring my [Public-sector ART clinic] file with me, hence I am not taking ART anymore. (Female public-sector participant)
It is important to note that the participants who discontinued ART in the public-sector did not attribute their decision to any provider or system-related factors. Instead, many felt that the clinic provided high-quality care and many expressed a strong desire to return there:
I still miss coming as we had a lot to share as patients. I miss the care I received from the doctors, and please tell my doctor that I miss him. (Female public-sector participant)
In contrast to the workplace, most public-sector participants believed in the existence of HIV and their own HIV-infected status. Only one female participant reported initial doubts about her HIV diagnosis:
I was having fits and admitted to the hospital. That is when the doctors advised me to test for HIV … I did not believe the results because I was never a naughty person … I was tested again at Z clinic [primary health clinic]. That's when I believed I had HIV. (Female public-sector participant)
Despite having dropped out of the programme, nearly all public-sector participants affirmed the beneficial value of ART and some stressed their desire to be able to access treatment again:
ARVs are helpful for this disease that is why I was taking them … I gained weight, I was active, was never tired … I want to continue to take ART so that I should live longer. (Female public-sector participant)
They [ART] were boosting me, because I was very weak the time I was not having them … but after I had them I am so much stronger. (Male public- sector participant)
Only one female participant was uncertain about the value of ART:
“I was well on them, nothing really happened [hesitant] … I don't know how they affected my health because I did not take them for a long time.” (Female public-sector participant)
Among the few participants in this group who reported using traditional medicines, none felt that it interfered with their ART use. One participant described choosing alternative medicines that would not interact negatively with ART:
They [traditional healers] gave me an emetic and an enema, but I did not use them, because it is said that when you have HIV you do not use medication that induces vomiting and diarrhoea so I then went to the church … where they gave me their tea. (Female public-sector participant)
Discussion
Despite being financially better resourced, attrition in the workplace program was double that of the community program. Most workplace participants who discontinued clinical follow-up were found to be alive but to have discontinued ART use, while most in the community program had died. Within the public-sector segment, death was more prevalent among men while treatment discontinuation was more prevalent among women. The higher number of deaths among males in the community program was likely due to later uptake of ART, characterized by lower baseline CD4 counts, a factor linked to increased risk of death.6–8
The study offered a unique opportunity to examine the interplay of organizational context and patient characteristics on participants' motivation to remain within care, once initiated on ART. In the workplace program, many participants reported that line managers refused to approve time off to attend clinic visits. Participants, especially those who were healthy and looked well, feared having to disclose their HIV status to their supervisors and risk further confrontation and/or harassment. Fear of stigma and discrimination has previously been reported to reduce treatment adherence,9–12 but there may be additional “structures of discrimination”13 in industries such as that of the mining company within which the workplace clinic operated. The mining industry is heavily reliant on reaching daily productivity targets. In this setting, managers might judge the need for an employee to take time off as less urgent than the need to achieve targets. Workers receiving treatment in the workplace may also fear that the company's “in-house” ART program could link their health records to their employment records and that this information could be used to justify sidelining them or terminating their employment. Mistrust of the company health service may have led some patients to discontinue follow-up and to minimize or avoid contact with the company health services.
By contrast, most public-sector program participants had voluntarily sought out HIV testing and treatment despite many structural obstacles. They also did so when they were sicker, as evidenced by lower CD4 counts at baseline, compared to the workplace participants. Their experience of being ill or seeing someone die from HIV may have motivated them to test for HIV,14 while feeling physically better on treatment may have reaffirmed their beliefs in the benefits of ART. Participants also reported having had positive experiences of care in the public-sector clinic. Relocation and financial constraints were the main reasons for attrition in this population, especially among women who were more likely to be unemployed than men. This was consistent with similar studies conducted in urban settings in South Africa reporting attrition largely due to factors outside participants' control.14,15
The workplace, through eliminating most structural barriers to ART uptake and proactively referring employees for HIV testing, had an estimated ART coverage exceeding 95% of those needing treatment. Workplace participants were thus less self-selected and perhaps more representative of HIV-infected individuals in need of treatment but not currently being seen in programs that rely mostly on patient-initiated testing.
Attrition reasons in the two patient populations differed in a number of respects, providing the opportunity to identify factors not previously reported in studies conducted among pilot and early ART programs with self-selected patient populations. For example, skepticism regarding the existence of HIV and/or one's own status has seldom been reported in published literature as barriers to retention16–18 but was common in the workplace program. This skepticism may be due to alternative (e.g., supernatural or mediated by human agency) constructs of disease etiology that may be more common in rural settings, such as those from where a majority of the workplace employees originated. Rejection of a biomedical understanding of HIV causation and treatment might also reflect mistrust of the company's health services, grounded in long-standing historical suspicion of Western medicine among previously disadvantaged South African communities.19,20 In the context of a climate of mistrust,20 many patients may reject the belief in the sexual mode of HIV transmission as an extension of their rejection of the racist apartheid interpretation of AIDS.19 These beliefs may have in turn contributed to a higher degree of uncertainty about the health benefits of ART. Skepticism regarding the benefits of ART may also reflect a “healthy worker effect” wherein the healthier workplace population may have been less likely to see the necessity of ART or to experience health improvements on treatment.5
As ART programs increase ART coverage partly by raising minimum CD4 count required for treatment initiation and placing more emphasis on the use of PITC, the first generation of highly self-selected patients enrolled in early ART programs may give way to a second generation of less self-selected, healthier, and perhaps less motivated patients. Among these patients, the existence of alternative beliefs regarding HIV and ART and mistrust of Western medicine may play a larger role in determining attrition.
Limitations
Self-reported accounts of poor adherence may be limited by participants' ability to remember their experiences accurately and some participants wanting to provide socially desirable responses. Also the small sample size may have limited the potential to obtain a conceptually dense theoretical account of attrition.21 However, the main strength of this study is that most patients who started treatment during the study recruitment period in the two clinics were enrolled in the main cohort study. Unlike many previous attrition studies, participants provided contact information and permission to be traced at study recruitment and before starting ART, in case they missed their 6-month clinic visit. All those who missed the 6-month visit by 1 month or more were traced and almost half agreed to participate in the in-depth interviews. Thus, although relatively small in number, the participants interviewed in this qualitative study can be considered more representative of ART patients who discontinued HIV care follow-up, than if the participants had been sampled purposively.
Conclusions and Recommendations
Attrition from care was more common in the well-resourced workplace programme than in the community program. In the workplace, the higher attrition rate may reflect the fact that patients are less self-motivated to start and continue treatment. However, it is important to consider that lower levels of motivation may be related to structural rather than individual-level factors. In workplaces like the mining industry, employees are often under pressure to maintain physical health and working capacity, but lack the social resources and support to do so, which may be reflected in “poor” compliance with health behaviors.22 Efforts to minimize the time between testing and treatment initiation should be balanced with the need to provide adequate forms of support for employees on treatment and tailored baseline counseling that takes existing concepts of health, illness, and healing into account. Moreover, management of employer-provided ART programs could explore peer-based approaches to addressing stigma and discrimination in the workplace and put in place rewards not only for achieving shorter term productivity goals but also for contributing to the overall long-term company goals of maintaining and improving employee health outcomes. In the public-sector program, the high proportion of deaths among those lost from the community program highlights the need for earlier HIV diagnosis and ART initiation to reduce early mortality, especially among men.8 It is essential that social services be strengthened to ensure that the lowest-income patients can obtain government assistance to cover treatment-related costs, especially transport to the clinic. Strategies should also be explored to facilitate pick up of ART at closer primary health care clinics or as part of home-based follow-up programs, if available.23
Acknowledgments
We would like to thank the study participants. We would also like to thank the staff members in the participating clinics, and the staff of the Aurum Institute for their support throughout data collection, analysis, and dissemination.
Funding for this study was provided by the Aurum Institute. Subjects in this study were enrolled in treatment programmes supported by the U.S. President's Emergency Plan for AIDS Relief and by Cooperative Agreement Number PS024055 from the Department of Health and Human Services/Centers for Disease Control and Prevention (CDC), National Center for HIV, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), Global AIDS Program (GAP). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of CDC. Alison Grant was supported by a Public Health Career Scientist award from the UK Department of Health. Gavin Churchyard is supported by grants from the National Institutes of Health (grant# AI069469 and AI51794) and from the President's Emergency Plan for AIDS Relief (PEPFAR) (U2GPS000811, SU062PS024055).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.WHO, UNAIDS, UNICEF. Towards Universal Access-Scaling up Priority HIV/AIDS interventions in the health sector. Progress Report 2009. 2009 [Google Scholar]
- 2.Rosen S. Fox M. Gill C. Patient retention in antiretroviral therapy programs in sub-Saharan Africa: A systematic review. PLoS Med. 2007;5:e298. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anglaret X. Toure S. Gourvellec G, et al. Impact of vital status investigation procedures on estimates of survival in cohorts of HIV-infected patients from Sub-Saharan Africa. J Acquir Immune Defic Syndr. 2004;35:320–323. doi: 10.1097/00126334-200403010-00015. [DOI] [PubMed] [Google Scholar]
- 4.Gill C. Hamer D. Simon J. Thea D. Sabin L. No room for complacency about adherence to antiretroviral therapy in sub-saharan Africa. AIDS. 2005;19:1243–1249. doi: 10.1097/01.aids.0000180094.04652.3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dahab M. Charalambous S. Karstaedt AS, et al. Contrasting predictors of poor antiretroviral therapy outcomes in two South African HIV programmes: A cohort study. BMC Public Health. 2010;10:430. doi: 10.1186/1471-2458-10-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferradini L. Jeannin A. Pinoges L, et al. Scaling up of highly active antiretroviral therapy in a rural district of Malawi: An effectiveness assessment. Lancet. 2006;367:1335–1342. doi: 10.1016/S0140-6736(06)68580-2. [DOI] [PubMed] [Google Scholar]
- 7.Badri M. Lawn SD. Wood R. Short-term risk of AIDS or death in people infected with HIV-1 before antiretroviral therapy in South Africa: A longitudinal study. Lancet. 2006;368:1254–1259. doi: 10.1016/S0140-6736(06)69117-4. [DOI] [PubMed] [Google Scholar]
- 8.Cornell M. Myer L. Kaplan R. Bekker LG. Wood R. The impact of gender and income on survival and retention in a South African antiretroviral therapy programme. Trop Med Int Health. 2009;14:722–731. doi: 10.1111/j.1365-3156.2009.02290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pinheiro CA. de-Carvalho-Leite JC. Drachler ML. Silveira VL. Factors associated with adherence to antiretroviral therapy in HIV/AIDS patients: A cross-sectional study in Southern Brazil. Braz J Med Biol Res. 2002;35:1173–1181. doi: 10.1590/s0100-879x2002001000010. [DOI] [PubMed] [Google Scholar]
- 10.Ramadhani HO. Thielman NM. Landman KZ, et al. Predictors of incomplete adherence, virologic failure, and antiviral drug resistance among HIV-infected adults receiving antiretroviral therapy in Tanzania. Clin Infect Dis. 2007;45:1492–1498. doi: 10.1086/522991. [DOI] [PubMed] [Google Scholar]
- 11.Molassiotis A. Nahas-Lopez V. Chung WYR. Lam SWC. Li CKP. Lau TFJ. Factors associated with adherence to antiretroviral medication in HIV infected patients. Int J STD AIDS. 2002;13:301–310. doi: 10.1258/0956462021925117. [DOI] [PubMed] [Google Scholar]
- 12.Dlamini PS. Wantland D. Makoae LN, et al. HIV stigma and missed medications in HIV- positive people in five African countries. AIDS Patient Care STDs. 2009;23:377–387. doi: 10.1089/apc.2008.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dickinson D. Managing HIV/AIDS in the South African workplace: Just another duty? S Afr J Econ Manage Sci. 2003;6:25–49. [Google Scholar]
- 14.Gilbert L. Walker L. “They (ARVs) are my life, without them I'm nothing”—Experiences of patients attending a HIV/AIDS clinic in Johannesburg, South Africa. Health Place. 2009;15:1123–1129. doi: 10.1016/j.healthplace.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Dalal R. MacPhail C. Mqhayi M, et al. Characteristics and outcomes of adult patients lost to follow-up at an antiretroviral treatment clinic in Johannesburg, South Africa. Epidemiol Soc Sci. 2008;47:101–107. doi: 10.1097/QAI.0b013e31815b833a. [DOI] [PubMed] [Google Scholar]
- 16.Dahab M. Charalambous S. Hamilton R, et al. “That is why I stopped the ART”: Patients' & providers' perspectives on barriers to and enablers of HIV treatment adherence in a South African workplace programme. BMC Public Health. 2008;18:63. doi: 10.1186/1471-2458-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Babb DA. Pemba L. Seatlanyane P. Charalambous S. Churchyard GJ. Grant AD. Use of traditional medicine by HIV-infected individuals in South Africa in the era of antiretroviral therapy. Psychol Health Med. 2007;12:314–320. doi: 10.1080/13548500600621511. [DOI] [PubMed] [Google Scholar]
- 18.Nam SL. Fielding K. Avalos A. Dickinson D. Gaolathe T. Geissler PW. The relationship of acceptance or denial of HIV-status to antiretroviral adherence among adult HIV patients in urban Botswana. Soc Sci Med. 2008;67:301–310. doi: 10.1016/j.socscimed.2008.03.042. [DOI] [PubMed] [Google Scholar]
- 19.Schneider H. Fassin D. Denial and defiance: a socio-political analysis of AIDS in South Africa. AIDS. 2002;16:S45–S51. doi: 10.1097/00002030-200216004-00007. [DOI] [PubMed] [Google Scholar]
- 20.Fassin D. London: University of California Press; 2007. When Bodies Remember: Experiences and Politics of AIDS in South Africa. [Google Scholar]
- 21.Green J. Thorogood N. Qualitative Methods for Health Research. 1st. London: Sage Publications; 2004. [Google Scholar]
- 22.Campbell C. Migrancy, masculine identities and AIDS: The psychosoical context of HIV transmission on the South African gold mines. Soc Sci Med. 1997;42:273–281. doi: 10.1016/s0277-9536(96)00343-7. [DOI] [PubMed] [Google Scholar]
- 23.Jaffar S. Amuron B. Foster S, et al. Rates of virological failure in patients treated in a home-based versus a facility-based HIV-care model in Jinja, southeast Uganda: A cluster-randomised equivalence trial. Lancet. 2009;374:2080–2089. doi: 10.1016/S0140-6736(09)61674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]