Abstract
In a randomized clinical trial with 111 families of parents with a history of major depressive disorder (86% mothers; 86% Caucasian), changes in adolescents’ (mean age 11 years; 42% female) coping and parents’ parenting skills were examined as mediators of the effects of a family group cognitive behavioral preventive intervention on adolescents’ internalizing and externalizing symptoms. Changes in hypothesized mediators were assessed at 6-months and changes in adolescents’ symptoms were measured at 12-month follow-up. Significant differences favoring the family intervention as compared with a written information comparison condition were found for changes in composite measures of parent-adolescent reports of adolescents’ use of secondary control coping skills and direct observations of parents’ positive parenting skills. Changes in adolescents’ secondary control coping and positive parenting mediated the effects of the intervention on depressive, internalizing and externalizing symptoms accounting for approximately half of the effect of the intervention on the outcomes. Further, reciprocal relations between children’s internalizing symptoms and parenting were found from baseline to 6-month follow-up. Implications for the prevention of psychopathology in offspring of depressed parents are highlighted.
Keywords: Prevention, parental depression, mediation, coping, parenting, family
Depression in parents is a significant risk factor for both internalizing and externalizing psychopathology in children and adolescents (e.g., Goodman, 2007; Weissman et al., 2006). Accordingly, the development and testing of preventive interventions targeting children of parents with a history of major depression has been identified as a significant public health priority in a recent report from the Institute of Medicine (England & Sims, 2009). Three randomized clinical trials have provided evidence for the efficacy of preventive interventions with this high-risk population. Two studies have found evidence that a cognitive-behavioral intervention for high-risk adolescents of parents with a history of depression was associated with lower depressive symptoms and episodes of major depressive disorder in adolescents, one assessing outcomes at 12-month follow-up (Clarke et al., 2001) and a second assessing episodes of depression at 8-months (Garber et al., 2009). In a recent third study with adolescents and their parents with a history of depression, a family group cognitive-behavioral intervention led to lower depressive, mixed anxiety-depression, internalizing, and externalizing symptoms and lower rates of psychiatric diagnoses at a 12-month follow-up (Compas et al., 2009). At present, however, possible mediators of the effects of these preventive interventions on mental health outcomes in children and adolescents of depressed parents have not been examined.
Identification of mediators of the effects of preventive interventions is important for the development of more efficacious interventions and to the advancement of theoretical understanding of mechanisms of risk (e.g., Kazdin, 2008; Kraemer et al., 2002; La Greca, Silverman, & Lochman, 2009). First, clinical practice can be enhanced through the identification of the active ingredients in interventions to focus future training and implementation efforts on those components that are most responsible for beneficial outcomes (LaGreca et al.). Most preventive interventions include multiple components; therefore, tests of the role of various aspects of an intervention are necessary to determine which elements could be emphasized and enhanced while other components could be reduced or omitted. Second, theory-driven tests of mediation can contribute to understanding of processes that link risk factors (e.g., parental depression) and outcomes (e.g., child/adolescent psychopathology). Further, most prevention trials examine the effects of interventions on several different outcomes. Mediators can be tested to determine if their effects are specific to one outcome or if a given mediator affects more than one outcome. Therefore, tests of mediation can contribute to understanding broad vs. specific risk and protective processes (e.g., LaGreca et al.; Tein et al., 2004; Zhou et al., 2008).
The current study examined potential mediators of a family group cognitive-behavioral (FGCB) preventive intervention for families of parents with a history of depression (Compas et al., 2009). The intervention was based on theory and research identifying two risk and protective processes in families of depressed parents--disruptions in parenting (and resulting parent-child stress that occurs in families of depressed parents) and the ways that children cope with parent-child stress (e.g., Jaser et al., 2005, 2008; Langrock et al., 2002). Parental depression is associated with parents’ withdrawal, unavailability, irritability, and intrusiveness that combine to form a pattern of inconsistent and affectively negative parenting (Lovejoy et al., 2000). These parenting behaviors contribute to stressful family environments for children of depressed parents (Hammen, Brennan, & Shih, 2004). Previous research has shown that parents continue to present problems in parenting and that environments in these families continue to be highly stressful even when parents are out of episode (Seifer et al., 2001). The adverse effects of these negative parenting behaviors and stress are mitigated in part by adolescents’ use of secondary control coping skills (acceptance, cognitive reappraisal, positive thinking, distraction) to adjust to these stressors (Jaser et al., 2005, 2008). That is, adolescents who cope with stressful interactions with their parents by accepting and reappraising these interactions, and by engaging in positive thoughts or activities to distract themselves, have lower levels of internalizing and externalizing symptoms than adolescents who do not use these strategies (e.g., Jaser et al., 2005).
Based on the identification of these risk and protective processes, a FGCB intervention was designed to use a two-pronged approach to enhance positive parenting skills in parents with a history of depression and to teach secondary control coping skills in children of these parents (Compas, Langrock, Keller, Merchant, & Copeland, 2001). Therefore, these two active components of the intervention, changes in parenting and changes in children’s coping, were selected a priori as possible mediators of children’s mental health outcomes. The efficacy of this FGCB intervention in reducing and preventing adolescents’ internalizing and externalizing psychopathology was tested in a randomized clinical trial (RCT) in comparison with the provision of written information only (Compas et al., 2009). Significant effects favoring the FGCB intervention at follow-up were found on adolescents’ depressive symptoms, anxiety-depression, total internalizing symptoms, and total externalizing problems.
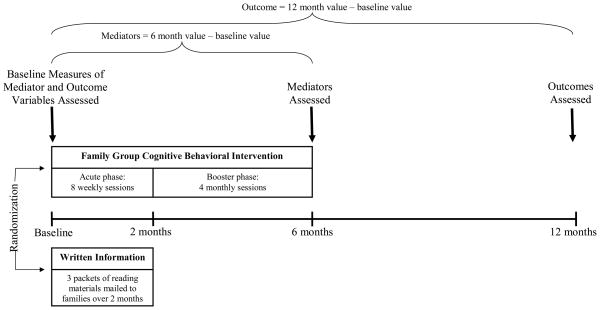
In the context of this RCT, the current study examined changes in adolescents’ use of secondary control coping skills and changes in parenting as mediators of the effects of this FGCB preventive intervention. Multiple methods, including composite indicators created from adolescents’ and parents’ reports and direct observations, were used to assess the hypothesized mediators, and adolescents’ mental health symptoms were measured by both adolescents’ and parents’ reports. Further, to establish that changes in the mediators preceded changes in adolescents’ mental health outcomes, changes in the mediators were assessed from baseline to 6-month follow-up and changes in adolescents’ internalizing and externalizing symptoms were assessed from baseline to 12-month follow-up (see Figure 1). Parents’ depressive symptoms at baseline were controlled for in all analyses.
Figure 1.
Study design.
First, we hypothesized that adolescents in the FGCB intervention would increase their use of secondary control coping (e.g., acceptance, cognitive reappraisal) in response to stressful interactions with their parents as compared to adolescents in the written information condition at the 6-month follow-up as compared with baseline levels of these behaviors. Second, we hypothesized that parents in the FGCB intervention would display higher rates of positive parenting behaviors (e.g., warmth, child centeredness, responsive listening) and lower rates of negative parenting behaviors (e.g., hostility, intrusiveness, neglecting/distancing) compared to parents in the written information condition at the 6-month follow-up as compared with baseline levels of these behaviors. Third, we hypothesized that changes in adolescents’ coping and changes in positive and negative parenting at 6-months would mediate the effects of the intervention on adolescents’ internalizing and externalizing symptoms at 12-months, controlling for baseline levels of these problems. Finally, based on recent findings suggesting that changes in parenting and changes in children’s emotional/behavioral problems may be reciprocally related (Silverman et al., 2009), we conducted supplementary analyses to examine changes in internalizing and externalizing symptoms as predictors of changes in parenting.
Method
Participants
Participants included 111 parents with current or past major depressive disorder during the lifetime of their child(ren) and 155 children of these parents from the areas in and surrounding Nashville, Tennessee and Burlington, Vermont. This sample includes all 111 families that comprised the sample reported in Compas et al. (2009); however, for families with multiple children in the target age range, one child was randomly selected for the current analyses (see below), yielding a sample of 111 children.
Target parents with a positive history of depression included 95 mothers (mean age of 41.9, SD = 6.8) and 16 fathers (mean age = 48.3, SD = 8.2). Parents’ level of education included less than high school (7.2%), completion of high school (8.1%), some college (31.5%), college degree (27%), and graduate education (26.1%). Eighty-six percent of target parents were Euro-American, 5.4% African-American, 2.7% Hispanic-American, 1% Asian-American, 1% Native American, and 3.6% mixed ethnicity. The racial and ethnic compositions of the samples were representative of the regions in Tennessee and Vermont from which they were drawn based on the 2000 U.S. Census data. Annual family income ranged from less than $5,000 to more than $180,000, with a median annual income of $40,000. Sixty-four percent of parents were married/partnered, 21.6% were divorced, 3.6% separated, 9.0% had never married, and 1.8% were widowed. Families randomized to the FGCB and written information conditions did not differ significantly on any of these demographic variables.
Children enrolled in the study and included in the current analyses ranged from 9 to 15-years-old and included 47 girls (mean age = 11.4, SD = 1.9) and 64 boys (mean age = 11.3, SD = 2.1). Seventy-eight percent of children were Euro-American, 7.3% African-American, 4.6% Asian American, 1% Hispanic American, and 9.2% mixed ethnicity. We targeted ages 9 to 15-years-old in order to intervene with children/adolescents before the documented increase in rates of depression that occurs in early to mid-adolescence (e.g., Hankin et al., 1998) and to include children who were old enough to learn the relatively complex cognitive coping skills taught in the intervention (see Compas et al., 2009, for a more detailed description of the sample).
Twenty-seven parents (24%) were in a current episode of major depression and 84 parents (76%) were not in episode at the time of the baseline assessment and randomization. Parents had experienced a median of three episodes during their child’s life. Thus, all of the parents had a history of depression and 24% were currently in episode (one parent experienced only one MDE during the post partum period). We compared the children and parents in our sample based on parents’ depression status at baseline and parental depression status was only related to externalizing scores on the CBCL. We also compared our sample at baseline on parental marital status; the only significant difference was found on observed negative parenting.
Setting and Personnel
All study procedures were approved by the Institutional Review Boards at Vanderbilt University and the University of Vermont. All assessments and group intervention sessions were conducted in the Department of Psychology and Human Development at Vanderbilt University and the Psychology Department at the University of Vermont. Doctoral candidates in clinical psychology and staff research assistants, who were naive to condition, conducted the structured diagnostic interviews after receiving extensive training. Each group intervention was co-facilitated by one of three clinical social workers and one of nine doctoral-level students in clinical psychology. Facilitators were trained by reading the intervention manual, listening to audiotapes of a pilot intervention, and discussing and role-playing each session with an experienced facilitator. Ongoing supervision was conducted by two Ph.D. clinical psychologists.
Measures
Mediators
Parent-adolescent reports of adolescents’ coping
The parental depression version of the Responses to Stress Questionnaire (Connor-Smith et al., 2000; Jaser et al., 2005, 2008) was used to assess how adolescents responded to stressors related to their parents’ depression (e.g., My mom seems to be sad or cries a lot of the time; My mom does not want to do things with the family; My mom is too upset, tense, grouchy, angry, and easily frustrated). In reference to these stressors, items cover five factors of coping and stress responses: primary control engagement coping, secondary control engagement coping, disengagement coping, involuntary engagement/stress reactivity, and involuntary disengagement (Connor-Smith et al., 2000). Adolescents and their parents were asked separately to rate each item with regard to the degree/frequency with which the adolescent responded to the identified stressors (1 = “not at all” to 4 = “a lot”). To control for response bias and individual differences in base rates of item endorsement, proportion scores were calculated by dividing the total score for each factor by the total score for the entire RSQ (Vitaliano, Maiuro, Russo, & Becker, 1987). We focused our analyses on secondary control coping (acceptance, positive thinking, cognitive restructuring, distraction) in the current study because these coping skills were identified in previous research to be most useful for coping with stress related to parental depression and were therefore taught in the FGCB intervention. Internal consistency for secondary control coping was α = .72 for parents and .78 for adolescents at baseline and .82 for parents and .77 adolescents at 6-months. To reduce the number of analyses and to reduce effects due to biases from single informants, a composite measure of adolescents’ coping was created by converting scores from adolescent and parent reports to z-scores and calculating the mean z-score for each participant (α = .75 for baseline and .78 at 6-months).
Observations of parenting
A global coding system, the Iowa Family Interaction Rating Scales (IFIRS; Melby, Conger et al., 1998), was used to code two videotaped 15-minute conversations, first about a pleasant activity that the target parent and child enjoyed doing together in the past couple of months, and second about a stressful time when the target parent was really depressed, down, or grouchy, which made it difficult for the family. The IFIRS is a global coding system designed to measure behavioral and emotional characteristics at both the individual and dyadic level. Behaviors are coded on two general types of scales: Individual Characteristic Scales and Dyadic Interaction Scales. Each behavioral code is rated on a 9-point scale, ranging from 1 which indicates that the behavior is “not at all characteristic” of the subject during the interaction to a 9 which indicates that the behavior is “mainly characteristic.” In determining the score for each code, frequency and intensity of behavior, as well as the contextual and affective nature of the behavior, are considered. This macro-level system is ideal for assessing patterns of behavior that comprise the ongoing, dynamic process of interaction (Melby & Conger, 2001). The validity of the IFIRS system has been established using correlational and confirmatory factor analyses (Aldefer et al., 2008; Melby & Conger, 2001).
Training for the IFIRS consisted of in-depth studying of the manual, a written test of the scale definitions, and establishment of inter-rate reliability. Successful completion of training consisted of passing a written test with at least 90% correct, and achieving at least 80% reliability on observational tests. Raters remained naive to the randomization of families to the FGCB intervention vs. the written information condition. Weekly training meetings were also held in order to prevent coder drift and to provide a forum in which questions about the different codes were addressed. All interactions were double-coded by two independent observers and coders met to establish consensus on any discrepant codes (i.e., codes that were rated greater than 2 points apart on the 9-point scales).
Following procedures used previously with the IFIRS codes (e.g., Lim et al., 2008; Melby et al., 1998), scores were averaged across tasks and then composite codes were created for positive and negative parenting that reflected the parenting skills that were taught in the FGCB intervention which were based on theory-driven and empirically-supported disruptions in parenting related to depression as well as establishing authoritative parenting skills (i.e., balance of warmth and structure). The positive parenting composite included parents’ warmth, child-centered behaviors, positive reinforcement, quality time, listener responsiveness, and child monitoring (α = .81 at baseline and .85 at 6-months). The negative parenting composite included parental negative affect (sadness and positive mood, reverse scored), hostility, intrusiveness, neglect/distancing, and externalize negative (α = .70 at baseline and .73 at 6-months).
Parental depressive symptoms
Parents’ current depressive symptoms were assessed at baseline with the Beck Depression Inventory-II (BDI-II), a standardized and widely used self-report checklist of depressive symptoms with adequate internal consistency (α = .91) and validity in distinguishing severity of MDD (Beck et al., 1996; Steer, Brown, Beck & Sanderson, 2001). Internal consistency in the current sample was α = .92.
Adolescents’ Mental Health Outcomes
Adolescents’ depressive symptoms
Depressive symptoms were assessed with the Center for Epidemiologic Studies-Depression scale (CES-D; Radloff, 1977), a self-report measure of the frequency of 20 depressive symptoms over the past week using a 4-point Likert scale. The CES-D is short and easy to read, has been successfully administered in several large school samples (e.g., Fendrich et al., 1990), and has good psychometrics (α = .89; test-retest reliability = .61; sensitivity of 83.7 and specificity of 75.2 predicting current MDD) with youth (Roberts et al., 1990). Internal consistency in the current sample was α = .91 at baseline and .84 at 12-months. The CES-D was used by Clarke et al. (2001) as a primary outcome in their prevention trial and was used in the current study to match the scales from this earlier study.
Adolescents’ internalizing and externalizing symptoms
The Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) was used to assess symptoms of anxiety/depression (as a measure of general emotional distress) and total internalizing and externalizing problems in children and adolescents. These scales were selected to represent the range of problems that have been identified in children of depressed parents and to match the scales reported by Clarke et al. (2001) and Beardslee et al. (2007). The CBCL includes a 118-item checklist of problem behaviors that parents rate as not true (0), somewhat or sometimes true (1), or very true or often true (2) of their child in the past 6 months. Adolescents completed the Youth Self-Report (YSR; Achenbach & Rescorla, 2001), the self-report version of the CBCL for adolescents ages 11 to 18-years-old. Reliability and validity of the CBCL and YSR are well established (Achenbach & Rescorla, 2001). Internal consistency for the scales used in this study ranged from α = .84 to .94 for the CBCL and α = .84 to .90 for the YSR. Test-retest reliability ranged from r = .82 to .91 for the CBCL and r = .74 to .89 for the YSR. Internal consistency in the current sample ranged from α = .79 to .91 for the scales used in this study. Nine and 10 year-old children completed the YSR to allow for complete data on all measures. The internal consistency for the YSR scales was adequate with this younger age group in the current sample (all alphas ≥ .80). Raw scores on the CBCL and YSR scores were used in all analyses to maximize variance (i.e., some variability is lost when the raw scores are converted to T scores). However, T scores are presented in Table 1 to allow for comparison to age and gender norms.
Table 1.
Means and standard deviations of parent depressive symptoms, adolescent mental health outcomes, adolescent coping, and parenting.
| Baseline | 6-months | 12-months | ||||
|---|---|---|---|---|---|---|
| Written Information | FGCB | Written Information | FGCB | Written Information | FGCB | |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Parent Depressive Symptoms | ||||||
| BDI-II | 16.79 (10.69) | 16.22 (12.05) | 14.10 (10.27) | 9.86 (9.75) | 14.38 (11.99) | 10.89 (11.07) |
| Adolescent Mental Health | ||||||
| CES-D | 13.32 (11.11) | 13.29 (10.35) | 10.06 (8.47) | 9.04 (8.34) | 9.64 (8.23) | 6.80 (5.77) |
| YSR (T scores) | ||||||
| Anxiety-Depression | 57.30 (8.04) | 56.07 (7.80) | 54.06 (6.67) | 51.72 (2.69) | 55.73 (8.63) | 51.55 (3.13) |
| Internalizing | 53.56 (11.73) | 54.96 (10.63) | 46.92 (12.27) | 46.69 (9.41) | 50.42 (12.72) | 44.63 (8.59) |
| CBCL (T scores) | ||||||
| Externalizing | 54.37 (8.37) | 52.41 (12.03) | 53.03 (9.04) | 48.66 (11.16) | 52.35 (9.21) | 47.77 (11.54) |
| Mediators | ||||||
| Parent-Adolescent Report of Adolescents’ Secondary Control Coping (z-scores) | .10 (.65) | −.08 (.84) | −.24 (.81) | .18 (.69) | -- | -- |
| Observed Positive Parenting | 28.81 (4.97) | 27.94 (4.82) | 27.74 (5.14) | 28.87 (5.56) | -- | -- |
| Observed Negative Parenting | 23.34 (5.17) | 22.32 (4.75) | 27.07 (5.20) | 24.60 (5.15) | -- | -- |
Design and Procedures
Figure 1 depicts the overall design of the study (see Compas et al., 2009, for details of patient screening and randomization). To model change in the mediators and outcomes, parenting and adolescents’ coping were assessed at baseline and at 6-month follow-up (after completion of the acute phase of the intervention and the booster sessions) and adolescents’ internalizing and externalizing symptoms were assessed at baseline and 12-month follow-up.
Retention rates
Through the 12-month follow-up, 85.6% of the families were retained in the study (82% of families assigned to the intervention and 89% of the comparison group), as defined by the provision of data for at least one follow-up data collection point.
Intervention and Comparison Conditions
Family group intervention
The family group cognitive-behavioral (FGCB) intervention is a manualized 12-session program (8 weekly and 4 monthly sessions) for up to 4 families in each group (Compas et al., 2009). The program is designed for participation by both parents and children. Goals are to educate families about depressive disorders, increase family awareness of the impact of stress and depression on functioning, help families recognize and monitor stress, facilitate the development of adaptive coping responses to stress, and improve parenting skills.
During sessions 1–3, parents and children meet together with the two facilitators to learn about depression and stress in families and receive an overview of skills for coping with depression. During session 4–8, parents and children meet together with the two facilitators briefly at the beginning and end of each session to discuss homework and practice skills. Parents and children meet separately for the majority of the time during each of these sessions, with parents learning parenting skills (i.e., praise, positive time with children, encouragement of child use of coping skills, structure, and consequences for positive and problematic child behavior) from one facilitator and children learning skills for coping with their parent’s depression from the other facilitator. The core coping skills are summarized by the acronym ADAPT: Acceptance, Distraction, Activities, and Positive Thinking which represent secondary-control coping skills. During sessions 1–8, skills are taught through didactic instruction, viewing a videotape, modeling, role-playing, and homework assignments.
The monthly booster sessions 9–12 are designed to problem-solve difficulties with implementation of parenting and child coping skills at home, provide additional practice of skills, support positive changes which have occurred, and assign new homework to reinforce the use of these skills. Parents and children meet together part of the time and separately part of the time during these sessions (see Compas et al., 2009, for more details on the intervention, including evaluation of treatment integrity).
Written information condition
The Written Information comparison condition was modeled after a self-study program used successfully by Wolchik et al. (2000) in their preventive intervention trial for families coping with parental divorce and the lecture information condition used by Beardslee et al. (2007). Families were mailed written materials to provide education about the nature of depression, the effects of parental depression on families, and signs of depression in children. Separate materials were developed for parents and children. Materials for children were based on age, with 9–11 year olds receiving materials written at a lower reading level than for 12–15 year olds. Following the method used by Wolchik et al., materials were sent in three sets over an 8-week interval to correspond with the first eight sessions in the FGCB intervention. Families were provided with a schedule for reading these materials. Research assistants checked with the families to ensure that they received the materials through the mail.
Data Analytic Approach
Analyses of mediation: Multivariate mixed-effects model
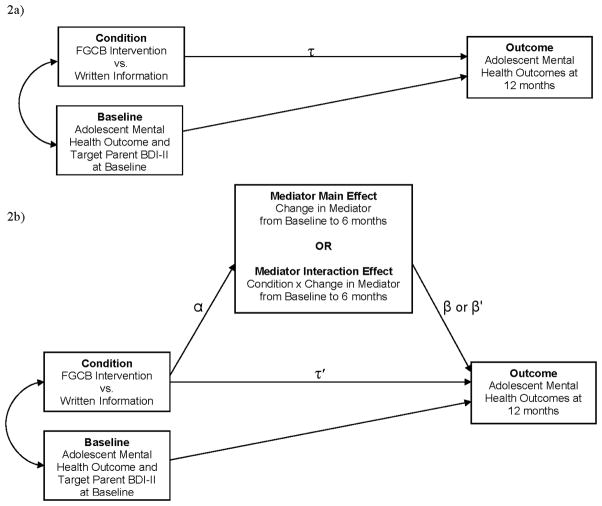
As depicted in Figure 2b, MacKinnon et al. (2002) propose that evidence for mediation is found by examining the joint significance of the path from the intervention to the mediator (α) and the path from the mediator to the outcome (β) after accounting for the effects of the intervention. Kraemer et al. (2002) propose that evidence for mediation of an intervention requires random assignment to an intervention and a comparison condition, a significant association between the intervention and change in the mediator (α), and either a significant main effect of changes in the mediator on changes in the outcome (β) or a significant effect of the interaction between the intervention and change in the mediator on changes in the outcome (β′). Further, MacKinnon et al. (2002) and Kraemer et al. (2002, 2008) argue that to establish mediation one must assess for changes in the mediator prior to and independent of changes in outcome. In prevention research, it is optimal to test for mediation by measuring the mediator after completion of the intervention program and to control for baseline levels for each proposed mediator and outcome variable. Therefore, in our mediation analyses we calculated a change score from baseline for each mediator variable (at 6-months in the present study), and measured the outcomes at a later follow-up assessment (at 12-months in the present study), covarying for baseline levels of these outcome variables as well as covarying for baseline levels of parents’ baseline depressive symptoms.
Figure 2.
Figure 2a and 2b. Heuristic model of mediation pathways of treatment effects on adolescent outcomes with and without the inclusion of the mediators.
A mixed-effects model was used to test the effects of the intervention on the mediators (α path) and to test the effects of change in the mediators on change in the outcomes (β and β′ paths). Specifically, we used a mixed-effects model developed for the analysis of treatment effects in the context of partially nested designs (Bauer, Sterba, & Hallfors, 2008). Similar to the approach used to test for the effects of the intervention on the outcome measures (Compas et al., 2009), using SAS PROC MIXED with restricted maximum likelihood estimation (i.e., method = REML), for each of the mediator variables we implemented a multivariate, mixed-effects model to test the effect of intervention condition (FGCB vs. Written Information) at 6-month follow-up. All participants were retained in the data analysis, including those with partial data. We treated our time 1 (baseline) measure of the outcome and parents’ baseline depressive symptoms on the BDI-II as global covariates. Within the FGCB intervention arm of the study, each set of participants was nested within one of the 14 FGCB intervention groups comprised of up to four families per group. Within the Written Information comparison arm, there was no such nesting. Fixed effects included our baseline and 6-month intercepts. Intervention (condition) was a random effect at baseline and 6-months, which allowed intervention means at each time point to vary across intervention condition. This amounted to estimating a between-groups random effect variance for intervention at each time point and estimating a within-group residual variance.
The FGCB intervention condition was coded in two ways to address the separate recommendations of Kraemer et al. (2002) for tests of mediation and of Bauer et al. (2008) to account for partial nesting. Following recommendations of Bauer et al., we coded the intervention condition as 1 and the comparison condition as 0 in the RANDOM statement of the Proc MIXED code. Because we included the treatment × mediator interaction terms, we followed the recommendation of Kraemer et al. and also coded the intervention condition as .5 and the comparison condition as −.5 in the MODEL statement of the MIXED code.
The dfs vary across analyses because they are approximated, not exact, and the information involved in the approximation varies across analyses. In the mixed model, when there is a complex covariance structure and an unbalanced sample size (as in the current analyses), there is an unknown null distribution for the F-statistic (Schaalje, McBride & Fellingham, 2002). Several ways of approximating this test distribution have been proposed in this context, and the most commonly recommended one (e.g., Fitzmaurice, Laird & Ware, 2004, p. 98; Fitzmaurice, Davidian, Verbeke & Molenberghs, 2009 p. 274) was used here--the Kenward-Roger (1997) method. This method uses a Taylor series approximation to generate approximate moments of the null distribution of the test statistic and equates these to an F-distribution to solve for a scaling factor and denominator degrees of freedom. Using this approximation, df may not be integers (Schaalje et al.).
Effect sizes for the mediators were calculated by computing a proportion of the effect of the intervention that was accounted for by the mediator. The numerator consisted of the difference between the direct effect of the intervention on outcome and the indirect effect of the intervention on outcome (τ-β) after controlling for effects of covariates, the baseline measure of the outcome variable as well as the parent’s baseline level of depressive symptoms measured by the BDI-II. The denominator consisted of the direct treatment effect (τ). This proportion-based method of calculating effect size is based on approaches presented by MacKinnon et al. (2007)1. We have also reported the unstandardized estimates (B’s) and SE’s for the effect of the intervention on the outcomes without the mediators (τ) and in the presence of the mediators (τ′); see Figure 2. Although other methods of computing effect sizes are reported in the literature (e.g., Fairchild et al., 2009), these methods are not appropriate for the current study’s multilevel model with a hierarchical structure that does not use ordinary least squares estimation.
We estimated power for our mediation analyses based on the parameters presented by MacKinnon et al. (2004). With a sample of 111 families, we have adequate power to detect medium to large effects.
Results
Preliminary Analyses
Means and standard deviations of the hypothesized mediators through 6-months and mental health outcomes through 12-months are presented in Table 1. Consistent with the expected effects of randomization, there were no significant differences between the FGCB intervention and the Written Information comparison condition at baseline. Adolescents’ scores on the CES-D at baseline correspond to mild to moderate levels of depressive symptoms. Specifically, the percentage of children at baseline who were in the clinical range on the anxiety/depression scale (i.e., T score ≥ 70) was 7.6% on the YSR and 14.2% on the CBCL (on the basis of normative data, 2% would be expected to exceed this narrow-band scale cutoff). The percentage in the clinical range at baseline on the internalizing scale (i.e., T score > 63) was 22.9% on the YSR and 37.7% on the CBCL; for the externalizing scale (i.e., T score > 63) 17.9% on the CBCL (10% would be expected to exceed these broad-band scale cutoffs on the basis of normative data). These data indicate that, as expected, this is an at-risk sample as reflected by moderately elevated mean T scores and the portion of the sample in the clinical range for various indicators of internalizing problems and parents’ reports of externalizing problems (2–7 times greater than would be expected on the basis of the norms). These levels of problems are consistent with the CBCL T scores reported for children of depressed parents in other studies, including the STAR*D trial (Foster et al., 2009), indicating that our sample is representative of children of parents with a history of depression. Further, because this was a selective prevention trial, children who met criteria for a current depressive episode were screened out, as they were not candidates for prevention of depression.
Parents’ BDI-II scores at baseline reflect low to moderately elevated levels of current depressive symptoms. As noted above, 24% of parents were in an episode of depression at baseline and had experienced a median of three episodes in their child’s life. Thus, this sample represents adolescents who are at risk for psychopathology as a result of exposure to a history of parental depression (see Compas et al., 2009, for more details).
In some cases more than one child from the same family participated. To address the possibility of non-independence, intraclass correlations (ICCs) were calculated to test the independence versus non-independence of children from the same families. ICCs were calculated to determine if there were significant differences as a function of parents completing a set of questionnaires on multiple children (a possible violation of independence of informant) and for children from the same family. The ICCs were non-significant and very small in magnitude ranging from .06 to .12, all p’s > .10, with the exception of the CBCL externalizing scale for which the ICC was .46, p = .002. ICCs for the outcome variables were also calculated for multiple families within groups for families randomized to the FGCB intervention and these ranged from .04 to .19, all non-significant.
We conducted ICCs to test for independence in the measures of the mediators (positive and negative parenting based on coding of observations of parent-child interactions and children’s coping as measured by the composite of parent and child reports on the RSQ). These analyses revealed that the ICCs for multiple children per family were non-significant for the composite measure of children’s coping (ICC = .16, p = .18). However, the ICCs were significant for observed positive (ICC = .66, p < .001) and negative parenting (ICC = .73, p < .001), indicating that there was significant within-family similarity in parents’ behaviors with their children. Therefore, we conducted mediation analyses using a much more conservative approach that includes only one child (n = 111) randomly selected for each family. The ICCs for the mediators for multiple families within groups in the FGCB intervention condition were all small in magnitude (less .13) and non-significant.
Direct Effects of Intervention on Outcomes
Due to the reduction of participants as a result of randomly selecting one child per family (n = 111), the effects of the intervention on the 12-month outcomes were reanalyzed controlling for baseline levels of these measures as well as covarying for parents’ depressive symptoms at baseline (τ path in Figure 2). Significant effects favoring the FGCB intervention as compared to the Written Information comparison condition were found for adolescent self-reports of depressive symptoms on the CES-D as well for the anxiety/depression and internalizing subscales on the YSR. Additionally, significant effects were found for parent reports of adolescent’s externalizing symptoms on the CBCL. Despite the reduction in the sample due to randomly selecting one child per family, these statistically significant effects of intervention on child outcomes at 12-months yielded effect sizes that were comparable to findings presented on the full sample (see Compas et al., 2009): CES-D, d = .36; YSR anxiety/depression, d = .48; YSR internalizing, d = .55; CBCL externalizing, d = .36.
Effects of Intervention on Mediators
The effects of the intervention on the hypothesized mediators at the 6-month follow-up, controlling for baseline levels of the mediator, are summarized in Table 2. Significant effects favoring the FGCB intervention as compared with the written information comparison condition were found for mediators assessed by the composite parent/adolescent report measure of adolescents’ secondary control coping and observations of positive, but not negative parenting. That is, the FGCB intervention as compared with the written information comparison condition was associated with significant changes in adolescents’ use of secondary control coping (p < .001) and observed positive parenting behaviors (p < .01). Thus, two of the three hypothesized mediators met the first criterion defined by MacKinnon et al. (2002) as necessary to establish mediation (α path in Figure 2b) based on the joint significance test.
Table 2.
Effects of intervention on adolescent coping and parenting mediators (α path): Type 3 fixed effects of intercept, condition, BDI-II covariate, and the Time 1 covariate on each mediator.
| Effect | Baseline | 6-months | ||
|---|---|---|---|---|
| df | F | df | F | |
| Parent-Adolescent Report of Adolescents’ Secondary Control Coping | ||||
| Intercept | -- | -- | 1, 67.2 | .50 |
| BDI-II (covariate) | -- | -- | 1, 60.9 | .25 |
| Baseline (covariate) | -- | -- | 1, 58.3 | 23.30*** |
| Intervention (α) | 1, 98.1 | 1.61 | 1, 63.2 | 11.35*** |
| Observed Positive Parenting | ||||
| Intercept | -- | -- | 1, 50.9 | 3.50* |
| BDI-II (covariate) | -- | -- | 1, 50.9 | .28 |
| Baseline (covariate) | -- | -- | 1, 50.4 | 40.44*** |
| Intervention (α) | 1, 96.7 | .77 | 1, 51 | 6.02** |
| Observed Negative Parenting | ||||
| Intercept | -- | -- | 1, 45.2 | 20.98*** |
| BDI-II (covariate) | -- | -- | 1, 49.6 | 1.62 |
| Baseline (covariate) | -- | -- | 1, 42.1 | 28.32*** |
| Intervention (α) | 1, 96.1 | 1.13 | 1, 18.7 | 2.27 |
p < .05;
p < .01,
p<.001
Analyses of Mediation of Intervention Effects on Mental Health Outcomes
Tests of the effects of the mediators on the outcomes are presented in Table 3. As outlined by Kraemer et al. (2002), evidence for mediation is provided by either a main effect for the mediator on the outcome in the presence of the main effect for the intervention (β path in Figure 2) or an interaction between the mediator and the intervention in predicting the outcome (β′ path in Figure 2b). We included the main effect of the intervention on the outcomes (path τ) and controlled for baseline levels of the outcomes and parents’ depressive symptoms at baseline.
Table 3.
Effects of adolescents’ coping and parenting as mediators of intervention effects on adolescents’ mental health outcomes (β and β′ paths).
| Adolescent Mental Health (12-Month Follow-Up) | ||||||||
|---|---|---|---|---|---|---|---|---|
| YSR | CBCL | |||||||
| Mediators (6-Month Follow-Up) | CES-D | Anxiety-Depression | Internalizing | Externalizing | ||||
| df | F | df | F | df | F | df | F | |
| Parent-Adolescent Report of Adolescents’ Secondary Control Coping | ||||||||
| Intercept | 1, 50.5 | 3.39* | 1, 46.4 | 3.03* | 1, 47.7 | 3.39* | 1, 57 | 0.05 |
| BDI-II (covariate) | 1, 52.7 | 0.13 | 1, 43.1 | 0.66 | 1, 41.3 | 0.00 | 1, 56.9 | 0.00 |
| Baseline Symptom (covariate) | 1, 42.2 | 39.70*** | 1, 47.6 | 3.68* | 1, 45.4 | 10.30** | 1, 55.5 | 76.43*** |
| Intervention Main Effect (τ) | 1, 54 | 0.25 | 1, 37.6 | 1.26 | 1, 36.7 | 1.71 | 1, 57 | 0.34 |
| Mediator Main Effect (β) | 1, 53.2 | 2.87* | 1, 44.3 | 3.38* | 1, 42.3 | 3.54* | 1, 57 | 0.74 |
| Interaction (β′) | 1, 53 | 0.00 | 1, 43.5 | 2.08 | 1, 41.4 | 2.71 | 1, 57 | 4.03* |
| Observed Positive Parenting | ||||||||
| Intercept | 1, 30.9 | 2.16 | 1, 36.6 | 2.56 | 1, 34 | 1.96 | 1, 41.5 | 0.07 |
| BDI-II (covariate) | 1, 31.3 | 0.04 | 1, 34.5 | 0.38 | 1, 33.1 | 0.09 | 1, 32.3 | 0.12 |
| Baseline Symptom (covariate) | 1, 27.8 | 42.03*** | 1, 30.6 | 1.59 | 1, 37.8 | 4.39* | 1, 42 | 53.45*** |
| Intervention Main Effect (τ) | 1, 15.8 | 0.00 | 1, 28.9 | 0.58 | 1, 27.3 | 0.35 | 1, 38.8 | 0.22 |
| Mediator Main Effect (β) | 1, 32.9 | 7.87** | 1, 33.9 | 0.75 | 1, 34.7 | 1.92 | 1, 35.6 | 3.65* |
| Interaction (β′) | 1, 31.7 | 0.42 | 1, 31.2 | 0.82 | 1, 30.8 | 0.50 | 1, 36.3 | 0.01 |
| Observed Negative Parenting | ||||||||
| Intercept | 1, 36.5 | 2.62 | 1, 40.2 | 2.02 | 1, 40.2 | 2.62 | 1, 41.1 | 0.40 |
| BDI-II (covariate) | 1, 30.5 | 0.00 | 1, 33.4 | 0.59 | 1, 32 | 0.36 | 1, 32 | 0.66 |
| Baseline Symptom (covariate) | 1, 30.5 | 27.22*** | 1, 28.8 | 1.41 | 1, 33.9 | 3.09* | 1, 41.5 | 56.29*** |
| Intervention Main Effect (τ) | 1, 39.9 | 0.39 | 1, 29.8 | 1.16 | 1, 29.3 | 2.02 | 1, 41.2 | 2.99* |
| Mediator Main Effect (β) | 1, 35.9 | 0.04 | 1, 33.8 | 0.03 | 1, 33.8 | 0.00 | 1, 36.3 | 3.45* |
| Interaction (β′) | 1, 37.6 | 0.01 | 1, 33.1 | 0.15 | 1, 32 | 1.15 | 1, 37.7 | 2.34 |
p < .05;
p < .01,
p<.001
First, we examined the composite parent/adolescent report measure of adolescents’ use of secondary control coping. Significant effects for secondary control coping were found for the CES-D (main effect, p < .05), anxious-depressed symptoms on the YSR (main effect, p < .05), internalizing symptoms on the YSR (main effect, p < .05), and externalizing symptoms on the CBCL (interaction effect, p < .05). Second, significant effects were also found for observed positive parenting on externalizing symptoms on the CBCL (main effect, p < .05) and for the CES-D (main effect, p < .01). Although there was a significant effect for observed negative parenting on externalizing symptoms on the CBCL (main effect, p < .05), this effect did not meet the joint significance criteria, as the effect of the intervention on change in negative parenting was not significant (α path in Figure 2b). Thus, evidence for mediation based on the joint significance test was found for coping on YSR anxiety/depression and internalizing symptoms, CBCL externalizing symptoms, and the CES-D; and for positive parenting on CBCL externalizing symptoms and the CES-D (see Table 4).
Table 4.
Summary of the Joint Significance Test of mediation.
| Mediators | Significant effects of intervention on mediators (α path)? | 12-month Outcomes | Significant effects of mediators on outcomes (β and/or β′ paths)? | Criteria for joint significance met? |
|---|---|---|---|---|
| Parent-Adolescent Report of Adolescents’ Secondary Control Coping | Yes | CES-D | Yes | Yes |
| YSR Anxiety/Depression | Yes | Yes | ||
| YSR Internalizing | Yes | Yes | ||
| CBCL Externalizing | Yes | Yes | ||
| Observed Positive Parenting | Yes | CES-D | Yes | Yes |
| YSR Anxiety/Depression | No | No | ||
| YSR Internalizing | No | No | ||
| CBCL Externalizing | Yes | Yes | ||
| Observed Negative Parenting | No | CES-D | No | No |
| YSR Anxiety/Depression | No | No | ||
| YSR Internalizing | No | No | ||
| CBCL Externalizing | Yes | No |
Effect sizes were calculated as the proportion of the effect of the intervention on the outcome that is accounted for by the mediator and we also calculated the unstandardized estimates (B’s) and SE’s for the effect of the intervention on the outcomes in the absence of the mediators (τ; see Figure 2a) and for the effect of the intervention in the presence of the mediators (τ′; see Figure 2b). These effect sizes were: .47 for coping on YSR anxiety/depression (τ: B = −1.94, SE = 0.84, p = .01; τ′: B = −1.03, SE = 0.92, p = .13); .44 for coping on YSR internalizing (τ: B = −4.28, SE = 1.65, p = .01; τ′: B = −2.41, SE = 1.84, p = .10); .68 for coping on CBCL externalizing (τ: B = −2.36, SE = 1.27, p = .03; τ′: B = −.75, SE = 1.29, p = .28); .73 for coping on the CES-D (τ: B = −2.58, SE = 1.38, p = .03; τ′: B = −.69, SE = 1.37, p = .31); and .68 for positive parenting on CBCL externalizing (τ: B = −2.36, SE = 1.27, p = .03; τ′: B = −.75, SE = 1.61, p = .32). It is noteworthy that all effects for intervention on the outcomes in the absence of the mediators (τ) were significant, but were no longer significant in the presence of the mediators (τ′). The effect size for positive parenting on the CES-D was out of range (1.04) because mediator effect accounted for such a large portion of the direct effect (i.e., the mediator reduced the direct treatment effect on outcome to zero which increases the standard error of the estimate).
Supplementary analyses
Guided by the findings of Silverman et al. (2009), we examined possible reciprocal effects of changes in children’s emotional and behavioral problems on parenting behaviors. Changes in children’s symptoms on CES-D, F (1, 58.2) = 2.80, p < .05; and YSR internalizing symptoms, F (1, 59.6) = 3.14, p < .05, at 2-months predicted changes in observed negative parenting from baseline to 6-months (after completion of the booster sessions).
Discussion
The present study provides the first evidence for specific mediators of a family group cognitive behavioral preventive intervention for families of parents with a history of major depressive disorder. Significant prevention effects were reported previously for this program that involves teaching effective parenting skills to parents and secondary control coping skills to adolescents (Compas et al., 2009). Specifically, beneficial effects for the intervention as contrasted with the provision of written information about depression were found on adolescents’ depressive, anxious-depressed, internalizing, and externalizing symptoms at 12-month follow-up. Using a more restricted sample based on one child randomly selected from families with more than one child in the target age range, the findings reported here identified significant mediators for these outcomes. Further, the changes in the hypothesized mediators were assessed at 6-month follow-up and these changes were used to predict changes in adolescents internalizing and externalizing symptoms at 12-month follow-up. Thus, there was evidence that changes in the mediators preceded changes in the outcomes, a necessary component for testing mediation (Kraemer et al., 2002; MacKinnon et al., 2002). Identification of mediators of the effects of preventive interventions is an important next step for the advancement of theoretical understanding of mechanisms of risk as well as the development of efficacious interventions for at-risk youth (e.g., Kazdin, 2008; Kraemer et al., 2002; La Greca et al., 2009).
One arm of the FGCB intervention involved teaching adolescents to use the secondary control coping skills of acceptance, cognitive reappraisal, positive (but realistic) thinking, and positively distracting thoughts and activities to cope with the stress associated with their parents’ depression in their families (Compas et al., 2001; 2009). We found that, based on a composite measure of parents’ and adolescents’ reports, adolescents in the FGCB intervention showed greater increases in their use of these coping skills from baseline to 6-month follow-up than adolescents in the written information condition. Increases in the use of these coping skills significantly mediated the effects of the intervention on internalizing, anxious/depressed, and depressive symptoms as reported by adolescents and on externalizing symptoms as reported by parents at 12-months. These findings suggest that secondary control coping may serve as a significant protective factor for a wide range of symptoms of psychopathology in children of depressed parents. This is consistent with previous descriptive studies that have found secondary control coping is related to lower levels of both internalizing and externalizing symptoms in children of parents with a history of depression (e.g., Fear et al., 2009; Jaser et al., 2005).
Although various types of coping skills are taught as part of preventive interventions, changes in coping are rarely measured and coping has been tested as a mediator of prevention effects in even fewer studies. One exception is the evaluation of a preventive intervention for children who experienced the death of a parent. The significant effects of the Family Bereavement Program (Sandler et al., 2003) were mediated in part by changes in children’s coping (Tein et al., 2006). The present findings add to those reported by Tein et al. and provide the first evidence that teaching skills to at-risk adolescents to cope with living in a family with a history of parental depression can contribute to beneficial mental health effects. Further, Tein et al. found effects for coping as a mediator when it was measured concurrently with the outcome; the present study built on these findings by demonstrating evidence for changes in coping (at 6-months) as a mediator of changes in mental health outcomes at a later time point (12-months), thus providing additional and even stronger support for the role of coping as a mediator.
With regard to parenting behaviors as mediators, the current findings provide the first but limited support for changes in the parenting skills of parents with a history of depression on reducing externalizing and depressive symptoms in adolescents in these families. Positive parenting changed as a result of the intervention and was found to have significant effects on child outcomes. The FGCB intervention focuses mainly on improving positive parenting (e.g., use of praise, scheduling family pleasant activities) and the findings suggest that changes in these aspects of parenting played a more active role in contributing to benefits for children. There is a large body of evidence supporting the association of parenting behaviors with child externalizing problems (see McKee et al., 2008), and there is support for the role of parenting as a mediator of interventions for externalizing problems (e.g., Eddy & Chamberlain, 2000). Of interest, effects for parenting were found in the current study based on a direct observation measure of parents’ behavior rather than parent or child reports.
Further, guided by recent findings reported by Silverman et al. (2009), we conducted supplementary analyses to test the reverse paths from changes in children problems to changes in parenting. Consistent with effects found by Silverman et al. in the treatment of children’s anxiety symptoms, we found that changes in children’s internalizing symptoms at the completion of the acute phase of the FGCB intervention predicted changes in negative parenting behavior at the 6-month follow-up (after completion of the booster sessions). This suggests that the dynamics of change may move from children to parents as well as from parents to children. For example, changes in children’s behavior may have made it more feasible for parents in the FGCB intervention to learn new parenting skills. These effects warrant continued attention in future research.
Overall, findings from the current study indicate that child coping and to a lesser extent parenting mediated intervention effects for internalizing and externalizing problems. The identification of both coping and parenting as mediators of child internalizing and externalizing problems indicates that these variables are active ingredients in the preventive intervention and should be measured and perhaps enhanced in future iterations of the current program.
There are several limitations in the current study that can be addressed in future research. First, the effects of the intervention were examined at 12-months. It will be important to examine longer-term effects of the intervention and for the role of coping and parenting be examined as mediators of these later outcomes. Second, the current study represents an efficacy trial, in which the delivery of the intervention occurred under tightly controlled conditions (e.g., in university psychology departments, use of highly trained therapists, frequent supervision, careful monitoring of treatment fidelity, strong emphasis on participant retention efforts). It is critical that future iterations of this intervention are conducted to examine its effectiveness under less controlled and more naturalistic conditions. Third, the current sample was somewhat limited in diversity and the efficacy of this intervention needs to be examined in more racially and ethnically diverse sample. Fourth, the role of parental depression status and depressive symptoms warrants continued attention in future research as a potential moderator of the effects of preventive intervention with families of depressed parents (Garber et al., 2009). Finally, comparison of the FGCB intervention to a no-intervention control condition and comparison to components of the overall intervention (e.g., a parent only intervention, an adolescent only intervention) is needed to further understand the active elements of this intervention.
These limitations notwithstanding, the current findings provide the first known evidence regarding mediators of the effects of preventive interventions for offspring of depressed parents. Further, this study provides evidence for the role of changes in coping skills as a mediator of a preventive intervention for at-risk adolescents and extends the role of positive parenting as a mediator of change in internalizing and externalizing problems to families where a parent has a history of depression. Finally, given the shortage of component analyses presented in the intervention research literature, our findings provide promising support for uncovering critical components that address how to reduce effects of the intergenerational transmission of psychopathology in children of depressed parents.
Footnotes
This proportion is not equivalent to an ordinary R2. Rather, these estimates reflect the proportion of the main effect of the intervention on the outcomes (d’s ranging from .36 to .55) accounted for by the mediator.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Bruce E. Compas, Vanderbilt University
Jennifer E. Champion, Vanderbilt University
Rex Forehand, University of Vermont.
David A. Cole, Vanderbilt University
Kristen L. Reeslund, Vanderbilt University
Jessica Fear, Vanderbilt University.
Emily J. Hardcastle, Vanderbilt University
Gary Keller, University of Vermont.
Aaron Rakow, University of Vermont.
Emily Garai, University of Vermont.
Mary Jane Merchant, University of Vermont.
Lorinda Roberts, University of Vermont.
References
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Alderfer MA, Fiese BH, Gold JI, Cutuli JJ, Holmbeck GN, Goldbeck L, Chambers CT, Abad M, Spetter D, Patterson J. Evidence-based assessment in pediatric psychology: Family measures. Journal of Pediatric Psychology. 2008;33:1046–61. doi: 10.1093/jpepsy/jsm083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer DJ, Sterba SK, Halfors DD. Evaluating group-based interventions when control participants are ungrouped. Multivariate Behavioral Research. 2008;43:210–236. doi: 10.1080/00273170802034810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Wright BJ, Gladstone TRG, Forbes P. Long-term effects from a randomized trial of two public health preventive interventions for parental depression. Journal of Family Psychology. 2007;21:702–713. doi: 10.1037/0893-3200.21.4.703. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories 1A and II in psychiatric outpatients. Journal of Personality Assessment. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Beardslee W, et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Archives of General Psychiatry. 2001;58:1127–1134. doi: 10.1001/archpsyc.58.12.1127. [DOI] [PubMed] [Google Scholar]
- Compas BE, Forehand R, Keller G, Champion A, Reeslund KL, McKee L, et al. Randomized clinical trial of a family cognitive-behavioral preventive intervention for children of depressed parents. Journal of Consulting and Clinical Psychology. 2009;77:1007–1020. doi: 10.1037/a0016930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Langrock AM, Keller G, Merchant MJ, Copeland ME. Children coping with parental depression: Processes of adaptation to family stress. In: Goodman S, Gotlib I, editors. Children of depressed parents: Alternative pathways to risk for psychopathology. Washington, DC: American Psychological Association; 2001. [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary responses to stress. Journal of Consulting and Clinical Psychology. 2000;68:976–992. [PubMed] [Google Scholar]
- Eddy JM, Chamberlain P. Family management and deviant peer association as mediators of the impact of treatment condition on youth antisocial behavior. Journal of Consulting and Clinical Psychology. 2000;68:857–863. doi: 10.1037/0022-006X.68.5.857. [DOI] [PubMed] [Google Scholar]
- England MJ, Sim LJ, editors. Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- Fairchild AJ, MacKinnon DP, Taborga MP, Taylor AB. R2 effect-size measures for mediation analyses. Behavior Research Methods. 2009;41:486–498. doi: 10.3758/BRM.41.2.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fear JM, Champion JE, Reeslund KL, Forehand R, Colletti C, Roberts L, Compas BE. Parental depression and interparental conflict: Children and adolescents’ self-blame and coping responses. Journal of Family Psychology. 2009;23:762–766. doi: 10.1037/a0016381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fendrich M, Weissman MM, Warner V, Mufson L. Two-year recall of lifetime diagnoses in offspring at high and low risk for major depression: The stability of offspring reports. Archives of General Psychiatry. 1990;47:1121–1127. doi: 10.1001/archpsyc.1990.01810240041008. [DOI] [PubMed] [Google Scholar]
- Fitzmaurice G, Davidian M, Verbeke G, Molenberghs G. Longitudinal data analysis. Chapman and Hall; 2009. [Google Scholar]
- Fitzmaurice G, Laird N, Ware J. Applied longitudinal data analysis. Wiley; 2004. [Google Scholar]
- Foster CE, Webster MC, Weissman MM, Pilowsky DJ, Wickramarante PJ, Talati A, et al. Remission of maternal depression: Relations to family functioning and youth internalizing and externalizing symptoms. Journal of Clinical Child and Adolescent Psychology. 2008;37:714–724. doi: 10.1080/15374410802359726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber J, Clarke GN, Weersing VR, Beardslee WR, Brent DA, Gladstone TRG, et al. Prevention of depression in at-risk adolescents: A randomized controlled trial. Journal of the American Medical Association. 2009;301:2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH. Depression in mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Shih JH. Family discord and stress predictors of depression and other disorders in adolescent children of depressed and nondepressed women. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:994–1002. doi: 10.1097/01.chi.0000127588.57468.f6. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Wells KC, Kraemer HC, Abikoff HB, Arnold LE, et al. Family processes and treatment outcome in the MTA: Negative/Ineffective parenting practices in relation to multimodal treatment. Journal of Abnormal Child Psychology. 2000;28:555–568. doi: 10.1023/a:1005183115230. [DOI] [PubMed] [Google Scholar]
- Jaser SS, Champion JE, Reeslund K, Keller G, Merchant MJ, Benson M, Compas BE. Cross-situational coping with peer and family stressors in adolescent offspring of depressed parents. Journal of Adolescence. 2007;30:917–932. doi: 10.1016/j.adolescence.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Jaser SS, Fear JM, Reeslund KL, Champion JE, Reising MM, Compas BE. Maternal sadness and adolescents’ responses to stress in offspring of mothers with and without a history of depression. Journal of Clinical Child and Adolescent Psychology. 2008;37:736–746. doi: 10.1080/15374410802359742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser SS, Langrock AM, Keller G, Merchant MJ, Benson M, Reeslund K, Champion JE, Compas BE. Coping with the stress of parental depression II: Adolescent and parent reports of coping and adjustment. Journal of Clinical Child and Adolescent Psychology. 2005;34:193–205. doi: 10.1207/s15374424jccp3401_18. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Evidence-based treatment and practice: New opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. American Psychologist. 2008;63:146–159. doi: 10.1037/0003-066X.63.3.146. [DOI] [PubMed] [Google Scholar]
- Kenward MG, Rogers JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53:983–997. [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27:101–108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Lochman JE. Moving beyond efficacy and effectiveness in child and adolescent intervention research. Journal of Consulting and Clinical Psychology. 2009;77:373–382. doi: 10.1037/a0015954. [DOI] [PubMed] [Google Scholar]
- Langrock AM, Compas BE, Keller G, Merchant MJ, Copeland ME. Coping with the stress of parental depression: Parents’ reports of children’s coping and emotional/behavioral problems. Journal of Clinical Child and Adolescent Psychology. 2002;31:312–324. doi: 10.1207/S15374424JCCP3103_03. [DOI] [PubMed] [Google Scholar]
- Lim J, Wood BL, Miller BD. Maternal depression and parenting in relation to child internalizing symptoms and asthma disease activity. Journal of Family Psychology. 2008;22:264–273. doi: 10.1037/0893-3200.22.2.264. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee L, Colletti CJM, Rakow A, Jones DJ, Forehand R. Parenting and child externalizing behaviors: Are the associations specific or diffuse? Aggression and Violent Behavior. 2008;13:201–215. doi: 10.1016/j.avb.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melby JN, Conger RD. The Iowa Family Interaction Rating Scales: Instrument summary. In: Kerig PK, Lindahl KM, editors. Family observational coding systems: Resources for systemic research. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2001. pp. 33–58. [Google Scholar]
- Melby JN, Conger RD, Book R, Rueter M, Lucy L, Repinski D, Rogers S, Rogers B, Scaramella L. Unpublished manuscript. 5. Institute for Social and Behavioral Research, Iowa State University; Ames, Iowa: 1998. The Iowa Family Interaction Rating Scales. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the Center for Epidemiologic Studies Depression Scale. Psycholoical Assessment. 1990;2:122–128. [Google Scholar]
- Sandler IN, Ayers TS, Wolchik SA, Tein J, Kwok O, Haine RA, et al. The Family Bereavement Program: Efficacy evaluation of a theory-based prevention program for parentally bereaved children and adolescents. Journal of Consulting and Clinical Psychology. 2003;71:587–600. doi: 10.1037/0022-006x.71.3.587. [DOI] [PubMed] [Google Scholar]
- Schaalje GB, McBride JB, Fellingham GW. Adequacy of approximations to distributions of test statistics in complex linear models. Journal of Agricultural, Biological, and Environmental Statistics. 2002;7:512–524. [Google Scholar]
- Seifer R, Dickstein S, Sameroff AJ, Magee KD, Hayden LC. Infant mental health and variability of parental depressive symptoms. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:1375–1382. doi: 10.1097/00004583-200112000-00007. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Kurtines WM, Jaccard J, Pina AA. Directionality of change in youth anxiety treatment involving parents: An initial examination. Journal of Consulting and Clinical Psychology. 2009;77:474–485. doi: 10.1037/a0015761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steer RA, Brown GK, Beck AT, Sanderson WC. Mean Beck Depression Inventory-II scores by severity of major depressive disorder. Psychological Reports. 2001;88:1075–1076. doi: 10.2466/pr0.2001.88.3c.1075. [DOI] [PubMed] [Google Scholar]
- Tein J, Sandler IN, Ayers TS, Wolchik SA. Mediation of the effects of the Family Bereavement Program on mental health problems of bereaved children and adolescents. Prevention Science. 2006;7:179–195. doi: 10.1007/s11121-006-0037-2. [DOI] [PubMed] [Google Scholar]
- Tein J, Sandler IN, MacKinnon DP, Wolchik SA. How did it work? Who did it work for? Mediation in the context of a moderated prevention effect for children of divorce. Journal of Consulting and Clinical Psychology. 2004;72:617–624. doi: 10.1037/0022-006X.72.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaliano PP, Maiuro RD, Russo J, Becker J. Raw versus relative scores in the assessment of coping strategies. Journal of Behavioral Medicine. 1987;10:1–18. doi: 10.1007/BF00845124. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remissions in maternal depression and child psychopathology: A STAR*D-child report. Journal of the American Medical Association. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Wolchik SA, West SG, Sandler IN, Tein JY, Coatsworth D, Lengua L, Weiss L, Anderson ER, Greene SM, Griffin WA. An experimental evaluation of theory-based mother and mother-child programs for children of divorce. Journal of Consulting and Clinical Psychology. 2000;68:843–856. [PubMed] [Google Scholar]
- Zhou Q, Sandler IN, Millsap RE, Wolchik SA, Dawson-McClure SR. Mother-child relationship quality and effective discipline as mediators of the 6-year effects of the New Beginnings Program for children of divorced families. Journal of Consulting and Clinical Psychology. 2008;76:579–594. doi: 10.1037/0022-006X.76.4.579. [DOI] [PMC free article] [PubMed] [Google Scholar]