Abstract
A 54-year-old woman started to loose vision two days prior to admission and also experienced left-sided headache, nausea, emesis and disorientation. Magnetic resonance imaging (MRI) revealed bilateral posterior cerebral artery and cerebellar infarctions. Transcranial power motion Doppler (PMD-TCD) showed blunted flow signal in the proximal basilar artery (BA) suggestive for a high grade stenosis also seen on MR-angiography. Dual antiplatelet therapy with aspirin and clopidogrel was started. Catheter angiography confirmed the proximal high grade BA stenosis. After angiography the patient experienced hypertensive crisis with severe headache. Blood pressure was lowered and headache resolved. One hour later she developed fluctuating level of consciousness and motor symptoms. PMD-TCD findings were suggestive for an intraluminal thrombus that moved from the proximal to the distal basilar artery presumably further contributing to brain stem hypoperfusion and neurological deterioration. To achieve a compromise between lower blood pressure and maintenance of brain perfusion, hypervolemic hemodilution with intravenous dextran-40 was initiated. Patient’s symptoms resolved to baseline and MRI showed no new parenchymal lesions.
Introduction
In acute ischemic stroke, the presence of an intraluminal thrombus with or without underlying atheroma carries a high risk for recurrent artery-to-artery embolization.1–3 The best treatment regimen for early secondary prevention in these patients has not yet been defined.1 This particularly applies to patients with recurrent symptoms and reocclusions, who are refractory to standard medical therapy including antiplatelet and anticoagulation agents.
In patients undergoing carotid endarterectomy (CEA), additional intravenous therapy with dextran-40, a high-molecular weight polysaccharide, was safe and resulted in a reduced rate of postoperative microembolization.4, 5
We report a patient with a symptomatic basilar artery stenosis, thrombo-embolism, hyperemic reperfusion and re-occlusion who responded to an additional treatment with dextran-40.
Case Report
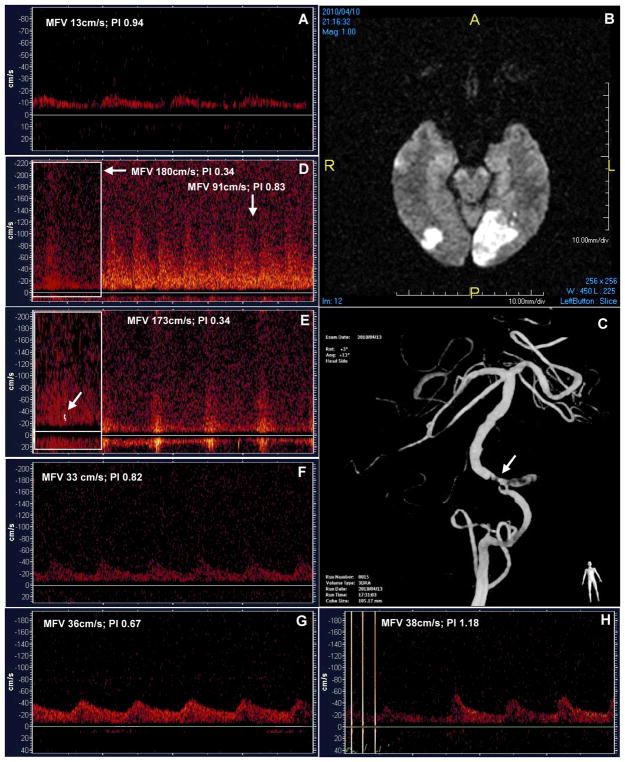
A 54-year-old African-American female with a history of arterial hypertension, breast cancer, and transient ischemic attack presented to the emergency department with new onset loss of vision, left-sided headache, nausea, emesis and disorientation that started two days ago. Her admission neurological examination showed residual light perception, bilateral horizontal nystagmus, and no motor weakness (National Institutes of Health Stroke Scale [NIHSS] score 4). PMD-TCD showed a blunted flow signal (Thrombolysis in Brain Ischemia [TIBI] score 2) in the proximal basilar artery (BA) compatible with a flow-limiting BA stenosis (figure). MR-angiography also showed a significant stenosis in the proximal BA. MRI revealed bilateral infarctions in occipital lobes and cerebellum (figure). The patient received aspirin 325 mg and clopidogrel 300 mg load followed by aspirin 325 mg and clopidogrel 75 mg daily. Her symptoms improved over 3 days with return of object recognition while vision field loss became limited to a right-sided homonymous hemianopsia (NIHSS 2). Catheter angiography (DSA) 3 days after admission showed a severe and irregular-surface proximal BA stenosis originating from the terminal right vertebral artery (figure).
Figure 1.
(A) Baseline TCD: delayed systolic flow acceleration (TIBI 2) at a depth of 81 mm, indicating high-grade proximal BA stenosis. (B) MRI: diffusion restriction in both PCAs (left>right). (C) Catheter angiography: 3-D reconstruction of a severe irregular-surface proximal BA stenosis (arrow). (D) TCD: improved mean flow velocity in the proximal BA at 80 mm (insert on the left) and possible hyperemic reperfusion of the distal BA at 99 mm. (E) high velocity turbulent flow and micro-emboli (insert on the left) in the mid-BA at 92 mm. (F) decreased flow velocity with delayed systolic flow acceleration in the mid-BA at 87 mm. (G–H) blunted flow signals at the proximal and mid-BA segments 24 hrs after administration of dextran-40.
One hour after DSA, the patient experienced severe (10/10) headache, her systolic blood pressure was found to be 240 mmHg, however she had no new focal deficits. At this point, PMD-TCD showed improved mean flow velocity (TIBI 4, MFV 180 cm/s) in the proximal BA indicating recanalization and possible hyperemic reperfusion of the distal vasculature (distal BA MFV 91 cm/s, figure). Headache resolved with systolic blood pressure lowering to 175 mmHg with nicardipine.
One hour later the patient developed vertigo and left-sided ataxia. She started to fluctuate with NIHSS changing from 2 to 6 points followed by an episode of unresponsiveness. Her blood pressure was 170 mmHg. Stat non-contrast CT showed no intracerebral hemorrhage. PMD-TCD showed embolic signals in the proximal BA with a high velocity jet in the middle BA (TIBI 4, MFV 173 cm/s), suggestive for artery-to-artery embolization and thrombus movement along BA stem (figure).
We initiated intravenous dextran-40 infusion (20ml/h over 24 hours). During the next hour, flow velocities through the proximal and mid-BA decreased to 33–46 cm/s with delayed systolic flow acceleration and no micro-embolic signals (figure). Patient’s symptoms resolved back to the NIHSS score of 2 with no subsequent fluctuation. At 24-hours, PMD-TCD showed blunted flow signals with low (36–39 cm/s) velocities throughout the basilar artery and positive diastolic flow (figure) while MRI/MRA showed no new parenchymal lesions and persistence of the proximal BA stenosis. The patient experienced no possible side-effects during or after the dextran-40 infusion. At the time of discharge, the patient’s only deficit was a right-sided homonymous hemianopsia. Two months later, at an outpatient visit she had no neurological deficit and was functionally independent without any assistance (NIHSS 0, modified Rankin Scale 0).
Discussion
Our case highlights a dilemma how to manage patients with persisting arterial stenoses, artery-to-artery embolization and re-occlusion particularly in the setting of evolving or subacute infarction. Our patient experienced these events while already receiving dual anti-platelets. Further problem was related as how to manage her blood pressure. Severe headache (and likely underlying hyperperfusion mechanism with excessively high blood pressure) required blood pressure lowering while persisting high grade BA stenosis and thrombus moving through BA stem prompted us not to lower it too low. Hypothetically, to achieve a compromise between lower blood pressure and maintenance of brain perfusion, volume expansion could be an option. The high-molecular weight polysaccharide dextran-40 provides volume expansion and it also has mild anti-thrombotic properties.4, 5 It has been safely applied in patients with extracranial atherosclerotic disease undergoing CEA effectively reducing postoperative Doppler-detectable microembolization due to its antithrombotic and antiplatelet effect.4–6
In this case report, dextran-40 was administered to a patient with fluctuating symptoms due to an unstable BA intraluminal thrombus despite combined aspirin and clopidogrel therapy. We also illustrate the possible extension of the intraluminal thrombus from proximal to middle-distal BA using PMD-TCD which allows a reliable and quick detection of flow abnormalities in hemodynamically significant BA stenoses.7, 8 This thrombus extension may have contributed to worsening brainstem hypoperfusion and neurological fluctuations. Interestingly, early trials of hemodilution therapy9, 10 included consecutive stroke patients, and as such may have been negative due in part to selection bias. Our experience suggests that the use of intravenous dextran-40 could be considered in treating patients with hemodynamically significant intracranial stenotic lesions detectable by PMD-TCD who do not respond to standard antithrombotic therapies.
Footnotes
Disclosures
Dr. Palazzo has no disclosures. Dr. Barlinn has no disclosures. Dr. Balucani has no disclosures. Dr. Zhao has no disclosures. Dr. Prestley has no disclosures. Dr. Alexandrov and University of Alabama Hospital, Comprehensive Stroke Center are funded by the National Institute of Neurological Disorders and Stroke (NINDS)/University of Texas-Houston Medical School to conduct studies on experimental combinatory therapies (SPOTRIAS Program).
References
- 1.Bhatti AF, Leon LR, Jr, Labropoulos N, et al. Free-floating thrombus of the carotid artery: literature review and case reports. J Vasc Surg. 2007 Jan;45(1):199–205. doi: 10.1016/j.jvs.2006.09.057. [DOI] [PubMed] [Google Scholar]
- 2.Markus HS, MacKinnon A. Asymptomatic embolization detected by Doppler ultrasound predicts stroke risk in symptomatic carotid artery stenosis. Stroke. 2005 May;36(5):971–5. doi: 10.1161/01.STR.0000162717.62684.40. Epub 2005 Apr 7. [DOI] [PubMed] [Google Scholar]
- 3.Ritter MA, Dittrich R, Thoenissen N, et al. Prevalence and prognostic impact of microembolic signals in arterial sources of embolism. A systematic review of the literature. J Neurol. 2008 Jul;255(7):953–61. doi: 10.1007/s00415-008-0638-8. [DOI] [PubMed] [Google Scholar]
- 4.Abir F, Barkhordarian S, Sumpio BE. Efficacy of dextran solutions in vascular surgery. Vasc Endovascular Surg. 2004 Nov–Dec;38(6):483–91. doi: 10.1177/153857440403800601. [DOI] [PubMed] [Google Scholar]
- 5.Jones CI, Payne DA, Hayes PD, et al. The antithrombotic effect of dextran-40 in man is due to enhanced fibrinolysis in vivo. J Vasc Surg. 2008 Sep;48(3):715–22. doi: 10.1016/j.jvs.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Lennard NS, Vijayasekar C, Tiivas C, et al. Control of emboli in patients with recurrent or crescendo transient ischaemic attacks using preoperative transcranial Doppler-directed Dextran therapy. Br J Surg. 2003 Feb;90(2):166–70. doi: 10.1002/bjs.4030. [DOI] [PubMed] [Google Scholar]
- 7.Ribo M, Garami Z, Uchino K, et al. Detection of reversed basilar flow with power–motion Doppler after acute occlusion predicts favorable outcome. Stroke. 2004 Jan;35(1):79–82. doi: 10.1161/01.STR.0000106760.25228.2C. [DOI] [PubMed] [Google Scholar]
- 8.Tsivgoulis G, Sharma VK, Hoover SL, et al. Applications and advantages of power motion-mode Doppler in acute posterior circulation cerebral ischemia. Stroke. 2008 Apr;39(4):1197–204. doi: 10.1161/STROKEAHA.107.499392. [DOI] [PubMed] [Google Scholar]
- 9.Aichner FT, Fazekas F, Brainin M, et al. Hypervolemic hemodilution in acute ischemic stroke: the multicenter austrian hemodilution stroke trial (MAHST) Stroke. 1998;29:743–749. doi: 10.1161/01.str.29.4.743. [DOI] [PubMed] [Google Scholar]
- 10.Asplund K. Haemodilution for acute ischaemic stroke. Cochrane Database Syst Rev. 2002;(4):CD000103. doi: 10.1002/14651858.CD000103. [DOI] [PubMed] [Google Scholar]