Abstract
A developmental cascade model tested associations among child maltreatment, internalizing and externalizing psychopathology, social competence, and cannabis abuse and dependence symptoms in a longitudinal cohort (N = 415). Nested structural equation models evaluated continuity and cross-domain influences among broad multi-informant constructs across four developmental periods: age 7 to 9, 10 to 12, 13 to 15, and 15 to 18. Results indicated significant paths from child maltreatment to early externalizing and internalizing problems and social competence, as well as to cannabis abuse and dependence (CAD) symptoms in adolescence. Youth CAD symptoms were primarily related directly to child maltreatment and externalizing problems. Childhood internalizing symptoms contributed to later childhood decreases in social competence, which predicted increases in late adolescent externalizing problems. Using a developmental psychopathology framework, results are discussed in relation to cascade and transactional effects and the interplay between problem behaviors during childhood and development of CAD symptoms during early and late adolescence.
Alcohol and substance use disorders are being increasingly conceptualized as developmental phenomena (Brown et al., 2009; Chassin, Hussong, & Beltran, 2009; Glantz & Leshner, 2000; Masten, Faden, Zucker, & Spear, 2009; Tarter, 2002; Windle et al., 2009; Zucker, 2006) with calls for more in-depth investigation into the developmental processes that contribute to these psychopathological outcomes. Moreover, as discussed below, child maltreatment has been frequently identified in the life histories of adolescents and adults in treatment for substance use disorders, as well as in epidemiological studies of risk factors for substance use and abuse. However, limited research has charted the unfolding developmental progression of maltreated children from the early years to demonstrate the emergence of substance use problems. To advance understanding in this area, the current investigation utilizes a developmental cascade conceptualization to model developmental processes that contribute to the emergence of adolescent marijuana abuse and dependence symptomatology in maltreated and nonmaltreated youth.
Child Maltreatment
For nearly 20 years, a transactional–ecological conceptualization of development in maltreated children has been promoted (Cicchetti & Lynch, 1993; Cicchetti & Valentino, 2006).Within this model the organizational structure of development is articulated, whereby competencies and liabilities attained at successive stages of development are hierarchically integrated within and among developmental systems to influence subsequent development. Child maltreatment has been regarded as a severe, fundamental failure of the caregiving system to provide essential experience-expectant nutriments for optimal psychological development (Cicchetti & Lynch, 1995). As a consequence, across the course of early ontogenesis, maltreated children have been shown to evince compromised developmental competencies on important developmental tasks, including emotion regulation, attachment organization, autonomous self development, representational development, peer relationship functioning, adaptation to school, adolescent autonomy, romantic relationships, and identity formation (Cicchetti & Rogosch, 2002; Cicchetti & Valentino, 2006; Masten & Coatsworth, 1998). Given the probability of accumulating compromises in early development, maltreated children are vulnerable to the emergence of behavioral maladaptation and psychopathology during childhood and across the life course. A wide range of psychopathological disorders have been shown to be potential sequelae of child abuse and neglect including conduct disorder, antisocial personality disorder, and disruptive behavior disorders, known more broadly as internalizing disorders including depression, anxiety diagnoses, and post-traumatic stress disorder, as well as personality dysfunction (Jaffee et al., 2005; Kaplow & Widom, 2007; Widom, DuMont, & Czaja, 2007).
In addition to a broad spectrum of externalizing and internalizing psychopathology among maltreated children, during adolescence and adulthood ample evidence exists for higher rates of substance abuse and dependence among maltreated individuals. In clinical samples undergoing treatment for substance use disorders, between one third and two thirds evince child abuse and neglect histories (Bayatour,Wells,& Holford, 1992; Cavaiola & Schiff, 1989; Dembo, Dertke, Borders, Washburn, & Schmeidler, 1988; Edwall, Hoffman, & Harrison, 1989; Pribor & DiWiddie, 1992; Schaefer, Sobieragi, & Hollyfield, 1988). In a survey of over 100,000 youth in 6th though 12th grade, Harrison, Fulkerson, and Beebe (1997) found that those reporting either physical or sexual abuse in childhood were from 2 to 4 times more likely to be using drugs than those not reporting abuse; the rates were even higher for youth reporting multiple forms of child maltreatment. Similar findings have been reported by Rodgers et al. (2004) and Moran, Vuchinich, and Hall (2004). Among youth with Child Protective Services documented maltreatment, Kelly, Thornberry, and Smith (1999) reported one-third higher risk for drug use among those with an abuse history. In a large epidemiological study, Fergusson, Boden, and Horwood (2008) have shown physical abuse and particularly sexual abuse to be related to illicit drug use, as well as abuse and dependence. Widom and colleagues have tracked a Child Protective Services identified sample into middle adulthood and have demonstrated ongoing linkages between child maltreatment and drug use problems, particularly among women (Widom, Marmorstein, & White, 2006; Wilson & Widom, 2009). Thus, a preponderance of evidence supports the linkage between experiences of child maltreatment and the development of adverse substance abuse outcomes among youth and adults.
Risk Factors for Substance Use and Abuse
In Hawkins, Catalano, and Miller’s (1992) seminal paper, a broad range of risk factors for adolescent substance abuse was identified. Among the risk factors emphasized by Hawkins and his colleagues, many are likely to be particularly salient in the lives of maltreated youth. For example, in terms of identified contextual factors, extreme economic deprivation characterizes many maltreating families who are residing in impoverished areas with substantial neighborhood disorganization and ample availability of drugs in the community. Individual and interpersonal risk factors also are prominent among maltreated children. Hawkins et al. highlighted poor and inconsistent family management practices, high family conflict, and poor bonding to family as risks for adolescent substance abuse, and these factors also are characteristic of the dysfunction in maltreating families in which abuse and neglect occur. Early and persistent problem behaviors, particularly antisocial and aggressive behavior, were noted, as well as peer rejection in the early elementary grades, academic failure, and low degree of commitment to school. These features are consistent with the progression of developmental failures exhibited by maltreated children (Cicchetti & Valentino, 2006). Consequently, compromised adaptation in the social and academic arena contributes to association with deviant peers, who escalate the access to and modeling of substance abuse, contributing to early onset of drug use. Accordingly, children in maltreating families are exposed to a progression of risk factors related to adolescent substance involvement, thereby heightening their vulnerability for substance abuse outcomes.
Among the prominent risk factors for alcohol and drug abuse in adolescence, co-occurring psychopathology has received particular attention (Cicchetti & Luthar, 1999; Cicchetti & Rogosch, 1999; Oshri, Tubman, Wagner, Leon-Morris, & Snyders, 2008; Weinberg, Radhert, Colliver, & Glantz, 1999). Disruptive behavior problems, including conduct disorder and oppositional defiant disorder, are routinely identified as major contributors to adolescent substance use. Costello (2007) provided an overview of several large-scale epidemiological studies examining linkages of various forms of psychopathology to substance abuse and dependence in adolescence and early adulthood, and concluded that a wealth of prospective data demonstrates that conduct problems precede drug use and abuse. In particular, Fergusson, Horwood, and Ritter (2007) demonstrated that conduct problems at age 7 to 9 predict cannabis and other illicit drug use and abuse at ages 18, 21, and 25. It is interesting that the influence of attention problems disappeared when comorbid conduct problems were controlled.
Internalizing problems, including major depression, bipolar disorder, and panic disorder, have been shown to predict cannabis use and cannabis use disorder as adolescents progress into adulthood (Wittchen et al., 2007), although some of these relations were attenuated when co-occurring externalizing problem were controlled. In general, there is epidemiological support for the role of internalizing psychopathology in predicting adolescent substance use and abuse, yet the strength of these relations is less robust when comorbid disruptive disorders are considered (Costello, 2007). Thus, for maltreated children who are at substantial risk for the development of early externalizing and internalizing psychopathology, the developmental course poses vulnerability for engaging in substance use and developing substance abuse problems.
Developmental Cascade Models of Adolescent Substance Use
Given evidence for early behavior problems to presage the emergence of later substance use and abuse in adolescence, developmental models of this progression represent an advance for understanding the early roots of substance abuse risk and their unfolding over ontogenesis. Recent work has begun to model these processes within a developmental cascades framework. Rather than relying on an ascertainment of the extent to which multiple risk factors aggregate to probabilistically predict substance use problems, these models strive to demonstrate a developmental sequence of risk processes, whereby early risk factors generate subsequent vulnerabilities in development, which in turn transact to produce further risk for competent adaptation. Such cascade models are consistent with the transactional–ecological formulation of the sequelae of maltreatment (Cicchetti & Lynch, 1993; Cicchetti & Valentino, 2006).
Consistent with Zucker’s (2006) developmental–biopsychosocial systems formulation of alcoholism, an important empirical demonstration of a cascade model has charted a developmental sequence from family risk because of paternal alcoholism, to early childhood difficult temperamental traits (i.e., negative emotionality, reactive control, low ego resiliency), to the emergence of childhood attention problems and subsequent disruptive behavior problems, to ensuing substance abuse in adolescence (Martel et al., 2009). Support was obtained for this model, illustrating the influence of compromises in one domain unfolding to difficulties in subsequent areas of behavioral control and regulation. Of note, early risk processes coalesced to promote conduct disturbance as an important link in the cascade to adolescent substance problems.
Dodge and colleagues (2009) have also evaluated a developmental cascade model of adolescent substance use onset based on a social learning theory formulation. This model originates with problems in early parenting that are promoted by adverse sociocultural contexts and difficult child characteristics that present challenges to parenting. Through these difficulties in early parenting, early behavior problems emerge. As children develop relationships with peers, their behavior problems lead to peer rejection, which further escalates their conduct problems. In turn, parenting these children is progressively more challenging, and parents have difficulty monitoring their child’s interactions with peers, who increasingly are more deviant, given the larger peer group social rejection they experience. Consequently, deviant peer models provide exposure to substances, and the vulnerable child is initiated into substance involvement.
The Martel et al. (2009) and the Dodge et al. (2009) cascade models both provide poignant illustrations of the unfolding progression of risks that transact over development to promote substance use involvement. One limitation with these models is the focus on one risk process at a time at successive stages of development. In contrast, as is central to a transactional–organizational model of development, in ontogenesis emergent domains remain important subsequently across the life course and their current status at successive stages of development must be considered (Cicchetti & Schneider-Rosen, 1986).
A somewhat different model of developmental cascades has been put forth by Masten and colleagues (Burt, Obradovic, Long, & Masten, 2008; Burt & Roisman, 2010; Masten et al., 2005). This conceptualization stresses the importance of evaluating, whenever feasible, all of the developmental constructs successively at each time period in the developmental cascade model. There has been particular interest within these models in examining the transactions between different forms of psychopathology (internalizing, externalizing) and competence (social, academic) across different developmental periods. By addressing both the continuity across development within domains as well as the within time period covariance among domains, stronger conclusions can be made about cross-domain influences contributing to change as development proceeds. Through this approach (Burt et al., 2008; Burt & Roisman, 2010;Masten et al., 2005), the cascade models have been able to demonstrate how internalizing problems can suppress the later development of externalizing problems, how childhood externalizing problems contribute negatively to academic competence in adolescence, and how social and academic competence in emerging adulthood contribute to lower internalizing problems in young adulthood.
In the current investigation, we utilize the strategy of Masten and colleagues to evaluate a developmental cascades model of the emergence of cannabis abuse and dependence (CAD) in adolescents who experienced child abuse and neglect earlier in development. Because we are contrasting the development of maltreated and nonmaltreated children, our models differ from those of Masten in that we have a primary exogenous variable of interest, and we seek to determine how child maltreatment influences the development of externalizing and internalizing psychopathology, as well as social competence, from childhood to late adolescence. Moreover, because we are interested in the development of CAD, our model includes this emergent adolescent outcome only during adolescence, given the virtually nonexistent use of marijuana during childhood (cf. Masten, Desjardins, McCormick, Kuo, & Long, 2010).
To evaluate a developmental cascade model linking child maltreatment to later adolescent psychopathology and cannabis abuse/dependence symptoms, we tested a series of nested longitudinal models, progressively evaluating within domain stability across time, the influence of maltreatment status, and cross-lag effects whereby one domain contributes to subsequent change in another domain. Constructs were assessed by multiple informants and measures, and the methodology allowed for examination of long-term longitudinal cross-domain paths while controlling for both cross-domain within-time associations and rank-order stability of each domain over time (Cole & Maxwell, 2003). Consequently, we advanced the following hypotheses in evaluating our cascade conceptualization:
We expected to observe continuity in the rank order stability of internalizing and externalizing symptomatology from the early school-age years to late adolescence; stability in social competence across the school-age years also was hypothesized.
Maltreatment occurring prior to the early school-age years was hypothesized to predict emergent internalizing and externalizing symptomatology during childhood, as well as deficiencies in social competence.
We also expected that child maltreatment experiences would predict early adolescent substance use problems, specifically CAD symptoms.
During childhood, cross-lagged relations from the early- to later school-aged years were examined. As observed by Masten et al. (2005), we anticipated that early internalizing problems would inhibit subsequent increases in externalizing problems in late childhood and decrease social competence. Early externalizing problems also were expected to contribute to decrements in later childhood social competence.
Consistent with prior research, we expected that late childhood externalizing problems and poor social competence would contribute to CAD symptoms in early adolescence. We also expected that late childhood difficulties in social competence would contribute to increases in externalizing and internalizing symptomatology during adolescence.
Finally, we hypothesized that the extent to which early adolescents were immersed in problematic cannabis use would contribute to increases in internalizing and externalizing problems in late adolescence, in addition to the continuity of these problems over development.
Method
Participants
The participants in this longitudinal investigation included 415 children whowere assessed across four waves of data collection, including ages 7 to 9, 10 to 12, 13 to 15, and 15 to 18. During the first two waves of data collection, Phase 1 of the study was conducted. Children attended a summer camp research program designed for school-aged low-income children (Cicchetti & Manly, 1990), with first wave participation occurring between the ages of 7 to 9. Children were invited to participate subsequently during childhood in the second wave at ages 10 to 12. In Phase 2 of the study, participants were followed up during adolescence and invited to take part in a series of individual interviews and research assessments. These assessments occurred during Wave 3 at ages 13 to 15, and again at Wave 4, ages 15 to 18. The sample included both maltreated children (n = 259) and nonmaltreated children (n = 156). The maltreatment groups were comparable in terms of gender, with 59.8% boys in the maltreatment group and 61.5% boys in the nonmaltreatment group, χ2 (1, N = 415) = 0.12, p > .05. The groups also were equivalent in the distribution of race, χ2 (2, N = 415) = 3.30, p > .05 (55.2% of the participants were African American, 31.6% were European American, and 13.3% were other racial groups), and ethnicity, χ2 (1, N = 415) = 1.15, p > .05 (11.8% Latino). The families of the children also were comparable on demographic characteristics. The families were impoverished; however, the groups were equivalent in terms of annual family income, t (389) = .84, p.>.05, average family income (M = $15,740, SD = $8,880), and history of receipt of public assistance, χ2 (1, N = 410) = 3.51, p > .05; 95.4% of families. The marital status of the primary caregiver in the families (primarily mothers) also was comparable across maltreatment groups, χ2 (2, N = 415) = 5.95, p > .05, with 34.7% never married, 29.4% married or living with partner, and 35.4% no longer married (divorced, separated, widowed).
At each wave of assessment, parents provided informed consent for their child’s participation, as well as consent for complete access to any family records in the Department of Human Services (DHS). Maltreated children were identified by a county DHS liaison based on the presence of documented records of child abuse and/or neglect reports. Comprehensive searches of DHS records were completed, and all maltreatment information was coded utilizing operational criteria from the maltreatment nosology specified in the Maltreatment Classification System (MCS; Barnett, Manly, & Cicchetti, 1993).
The MCS utilizes DHS records detailing investigations and findings involving maltreatment in identified families over time. Rather than relying on official designations and case dispositions, the MCS codes all available information from DHS records, making independent determinations of maltreatment experiences. Based on operational criteria, the MCS designates all of the subtypes of maltreatment children have experienced (i.e., neglect, emotional maltreatment, physical abuse, sexual abuse). Coding of the DHS records was conducted by trained research assistants, doctoral students, and clinical psychologists. Adequate reliability has been obtained (weighted κs = 0.86–0.98; Manly, 2005; Manly, Kim, Rogosch, & Cicchetti, 2001). Other investigators have demonstrated that the MCS is reliable and valid in classifying maltreatment (Bolger & Patterson, 2001; English et al., 2005; Manly, Cicchetti, & Barnett, 1994; Manly et al., 2001; Stouthamer-Loeber, Loeber, Homish, & Wei, 2001). Among the maltreated children, 69.5% had experienced neglect, 54.8% had experienced emotional maltreatment, 36.3% had experienced physical abuse, and 12.7% had experienced sexual abuse. As is typical in maltreated populations (Bolger & Patterson, 2001; Manly et al., 1994, 2001), the majority of maltreated participants had experienced multiple subtypes of maltreatment. Specifically, 60.7% of the maltreated children had experienced two or more maltreatment subtypes.
Because maltreated children are predominantly from low socioeconomic status families, demographically comparable nonmaltreated children were recruited from families receiving Aid to Families with Dependent Children. DHS record searches were completed for these families to verify the absence of any record of child maltreatment. Trained research assistants also interviewed mothers of children recruited for the nonmaltreatment group to confirm a lack of DHS involvement and prior maltreatment experiences (Cicchetti, Toth, & Manly, 2003). In addition, families who had received preventive services through DHS because of concerns over risk for maltreatment also were excluded from the nonmaltreated comparison group to reduce the potential for unidentified maltreatment existing within this group.
Procedure
During Phase 1 of the study, children attended a week-long day camp program and participated in research assessments (see Cicchetti & Manly, 1990, for detailed descriptions of camp procedures). At the camp, children were assigned to groups of eight (four maltreated, four nonmaltreated) same-age and same-sex peers. Each group was led by three trained camp counselors, who were unaware of the maltreatment status of children and the hypotheses of the study. The camp lasted 7 hr/day for 5 days, providing 35 hr of interaction between children and counselors. In addition to the recreational activities, after providing assent, children participated in various research assessments. Trained research assistants, who also were unaware of research hypotheses and maltreatment status, conducted individual research sessions with children, in which questionnaires and other research measures were administered. Clinical consultation and intervention occurred if any concerns over danger to self or others emerged during research sessions. The counselors, who had been trained extensively for 2 weeks prior to the camp, also completed assessment measures on individual children, based on their 35 hr of observations and interactions with children in their respective groups.
In Phase 2 of the study during adolescence, the participants were individually interviewed in private interview rooms by trained research assistants who were unaware of the participant’s maltreatment group status and research hypotheses. The participants completed a range of assessments, including self-report measures and interviews regarding their behavioral functioning and substance use.
Measures
Phase 1
The camp context and associated measurement battery provide a multi-informant, multiperspective view of child behavioral functioning and social relations with peers. Measures include child self-report, peer evaluations, counselor observations, and counselor-report assessments of individual children.
Peer nominations
After children had interacted with each other during the week of summer camp, children evaluated the characteristics of their peers in their respective camp groups using a peer nomination method on the last day of camp (cf. Coie & Dodge, 1983). Counselors conducted the peer rating assessment with individual children. For each peer in the camp group, children were given five brief behavioral descriptors characterizing different types of social behavior and asked to select one peer from the group who best file the behavioral description, as well as select the one child who he/she liked most and liked least. The behavioral descriptors included a child who was: cooperative, a leader, shy, disruptive, and a fighter. The total number of nominations that each individual child received from peers in each category was determined, and these totals were converted to proportions of the possible nominations in each category, and these scores in each category were standardized within each year of camp. A summary peer acceptance score was calculated as the difference between scores for liked most and liked least. Scores for peer acceptance, leadership, and cooperativeness were used to assess social competence during the school age years.
Pupil Evaluation Inventory (PEI)
The PEI (Pekarik, Prinz, Liebert, Weintraub, & Neale, 1976) was completed by camp counselors for children in their respective groups at the end of each camp week. The PEI consists of 35 items assessing social behavior, yielding three homogeneous and stable factors, including likeability, aggression, and withdrawal. Similar to peer nomination procedures, counselors were asked to select no more than two children who were best characterized by each individual item. Interrater reliabilities based intraclass correlations across the years of camp ranged from .72 to .85 (M = .78) for likeability, .85 to .90 (M = .88) for aggression, and .72 to .84 (M = .78) for withdrawal.
Teacher Report Form (TRF)
Behavioral symptomatology was evaluated at the end of each week by counselors’ completion of the TRF (Achenbach, 1991a). The TRF is a widely used and validated instrument to assess behavioral disturbance from the perspective of teachers, and the measure was used in the present study, because camp counselors are able to observe similar behaviors to that of teachers. The TRF, containing 118 items rated for frequency, assesses two broadband dimensions of child symptomatology, externalizing and internalizing, as well as total behavior problems. Subscales scores are also computed for the following factors: withdrawn, somatic problems, anxiety/depression, social problems, thought problems, attention problems, delinquent behavior, and aggressive behavior. In the present study, interrater reliability for the internalizing and externalizing scales based on average intraclass correlations among pairs of raters. Across the years, reliabilities ranged from .56 to .84 (M = .68) for internalizing and from .78 to .88 (M = .83) for externalizing. The counselors’ scores for each child were averaged to obtain individual child scores for the broadband dimensions.
Phase 2
During Waves 3 and 4, two measures are of interest for the current investigation, including assessments of behavior functioning and substance use and abuse/dependence symptomatology.
Youth Self-Report (YSR)
The YSR (Achenbach, 1991c) is a self-report version of the widely used Child Behavior Checklist (Achenbach, 1991b). The questionnaire is designed for 11- to 18-year-olds to rate their own competencies and problems in a standardized format. As with the Child Behavior Checklist, the YSR yields broadband continuous dimensions of internalizing and externalizing symptoms. Syndrome subscales of interest in the current investigation included anxious/depressed symptoms, withdrawal, somatic complaints, aggressive, and delinquency. The YSR was normed on a representative US sample of 1,719 youth, aged 11 to 18 years. The YSR has acceptable reliability and validity (Achenbach, 1991c).
Diagnostic Interview Schedule for Children (DISC)
The DISC (Fisher et al., 1993; Piacentini et al., 1993; Schwab-Stone et al., 1993; Shaffer et al., 1993) is a highly structured psychiatric interview for children and adolescents, specifically designed for use by lay interviewers in epidemiological studies. The DISC questions are organized around diagnostic categories. The DISC provides both diagnostic scoring for DSM diagnoses, as well as symptom scales. Extensive evaluation of the psychometric properties of the DISC has been conducted, demonstrating its interrater reliability, test–retest reliability, criterion validity, and sensitivity (Fisher et al., 1993; Piacentini et al., 1993; Schwab-Stone et al., 1993; Shaffer et al., 1993). At Waves 3 and 4 of the study, the substance use module of the DISC was administered. The total count of CAD symptoms in the past year was utilized as the primary outcome measure of interest.
Results
Data analytic plan
Statistical analyses for this study were preformed using Mplus Version 5.21 (Muthén & Muthén, 2008). The following main idiosyncratic data issues were considered in the current analysis: (a) missing data, (b) nonnormality of some indicators, and (c) dependence of observations because of measurement error. Descriptive statistics showed that the percentage of missing data varied by indicator and time, ranging from 0% to 39.8% with a mean of 16% over all indicators and times. Missing data were analyzed as recommended by Shafer and Graham (2002) and were determined to be missing at random. Descriptive statistics also indicated that several of the indicators were skewed and slightly kurtotic. In order to account for data nonnormality, a robust maximum likelihood estimator (MLR) was utilized; MLR standard errors are computed by using a sandwich estimator based on a Huber–White algorithm (Muthén & Muthén, 2008). Maximum likelihood parameter estimates with standard errors and the chi-square test statistic are robust to nonnormality and nonindependence of observations. The MLR chi-square test statistic is asymptotically equivalent to the Yuan-Bentler (1997, 2000) T2 test statistic.
Statistical analyses
For all models, a variety of global fit indices was used, including indices of absolute fit, indices of relative fit, and indices of fit with a penalty function for lack of parsimony. These include the traditional overall chi-square test of model fit (which should be statistically nonsignificant) and the following statistical criteria: the root mean square error of approximation (RMSEA, <0.08; McDonald & Ho, 2002; but see Hu & Bentler, 1998), the Test of Close Fit (p > .05), the comparative fit index (CFI > 0.95), and the standardized root mean square residual (S-RMR, <0.07). The stepwise testing of improvement of fit in the nested models was based on additional absolute model fit indices: the Akaike information criterion (AIC = −2 × model log-likelihood + 2 × number of model parameters), the Bayesian information criterion (BIC = −2 × model log-likelihood + log(n) × number of model parameters), and the sample-size adjusted BIC (i.e., the adjusted BIC). Low values for the AIC, BIC, and adjusted BIC indicate a good-fitting model (Muthén & Muthén, 2008). In addition to the global fit indices, more focused tests included examination of the standardized residual covariances (i.e., values ranging between −2.00 and 2.00) and modification indices (<3.84).
Measurement model
As recommended by Cole and Maxwell (2003), a model in which every latent variable is allowed to correlate with every other latent variable was evaluated for both maltreatment and comparison groups. Manifest variables were related strictly to the latent variables they represented and associations between measurement error terms across time and measures were examined. Among equivalent measures and constructs, correlations of measurement errors were allowed to improve overall model fit. However, this practice was minimized and conducted strictly (i.e., modification index criterion >3.84) when consistent measurement error across measures was methodologically and conceptually expected, such as when the same instrument or construct were used or when previous research suggested interresidual correlation in specific measures (Masten et al., 2005). Table 1 presents the final measurement model indicators, and final cross-domain model’s standardized factor loadings and observed variable R2 values. The measurement model showed good model fit as indicated by the following fit values: CFI = 0.96, RMSEA < 0.037 (90% confidence interval = 0.031–0.044), and S-RMR < 0.068.
Table 1.
Measurement model
| Factor and Indicators | Informant | λ | R2 | Est./SE* |
|---|---|---|---|---|
| Externalizing T1 (age 7–9 years) | ||||
| TRF total externalizing | Counselors | 0.665 | 0.442 | 9.009 |
| PEI Aggression Scale | Counselors | 0.837 | 0.7 | 15.631 |
| PNM Fights Scale | Peers | 0.82 | 0.672 | 13.883 |
| PNM Disruptive Scale | Peers | 0.902 | 0.813 | 24.335 |
| Social competence T1 | ||||
| PNM leader | Peers | 0.413 | 0.171 | 3.446 |
| PNM cooperation | Peers | 0.841 | 0.708 | 4.409 |
| PNM liked most/liked least | Peers | 0.900 | 0.811 | 4.527 |
| Internalizing T1 | ||||
| TRF total internalizing | Counselors | 0.591 | 0.046 | 7.681 |
| PEI Withdrawn Scale | Counselors | 0.893 | 0.798 | 8.731 |
| Externalizing T2 (age 10–12 years) | ||||
| TRF total externalizing | Counselors | 0.667 | 0.586 | 8.527 |
| PEI Aggression Scale | Counselors | 0.806 | 0.666 | 17.081 |
| PNM Fights Scale | Peers | 0.828 | 0.65 | 12.196 |
| PNM Disruptive Scale | Peers | 0.816 | 0.686 | 14.231 |
| Social competence T2 | ||||
| PNM leader | Peers | 0.486 | 0.236 | 5.01 |
| PNM cooperation | Peers | 0.351 | 0.123 | 3.19 |
| PNM liked most/liked least | Peers | 0.905 | 0.819 | 8.215 |
| Internalizing T2 | ||||
| TRF total internalizing | Counselors | 0.784 | 0.523 | 9.74 |
| PEI Withdrawn Scale | Counselors | 0.915 | 0.838 | 12.24 |
| Externalizing T3 (age 13–15 years) | ||||
| YSR Delinquency Scale | Self | 0.704 | 0.496 | 8.085 |
| YSR Aggression Scale | Self | 0.877 | 0.787 | 11.427 |
| Internalizing T3 | ||||
| YSR Withdrawn Scale | Self | 0.671 | 0.454 | 6.908 |
| YSR Somatic Problems Scale | Self | 0.578 | 0.334 | 4.001 |
| YSR Anxious/Depressed Scale | Self | 0.907 | 0.822 | 12.976 |
| Cannabis abuse and dependence | ||||
| Symptoms T3 DISC (1 indicator) | Self | NA | 0.033 | 2.154 |
| Externalizing T4 (age 15–18 years) | ||||
| YSR Delinquency Scale | Self | 0.712 | 0.507 | 7.423 |
| YSR Aggression Scale | Self | 0.817 | 0.668 | 8.518 |
| Internalizing T4 | ||||
| YSR Anxious/Depressed Scale | Self | 0.751 | 0.693 | 12.593 |
| YSR Withdrawn Scale | Self | 0.652 | 0.564 | 7.999 |
| YSR Somatic Problems Scale | Self | 0.832 | 0.425 | 5.192 |
| Cannabis abuse and dependence | ||||
| Symptoms DISC T4 (1 indicator) | Self | NA | 0.296 | 4.018 |
Note: T1, Time 1; TRF, Teacher Report Form (Achenbach, 1991a); PEI, Pupil Evaluation Inventory (Pekarik, Prinz, Liebert, Weintraub,&Neale, 1976); PNM, peer nomination method; T2, Time 2; T3, Time 3; YSR,Youth Self-Report (Achenbach, 1991c); DISC, Diagnostic Interview Schedule for Children; T4, Time 4.
p < .05.
In the measurement model, at Time 1 (T1) and Time 2 (T2), externalizing problems were composed of scores for counselor-rated externalizing symptoms from the TRF and aggressive behavior from the PEI, as well as peer nominations for aggressive and disruptive social behavior. Similarly, indicators for internalizing problems in both waves during childhood included counselor-rated internalizing symptoms from the TRF and nominations for withdrawn behavior from the PEI. The social competence indicators included peer nominations of leadership and cooperativeness, as well as scores for peer acceptance. During the two waves of assessment during adolescence, manifest variables for the externalizing latent variables included YSR scores for the delinquency and the aggression subscales; similarly, indicators for the internalizing latent variables were YSR scores for the subscales of withdrawn, anxious/depressed, and somatic problems.
Gender analyses
The extent to which the final model was invariant across gender was examined. The test of gender invariance revealed significant differences, and a model that assumed gender invariance yielded low and unacceptable fit on a range of fit indices. Thus, gender was used as a covariate for each time point, to examine whether it was significant and whether effects retained significance after partialing out the gender effect. Specifically, no modification indices (>3.84) involving gender were found. Furthermore, path coefficients within the structural model did not differ significantly with the inclusion of gender as a measurement covariate.
Evaluation of cascade models
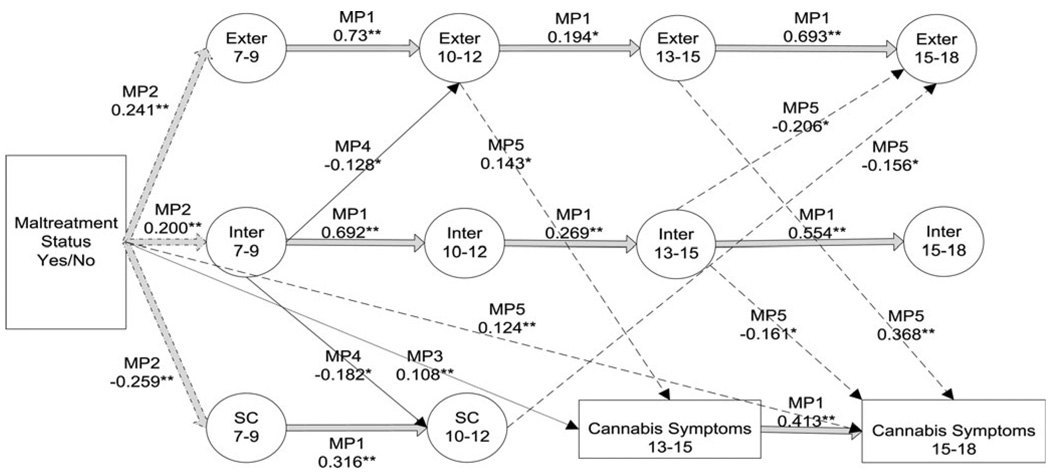
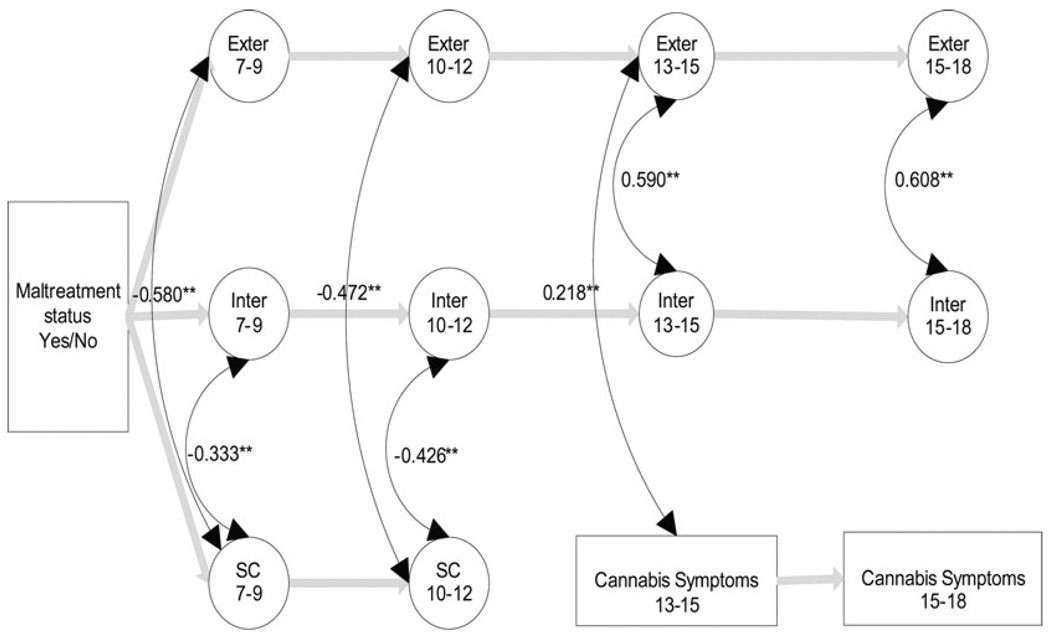
Table 2 presents estimated correlations among variables in the cascade analysis, including the latent constructs for externalizing, internalizing, and social competence, and the observed CAD symptoms variables. Figure 1 depicts the evaluated nested models progressing from Models 1 to 6 by gradually freeing parameters, based on theory and comparing nested models. In Table 3, the paths freed in each of the successive nested models are indicated. Relative fit was evaluated with a scaled chi-square difference test for nested models (Satorra, 2000). Each of the more parsimonious models was compared with the next most complex model (see Table 4). The c coefficient in Table 4 refers to a scaling constant used in chi-square difference tests (see Satorra, 2000). Significant chi-square difference tests were used to assess for relative fit between more to less parsimonious nested models. The AIC, BIC, and chi-square difference tests confirm statistically significant incremental fit from Model 1 up to Model 5, whereas Model 6 shows no statistically enhanced fit. In the current cascade analysis within-time covariation could not be controlled at Wave 1 due to the common variance stemming from maltreatment status as an exogenous variable. However, as shown in Figure 2, cross-lagged effects as well as intercorrelations between residual variances of constructs assessed within waves were freed and evaluated order to debias within-time correlation effects (Cole & Maxwell, 2003; Preacher & Hays, 2008).
Table 2.
Estimated correlation matrix for the latent and observed variables in the cascade analysis
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | LExt 1 | 1.000 | ||||||||||
| 2. | LInt 1 | 0.052 | 1.000 | |||||||||
| 3. | LSC 1 | −0.582 | −0.053 | 1.000 | ||||||||
| 4. | LExt 2 | 0.753 | −0.097 | −0.444 | 1.000 | |||||||
| 5. | LInt 2 | 0.031 | 0.723 | −0.037 | −0.075 | 1.000 | ||||||
| 6. | LSC 2 | −0.275 | −0.311 | 0.348 | −0.459 | −0.224 | 1.000 | |||||
| 7. | LExt 3 | 0.125 | −0.021 | −0.073 | 0.170 | −0.016 | −0.077 | 1.000 | ||||
| 8. | LInt 3 | 0.004 | 0.084 | −0.004 | −0.009 | 0.116 | −0.026 | 0.589 | 1.000 | |||
| 9. | CAD 3 | 0.116 | −0.019 | −0.064 | 0.154 | −0.015 | 0.002 | 0.187 | −0.002 | 1.000 | ||
| 10. | LExt 4 | 0.113 | 0.024 | −0.093 | 0.169 | 0.011 | −0.188 | 0.535 | 0.241 | 0.110 | 1.000 | |
| 11. | LInt 4 | 0.042 | 0.074 | −0.055 | 0.099 | 0.072 | −0.165 | 0.216 | 0.337 | −0.001 | 0.623 | 1.000 |
| 12. | CAD 4 | 0.082 | −0.014 | −0.046 | 0.128 | −0.011 | −0.018 | 0.332 | 0.146 | 0.485 | 0.350 | 0.175 |
Note: LExt, latent externalizing variable; LInt, latent internalizing variable; LSC, latent social competence; CAD, cannabis abuse dependence symptoms. Time periods are listed for respective constructs.
Figure 1.
The significant paths of the final structural model (Model 5; N = 415). Exter, externalizing latent variable; Inter, internalizing latent variable; SC, social competence latent variable; MP1–5, model number and associated significant paths. *p < .05. **p < .01.
Table 3.
Hypothesized nested structural equation modeling models tested in the cascade analysis
| β | CR | β | CR | β | CR | |||
|---|---|---|---|---|---|---|---|---|
| Model 1: baseline | ||||||||
| 1. Ext1 → Ext2* | 0.759 | 21.610 | 4. Int2 → Int3* | 0.233 | 3.251 | 7. Ext3 → Ext4* | 0.494 | 7.859 |
| 2. Int1 → Int2* | 0.625 | 11.519 | 5. Ext2 → Ext3* | 0.143 | 2.271 | 8. Int3 → Int4* | 0.346 | 4.444 |
| 3. SC1 → SC2* | 0.488 | 8.487 | 6. CAD3→CAD4* | 0.509 | 6.161 | |||
| Model 2: child maltreatment | ||||||||
| 1. CM → Ext1* | 0.237 | 5.279 | ||||||
| 2. CM → Int1* | 0.197 | 3.654 | ||||||
| 3. CM → SC1* | −0.273 | −5.287 | ||||||
| Model 3: CM to CAD | ||||||||
| 1. CM → CAD3* | 0.119 | 3.040 | ||||||
| Model 4: early cascade | ||||||||
| 1. Ext1 → Int2 | 0.037 | 0.445 | 4. Int1 → Ext2* | −0.125 | −2.094 | |||
| 2. Ext1 → SC2 | −0.066 | −0.743 | 5. SC1 → Ext2 | −0.020 | −0.300 | |||
| 3. Int1 → SC2* | −0.186 | −2.586 | 6. SC1 → Int2 | 0.086 | 0.904 | |||
| Model 5: late cascade | ||||||||
| 1. SC2 → Ext3 | −0.041 | −0.484 | 6. SC2 → Int4 | −0.124 | −1.577 | 11. Ext2→CAD3* | 0.143 | 2.240 |
| 2. SC2 → Int3 | −0.023 | −0.191 | 7. Int2 → Ext3 | −0.041 | −0.503 | 12. Ext2 → Int3 | 0.069 | 0.575 |
| 3. SC2 → Ext4* | −0.156 | −2.327 | 8. Int2 → CAD3 | −0.054 | −0.793 | 13. Ext3→CAD4* | 0.368 | 4.385 |
| 4. SC2 → CAD 3 | 0.061 | 0.842 | 9. Int3 → Ext4* | −0.206 | −2.356 | 14. CM → CAD4* | 0.124 | 2.692 |
| 5. SC2 → CAD 4 | −0.009 | −0.190 | 10. Int3→CAD 4* | −0.161 | −2.309 | |||
| Model 6: CAD | ||||||||
| 1. Ext3 → Int4 | −0.443 | −0.490 | 2. CAD3 → Ext4 | 0.015 | 0.163 | |||
| 3. CAD3 → Int4 | 0.047 | 0.360 |
Note: CR, critical ratio; Ext, externalizing; Int, internalizing; SC, social competence; CM, child maltreatment; CAD, cannabis abuse dependence, for respective time periods.
p < .05.
Table 4.
Fit statistic and model comparisons for hierarchically nested structural equation models
| Model | Cross-Domains | df | c | χ2 | CFI | S-RMR | RMSEA | Model Comparison | AIC | BIC SS Adj. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 0 | 422 | 1.025 | 759.6* | 0.924 | 0.085 | 0.044 | — | 47,572 | 47,686 |
| 2 | 0 | 419 | 1.026 | 720.2* | 0.932 | 0.078 | 0.042 | 1 vs. 2 | 47,538 | 47,655 |
| 3 | 0 | 418 | 1.027 | 713.9* | 0.933 | 0.077 | 0.041 | 2 vs. 3 | 47,534 | 47,652 |
| 4 | 6 | 412 | 1.024 | 697.7* | 0.935 | 0.078 | 0.041 | 3 vs. 4 | 47,529 | 47,651 |
| 5 | 14 | 397 | 1.026 | 646.8* | 0.944 | 0.066 | 0.039 | 4 vs. 5 | 47,507 | 47,642 |
| 6 | 3 | 394 | 1.020 | 649.1* | 0.942 | 0.066 | 0.039 | 5 vs. 6 | 47,511 | 47,649 |
Note: c, the weighting constant for computing the chi-square statistic using the robust estimation method; CFI, comparative fit index; S-RMR, standardized root mean square residual; RMSEA, root mean square error of approximation; AIC, Akaike information criterion; BIC SS Adj., Bayesian information criterion, sample-size adjusted.
p < .05.
Figure 2.
The standardized within-time covariances among residual variances for Model 5 (N = 415). Exter, externalizing latent variable; Inter, internalizing latent variable; SC, social competence latent variable. **p < .01.
Table 3 provides standardized path coefficients for paths that were released within each of the six nested models. Figure 1 depicts the sequence of nested models with final standardized path coefficients of Model 5.
First model
The goal of the first model was to evaluate the stability of social competence, internalizing and externalizing problems across the four developmental periods. The path analysis supports substantial stability across all of the investigated domains. Children with high externalizing, internalizing, and social competence at T1 were predicted to show similarly high levels in these domains at subsequent time points up to late adolescence. Similarly, early adolescence (i.e., Time 3 [T3]) CAD symptoms significantly predicted positive symptoms in late adolescence at Wave 4.
Second model
The goal of the second model was to evaluate the rank-order developmental stability of internalizing and externalizing problem across four developmental periods when child maltreatment status (vs. nonmaltreatment) was an independent variable. Thus, by adding child maltreatment status as an exogenous variable the second model examined how child maltreatment sets off diverse maladaptive developmental processes and whether these maladaptive outcomes were stable over time. Results supported the maladaptive effect child maltreatment shows across all of the examined levels: internalizing, externalizing, and social competence.
Third model
The aim of the third model was to test the third hypothesis regarding the direct role of childhood maltreatment experiences on the development of youth CAD symptoms. The third model indicated significant relations between child maltreatment prior to Wave 1 and CAD symptoms at Wave 3 (age range = 13–15 years; critical ratio [CR] = 2.77; p < .001). After adding maltreatment as an independent variable predicting CAD symptoms at Wave 3, continuity in predictive relationship from Wave 3 to Wave 4 in CAD symptoms sustained statistical significance, suggesting an indirect path from child maltreatment to late adolescence CAD symptoms via early adolescence CAD symptoms.
Fourth model
The aim of the fourth model was to test the fourth hypothesis regarding cross-domain relations between constructs at earlier childhood (Wave 1) to compromised internalizing, externalizing, and social competence at late childhood (Wave 2) as suggested by previous research (Kerr, Tremblay, Pagani, & Vitaro, 1997; Masten et al. 2005). The model confirmed relations for the influence of internalizing on cross-domains from age 7 to 9 years to 10 to 12 years. Specifically, internalizing problems at age 7 to 9 years (Wave 1) significantly predicted lower social competence at age range 10 to 12 (Wave 2; CR = 2.77, p < .01). In addition, internalizing problems at age range 7 to 9 showed negative predictive relations with externalizing problems at ages 10 to 12 (CR = −2.09; p < .05).
Fifth model
The aim of the fifth model was to test the fifth hypothesis regarding adjacent cross domain hypothesized relations of the assessed behaviors in the current study from late childhood into adolescence. Thus, the fifth model evaluated whether externalizing problems at Waves 2 and 3 predicted CAD symptoms at Wave 3 and Wave 4, respectively. Similarly, relations between social competence at late childhood (Wave 2) and internalizing and externalizing in adolescence were evaluated. An additional aim was to determine whether a direct effect from child maltreatment status before age 8 to CAD symptoms would be observed after accounting for all of the indirect effects released up to model 5. Results suggested significant relations between externalizing problems and subsequent CAD symptoms, with Wave 2 externalizing predicting Wave 3 CAD (CR = 2.24, p < .05) symptoms and Wave 3 externalizing further contributing to Wave 4 CAD (CR = 4.38, p < .01) symptoms. In contrast, social competence at late childhood as well as internalizing problems at Wave 3 negatively predicted externalizing problem at late adolescence (CR = −2.32, p < .05; CR = −2.35, p < .05, respectively). Furthermore, internalizing at Wave 3 negatively predicted CAD at Wave 4 (CR = −2.30, p < .05). Finally, child maltreatment status prior to age 8 maintained a significant contribution to prediction of CAD symptoms at Wave 4 (CR = 2.69, p < .01).
Sixth model
Last, we evaluated our sixth hypothesis specifying that CAD symptoms in early adolescence would contribute to increases in internalizing and/or externalizing symptoms in late adolescence. We also included unexamined cross-domain paths predicting internalizing symptoms at Wave 4 via externalizing. None of the additional paths were statistically significant. The addition of these paths contributed to deterioration in model fit on a range of fit indices, including model parsimony indices (Table 4), and resulted in a nonsignificant change in the chi-square value. Thus, an independent influence of early adolescent cannabis use problems on increasing late adolescent internalizing and externalizing symptoms was not supported.
Discussion
In the current investigation we sought to understand the development of substance abuse problems, in particular, CAD symptoms, utilizing a developmental cascades formulation (Burt et al., 2008; Burt & Roisman, 2010; Masten et al., 2005). Unique to the current work was the application of a cascades analysis to evaluate specific developmental pathways promoting drug use problems ensuing from early experiences of abuse and neglect. In addition, the approach focused on an emergent adolescent problem behavior, cannabis abuse, and dependence, an adverse outcome not salient or observed earlier in development.
Consistent with Masten and Burt and their colleagues’ findings, we found support for continuity of behavior problems, both internalizing and externalizing symptomatology, across the four developmental waves of assessment, from the earlier school-age years to later adolescence. These findings support the concept of rank-order stability in these two broadband forms of psychopathology across development and indicate that early occurring behavior problems are not transient concerns. Moreover, earlier social competence was related to late childhood social competence, and early adolescent cannabis use problems portended continuity of these problems later in adolescence.
With these patterns of continuity established, a more interesting picture emerged when child maltreatment occurring earlier in development was added to the cascades model. Child maltreatment prior to age 8 significantly predicted the three early school-age domains, externalizing and internalizing problems, as well as low social competence. These findings are consistent with prior work that has demonstrated the risk for heightened behavioral disturbance occurring among maltreated children, as well as compromises in the development of social competence, an important overarching stage salient issue of childhood (Cicchetti & Valentino, 2006; Masten et al., 1999; Sroufe, 1989). It is important that we also found evidence for a direct effect of early child maltreatment on higher levels of CAD symptoms in the early adolescent period. Moreover, early maltreatment continued to contribute independently to increases in problem cannabis use in late adolescence. Thus, our expectation of higher risk for substance use problems among youth with a history of maltreatment was confirmed.
Our next step in the cascades analysis was to progressively consider the influence of pathways in a developmental sequence. Thus, we evaluated cross-lagged relations occurring among domains from earlier to later childhood. Internalizing problems were found to play an influential role. In particular, early internalizing problems served to curb the development of later increases in childhood externalizing difficulties, a finding consistent with the braking effect of internalizing symptoms on antisocial development (Burt et al., 2008; Masten et al., 2005). In addition, early internalizing difficulties contributed to decreases in social competence later in childhood. Thus, children who socially withdraw and struggle with anxiety and depression increasingly are less successful in engaging with their peers, forming friendships, and developing prosocial behaviors. Note also that, with the addition of this pathway, both direct and indirect contributions of child maltreatment to diminished social competence among peers were identified; maltreatment was related to social competence directly while also contributing to internalizing problems, leading to further decrements in competence in the peer arena.
We next sought to examine cross-lagged influences across the transition from late childhood into the early adolescent years, and these respective paths were added to the cascades model. It is important that a significant path emerged linking late childhood externalizing problems to CAD symptoms in early adolescence. This finding is consistent with a substantial range of findings linking adolescent substance use to conduct disturbance. Furthermore, this relation is further instantiated by the significant path between early adolescent externalizing problems, and late adolescent cannabis use problems. Thus, continuities in externalizing problems further contribute to increases in substance abuse difficulties later in adolescence. Of note, in addition to the direct influence of child maltreatment on CAD symptoms, indirect pathways to early substance problems and increases in these problems in late adolescence via externalizing pathology are supported.
In addition to the cross-domain influences in the current cascade model, it is important to note that we obtained independent direct pathways between child maltreatment and early as well as late adolescent cannabis problem use, and the influence of late childhood antisocial behavior did not account for this association. These direct effects suggest that there are other processes associated with child maltreatment that are not accounted for by the development of behavioral problems or poor social competence. In determining what these processes are, it is important to note that the nonmaltreated youth reside in the same impoverished neighborhood contexts as the maltreated youth, suggesting that other familial influences are likely involved. Examination of a potentially higher likelihood of parental substance use in the maltreating families, greater exposure to substance use in the home, and/or poor parental monitoring in maltreating families are possible processes that may account for this effect. Further investigation of mediators of the direct effect of maltreatment on adolescent problem use would be important to address in future work.
Evidence for linkages between child and adolescent internalizing difficulties and cannabis problem use received some limited support in these analyses. Rather than contributing to substance use problems, early adolescent internalizing problems were found to reduce increases in late adolescent CAD symptoms, as well as externalizing problems. These relations are similar to the braking influence of internalizing symptomatology on externalizing difficulties observed in the current study during childhood. The more restricted contribution of internalizing difficulties to substance use is consistent with the more equivocal role for internalizing pathology in substance abuse during the adolescent period of development. Contrary to expectations, an association between late childhood social competence and cannabis use problems also was not supported. It may be that the influence of social difficulties and rejection by peers, and the development of relations with deviant peers in adolescence on substance involvement is accounted for more directly and fully by child externalizing problems. However, a very interesting significant path was found between diminished late childhood social competence and increases in late adolescent externalizing problems. This effect is above and beyond the influence of stability in externalizing difficulties stemming from the childhood years. Moreover, it is noteworthy that this pathway also links early childhood internalizing problems to increases in late adolescent antisocial behaviors via diminished social competence in late childhood. Thus, cascading influences across development among the three domains are demonstrated, and these linkages again are sequelae of early maltreatment experiences. The externalizing stability pathway from child maltreatment to late adolescent externalizing problems is suggestive of Moffitt’s (1993) life course persistent trajectory, whereas the cascading pathway from maltreatment to early internalizing difficulties to late childhood decrements in social competence to increases in late adolescent antisocial behavior may reflect youth following an adolescent onset or adolescent limited trajectory.
Finally, we did not find support for early adolescent CAD symptoms contributing to changes in late adolescent externalizing and internalizing pathology. It may be the case that the adverse consequences of substance use problems on functioning have not yet emerged during the adolescent period. However, if further assessment of this sample were available, then the influence of adolescent substance abuse problems on young adult functioning may become apparent.
The findings of this investigation are important on a number of levels. First, the evidence in support of a cascade model linking childhood functioning to adolescent self-report of DSM cannabis and abuse symptoms provides further empirical demonstration of the developmental contributions to emerging substance use problems in early adolescence and their continuity. Adolescent substance use problems and disorders are clearly a form of developmental dysfunction with influences extending back to early childhood. Second, the results specify the linkages between early childhood maltreatment and ensuing engagement in problematic substance use during the adolescent period of development, further delineating the processes through which child abuse and neglect sequentially impair developmental competencies and eventuate in later adverse outcomes.
Our findings are consistent with the cascade models linking early experience and resulting behavior problems to adolescent substance use and abuse (Dodge et al., 2009; Martell et al., 2009). Neither of these models was specifically focused on the impact of child maltreatment on substance use and abuse. However, both models note early parenting risk as an important instigating source for the unfolding of subsequent child maladaptation and conduct disturbance. Utilizing the cascade modeling approach of Masten and colleagues (Burt & Roisman, 2010; Burt et al., 2008; Masten et al., 2005) with repeated assessment of the developmental constructs across assessment waves and controlling for within-wave covariation among constructs, allowed for amore precise delineation of influences among externalizing, internalizing, and social competence across development. We also focused on CAD symptoms rather than the onset of substance use in general (cf. Dodge et al., 2009).Marijuana is an illicit substance, and examination of problematic cannabis use as indicated by abuse and dependence symptoms indicates further penetrance of problematic substance use than initiation alone. Problems with cannabis use have been identified as particularly salient among maltreated youth and young adults (Fergusson et al., 2007), and Widom has identified continuing problems with cannabis use among maltreated individuals extending into middle adulthood (Widom et al., 2006). Thus, the current findings suggest that early emerging CAD may presage long term difficulties with substance use problems among maltreated individuals.
Limitations and Conclusion
A number of limitations of the current investigation should be noted. The current research would have been enhanced by knowledge of the developmental trajectories of maltreated and nonmaltreated children prior to the initial wave of assessment at ages 7 to 9. The maltreated children in this sample had experienced abuse and/or neglect earlier in childhood prior to recruitment. A burgeoning body of research (Cicchetti & Lynch, 1995; Cicchetti & Valentino, 2006) has articulated the processes through which child maltreatment threatens the competent resolution of developmental tasks across the earlier years of life, and these compromised adaptations are likely to be represented in the behavior problems and poor social competence observed in the early elementary school years. This knowledge would allow for a more refined delineation of earlier developmental liabilities in emotion regulation, attachment organization, autonomous self development, and representational capacities that unfold into behavioral disturbances in the childhood years (Sroufe, 1990) and subsequently contribute to adolescent substance abuse problems (Masten et al., 2009).
Our measurement approach did not include a comparable measure of social competence across the two waves of assessment during adolescence as we had obtained during childhood. The results of the cascade model may have been altered had we been able to incorporate social competence indicators during adolescence. In addition, our measures of adolescent psychopathology and substance use were obtained through self-report, and the findings may have been enhanced if other methods of assessment were obtained. It also would have been beneficial had we been able to incorporate an ascertainment of parental substance use disorders into our developmental model in order to interweave this prominent risk factor into our findings. Finally, the complexity of our cascade model would likely have been increased had a consideration of the diversity of maltreatment experiences (i.e., variation in the subtypes of maltreatment, severity, chronicity, and developmental timing) been investigated; attention to this variation should be addressed in subsequent investigations.
The current cascade model is primarily psychosocial in conceptualization. Further research in this area would benefit from incorporating a more multidisciplinary appreciation of the biological contributions to the developmental progressions we have identified contributing to substance abuse problems (Brown et al., 2009; Zucker, 2006). Increasingly, the biological sequelae of child maltreatment are being documented. For example, the chronic stress associated with child maltreatment has been shown to influence neuroendocrine dysregulation (Cicchetti & Rogosch, 2001a, 2001b; Cicchetti, Rogosch, Gunnar, & Toth, 2010; DeBellis, 2001; Heim, Newport, Mletzko, Miller, & Nemeroff, 2008; Trickett, Noll, Susman, Shenk, & Putman, 2010) and psychopathology, and aberrations in the physiological regulation of stress may then extend to vulnerabilities for substance use and abuse directly or through associations with other forms of psychopathology. Neurophysiological atypicalities in the processing of emotions among maltreated children (Cicchetti & Curtis, 2005; Pollak, Cicchetti, Klorman, & Brumaghim, 1997; Pollak, Klorman, Thatcher, & Cicchetti, 2001) also may influence social information processing and social functioning, as well as behavioral adjustment, thereby contributing to the developmental cascade toward substance use problems and vulnerability to addiction (Koob & Volkow, 2010). Deficits in cognitive executive functions may contribute to impulsivity and poor decision making, creating heightening risk for substance abuse among maltreated youth (Tarter, 2002; Tarter et al., 2003). In addition, investigations of gene by environment interactions have shown that allelic variations in certain genes (e.g., MAOA, 5-HTTLPR, CRHR1) moderate the impact of maltreatment on the development of psychopathology and personality functioning and may serve a protective function (Bradley et al., 2008; Caspi et al., 2002, 2003; Cicchetti, Rogosch, & Sturge-Apple, 2007; DeYoung, Cicchetti, & Rogosch, 2010; Kim-Cohen & Gold, 2009; Polanczyk et al., 2009). Investigation of Gene × Environment interactions in the context of the current cascade model could more clearly delineate which youth are more vulnerable to substance use problems in context of child maltreatment and environmental adversity.
The findings of this investigation also have important implications for prevention and intervention. The developmental cascade model supports the growing evidence indicating that substance use problems in adolescence have roots that unfold from earlier adverse developmental experience and consequent maladaptations. To avert this cascading process, early preventive intervention with vulnerable families to reduce the emergence of child abuse and neglect would eliminate this major risk factor. Moreover, when maltreatment has occurred, interventions to decrease family dysfunction and promote competence in children would contribute to diverting children from engaging maladaptive developmental trajectories. The continuities in early externalizing problems and their contributions to adolescent substance abuse and dependence also indicate that these problems are not transient and that effective early interventions to reduce aggressive and conduct problem behavior are clearly warranted.
Acknowledgments
This research was supported by funding from the National Institute on Drug Abuse (DA12903, DA17741) and the Spunk Fund, Inc.
References
- Achenbach T. Manual for the Child Behavior Checklist and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991a. [Google Scholar]
- Achenbach T. Manual for the Teacher Report Form and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991b. [Google Scholar]
- Achenbach T. Manual for the Youth Self-Report and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991c. [Google Scholar]
- Barnett D, Manly JT, Cicchetti D. Defining child maltreatment: The interface between policy and research. In: Cicchetti D, Toth SL, editors. Child abuse, child development, and social policy. Norwood, NJ: Ablex; 1993. pp. 7–73. [Google Scholar]
- Bayatpour M, Wells RD, Holford S. Physical and sexual abuse as predictors of substance abuse and suicide among pregnant teenagers. Journal of Adolescent Health. 1992;13:128–132. doi: 10.1016/1054-139x(92)90079-q. [DOI] [PubMed] [Google Scholar]
- Bolger KE, Patterson CJ. Developmental pathways from child maltreatment to peer rejection. Child Development. 2001;72:549–568. doi: 10.1111/1467-8624.00296. [DOI] [PubMed] [Google Scholar]
- Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, et al. Influence of child abuse on adult depression: Moderation by the corticotropin-releasing hormone receptor gene. Archives of General Psychiatry. 2008;65:190–200. doi: 10.1001/archgenpsychiatry.2007.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, et al. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. 2009;121:S290–S310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt KB, Obradovic J, Long JD, Masten AS. The interplay of social competence and psychopathology over 20 years: Testing transactional and cascade models. Child Development. 2008;79:359–374. doi: 10.1111/j.1467-8624.2007.01130.x. [DOI] [PubMed] [Google Scholar]
- Burt KB, Roisman GI. Competence and psychopathology: Cascade effects in the NICHD Study of Early Child Care and Youth Development. Development and Psychopathology. 2010;22:557–567. doi: 10.1017/S0954579410000271. [DOI] [PubMed] [Google Scholar]
- Caspi A, McClay J, Moffitt TE, Mill J, Martin J, Craig IW, et al. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cavaiola AA, Schiff M. Behavioral sequelae of physical and/or sexual abuse in adolescents. Child Abuse & Neglect. 1988;12:181–188. doi: 10.1016/0145-2134(88)90026-9. [DOI] [PubMed] [Google Scholar]
- Chassin L, Hussong A, Beltran I. Adolescent substance abuse. In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology. 3rd ed. New York: Wiley; 2009. pp. 723–763. [Google Scholar]
- Cicchetti D, Curtis WJ. An event-related potential study of processing of affective facial expressions in young children who have experienced maltreatment during the first year of life. Development and Psychopathology. 2005;17:641–677. doi: 10.1017/S0954579405050315. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Lynch M. Toward an ecological/transactional model of community violence and child maltreatment: Consequences for children’s development. Psychiatry. 1993;56:96–118. doi: 10.1080/00332747.1993.11024624. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Lynch M. Failures in the expectable environment and their impact on individual development: The case of child maltreatment. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 2. Risk, disorder, and adaptation. New York: Wiley; 1995. pp. 32–71. [Google Scholar]
- Cicchetti D, Luthar SS, editors. Development and Psychopathology. Vol. 11. 1999. Developmental approaches to substance use and abuse; pp. 655–988. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Manly JT. A personal perspective on conducting research with maltreating families: Problems and solutions. In: Brody G, Sigel I, editors. Methods of family research: Families at risk. Vol. 2. Hillsdale, NJ: Erlbaum; 1990. pp. 87–133. [Google Scholar]
- Cicchetti D, Rogosch FA. Psychopathology as risk for adolescent substance use disorders: A developmental psychopathology perspective. Journal of Clinical Child Psychology. 1999;28:355–365. doi: 10.1207/S15374424jccp280308. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Diverse patterns of neuroendocrine activity in maltreated children. Development and Psychopathology. 2001a;13:677–694. doi: 10.1017/s0954579401003145. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. The impact of child maltreatment and psychopathology upon neuroendocrine functioning. Development and Psychopathology. 2001b;13:755–758. [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology. 2002;70:6–20. doi: 10.1037//0022-006x.70.1.6. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Gunnar MR, Toth SL. The differential impacts of early abuse on internalizing problems and diurnal cortisol activity in school-aged children. Child Development. 2010;81:252–269. doi: 10.1111/j.1467-8624.2009.01393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Sturge-Apple ML. Interactions of child maltreatment and serotonin transporter and monoamine oxidase A polymorphisms: Depressive symptomatology among adolescents from low socioeconomic status backgrounds. Development and Psychopathology. 2007;19:1161–1180. doi: 10.1017/S0954579407000600. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Schneider-Rosen K. An organizational approach to childhood depression. In: Rutter M, Izard C, Read P, editors. Depression in young people, clinical and developmental perspectives. New York: Guilford Press; 1986. pp. 71–134. [Google Scholar]
- Cicchetti D, Toth SL, Manly JT. Maternal Maltreatment Classification Interview. Rochester, NY: Mt. Hope Family Center; 2003. Unpublished manuscript. [Google Scholar]
- Cicchetti D, Valentino K. An ecological transactional perspective on child maltreatment: Failure of the average expectable environment and its influence upon child development. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 3. Risk, disorder, and adaptation. 2nd ed. New York: Wiley; 2006. pp. 129–201. [Google Scholar]
- Coie JD, Dodge KA. Continuities and changes in children’s social status: A five-year longitudinal study. Merrill-Palmer Quarterly. 1983;29:261–282. [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Costello EJ. Psychiatric predictors of adolescent and young adult drug use and abuse. Drug and Alcohol Dependence. 2007;88S:S97–S99. doi: 10.1016/j.drugalcdep.2006.12.027. [DOI] [PubMed] [Google Scholar]
- DeBellis MD. Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology. 2001;13:539–564. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- Dembo R, Dertke M, Borders S, Washburn M, Schmeidler J. The relationship between physical abuse, sexual abuse and tobacco, alcohol, and illicit drug use among youths in a juvenile detention center. International Journal of the Addictions. 1988;23:351–378. doi: 10.3109/10826088809039203. [DOI] [PubMed] [Google Scholar]
- DeYoung C, Cicchetti D, Rogosch FA. Variation in the CRHR1 gene and moderation of the association between childhood maltreatment and neuroticism. 2010 doi: 10.1111/j.1469-7610.2011.02404.x. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Malone PS, Landsford JE, Miller S, Pettit GS, Bates JE. A dynamic cascade model of the development of substance-use onset. Monographs of the Society for Research in Child Development. 2009;74:1–120. doi: 10.1111/j.1540-5834.2009.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwall GE, Hoffman NG, Harrison PA. Psychological correlates of sexual abuse in adolescent girls in chemical dependency. Journal of Adolescent Chemical Dependency. 1989;1:53–68. [PubMed] [Google Scholar]
- English DJ, Upadhyaya MP, Litrownik AJ, Marshall JM, Runyan DK, Graham JC, et al. Maltreatment’s wake: The relationship of maltreatment dimensions to child outcomes. Child Abuse & Neglect. 2005;29:597–619. doi: 10.1016/j.chiabu.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Exposure to childhood sexual and physical abuse and adjustment in early adulthood. Child Abuse & Neglect. 2008;32:607–619. doi: 10.1016/j.chiabu.2006.12.018. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Conduct and attentional problems in childhood and adolescence: Results of a 25-year longitudinal study. Drug Abuse and Dependence. 2007;88S:S14–S26. doi: 10.1016/j.drugalcdep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- Fisher P, Shaffer D, Piacentini J, Lapkin J, Kafantaris V, Leonard H, et al. Sensitivity of the Diagnostic Interview Schedule for Children (2nd ed., DISC-2.1) for specific diagnoses of children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:666–673. doi: 10.1097/00004583-199305000-00026. [DOI] [PubMed] [Google Scholar]
- Glantz MD, Leshner AI. Drug abuse and developmental psychopathology. Development and Psychopathology. 2000;12:795–814. doi: 10.1017/s0954579400004120. [DOI] [PubMed] [Google Scholar]
- Harrison PA, Fulkerson JA, Beebe TJ. Multiple substance use among adolescent physical and sexual abuse victims. Child Abuse & Neglect. 1997;21:529–539. doi: 10.1016/s0145-2134(97)00013-6. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33:693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Dodge KA, Rutter M, Taylor A, et al. Nature × nurture: Genetic vulnerabilities interact with physical maltreatment to promote conduct problems. Development and Psychopathology. 2005;17:67–84. doi: 10.1017/s0954579405050042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology. 2007;116:176–187. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]
- Kelly BT, Thornberry TP, Smith CA. In the wake of child maltreatment. Washington, DC: Office of Juvenile Justice and Delinquency Prevention; 1997. pp. 1–15. [Google Scholar]
- Kerr M, Tremblay RE, Pagani L, Vitaro F. Boys’ behavioral inhibition and the risk of later delinquency. Archives of General Psychiatry. 1997;54:809–816. doi: 10.1001/archpsyc.1997.01830210049005. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Gold AL. Measured gene-environement interactions and mechanisms promoting resilient development. Current Directions in Psychological Science. 2009;18:138–142. [Google Scholar]
- Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology Reviews. 2010;35:217–238. doi: 10.1038/npp.2009.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald RP, Ho M-HR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7:64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- Manly JT. Advances in research definitions of child maltreatment. Child Abuse & Neglect. 2005;29:425–439. doi: 10.1016/j.chiabu.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Manly JT, Cicchetti D, Barnett D. The impact of subtype, frequency, chronicity, and severity of childmaltreatment on social competence and behavior problems. Development and Psychopathology. 1994;6:121–143. [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, Cicchetti D. Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and Psychopathology. 2001;13:759–782. [PubMed] [Google Scholar]
- Martell MM, Pierce L, Nigg JT, Jester JM, Adams K, Puttler LI, et al. Temperamental pathways to childhood disruptive behavior and adolescent substance abuse: Testing a cascade model. Journal of Abnormal Child Psychology. 2009;37:363–373. doi: 10.1007/s10802-008-9269-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Coatsworth JD. The development of competence in favorable and unfavorable environments: Lessons from research on successful children. American Psychologist. 1998;53:205–220. doi: 10.1037//0003-066x.53.2.205. [DOI] [PubMed] [Google Scholar]
- Masten AS, Desjardins CD, McCormick CM, Kuo SI, Long JD. The significance of childhood competence for adult success at work: A developmental cascade analysis. Development and Psychopathology. 2010;22:679–694. doi: 10.1017/S0954579410000362. [DOI] [PubMed] [Google Scholar]
- Masten AS, Faden VB, Zucker RA, Spear LP. Underage drinking: A developmental framework. Pediatrics. 2009;121:S235–S251. doi: 10.1542/peds.2007-2243A. [DOI] [PubMed] [Google Scholar]
- Masten AS, Hubbard JJ, Gest SD, Tellegen A, Garmezy N, Ramirez M. Competence in the context of adversity: Pathways to resilience and maladaptation from childhood to late adolescence. Development and Psychopathology. 1999;11:143–169. doi: 10.1017/s0954579499001996. [DOI] [PubMed] [Google Scholar]
- Masten AS, Roisman GI, Long JD, Burt KB, Obradovic J, Riley JR, et al. Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. Developmental Psychology. 2005;41:733–746. doi: 10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. “Life-course persistent” and “adolescence-limited” antisocial behavior: A developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Moran PB, Vuchinich S, Hall NK. Associations between types of maltreatment and substance use during adolescence. Child Abuse & Neglect. 2004;28:565–574. doi: 10.1016/j.chiabu.2003.12.002. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6th ed. Los Angeles: Author; 2008. [Google Scholar]
- Oshri A, Tubman JG, Wagner EF, Leon-Morris S, Snyders J. Psychiatric symptom patterns, proximal risk factors, and sexual risk behaviors among youth in outpatient substance abuse treatment. American Journal of Orthopsychiatry. 2008;78:430–441. doi: 10.1037/a0014326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekarkik E, Prinz R, Liebert D, Weintraub S, Neale J. The Pupil Evaluation Inventory: A sociometric technique for assessing children’s social behavior. Journal of Abnormal Child Psychology. 1976;4:83–97. doi: 10.1007/BF00917607. [DOI] [PubMed] [Google Scholar]
- Piacentini J, Shaffer D, Fisher P, Schwab-Stone M, Davies M, Goia P. The Diagnostic Interview Schedule for Children—Revised (DISC-R): III. Concurrent criterion validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:658–665. doi: 10.1097/00004583-199305000-00025. [DOI] [PubMed] [Google Scholar]
- Polanczyk G, Caspi A, Williams B, Price TS, Danese A, Sugden K, et al. Protective effect of CRHR1 gene variants on the development of adult depression following childhood maltreatment: Replication and extension. Archives of General Psychiatry. 2009;66:978–985. doi: 10.1001/archgenpsychiatry.2009.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD, Cicchetti D, Klorman R, Brumaghim JT. Cognitive brain event-related potentials and emotion processing in maltreated children. Child Development. 1997;68:773–787. doi: 10.1111/j.1467-8624.1997.tb01961.x. [DOI] [PubMed] [Google Scholar]
- Pollak SD, Klorman R, Thatcher JE, Cicchetti D. P3b reflects maltreated children’s reactions to facial displays of emotion. Psychophysiology. 2001;38:267–274. [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Pribor EF, Dinwiddie SH. Psychiatric correlates of incest in childhood. American Journal of Psychiatry. 1992;149:52–56. doi: 10.1176/ajp.149.1.52. [DOI] [PubMed] [Google Scholar]
- Rodgers CS, Lang AJ, Laffaye C, Satz LE, Dresselhaus TR, Stein MB. The impact of individual forms of child maltreatment on health behavior. Child Abuse & Neglect. 2004;28:575–586. doi: 10.1016/j.chiabu.2004.01.002. [DOI] [PubMed] [Google Scholar]
- Satorra A. Scaled and adjusted restricted tests in multi-sample analysis of moment structures. In: Heijmans RDH, Pollock DSG, Satorra A, editors. Innovations in multivariate statistical analysis: A festschrift for Heinz Neudecker. London: Kluwer Academic; 2000. pp. 233–247. [Google Scholar]
- Schaefer MR, Sobieragi K, Hollyfield RL. Prevalence of child physical abuse in adult male veteran alcoholics. Child Abuse & Neglect. 1988;12:141–150. doi: 10.1016/0145-2134(88)90022-1. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schwab-Stone M, Fisher P, Piacentini J, Shaffer D, Davies M, Briggs M. The Diagnostic Interview Schedule for Children—Revised Version (DISC-R): II. Test–retest reliability. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:651–657. doi: 10.1097/00004583-199305000-00024. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Schwab-Stone M, Fisher P, Cohen P, Piacentini J, Davies M, et al. The Diagnostic Interview Schedule for Children—Revised (DISC-R): I. Preparation, field testing, and interrater reliability. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:643–650. doi: 10.1097/00004583-199305000-00023. [DOI] [PubMed] [Google Scholar]
- Sroufe LA. Relationships, self, and individual adaptation. In: Sameroff AJ, Emde RN, editors. Relationship disturbances in early childhood. New York: Basic Books; 1989. pp. 70–94. [Google Scholar]
- Sroufe LA. Considering normal and abnormal together: The essence of developmental psychopathology. Development and Psychopathology. 1990;2:335–347. [Google Scholar]
- Stouthamer-Loeber M, Loeber R, Homish DL, Wei E. Maltreatment of boys and the development of disruptive and delinquent behavior. Development and Psychopathology. 2001;13:941–956. [PubMed] [Google Scholar]
- Tarter RE. Etiology of adolescent substance abuse: A developmental perspective. American Journal on Addictions. 2002;11:171–191. doi: 10.1080/10550490290087965. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, et al. Neurobehavioral disinhibition in childhood predicts early onset of substance use disorder. American Journal of Psychiatry. 2003;160:1078–1085. doi: 10.1176/appi.ajp.160.6.1078. [DOI] [PubMed] [Google Scholar]
- Trickett PK, McBride-Chang C. The developmental impact of different types of child abuse and neglect. Developmental Review. 1995;15:311–337. [Google Scholar]
- Trickett PK, Noll JG, Susman EJ, Shenk CE, Putnam FW. Attenuation of cortisol across development for victims of sexual abuse. Development and Psychopathology. 2010;22:165–175. doi: 10.1017/S0954579409990332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg NZ, Rahdert E, Colliver JD, Glantz MD. Adolescent substance abuse: A Review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;37:252–261. doi: 10.1097/00004583-199803000-00009. [DOI] [PubMed] [Google Scholar]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- Widom CS, Mamorstein NR, White HR. Childhood victimization and illicit drug use in middle adulthood. Psychology of Addictive Behaviors. 2006;20:394–403. doi: 10.1037/0893-164X.20.4.394. [DOI] [PubMed] [Google Scholar]
- Wilson HW, Widom CS. A prospective examination of the path from child abuse and neglect to illicit drug use in middle adulthood: The potential mediating role of four risk factors. Journal of Youth and Adolescence. 2009;38:340–354. doi: 10.1007/s10964-008-9331-6. [DOI] [PubMed] [Google Scholar]
- Windle M, Spear LP, Fuglini AJ, Angold A, Brown JD, Pine D, et al. Transitions to underage and problem drinking: Developmental processes and mechanisms between 10 and 15 years of age. Pediatrics. 2009;121:S273–S289. doi: 10.1542/peds.2007-2243C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen H, Frohlich C, Behrendt S, Gunter A, Rehm J, Zimmerman P, et al. Cannabis use and cannabis use disorders and their relationship to mental disorders: A 10-year prospective-longitudinal community sample of adolescents. Drug and Alcohol Dependence. 2007;88S:S60–S70. doi: 10.1016/j.drugalcdep.2006.12.013. [DOI] [PubMed] [Google Scholar]
- Yuan H, Bentler PM. Finite sample distribution-free test statistics for nested structural models. Behaviormetrika. 1997;24:19–26. [Google Scholar]
- Yuan H, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology. 2000;30:165–200. [Google Scholar]
- Zucker RA. Alcohol use and the alcohol use disorders: A developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 3. Risk, disorder, and adaptation. 2nd ed. New York: Wiley; 2006. pp. 620–656. [Google Scholar]