Abstract
There are few studies about school-environment in relation to pupils' respiratory health, and Korean school-environment has not been characterized. All pupils in 4th grade in 12 selected schools in three urban cities in Korea received a questionnaire (n = 2,453), 96% participated. Gaseous pollutants and ultrafine particles (UFPs) were measured indoors (n = 34) and outdoors (n = 12) during winter, 2004. Indoor dampness at home was investigated by the questionnaire. To evaluate associations between respiratory health and environment, multiple logistic- and multi-level regression models were applied adjusting for potential confounders. The mean age of pupils was 10 yr and 49% were boys. No school had mechanical ventilation and CO2-levels exceeded 1,000 ppm in all except one of the classrooms. The indoor mean concentrations of SO2, NO2, O3 and formaldehyde were 0.6 µg/m3, 19 µg/m3, 8 µg/m3 and 28 µg/m3, respectively. The average level of UFPs was 18,230 pt/cm3 in the classrooms and 16,480 pt/cm3 outdoors. There were positive associations between wheeze and outdoor NO2, and between current asthma and outdoor UFPs. With dampness at home, pupils had more wheeze. In conclusion, outdoor UFPs and even low levels of NO2 may adversely contribute to respiratory health in children. High CO2-levels in classrooms and indoor dampness/mold at home should be reduced.
Keywords: Asthma, Indoor Dampness, Mold Nitrogen Dioxide, Ultrafine Particles
INTRODUCTION
Air pollution exposure in relation to human health is of great concern. Many studies have shown associations between air pollution and decrease in pulmonary function (1), increased mortality (2), and increased prevalence of respiratory symptoms (1, 3). There is a growing concern for effects of inhaled ambient fine/ultrafine particles (UFPs) in relation to especially pulmonary and respiratory diseases (4, 5).
Therefore, research has paid special attention to susceptible persons such as the elderly, children and persons with chronic respiratory diseases. There have been many studies about children's respiratory health effects in relation to the indoor home environment such as dampness (6, 7), nitrogen dioxide (NO2) (8) and formaldehyde (7).
When considering the increase of the prevalence of asthma and respiratory illnesses among children during last decades, the school environment has been pointed out as an important factor besides homes. However, there are still relatively few studies on the school environment in relation to pupils' respiratory health.
Moreover, most of the studies published in Korea have been about association between prevalence of asthma or respiratory symptoms and outdoor air pollution (9-11) such as respirable suspended particulate, sulphur dioxide (SO2), NO2, ozone (O3), carbon monoxide and volatile organic compounds (VOCs). Only a few studies of indoor air pollution have been reported in relation to effects of respiratory symptoms or pulmonary function (9, 10). Moreover, these previous studies have been performed regarding health effects either by only outdoor exposure or among adult population. From these one can not generalize conclusions for children, who are also intensively exposed to the school environment.
The first aim of the present study was to characterize exposure of ambient air pollutions in classrooms and outside of schools in three selected cities in Korea. Secondly, we aimed to evaluate associations between home, indoor and outdoor school environment and pupils' respiratory health.
MATERIALS AND METHODS
Study design
In the year 2004, we performed a school-based cross-sectional study in three urban cities, Guri (GU), Namyangju (NY) and Chunchon (CC), in Korea. City GU (approximately 200,000 inhabitants) is located northeast at the borderline of Seoul, the capital city of Korea whereas NY (approximately 450,000 inhabitants) and CC (approximately 260,000 inhabitants) are located at 40 km and 80 km northeast from Seoul.
In total, twelve schools in the three cities were randomly selected and the school administrators in these schools were contacted and they all agreed to participate: namely, two of 14 schools in GU, six of 38 in NY and four of 43 in CC. None of the schools had previously reported complaints with respect to indoor air quality.
For the current study, we invited all pupils attending 4th grade in the 12 schools for the questionnaire study. For building inspections and indoor measurements, three home classrooms in each school were randomly selected to represent different parts of the buildings.
Questionnaire
The questionnaire contained questions about asthma which included doctor-diagnosed asthma, current asthma medication and/or asthma attacks during the last 12 months. Current asthma was defined as either having current asthma medication or having had an asthma attack during the last 12 months. Moreover, there were questions asking about wheezing or whistling in the chest during the last 12 months. Self-reported atopy was defined as affirmative answer to either allergy to pollen or furry pets. This questionnaire has been used in previous school investigation (12).
In addition to respiratory items, the questionnaire contained questions about current home environment including remodeling and indoor painting or changing floor material during the last 12 months, house age, environmental tobacco smoking (ETS: the frequency was set as 0 = never; 1 = 1-3 times a month; 2 = 1-4 times a week; and 3 = every day) and indoor dampness and mold growth during the last 12 months. Indoor dampness and mold growth was defined as if any of the following four types had been observed within the home during the last 12 months: 1) water leakage or water damage indoors on walls, floors or ceilings; 2) bubbles or yellow discoloration on plastic floor covering or black discoloration of parquet floor; 3) visible mold growth indoors on walls, floor or ceilings; 4) moldy odor indoors except in basement or storage. Subjects reporting one or more signs of dampness are referred to as reporting any sign of indoor dampness and mold growth during the last 12 months.
Finally, there were two questions asking about headache and tiredness in the preceding 3 months with four alternatives for answering as follows: never; 1-3 times a month; 1-4 times a week; and every day. For statistical analysis, the four alternatives were coded as binary (0 = never or 1-3 times a month; 1 = 1-4 times a week or every day).
Building assessments and environmental measurements
Three home-classrooms were randomly selected from each school for the building inspection and environmental measurements which were collected during normal school activities in winter (November-December), 2004. The only exception was two schools, which only had two classrooms and both were included.
The school buildings were inspected and details on construction, materials, type of ventilation system, cleaning routines, amount of open shelves and textiles and number of pupils were noted. The room volume (m3), shelf factor (m/m3), textile factor (m2/m3) and population density (person/m3) were calculated in each classroom. The shelf factor is defined as the length of open shelves divided by the room volume and textile factor as the surface area of fabrics divided by the room volume (13). Temperature (℃), relative air humidity (RH) and concentration of carbon dioxide (CO2) were measured in each classroom during normal activities with closed windows and doors. These factors were measured over time (45-60 min) with Q-Trak™ IAQ Monitor (TSI Incorporated, St Paul, MN, USA), a direct reading instrument with an in-build data logger, by sampling average values over one minute. The instruments were regularly calibrated by Comfort Control, the Swedish service laboratory for TSI equipment. The average concentration for each school was calculated and used in the statistical models.
Sampling of SO2, NO2 and O3 and formaldehyde were performed during a continuous 7-day period for both indoor (n = 34) and outdoor environment (n = 12) using diffusive samplers: sampler for SO2, NO2 and O3 (IVL Swedish Environmental Research Institute Ltd., Gothenburg, Sweden) and sampler for formaldehyde (SKC UME × 100, Eighty Four, PA, USA). Indoor samplers were placed on a wall in each classroom (approximately 1.5 m above the floor) while outdoor samplers were placed inside a plastic box hanging outside a classroom window protected from rain. Both indoor and outdoor ultrafine particles (UFPs) were measured with a P-Trak™ (model 8525 ultrafine particle counter, TSI), measuring particles in the size range of 0.02 to 1 µm.
The samplers for SO2, NO2 and O3 were analyzed by an accredited laboratory (IVL Swedish Environmental Research Institute Ltd.) and the samples for formaldehyde were analyzed by another accredited laboratory (Occupational and Environmental Medicine, University Hospital, Orebro, Sweden).
Statistical analysis
Differences in prevalence were analyzed by chi-square test. Correlations between different exposure variables were tested by Kendall's Tau-beta rank correlation and the results were considered for multicollinearity in further analyses.
For appropriate calculations, we used two different study populations for regression analysis: model a) home and outdoor environment in which all subjects were included whereas model b) indoor environment, the study population was restricted to pupils who participated in both the questionnaire study and belonged to the classrooms where indoor measurements were performed.
In analysis regarding respiratory symptoms, SO2 was excluded due to its very low level. The exposure of NO2, CO2, formaldehyde and temperature were normally distributed. The distribution of O3 and UFPs were right skewed and therefore, base-10 logarithm transformation was applied for normal distribution. Age of school building was categorized into quartiles, namely, 0 = less than or equal to 5 yr; 1 = less than or equal to 10 yr; 2 = less than or equal to 17 yr; and 3 = greater than 17 yr.
For associations between respiratory symptoms and classroom and outdoor exposure, multiple logistic regression models were performed adjusting for potential confounding factors such as age, sex, self-reported atopy and home environmental factors. Each ambient chemical exposure was included in the regression models separately.
Hosmer-Lemeshow goodness-of-fit statistics were used to assess the calibration of the models and all models which met the criteria were presented either in text or table.
Additionally, multi-level logistic regression analysis was conducted to take into account the hierarchical structure of our data. Since the study individuals were nested within schools within cities, three-level (individual-school-city) random intercept logistic regression models were applied. As a first step, a multilevel model without any independent variable (empty model) was conducted to test variance within school-level and within city-level. If the variance by school-level or city-level is larger than zero, then we applied multilevel models including same explanatory variables as in the conventional logistic regression models. In the all models, each chemical exposure variables were separately included. To fit the multi-level logistic regression model, we used generalized linear and latent mixed models (GLLAMM) with the default estimation method as the maximum likelihood with adaptive quadrature in STATA 10.1. Otherwise, all statistical calculations were performed with Statistical Package for Social Sciences (SPSS) for Windows, version 15.0, using two-tailed tests and a 5% level of significance.
Ethics statement
The researchers performing the study had Uppsala University as their affiliation. The study protocol including the questionnaire was reviewed by the Regional Ethical Board of Uppsala, Sweden, and there were no objections against the study (Dnr 2006/210).
RESULTS
Questionnaire data on respiratory symptoms and atopy
Overall, 2,453 pupils in the 12 schools received a questionnaire during November-December, 2004, of which 2,365 (96%) completed it. We excluded 450 subjects for whom key study factor were missing and consequently 1,922 pupils met the inclusion criteria of the current study. Of these 1,028 pupils belonged to the classrooms where indoor measurements were carried out and the response rate among them did not differ from the total population.
The mean age was 10 yr and 49% were boys. Boys reported more doctor-diagnosed asthma (P = 0.01) and current asthma (P < 0.01). The detailed data on respiratory symptoms are shown in Table 1.
Table 1.
Prevalence of self-reported respiratory symptoms, atopy and headache among Korean pupils
*Subjects participated for both questionnaire and belonged to the classrooms where indoor measurements performed; †Difference by sex calculated by chi-square test for four-fold contingency tables; ‡Current asthma medication and/or asthma attacks during the last 12 months; §Allergy to pollen and/or furry pets; ∥One to four times a week or everyday in the preceding 3 months.
Outcomes on school building assessments
The mean age of the school buildings was 11 yr (range 2-30 yr). None of the schools had a mechanical ventilation system. All schools had painted indoor walls and were made of concrete with windows which can be opened. Floors were made of wood (61.8%), unpainted concrete (8.8%) or polyvinyl chloride (PVC) (26.5%) and only one had laminated floor. Classrooms had daily cleaning of floors and desks 1-6 times per week performed by the pupils who go to school 6 days/week.
Indoor and outdoor environment
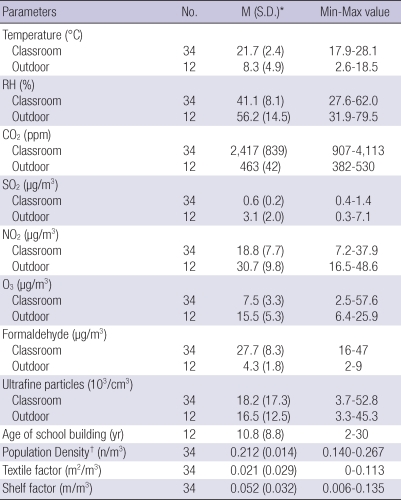
The mean temperature in the 34 classrooms was 21.7℃ and 8.3℃ outdoors (n = 12). RH was 41% indoors and 56% outdoors. Indoor mean concentration of CO2 was 2,417 ppm and maximum CO2 level was 4,113 ppm (Table 2). The levels of SO2, NO2, O3 and formaldehyde were lower than Air Quality Guidelines (AQG) by World Health Organization (WHO) (14, 15). According to AQG, the following values are recommended; SO2 at 20 µg/m3 for 24 hr mean, NO2 at 40 µg/m3 for annual mean, O3 at 100 µg/m3 for daily maximum 8-hr mean and formaldehyde at 100 µg/m3 for a 30-min average. The mean level of UFPs was 18,230 pt/cm3 in the classrooms while it was 16,480 pt/cm3 outdoors. The mean levels of indoor NO2 in city GU, NY and CC were 20.5, 21.6 and 13.8 µg/m3, and the mean levels of indoor O3 were 7.3, 8.5 and 4.6 µg/m3, respectively. The mean levels of indoor formaldehyde in city GU, NY and CC were 28.2, 29.0 and 22.5 µg/m3, and the mean levels of indoor UFPs were 18,140, 21,397 and 16,010 pt/cm3, respectively. The mean levels of indoor SO2 were not varied among the cities.
Table 2.
Indoor/Outdoor climate and airborne pollutants in 12 Korean schools
*Arithmetic mean with standard deviation; †Number of students/room volume. RH, relative humidity.
Age of school-building was positively correlated with indoor temperature (Tau beta = 0.49; P < 0.001) whereas negatively associated with RH (Tau beta = -0.52; P < 0.001) and formaldehyde (Tau beta = -0.41; P < 0.001). In addition, indoor temperature was negatively associated with RH (Tau beta = -0.41; P < 0.001). Shelf factor was not correlated with any indoor factors. Textile factor was calculated, but it was not tested for correlation since it was low in Korean schools. Among outdoor environmental factors, there was no significant correlation between any ambient pollutants except a negative correlation between formaldehyde and O3 (Tau beta = -0.626; P = 0.008).
Home environment and its association to respiratory symptoms
The mean age of home building was 7 yr and it was categorized into quartiles for further analyses (0 = less than or equal to 3 yr; 1 = less than or equal to 6 yr; 2 = less than or equal to 10 yr; and 3 = greater than 10 yr). Remodeling and indoor painting during the last 12 months was reported by 11.5%, changing floor during the last 12 months by 18.9% and indoor dampness and mold growth during the last 12 months by 21.9% (water damage 12.1%, floor bubbling 0.8%, visible mold growth 11.8% and moldy odor 4.0%). The frequency of ETS was reported as follows: never = 50%; 1-3 times a month = 11.5%; 1-4 times a week = 18.1%; and every day = 20.5%.
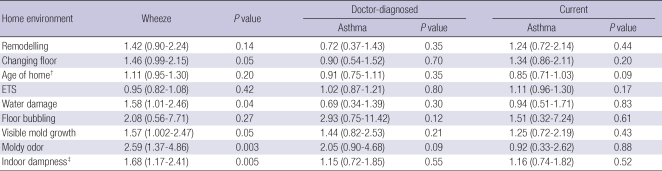
In all subjects (n = 1,915) who completed questionnaire, associations between respiratory symptoms and selected home environment were studied with adjustment for age, sex and self-reported furry pet or pollen allergy. We found consistent associations between wheeze and problems related to indoor dampness such as water damage (odds ratio [OR] 1.58, 95% confidence interval [CI] 1.01-2.46), visible mold growth (OR 1.57, 95% CI 1.00-2.47) and moldy odor (OR 2.59, 95% CI 1.37-4.86) during the last 12 months (Table 3). In addition, there was a marginal association between wheeze and changing floor during the last 12 months (OR 1.46, 95% CI 0.99-2.15, P = 0.053). Unexpectedly, we found no association between asthma and wheeze, and exposure to ETS.
Table 3.
Association between wheeze and asthma and home environment*
*Each exposure was separately included in multiple logistic regression model with adjustment for age, sex and self-reported furry pet or pollen allergy (n = 1,915); †Continuous variable was categorized into quartiles (0 = less than or equal to 3 yr; 1 = less than or equal to 6 yr; 2 = less than or equal to 10 yr; and 3 = greater than 10 yr); ‡Water damage, floor bubbling, visible mold growth or moldy odor during the last 12 months. ETS, environmental tobacco smoke.
As observed, there were consistent associations between wheeze and selected home environmental factors, and we therefore included these factors as covariates when analyzing effects on respiratory health in relation to classroom and outdoor environments.
Association between respiratory symptoms and classroom and outdoor environment
We studied associations between respiratory symptoms and outdoor ambient pollutants in all study populations (n = 1,915) adjusting for age, sex, self-reported furry pet or pollen allergy and selected home environment factors mentioned above. Regarding analysis of classroom environment, we applied the same models but in the restricted study population (n = 1,028) (See details in Method).
There was an association between wheeze and outdoor level of NO2 (OR 1.27, 95% CI 1.06-1.53) and a similar tendency on wheeze regarding classroom level of NO2 (P = 0.07) (Table 4). In contrast, we observed a negative association between wheeze and outdoor O3 (OR 0.21, 95% CI 0.08-0.5). At increased levels of outdoor UFPs, pupils reported more current asthma (OR 1.93, 95% CI 1.08-3.46). However, none of these associations were found regarding classroom ambient exposure. Although CO2 levels in the classrooms were much higher than the recommended level of 1,000 ppm, pupils reported slightly more wheeze (OR 1.03, 95% CI 1.001-1.06) but not for other health related problems such as headache (OR 1.00, 95% CI 0.97-1.02) and tiredness (OR 1.01, 95% CI 1.00-1.03). Moreover, none of respiratory symptoms had an association with age of school-building (data not shown).
Table 4.
Association between wheeze and asthma, and classroom- and outdoor environment*
*Each exposure was separately included in multiple logistic regression model with adjustment for age, sex, self-reported furry pet or pollen allergy and home environment (remodelling, changing floor, age of home building, environmental tobacco smoke and indoor dampness); †Analysis was applied in all population who completed a questionnaire (n = 1,915); ‡Odds ratio expressed as change of coefficient per 10 µg/m3; §Odds ratio expressed as change of coefficient by base-10 logarithm transformation for O3 (µg/m3) and ultrafine particles (pt/m3); ∥Analysis was restricted in subjects who belonged to the classroom where indoor measurements were performed (n = 1,028); ¶Odds ratio expressed as change of coefficient per 102 ppm.
With regard to the nested structure of data, we applied multilevel (individual-school-city) analyzes and there were generally low level of random variance of school-level and city-level (random variance < 0.001). In the empty model regarding wheeze, school-level random variance (standard error, SE) was 0.196 (0.128) and the model regarding current asthma, school-level random variance with SE was 0.011 (0.055). As we expected with regard to their low random variances of school and city level, the associations between wheeze/current asthma and the ambient exposures in the multilevel models remained same as the results by the conventional multiple regression models. In brief, there was still negative association between wheeze and outdoor O3 (OR 0.20, 95% CI 0.04-0.98, school-level random variance 0.106 (SE 0.091) and city-level random variance < 0.001). Pupils reported more current asthma at the increased level of outdoor UFPs (OR 1.93, 95% CI 1.08-3.45, school-level and city-level random variance < 0.001). The association between wheeze and outdoor level of NO2 was not statistically significant but had a similar tendency (OR 1.26, 95% CI 0.93-1.70, school-level random variance 0.132 (SE 0.102) and city-level random variance < 0.001).
DISCUSSION
Airborne chemical exposure in classrooms and outdoor environment were characterized and the association with the prevalence of respiratory symptoms among schoolchildren was evaluated. The main finding was that at increased outdoor NO2 levels, pupils reported more wheeze even though the levels of NO2 were not relatively high. Moreover, pupils reported more current asthma at increased levels of outdoor UFPs. Furthermore, there were consistent associations between wheeze and the problem of indoor dampness and mold growth at home.
For the current study, schools in three selected cities were randomly selected. Questionnaires were distributed before any sampling, so that study subjects were not aware of any measurements. The response rate was high (96%). We have no information about non-responders, but there were similar proportion of boys and girls. The questions on respiratory symptoms, asthma or self-reported atopy have been used in other epidemiological studies and some validation studies have been performed (16).
Prevalence of wheeze was reported by 8.0% which is similar to previous Korean studies (17, 18). In the current study, prevalence of doctor-diagnosed asthma and current asthma was reported by 5.3% and 6.0%, respectively. The prevalence of doctor-diagnosed asthma in our study was in agreement with a previous study performed in the year 2000 (19). However, the prevalence of current asthma in our study was slightly higher than in previous studies (18, 20). One of them carried out in rural areas during 1994-1995, reported a prevalence rate for current asthma by 2.2% and another national study in 1995 showed that current asthma was 3.2%. The difference in prevalence of current asthma to our study may be due to almost 10-yr time interval and different regional selection. Prevalence of furry pet allergy was reported by 6.0% and pollen allergy by 4.0%. The prevalence of pollen allergy was similar to a previous Korean study in which allergy was verified by skin prick test (17). The same study reported cat allergy as high as 20.4%, but presented no data on other furry pet allergies.
Home environmental factors were assessed by questions in the same questionnaire and we found consistent associations between wheeze and home dampness such as water damage, visible mold growth and moldy odor. This finding is in agreement with many previous studies (6, 21). The associations between dampness/mould at home and wheeze could either be related house dust mite exposure, mold exposure or chemical exposure related to dampness. One previous study including various parts of Korea reported that the house dust mite D. farinae was found in 20.6% and D. pteronyssinus in 6.5% of homes (22). Also, we previously reported the levels of dust mite allergen (D. farinae and D. pteronyssinus) from the same schools included for the current study and D. farinae was detected in 62% of the classrooms but rather low levels (23). We thus speculate that one factor related to dampness at home can be house dust mite allergens. Unexpectedly, we found no significant association between pupils' respiratory health and ETS at home. Approximately 70% of our study subjects are living in an apartment complex where most of those buildings are built with glassed-in balcony with a closable door. Concerning these building structures, there may be some of responders who considered the glassed-in balcony as indoors, although the door for balcony may be closed during smoking process. Thus, it may result in some extent underestimation of ETS.
In our study, we measured SO2, NO2 and O3 during a continuous 7-day period in winter season. The relatively short measurement period can contribute to some limitation regarding their association to respiratory symptoms in the preceding year. When we additionally compared our outdoor pollutants (SO2, NO2 and O3) levels with the annual levels reported by Korean governmental air quality data obtained from the official home page of Gyeonggi-do and Gangwon-do, most of the levels of the pollutants in our study were lower than the levels in the annual reports, especially SO2. Even if climatological or seasonal variation may modify the absolute level of outdoor pollutants, the relative levels can be more constant. This assumption is supported but the fact that the relative levels between the areas agreed between our study and the monitoring stations. The difference of the levels can be due to not only seasonal variance but also the different location for the measurements. We measured all samples right outside of the school buildings whereas the annual reported data may include even heavy-traffic area.
To depict accurate overall exposure to schoolchildren, however, there need either dispersion modeling or repeated environmental monitoring, especially from the place where school zone is located. To our knowledge, this is the first study on Korean school environment (both classrooms and school outdoors) in relation to health effects among schoolchildren and the first epidemiological study on pupils' respiratory health regarding exposure of ultrafine particles in schools. Our study is not aiming to calculate attributable fraction for different risk factors for childhood asthma. However, we have controlled for factors in the home environment, in order to isolate the effect of the school environment, to avoid general socio-economic effects related to both school and home environment in certain areas. The issue on respiratory infections is complicated, and was not studied here. It is known that severe respiratory infections in early childhood can be associated with asthma in adulthood, and some viral infections in schoolchildren could trigger asthma development, but the association could partly be due to increased infection proneness in those with heredity for asthma. We speculate that environmental factors can increase susceptibility to infections, and crowdedness or poor ventilation at school (or at home) can increase the exposure to airborne pathogens.
The mean indoor levels of CO2 exceeded 1,000 ppm, the ASHRAE standard (24) in all except one of the classrooms. High levels of CO2 in classrooms during winter season were previously observed in a study by Sohn and co-workers (mean level of CO2 = 1,271 ppm; max. value = 3,000 ppm) (25). The levels of NO2 in our study were lower than two previous Korean studies: one in dwellings (64 µg/m3) (26) and another one in a shoe stall near a heavy-traffic roadside (108 µg/m3) (9). However, these previous studies can not be compared with our study since these environments are distinguished from school environment. The level of formaldehyde was higher in the classrooms than outdoors (mean indoor/outdoor ratio 7.2, SD 3.1), which may mainly be originated from indoor sources. The study by Sohn and coworkers also reported the level of formaldehyde in classrooms during winter and these levels were three times higher than in our study (mean level 86 µg/m3 vs 28 µg/m3) (25). The difference in formaldehyde level to our study can be explained by the fact that in the study by Sohn and co-workers the majority of schools investigated had recently been renovated and/or reconstructed.
There are only a limited number of studies measuring UFP in school classrooms. The mean value of UFP counts in our study (18,000 pt/cm3) was similar to a previous study conducted in 11 classrooms in Athens, Greece (24,000 pt/cm3) (27) but much higher compared with a study in the rural parts of Canada (5,017 pt/cm3) (28). The levels of ambient pollutants in our study may not represent all school environments in Korea since there are several cities such as Seoul, with even heavier traffic density.
Although most of the levels of CO2 in the classrooms exceeded 1,000 ppm, we found relatively small effect on wheeze but not for other health problems, e.g., headache. In the present study, we could not find any significant association between exposure of formaldehyde from both indoor and outdoor environment and respiratory symptoms. This could be explained by the low levels of formaldehyde both in classrooms and outdoor, which were below of WHO AQG (15).
In the current study, pupils reported more wheeze at increased outdoor level of NO2 and the result was consistent in different statistical models. Previous studies showed that NO2 can be a risk factor for respiratory health among children (8, 29). In contrast, we found negative association between outdoor O3 and wheeze. The negative association between O3 and respiratory symptoms was previously observed in a study of the Shanghai schools (29). One possible explanation could be reactive characteristic of O3. Ozone concentrations are often low in heavy traffic urban area where nitric oxide (NO) is abundant since O3 reacts with NO resulting in formation of NO2. In our study, the levels of O3 were well below of WHO AQG (14) but we found no associations between NO2 and O3. It is also well known that particles consume O3, but we did not measure PM10 or PM2.5 but only UFP. Moreover, smog is formed from VOCs and O3, when O3 is consumed and irritative compounds are formed. We thus can only speculate on the negative association between O3 and wheeze that could be due to secondary pollutants e.g. higher PM levels or formation of smog, when O3 is consumed.
We found association between current asthma and outdoor UFPs. Several previous studies reported an adverse effect of UFPs on pulmonary and respiratory health (4, 5) since UFPs can promote the formation of reactive oxygen species and contribute to oxidative stress and inflammatory process in the lungs (30). In addition, one review study by Weichenthal and co-workers concluded that UFPs toxicity may contribute to exacerbation of asthma symptoms in susceptible individuals (5). However, we could not observe a similar finding regarding indoor UFPs although indoor/outdoor UFPs ratio had value of 1.7, indicating more emission from indoor sources. One possible explanation can be the toxicity of outdoor UFPs may be differed from UFPs emitted from indoor sources since UFPs can be significantly enhanced by gaseous co-pollutants and compose of variance kinds of toxic chemicals (5).
In conclusion, our study suggests that even low levels of NO2 may contribute to adverse respiratory health among schoolchildren. Ultrafine particles in outdoor environment may adversely affect pupils' respiratory health. Moreover, mechanical ventilation systems need to be considered in Korean schools to reduce CO2 levels to fulfill ventilation standards. Furthermore, problems of home dampness/mold should be considered in relation to pupils' respiratory health.
ACKNOWLEDGMENTS
We are extremely grateful to all the pupils and their parents who took part and to the administrators in the schools for their cooperation.
AUTHOR SUMMARY
Respiratory Health among Korean Pupils in Relation to Home, School and Outdoor Environment
Jeong-Lim Kim, Lena Elfman, Gunilla Wieslander, Martin Ferm, Kjell Torén, and Dan Norbäck
The factors of school-environment influencing the pupils' respiratory health are not adequately reported in Korea. All pupils in 4th grade in 12 selected schools in Korea received a questionnaire (N = 2,453). Gaseous pollutants and ultrafine particles (UFPs) were measured indoors and outdoors during winter, 2004. Indoor dampness at home was investigated by questionnaire. Multiple logistic- and multilevel regression models were applied adjusting for confounders. No school had mechanical ventilation and most indoor CO2-levels exceeded 1,000 ppm. The indoor mean concentrations of SO2, NO2, O3 and formaldehyde were measured. The average level of UFPs was similar between indoors and outdoors, 18,230 pt/cm3 and 16,480 pt/cm3, respectively. There were positive associations between wheeze, a representative symptom of asthma, and outdoor NO2, and between current asthma and outdoor UFPs. With dampness at home, pupils had more wheeze. In conclusion, outdoor UFPs and even low NO2 level may adversely contribute to respiratory health. High CO2-levels in classrooms and indoor dampness at home should be reduced.
References
- 1.Nordling E, Berglind N, Melén E, Emenius G, Hallberg J, Nyberg F, Pershagen G, Svartengren M, Wickman M, Bellander T. Traffic-related air pollution and childhood respiratory symptoms, function and allergies. Epidemiology. 2008;19:401–408. doi: 10.1097/EDE.0b013e31816a1ce3. [DOI] [PubMed] [Google Scholar]
- 2.Yorifuji T, Kashima S, Tsuda T, Takao S, Suzuki E, Doi H, Sugiyama M, Ishikawa-Takata K, Ohta T. Long-term exposure to traffic-related air pollution and mortality in Shizuoka, Japan. Occup Environ Med. 2010;67:111–117. doi: 10.1136/oem.2008.045542. [DOI] [PubMed] [Google Scholar]
- 3.Andersen ZJ, Loft S, Ketzel M, Stage M, Scheike T, Hermansen MN, Bisgaard H. Ambient air pollution triggers wheezing symptoms in infants. Thorax. 2008;63:710–716. doi: 10.1136/thx.2007.085480. [DOI] [PubMed] [Google Scholar]
- 4.Penn A, Murphy G, Barker S, Henk W, Penn L. Combustion-derived ultrafine particles transport organic toxicants to target respiratory cells. Environ Health Perspect. 2005;113:956–963. doi: 10.1289/ehp.7661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weichenthal S, Dufresne A, Infante-Rivard C. Indoor ultrafine particles and childhood asthma: exploring a potential public health concern. Indoor Air. 2007;17:81–91. doi: 10.1111/j.1600-0668.2006.00446.x. [DOI] [PubMed] [Google Scholar]
- 6.Bornehag CG, Sundell J, Hagerhed-Engman L, Sigsggard T, Janson S, Aberg N DBH Study Group. 'Dampness' at home and its association with airway, nose, and skin symptoms among 10,851 preschool children in Sweden: a cross-sectional study. Indoor Air. 2005;15(Suppl 10):48–55. doi: 10.1111/j.1600-0668.2005.00306.x. [DOI] [PubMed] [Google Scholar]
- 7.Venn AJ, Cooper M, Antoniak M, Laughlin C, Britton J, Lewis SA. Effects of volatile organic compounds, damp, and other environmental exposures in the home on wheezing illness in children. Thorax. 2003;58:955–960. doi: 10.1136/thorax.58.11.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belanger K, Gent JF, Triche EW, Bracken MB, Leaderer BP. Association of indoor nitrogen dioxide exposure with respiratory symptoms in children with asthma. Am J Respir Crit Care Med. 2006;173:297–303. doi: 10.1164/rccm.200408-1123OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bae H, Yang W, Chung M. Indoor and outdoor concentrations of RSP, NO2 and selected volatile organic compounds at 32 shoe stalls located near busy roadways in Seoul, Korea. Sci Total Environ. 2004;323:99–105. doi: 10.1016/j.scitotenv.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 10.Hong YC, Leem JH, Lee KH, Park DH, Jang JY, Kim ST, Ha EH. Exposure to air pollution and pulmonary function in university students. Int Arch Occup Environ Health. 2005;78:132–138. doi: 10.1007/s00420-004-0554-x. [DOI] [PubMed] [Google Scholar]
- 11.Lee JT, Kim H, Song H, Hong YC, Cho YS, Shin SY, Hyun YJ, Kim YS. Air pollution and asthma among children in Seoul, Korea. Epidemiology. 2002;13:481–484. doi: 10.1097/00001648-200207000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Kim JL, Elfman L, Mi Y, Johansson M, Smedje G, Norbäck D. Current asthma and respiratory symptoms among pupils in relation to dietary factors and allergens in the school environment. Indoor Air. 2005;15:170–182. doi: 10.1111/j.1600-0668.2005.00334.x. [DOI] [PubMed] [Google Scholar]
- 13.Skov P, Valbjørn O, Pedersen BV The Danish Indoor Climate Study Group. Influence of indoor climate on the sick building syndrome in an office environment. Scand J Work Environ Health. 1990;16:363–371. doi: 10.5271/sjweh.1772. [DOI] [PubMed] [Google Scholar]
- 14.Air quality guidelines global update. Report on a working group metting, Bonn, Germany, 18-20 October, 2005. World Health Organization. [accessed on 21 Dec 2009]. Available at http://www.euro.who.int/__data/assets/pdf_file/0005/78638/E90038.pdf.
- 15.Air quality guidelines for Europe: Second edition Cophenhagen, 2000. WHO regional office for Europe. [accessed on 21 Dec 2009]. Available at http://www.euro.who.int/__data/assets/pdf_file/0005/74732/E71922.pdf.
- 16.Braun-Fahrländer C, Wüthrich B, Gassner M, Grize L, Sennhauser FH, Varonier HS, Vuille JC. Validation of a rhinitis symptom questionnaire (ISAAC core questions) in a population of Swiss school children visiting the school health services. SCARPOL-team. Swiss Study on Childhood Allergy and Respiratory Symptom with respect to Air Pollution and Climate. International Study of Asthma and Allergies in Childhood. Pediatr Allergy Immunol. 1997;8:75–82. doi: 10.1111/j.1399-3038.1997.tb00147.x. [DOI] [PubMed] [Google Scholar]
- 17.Kim YY, Cho SH, Kim WK, Park JK, Song SH, Kim YK, Jee YK, Ha MN, Ahn YO, Lee SI, Min KU. Prevalence of childhood asthma based on questionnaires and methacholine bronchial provocation test in Korea. Clin Exp Allergy. 1997;27:761–768. doi: 10.1046/j.1365-2222.1997.710839.x. [DOI] [PubMed] [Google Scholar]
- 18.Lee SI, Shin MH, Lee HB, Lee JS, Son BK, Koh YY, Kim KE, Ahn YO. Prevalences of symptoms of asthma and other allergic diseases in Korean children: a nationwide questionnaire survey. J Korean Med Sci. 2001;16:155–164. doi: 10.3346/jkms.2001.16.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong SJ, Lee MS, Sohn MH, Shim JY, Han YS, Park KS, Ahn YM, Son BK, Lee HB Korean ISAAC Study Group. Self-reported prevalence and risk factors of asthma among Korean adolescents: 5-year follow-up study, 1995-2000. Clin Exp Allergy. 2004;34:1556–1562. doi: 10.1111/j.1365-2222.2004.02084.x. [DOI] [PubMed] [Google Scholar]
- 20.Lee JG, Moon HJ, Kim KS, Yoon JH, Kim SS, Park IY. Epidemiological study for allergic disease of school aged children and adolescence in rural area of Korea. Korean J Otolaryngol-Head Neck Surg. 1998;41:1156–1163. [Google Scholar]
- 21.Hagmolen of Ten Have W, van den Berg NJ, van der Palen J, van Aalderen WM, Bindels PJ. Residential exposure to mould and dampness is associated with adverse respiratory health. Clin Exp Allergy. 2007;37:1827–1832. doi: 10.1111/j.1365-2222.2007.02841.x. [DOI] [PubMed] [Google Scholar]
- 22.Ree HI, Jeon SH, Lee IY, Hong CS, Lee DK. Fauna and geographical distribution of house dust mites in Korea. Korean J Parasitol. 1997;35:9–17. doi: 10.3347/kjp.1997.35.1.9. [DOI] [PubMed] [Google Scholar]
- 23.Kim JL, Elfman L, Norbäck D. Respiratory symptoms, asthma and allergen levels in schools--comparison between Korea and Sweden. Indoor Air. 2007;17:122–129. doi: 10.1111/j.1600-0668.2006.00460.x. [DOI] [PubMed] [Google Scholar]
- 24.ASHRAE. Ventilation for acceptable indoor air quality. ASHRAE-Standard 62-1989. Atlanta: American Society of Heating, Refrigerating and Air-Conditioning Engineers, INC; 1989. [Google Scholar]
- 25.Sohn J, Yang W, Kim J, Son B, Park J. Indoor air quality investigation according to age of the school buildings in Korea. J Environ Manage. 2009;90:348–354. doi: 10.1016/j.jenvman.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Yang W, Lee K, Chung M. Characterization of indoor air quality using multiple measurements of nitrogen dioxide. Indoor Air. 2004;14:105–111. doi: 10.1046/j.1600-0668.2003.00216.x. [DOI] [PubMed] [Google Scholar]
- 27.Diapouli E, Chaloulakou A, Mihalopoulos N, Spyrellis N. Indoor and outdoor PM mass and number concentrations at schools in the Athens area. Environ Monit Assess. 2008;136:13–20. doi: 10.1007/s10661-007-9724-0. [DOI] [PubMed] [Google Scholar]
- 28.Weichenthal S, Dufresne A, Infante-Rivard C, Joseph L. Characterizing and predicting ultrafine particle counts in Canadian classrooms during the winter months: model development and evaluation. Environ Res. 2008;106:349–360. doi: 10.1016/j.envres.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 29.Mi YH, Norbäck D, Tao J, Mi YL, Ferm M. Current asthma and respiratory symptoms among pupils in Shanghai, China: influence of building ventilation, nitrogen dioxide, ozone, and formaldehyde in classrooms. Indoor Air. 2006;16:454–464. doi: 10.1111/j.1600-0668.2006.00439.x. [DOI] [PubMed] [Google Scholar]
- 30.Dick CA, Brown DM, Donaldson K, Stone V. The role of free radicals in the toxic and inflammatory effects of four different ultrafine particle types. Inhal Toxicol. 2003;15:39–52. doi: 10.1080/08958370304454. [DOI] [PubMed] [Google Scholar]