Abstract
The morbidity of travelers' diarrhea (TD) is still high. This study examined the incidence of common pathogens and characteristics of TD among Korean travelers who visited South-East Asian countries. We performed a prospective study involving 479 Korean travelers with diarrheal disease from February 2009 to April 2009 and stool samples were examined and questionnaire surveys were done after arrival. Enterotoxigenic Escherichia coli (ETEC) was found in 36.0% of TD cases, as were the following: Enteroaggregative Escherichia coli (EAEC) in 27.0%, Vibrio parahaemolyticus in 13.1%, and Norovirus in 11.5%. The detected rate of classic TD was higher in men (P = 0.007), in patients who had a shorter duration trip (P = 0.023) and in patients who drank more than 1 liter of water per day (P = 0.037). Positive stool culture rates were higher in men (P = 0.005), in hospitalized patients (P = 0.013). and in those who consumed impure water or raw foods (P = 0.033). A higher severity of disease corresponded to a significantly higher culture positivity rate (P = 0.029). We should consider the possibility of other pathogens in addition to ETEC in patients with TD who visit South-East Asia. Travelers need to educate about risk factors associated with TD.
Keywords: Travelers' Diarrhea, Enterotoxigenic Escherichia coli, Enteroaggregative Escherichia coli, Vibrio parahaemolyticus, Norovirus
INTRODUCTION
Travelers' diarrhea (TD) is an important health issue among travelers of developed countries who visit developing countries and tropical areas. Morbidity rates of TD have been reported up to 55% by travelers; but there is no exact report from each country in the world (1-3). Although travelers' diarrhea is self-limiting and is usually spontaneously cured within a few days, it can hinder a planned business or pleasure trip. Enterotoxigenic Escherichia coli (ETEC) is the most common cause of TD worldwide (2, 4, 5), while the distribution of other pathogens is different. Even though many studies on the prevalence and etiology of TD have been done, little is known about which pathogens are most common in the South-East Asian countries popular with tourists. With the recent increases in Korean travelers visiting South-East Asian countries, TD is increasing in Korea, and the morbidity of TD is still high. This study was undertaken to analyze risk factors among South-East Asia travelers returning to Korea and reports on the epidemiology of TD. Our results contribute to reducing health risks for travelers and decreasing the burden on the Korean public health system.
MATERIALS AND METHODS
Study population
This study was prospectively conducted on Korean travelers who reported diarrhea when returning from South-East Asia to Incheon International Airport of Korea from February to April 2009. The quarantine officers at the Airport collected stool samples by rectal swab and demographic data of the reported travelers. We excluded travelers from analysis, those with underlying gastrointestinal diseases (inflammatory bowel disease, irritable bowel syndrome, and operation history of gastrointestinal tract), previous diarrhea before travel, children less than 10 yr old who were unable to properly explain symptoms and medical history, and travelers who stayed longer than 12 months due to possible increased immunity (6).
Case definition
Classic diarrhea was defined as passage of more than 3 unformed stools in 24 hr, plus the development of more than one symptom of enteric infection (fever, abdominal pain or cramps, increased intestinal gas, nausea, vomiting, and passage of bloody stools) (7). Moderate diarrhea was defined as passage of 1 or 2 unformed stools with more than one additional enteric symptom or more than 2 unformed stools without additional symptoms. Mild disease was defined as passage of 1 or 2 unformed stools without enteric symptoms.
Bacterial and viral isolation
A rectal swab taken from the diarrheal patient was suspended 1 mL Phosohate-buffered saline (PBS), and 100 µL of this suspension was inoculated into 5 mL of Tryptic soy broth (TSB) (Difco, Detroit, USA), 5 mL of alkaline peptone water (APW) (Difco) or 5 mL of Preston broth (Oxoid, Cambridge, UK), respectively. To amplify Vibrio species, inoculated APW was incubated at 37℃ for 6 to 8 hr. After incubation, the culture was inoculated on to thiosulfate citrate bile sucrose (TCBS) (Difco) agar plate, and growth was further tested for biochemical identification. Existence of Escherichia coli, Salmonella species, and Shigella species was confirmed by polymerase chain reaction (PCR). The TSB culture of the PCR positive samples was plated onto MacConkey agar (Difco) and cultured at 37℃ for 15 to 18 hr. After incubation, colonies suspected as Salmonella or Shigella species were subcultured to Tryptic soy agar (TSA) (Difco) and biochemically identified by using the VITEK system with the VITEK GNI+ card (Biomerieux, St. Louis, MO, USA). Preston broth incubated at 37℃ for 6 to 8 hr was used to amplify Campylobacter species. After amplification, the culture was spread onto a mCCDA agar plate (Oxoid) and cultured at 42℃ for 2 or 3 days with 5% O2, 10% CO2, and 85% N2; positive colonies were identified using an API Campy kit (Biomerieux).
Viral RNA was extracted using a magnetic bead separator (Tecan, Männedorf, Switzerland) with reagents provided in the GM AUTOPREP® Viral Nucleic Acid prep kit (Greenmate Co., Seoul, Korea) according to the manufacturer's protocol. Norovirus was detected by one step reverse transcription-PCR (RT-PCR) and seminested PCR with specific primers that target the junction between ORF1 and ORF2 as previously described (8).
Questionnaire
A structured questionnaire included personal information, medical history, travel history, clinical symptoms, and eating and drinking history.
Statistical analysis
We described the proportional data according to their characteristics and analyzed the categorical variables using a chi-square test. Continuous variables were compared with a Kruskal-Wallis test in accordance with the classification of travelers' diarrhea or detection results. A P value of < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS software, version 10.0 (Chicago, IL, USA, Korean version. KCDC licensed).
Ethics statement
The Korea Centers for Disease Control and Prevention (KCDC) reviewed the protocols. And the institutional review board of the KCDC approved the protocol (approval number 2009-I14).
RESULTS
During the study period, 707,150 passengers returned to Incheon International Airport after visiting South-East Asian countries. Of them, 1,484 travelers reported symptom of diarrhea to the quarantine officers. Among them, 479 travelers agreed to perform rectal swab and 338 travelers submitted the structured questionnaires to the quarantine officers.
Patient characteristics and clinical features
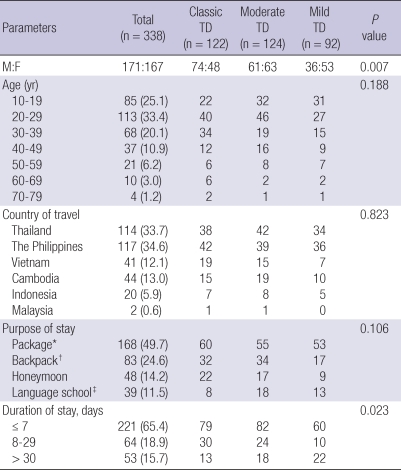
Of the 338 travelers with diarrhea who answered the questionnaire form, 122 (36.1%) patients were classic TD, 124 (36.7%) were moderate TD, and 92 (27.2%) were mild TD. The median age of patients was 27 yr (range 19.5-37.5 yr). The proportion of males was 50.6% (171 out of 338). The patients most commonly had returned Korea after package travel and had stayed less than 7 days (Table 1). On average, diarrhea occurred on the 4th day after arrival in the tour area. Of 388 travelers with TD, 114 (33.7%) had visited Thailand, 117 (34.6%) the Philippines, and 41 (12.1%) Vietnam. The patients manifested various enteric symptoms: 144 (42.6%) had abdominal pain and/or cramping, 67 (19.8%) had nausea and 35 (10.4%) had vomiting.
Table 1.
Demographic characteristics of Korean travelers with diarrhea returned from South-East Asian countries
Note. Data are no. (%) of patients. *Travel planned by tour company with regular schedule in residence of one hotel; †Travel without regular schedule and resident place; ‡Resident in one place. M, male; F, female; NS, not significant.
Factors related to the severity of diarrhea and clinical statuses according to TD classification are shown in Tables 1, 2. The rate of classic TD was significantly higher in men and that of mild TD was relatively lower (P = 0.007). A shorter stay in a country resulted in a higher classic TD rate (P = 0.023). Travelers who drank water, regardless of whether it was pure water or tap water, who drank more than 1 liter per day (P = 0.037) and who ate raw seafood tended to have more severe TD (P = 0.015). If foods suspicious for infection were known, the rates of classic and moderate TD were higher than mild (P = 0.000). In the severe TD class, more patients visited the outpatient department (OPD) (P = 0.001), were hospitalized (P = 0.004), and had detectable pathogens (P = 0.029). However, age and the purpose of stay were not significantly different in connection with the classification level of TD (P = 0.188 and P = 0.106).
Table 2.
Clinical features of travelers' diarrhea in Koreans from South-East Asian countries
Note. Data are no. (%) of patients. *Suspicious foods included impure water and raw foods. NS, not significant; OPD, outpatient department.
Isolated pathogens
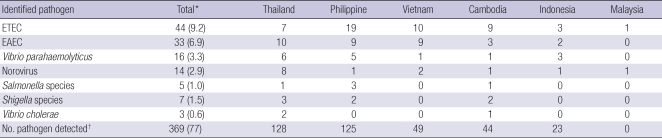
The detection rate of diarrheal pathogens was 23.0% (110/479) based on the rectal swab method. A total of 122 bacterial and viral pathogens were identified. Ten cases had 2 different pathogens and 1 case had 3 different pathogens. The distribution of etiologic agents from the 479 patients that were enrolled is shown in Table 3. ETEC was the most commonly identified pathogen (44 cases, 36.0%), followed by Enteroaggregative Escherichia coli (EAEC) (33 cases, 27.0%), Vibrio parahaemolyticus (16 cases, 13.1%), and Norovirus (14 cases, 11.5%). Also there were small number of Salmonella species (5 cases, 1.0%), Shigella species (7 cases, 1.5%) and Vibrio cholerae (3 cases, 0.6%).
Table 3.
Enteric pathogens identified in Korean travelers with diarrhea from South-East Asian countries
Note. Data are no. (%) of patients. *Mixed cases were scattered. (10 cases were mixed with 2 pathogens, 1 case with 3 pathogens), so total % can exceed 100; †No pathogen indicates cases of travelers' diarrhea with a non-identified etiologic agent. ETEC, Enterotoxigenic Escherichia coli; EAEC, Enteroaggregative Escherichia coli.
DISCUSSION
The incidence rate of TD in South-East Asia was reported too high (9, 10), and the number of tourist becoming infected is increasing. However, recent reports on TD are not enough when it comes to South-East Asia, the most populated region over the world. This study was important for evaluating the current situation even though there were limitations. In this study, EAEC (27.0%), Vibrio parahaemolyticus (13.1%) and Norovirus (11.5%) were found important pathogens in Korean patients with TD returning from South-East Asia. To our knowledge, ETEC is the most commonly found TD pathogen worldwide, while EAEC, Vibrio parahaemolyticus and Norovirus have been reported less frequently (4, 5, 11, 12). Some reports have described intestinal protozoa such as Giardia lamblia, Entamoeba histolytica, Cyclospora species and Cryptosporidium species as pathogens in 0%-17% of cases of TD (13-16). However, infection of protozoa was not included in this study. EAEC has been implicated as an etiologic agent of persistent diarrhea among children in developing countries (17), and patients with AIDS-associated chronic diarrhea (18). However, while EAEC has been reported as a cause of TD in some regions of the world since 1985 (19-21), there is insufficient data from South-East Asia.
Vibrio parahaemolyticus is frequently isolated from a variety of raw and undercooked sea foods such as shellfish and sushi. Because of the food culture of eating raw fish in South-East Asia, V. parahaemolyticus food poisoning is more common in South-East Asia than in western countries (22). In 1986, the incidence of V. parahaemolyticus in Thailand and Bangladesh was reported to be 13% of all TD cases (23), which is similar to the TD rates of other South-East Asian countries studied. In this study, there was no significant relationship between a history of raw seafood ingestion and the severity of diarrhea; because of the small scale, we were unable to confirm a relationship with V. parahaemolyticus. Nevertheless, we need to consider that V. parahaemolyticus infection in conjunction with E. coli species could be causing the diarrhea in patients from South-East Asia. More studies with large number should be performed.
Norovirus has been recognized as one of the leading causes of nonbacterial gastroenteritis outbreaks in many countries (24-26), and even though a 2005 study reported the status of Norovirus in TD, the sample size was too small to draw any conclusions (21). The rate of Norovirus in their study is similar with our result. In spite of these two reports, previous studies may have significantly underestimated the etiological role of viruses until now due to the limitation of detection methods and the short naming history of Norovirus. With our new results, we will need to carefully determine whether to use antibiotics even when the pathogen is not detected.
Here, we showed that the detection rate of pathogens was proportionately high according to the severity of diarrhea; and the amount of consumed water was proportionately related with the severity of diarrhea. We also learned that patients with classic TD and pathogen-detected TD were admitted to hospitals more than others. Therefore, we can support that the classification of TD is still useful to estimate the severity of TD in Korean travelers from South-East Asia. On the basis of this, more attention should be paid to the group of classic TD cases at the international airport; and need to supply an easy classification system for general officers to use.
In this study, the pathogen detection rate (17.7%) was lower than other studies (4, 5, 11, 19) even though we examined rectal swab samples. Many studies have reported that there is no difference in pathogen detection between direct stool sampling and rectal swab (27, 28). Maybe our low detection rate of pathogens is one of the limitations in this study. We did find that TD affects young adults at a higher rate than older people with the same length of stay, staying at the same hotel, and having the same meal plans (4). This may be due to a greater appetite on the part of the younger tourists leading to to ingestion of a larger dose of pathogens.
Travelers to South-East Asian countries are increasing annually by more than 200,000 persons, with a total number of travelers to Korea of more than 5 million per year. This study shows that the rates of EAEC, V. parahaemolyticus and Norovirus in South-East Asian countries among Korean travelers are higher than those seen in other countries and that severe TD with a higher detection rate can cause more aggravated clinical problems.
In conclusion, with our results, the Korea Centers for Disease Control and Prevention can make better and more efficient strategies to prevent and treat TD. A larger scale survey is needed to make more exact plans for dealing with TD due to the limitations of this study. Assistance in our studies from other South-East Asian countries would significantly expand our understanding of TD in Korea and the surrounding area.
ACKNOWLEDGMENTS
We thank the members of the Division of Enteric Bacterial Infections, Enteric and Hepatitis Viruses, Center for Infectious Disease, National Institute of Health, Korea Centers for Disease Control and Prevention for performing the laboratory help, and the National Quarantine Station of Incheon Airport for their help in obtaining stool samples and questionnaire. We are also indebted to the members of the Division of Epidemic Intelligence Service, Korea Centers for Disease Control and Prevention.
AUTHOR SUMMARY
Clinical Characteristics and Etiology of Travelers' Diarrhea among Korean Travelers Visiting South-East Asia
Ji Yong Ahn, Jin-Won Chung, Kyu-Jin Chang, Myung Hwan You, Jin Sung Chai, Young A Kang, Seong-Han Kim, Hyesook Jeoung, Doosung Cheon, Ahyong Jeoung, and Eun Suk Choi
This study examined the incidence of common pathogens and characteristics of travelers' diarrhea (TD) among Koreans visited South-East Asian countries. We performed a prospective study involving 479 travelers with diarrhea from February 2009 to April 2009. Enterotoxigenic Escherichia coli (ETEC) were found in 36.0% of TD cases, as were the following: Enteroaggregative Escherichia coli in 27.0%, Vibrio parahaemolyticus in 13.1%, and Norovirus in 11.5%. The detected rate of classic TD was higher in men, in patients who had a shorter duration trip and in patients who drank more than 1 liter of water per day. Positive stool culture rates were higher in men, in hospitalized patients, and in those who consumed impure water or raw foods. A higher severity of disease corresponded to a significantly higher culture positivity rate. We should consider the possibility of other pathogens besides ETEC in TD and educate travelers about the risk factors.
References
- 1.Castelli F, Pezzoli C, Tomasoni L. Epidemiology of travelers' diarrhea. J Travel Med. 2001;8(Suppl 2):S26–S30. doi: 10.1111/j.1708-8305.2001.tb00543.x. [DOI] [PubMed] [Google Scholar]
- 2.von Sonnenburg F, Tornieporth N, Waiyaki P, Lowe B, Peruski LF, Jr, DuPont HL, Mathewson JJ, Steffen R. Risk and aetiology of diarrhoea at various tourist destinations. Lancet. 2000;356:133–134. doi: 10.1016/S0140-6736(00)02451-X. [DOI] [PubMed] [Google Scholar]
- 3.Steffen R, van der Linde F, Gyr K, Schär M. Epidemiology of diarrhea in travelers. JAMA. 1983;249:1176–1180. [PubMed] [Google Scholar]
- 4.Steffen R, Collard F, Tornieporth N, Campbell-Forrester S, Ashley D, Thompson S, Mathewson JJ, Maes E, Stephenson B, DuPont HL, von Sonnenburg F. Epidemiology, etiology, and impact of traveler's diarrhea in Jamaica. JAMA. 1999;281:811–817. doi: 10.1001/jama.281.9.811. [DOI] [PubMed] [Google Scholar]
- 5.Jiang ZD, Lowe B, Verenkar MP, Ashley D, Steffen R, Tornieporth N, von Sonnenburg F, Waiyaki P, DuPont HL. Prevalence of enteric pathogens among international travelers with diarrhea acquired in Kenya (Mombasa), India (Goa), or Jamaica (Montego Bay) J Infect Dis. 2002;185:497–502. doi: 10.1086/338834. [DOI] [PubMed] [Google Scholar]
- 6.DuPont HL, Ericsson CD. Prevention and treatment of traveler's diarrhea. N Engl J Med. 1993;328:1821–1827. doi: 10.1056/NEJM199306243282507. [DOI] [PubMed] [Google Scholar]
- 7.Hoge CW, Shlim DR, Echeverria P, Rajah R, Herrmann JE, Cross JH. Epidemiology of diarrhea among expatriate residents living in a highly endemic environment. JAMA. 1996;275:533–538. [PubMed] [Google Scholar]
- 8.Kim SH, Cheon DS, Kim JH, Lee DH, Jheong WH, Heo YJ, Chung HM, Jee Y, Lee JS. Outbreaks of gastroenteritis that occurred during school excursions in Korea were associated with several waterborne strains of norovirus. J Clin Microbiol. 2005;43:4836–4839. doi: 10.1128/JCM.43.9.4836-4839.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steffen R. Epidemiology of traveler's diarrhea. Clin Infect Dis. 2005;41(Suppl 8):S536–S540. doi: 10.1086/432948. [DOI] [PubMed] [Google Scholar]
- 10.Echeverria P, Blacklow NR, Sanford LB, Cukor GG. Travelers' diarrhea among American Peace Corps volunteers in rural Thailand. J Infect Dis. 1981;143:767–771. doi: 10.1093/infdis/143.6.767. [DOI] [PubMed] [Google Scholar]
- 11.Bouckenooghe AR, Jiang ZD, De La Cabada FJ, Ericsson CD, DuPont HL. Enterotoxigenic Escherichia coli as cause of diarrhea among Mexican adults and US travelers in Mexico. J Travel Med. 2002;9:137–140. doi: 10.2310/7060.2002.23206. [DOI] [PubMed] [Google Scholar]
- 12.Jiang ZD, Mathewson JJ, Ericsson CD, Svennerholm AM, Pulido C, Du-Pont HL. Characterization of enterotoxigenic Escherichia coli strains in patients with travelers' diarrhea acquired in Guadalajara, Mexico, 1992-1997. J Infect Dis. 2000;181:779–782. doi: 10.1086/315272. [DOI] [PubMed] [Google Scholar]
- 13.Egorov A, Paulauskis J, Petrova L, Tereschenko A, Drizhd N, Ford T. Contamination of water supplies with Cryptosporidium parvum and Giardia lamblia and diarrheal illness in selected Russian cities. Int J Hyg Environ Health. 2002;205:281–289. doi: 10.1078/1438-4639-00153. [DOI] [PubMed] [Google Scholar]
- 14.Gascon J, Vila J, Valls ME, Ruiz L, Vidal J, Corachan M, Prats G, Jimenez de Anta MT. Etiology of traveller's diarrhea in Spanish travellers to developing countries. Eur J Epidemiol. 1993;9:217–223. doi: 10.1007/BF00158796. [DOI] [PubMed] [Google Scholar]
- 15.Okhuysen PC. Traveler's diarrhea due to intestinal protozoa. Clin Infect Dis. 2001;33:110–114. doi: 10.1086/320894. [DOI] [PubMed] [Google Scholar]
- 16.Sanders JW, Tribble DR. Diarrhea in the returned traveler. Curr Gastroenterol Rep. 2001;3:304–314. doi: 10.1007/s11894-001-0053-0. [DOI] [PubMed] [Google Scholar]
- 17.Bhan MK, Raj P, Levine MM, Kaper JB, Bhandari N, Srivastava R, Kumar R, Sazawal S. Enteroaggregative Escherichia coli associated with persistent diarrhea in a cohort of rural children in India. J Infect Dis. 1989;159:1061–1064. doi: 10.1093/infdis/159.6.1061. [DOI] [PubMed] [Google Scholar]
- 18.Wanke CA, Gerrior J, Blais V, Mayer H, Acheson D. Successful treatment of diarrheal disease associated with enteroaggregative Escherichia coli in adults infected with human immunodeficiency virus. J Infect Dis. 1998;178:1369–1372. doi: 10.1086/314443. [DOI] [PubMed] [Google Scholar]
- 19.Adachi JA, Jiang ZD, Mathewson JJ, Verenkar MP, Thompson S, Martinez-Sandoval F, Steffen R, Ericsson CD, DuPont HL. Enteroaggregative Escherichia coli as a major etiologic agent in traveler's diarrhea in 3 regions of the world. Clin Infect Dis. 2001;32:1706–1709. doi: 10.1086/320756. [DOI] [PubMed] [Google Scholar]
- 20.Mathewson JJ, Johnson PC, DuPont HL, Morgan DR, Thornton SA, Wood LV, Ericsson CD. A newly recognized cause of travelers' diarrhea: enteroadherent Escherichia coli. J Infect Dis. 1985;151:471–475. doi: 10.1093/infdis/151.3.471. [DOI] [PubMed] [Google Scholar]
- 21.Ko G, Garcia C, Jiang ZD, Okhuysen PC, Belkind-Gerson J, Glass RI, DuPont HL. Noroviruses as a cause of traveler's diarrhea among students from the United States visiting Mexico. J Clin Microbiol. 2005;43:6126–6129. doi: 10.1128/JCM.43.12.6126-6129.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Su YC, Liu C. Vibrio parahaemolyticus: a concern of seafood safety. Food Microbiol. 2007;24:549–558. doi: 10.1016/j.fm.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Taylor DN, Echeverria P. Etiology and epidemiology of travelers' diarrhea in Asia. Rev Infect Dis. 1986;8(Suppl 2):S136–S141. doi: 10.1093/clinids/8.supplement_2.s136. [DOI] [PubMed] [Google Scholar]
- 24.Fankhauser RL, Monroe SS, Noel JS, Humphrey CD, Bresee JS, Parashar UD, Ando T, Glass RI. Epidemiologic and molecular trends of "Norwalk-like viruses" associated with outbreaks of gastroenteritis in the United States. J Infect Dis. 2002;186:1–7. doi: 10.1086/341085. [DOI] [PubMed] [Google Scholar]
- 25.de Wit MA, Koopmans MP, Kortbeek LM, Wannet WJ, Vinjé J, van Leusden F, Bartelds AI, van Duynhoven YT. Sensor, a population-based cohort study on gastroenteritis in the Netherlands: incidence and etiology. Am J Epidemiol. 2001;154:666–674. doi: 10.1093/aje/154.7.666. [DOI] [PubMed] [Google Scholar]
- 26.Hale A, Mattick K, Lewis D, Estes M, Jiang X, Green J, Eglin R, Brown D. Distinct epidemiological patterns of Norwalk-like virus infection. J Med Virol. 2000;62:99–103. doi: 10.1002/1096-9071(200009)62:1<99::aid-jmv15>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 27.Adkins HJ, Santiago LT. Increased recovery of enteric pathogens by use of both stool and rectal swab specimens. J Clin Microbiol. 1987;25:158–159. doi: 10.1128/jcm.25.1.158-159.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lautenbach E, Harris AD, Perencevich EN, Nachamkin I, Tolomeo P, Metlay JP. Test characteristics of perirectal and rectal swab compared to stool sample for detection of fluoroquinolone-resistant Escherichia coli in the gastrointestinal tract. Antimicrob Agents Chemother. 2005;49:798–800. doi: 10.1128/AAC.49.2.798-800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]