Abstract
The objective of this study was to evaluate the prevalence of asthma, allergic rhinitis, and atopic dermatitis, as well as the risk factors of wheezing among young adults in the Korean military. Young military conscripts in five areas completed a modified International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire. For subjects with current wheeze in one sample area, baseline spirometry and bronchodilator response were measured. For subjects without a significant response to bronchodilator (improvement in FEV1 of more than 200 mL and 12%), methacholine challenge tests (MCT) were also performed. Of 3,359 subjects that completed the questionnaire, 354 (10.5%) had current wheeze, 471 (14.0%) had current allergic rhinitis, and 326 (9.7%) had current eczema. Current wheeze was associated with family history of allergic disease, overweight, current smoking, allergic rhinitis, and atopic dermatitis. Of 36 subjects with current wheeze who underwent PFT with or without MCT in the Anyang area, 24 (66.7%) were confirmed to have current asthma. In conclusion, the prevalence of allergic disease in young adults of Korean military is not low, and the risk factors of wheezing include family history of allergic disease, overweight, current smoking, allergic rhinitis, and atopic dermatitis.
Keywords: Allergic Rhinitis; Asthma; Dermatitis, Atopic; Prevalence; Risk Factors; Respiratory Sounds
INTRODUCTION
Asthma is becoming a public health problem worldwide and there is a various concern for increasing prevalence (1). Asthma is characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, which can influence on a daily life of individual patient, and furthermore his or her community as well (1). Therefore, understanding the prevalence of asthma is important for making community health policies and controlling the disease. Predominantly based on physicians' diagnoses in military recruits, the prevalence of asthma among young adults in Western countries has been extensively investigated (2-6). However, there are few reports on prevalence of asthma among young adults of military conscript in Asian countries.
Asthma is known to be associated with other allergic diseases including allergic rhinitis and atopic dermatitis, sharing a temporal allergic inflammation relationship ('atopic march') (7). In this regard, the prevalence of asthma, allergic rhinitis, and atopic dermatitis has been globally and systematically investigated at the same time using standardized self-reported questionnaires which are prepared by the International Study of Asthma and Allergies in Childhood (ISAAC) (8). It has been found that the prevalence of all three disorders has generally increased in Asia-Pacific, India, North America, Latin America, eastern Mediterranean, and Europe (8).
In Korea, the previous studies have examined the prevalence of allergic disease in children and adolescents using a modified ISAAC questionnaire (9-13). A few studies reported the prevalence of allergic diseases in adults (14, 15). However, these studies did not include young adults of military conscript and only evaluated the prevalence of asthma. The objective of this study was to investigate the prevalence of asthma, allergic rhinitis, and atopic dermatitis, as well as risk factors of wheezing, among young adults in the Korean military.
MATERIALS AND METHODS
Subjects and questionnaires
Military conscripts in five areas (Seoul, Anyang, Cheolwon/Hwacheon, Pocheon, Cheongju) were subjected in this questionnaire and examination survey, as a representative sample of Korean soldiers selected randomly by sampling. Each subject provided a written informed consent, and answered the modified ISSAC questionnaire, which included demographic data and items of core symptoms of allergic diseases, such as asthma, allergic rhinitis, and atopic dermatitis (8, 16).
Pulmonary function test and methacholine challenge test
For subjects in Anyang area who experienced wheeze in the past 12 months (current wheeze), we performed a pulmonary function test (PFT) and a methacholine challenge test (MCT) at the Armed Forces Capital Hospital. PFT was repeated 15 min after 400 µg salbutamol inhalation. A positive bronchodilator response (BDR) or reversible airway obstruction was defined if forced expiratory volume in 1 sec (FEV1) increased by more than 200 mL and 12% from the basal level after salbutamol inhalation. For subjects without positive BDRs, MCTs were conducted according to the American Thoracic Society guidelines. Briefly, methacholine was inhaled during inspiration using an automatic nebulizing device (NE-U17; OMRON, Kyoto, Japan) until a provocative concentration of methacholine producing a 20% decline in FEV1 (PC20) was obtained or a concentration of 16 mg/mL was reached. A PC20 < 16 mg/mL was classified as airway hyperresponsiveness. Current wheeze with reversible airway obstruction or airway hyperresponsiveness was defined as current asthma (9, 14, 15).
Statistical analyses
Demographic and clinical data were compared between subjects with current wheeze and without current wheeze by Student's t-test in continuous variables and the chi-squared test in categorical variables. A logistic regression model was constructed with current wheeze as the dependent variable and family history of allergic disease, overweight, current smoking, current allergic rhinoconjunctivitis, and current eczema as independent variables. A forward selection method was used to exclude multicolinearity of each variable. All of the statistical analyses were performed using PASW 17.0 (SPSS Inc. Chicago, IL, USA). A P value < 0.05 was deemed to indicate statistical significance. Results are presented as mean ± standard deviation, or numbers with percentages.
Ethics statement
The research protocol was approved by the ethics committee of the Armed Forces Medical Command. This study was registered in an open-access trials registry prior to the enrollment of the first participant (registry URL: www.clinicaltrials.gov, assigned database number: NCT00982085).
RESULTS
Characteristics of subjects according to current wheeze
Out of 3,359 subjects that completed the questionnaire, 354 (10.5%) had current wheeze. Among the subjects with current wheeze, 267 (75.4%) also experienced wheeze after exercise in the past year. Out of all the subjects, 209 (6.2%) had been diagnosed with asthma by doctors (diagnosed asthma), and 46 subjects (1.4%) had been treated for asthma within the past 12 months (currently treated asthma).
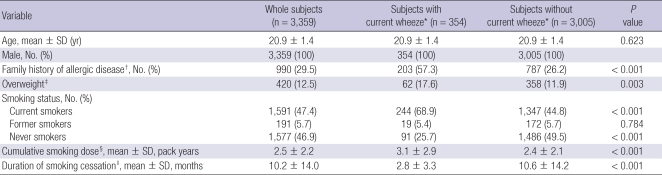
Demographic characteristics were compared between subjects with and without current wheeze (Table 1). Age was not different between the two groups. All the subjects were male. The proportion of subjects who had a family history of allergic disease was higher among subjects with current wheeze than those without (57.3% vs 26.2%; P < 0.001). The proportions of subjects who were overweight (BMI > 25) and who were current smokers were significantly higher in the group with current wheeze than the group without (17.6% vs 11.9%; P = 0.003 and 68.9% vs 44.8%; P < 0.001, respectively). Among smokers, the mean cumulative smoking dose was higher among those with current wheeze than those without (3.1 ± 2.9 pack year [PY] vs 2.4 ± 2.1 PY; P < 0.001). Among former smokers, duration of smoking cessation was significantly shorter among subjects with current wheeze than those without (2.8 ± 3.3 vs 10.6 ± 14.2 months; P < 0.001).
Table 1.
Demographic characteristics according to current wheeze
Continuous data are presented as mean ± SD. Dichotomous data are presented as number (%). *Wheeze in the past 12 months; †Family history of asthma, allergic rhinitis, and atopic dermatitis; ‡Body mass index (kg/m2) ≥ 25; §Cumulative smoking dose is presented among current smokers and former smokers; ∥Duration of cessation of smoking is presented among former smokers.
Prevalence of allergic rhinitis, and atopic dermatitis according to current wheeze
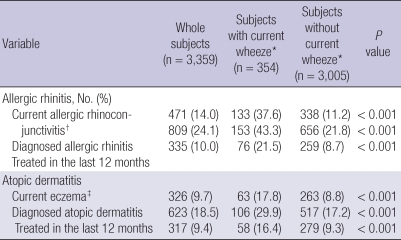
The percentage of subjects with current allergic rhinoconjunctivitis (i.e., the presence of sneezing or a runny or blocked nose, accompanied by itchy watery eyes without a cold or the flu in the past 12 months) was significantly higher among subjects with current wheeze (37.6% vs 11.2%; P < 0.001; Table 2). Current wheeze was also higher among subjects with diagnosed allergic rhinitis and currently treated allergic rhinitis (43.3% vs 21.8%; P < 0.001 and 21.5% vs 8.7%; P < 0.001, respectively) as well as those with current eczema (i.e., the presence of an itchy rash at any time in the past 12 months affecting the following places: the folds of the elbows; behind the knees; in front of the ankles; under the buttocks; or around the neck, ears, or eyes) (17.8% vs 8.8%; P < 0.001). The proportions of subjects with diagnosed atopic dermatitis and currently treated atopic dermatitis were also higher among subjects with current wheeze (29.9% vs 17.2%; P < 0.001 and 16.4% vs 9.3%; P < 0.001, respectively).
Table 2.
Allergic rhinitis and atopic dermatitis according to current wheeze
Data are presented as number (%). *Wheeze in the past 12 months; †Sneezing or a runny or blocked nose accompanied by itchy watery eyes without a cold or the flu in the past 12 months; ‡Itchy rash at any time in the past 12 months affecting following body parts: the folds of the elbows; behind the knees; in front of the ankles; under the buttocks; or around the neck, ears, or eyes.
Risk for current wheeze
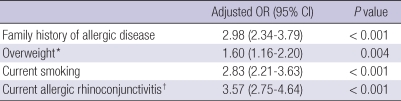
Multivariate analysis indicated that family history of allergic disease (odds ratio [OR] = 2.98; 95% confidence interval [CI]: 2.34-3.79), overweight (OR = 1.60; 95% CI: 1.16 2.20), current smoking (OR = 2.83; 95% CI: 2.21-3.63), and current allergic rhinoconjunctivitis (OR = 3.57; 95% CI: 2.75-4.64) were independent risk factors for asthma (Table 3).
Table 3.
Odds ratio (OR) of current wheeze in whole subjects
*Body mass index (kg/m2) ≥ 25; †The presence of sneezing or a runny or blocked nose accompanied by itchy watery eyes without a cold or the flu in the past 12 months.
Frequency of current wheeze and nocturnal awakening and the duration of absence from work due to wheeze
Among subjects with current wheeze, 54.5% had experienced wheeze one to three times in the past year, 26.6% four to twelve times, and 18.9% more than 12 times. Of subjects with current wheeze, 62.7% had never experienced nocturnal awakening due to wheeze, while 25.4% had once or less a week, and 11.9% had once or more a week, respectively. Seventy-nine percent of the subjects with current wheeze were not absent from work due to wheeze, but 13.6% were absent from work due to wheeze for 1-3 days, 2.0% for 4-6 days and 5.4% for more than 7 days in a year, respectively.
Current asthma evaluated by PFT and MCT
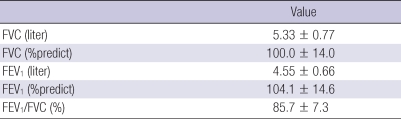
A total of 74 subjects with current wheeze in Anyang were asked for visiting the study hospital for PFT two months after the questionnaire survey. Of them, 16 subjects had been discharged from military service and 19 subjects were unable to visit due to military unit duties. In total, 39 subjects visited the study hospital and three soldiers declined PFT. Of the 36 subjects who underwent PFT and BDR, one was positive for BDR and other 35 were negative for BDR (Table 4). Of the 35 subjects with negative BDR, airway hyperresponsiveness could be defined in 23 by MCT. Among 23 subjects with airway hyperresponsiveness, PC20 was less than 1 mg/mL in 6 subjects, ranges from 1 mg/mL to 4 mg/mL in 7 subjects, 4 mg/mL to 8 mg/mL in 7 subjects, and 8 mg/mL to 16 mg/mL in 3 subjects. Current asthma was diagnosed in 24 subjects (66.7%) out of 36 subjects who underwent PFT.
Table 4.
Results of pulmonary function test (PFT) among 36 subjects in Anyang area*
*Data are presented as mean ± SD.
DISCUSSION
Relatively few studies have undertaken on the prevalence of asthma in young adults in Asia. The prevalence of asthma in young adults was currently reported to be 6.5%-7.8% in Western countries based on physician diagnosis (2-4). The rate of diagnosed asthma in this study is quite similar to those rates in Western countries. Geographic and temporal differences should be considered when comparing the prevalence of asthma (8).
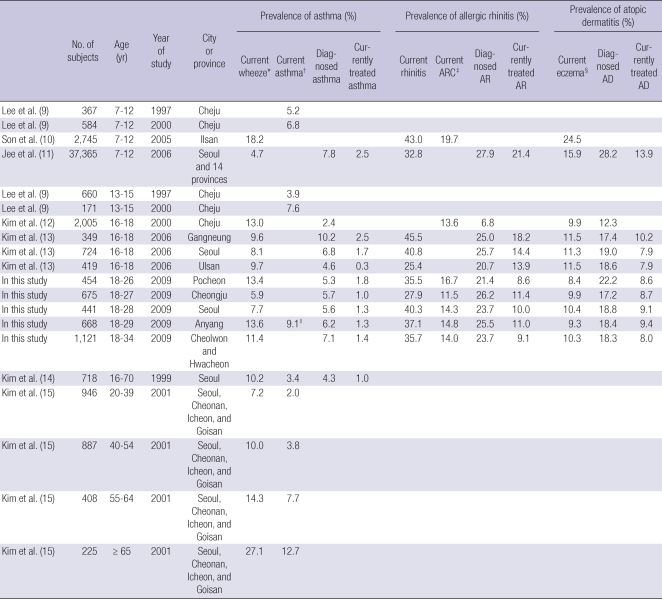
In comparison with several reports on the prevalence of allergic diseases among children and middle aged adults in Korea (Table 5 in online supplement), our findings showed similar prevalence, only a slightly different due to area, time of study, and age of the population. The prevalence of allergic diseases was low among adolescents in Jeju Island located in the southern to Korea Peninsula (12, 13). The low prevalence may be caused by different condition of climate, air pollution, and allergens from other areas of the Korea Peninsula (9, 12), with the recent increase in asthma prevalence (9). The prevalence of allergic diseases in adolescents in three cities of Korea was similar to the rate reported in this study (13). This may be the result of a similar age group and few temporal gaps between the two studies. In other studies on adults, the prevalence of current wheeze was also similar to that in this study (14, 15).
Table 5.
Prevalence of allergic diseases in Korea
*Wheeze in the past 12 months; †Current asthma was indicated if a subject with current wheeze showed an airway hyperresponsiveness in methacholine challenge test according to the definition of each study; ‡Sneezing or a runny or blocked nose accompanied by itchy watery eyes without a cold or the flu in the past 12 months; §Itchy rash at any time in the past 12 months affecting following places: the folds of the elbows; behind the knees; in front of the ankles; under the buttocks; or around the neck, ears, or eyes; ∥Extrapolated from the results that 24 (66.7%) out of 36 subjects with current wheeze who underwent pulmonary function test (PFT) with or without methacholine challenge test (MCT) showed bronchodilator response in PFT or airway hyperresponsiveness in MCT. ARC, allergic rhinoconjunctivitis; AR, allergic rhinitis; AD, atopic dermatitis.
In this study, current wheeze was associated with a family history of allergic disease, overweight, current smoking, current rhinoconjunctivitis, and current eczema. Current wheeze was strongly associated with current allergic rhinoconjunctivitis more than eczema. There are several reports describing the correlation of asthma with allergic rhinitis or eczema (17-20). Considering that atopic dermatitis or eczema generally proceeds subsequent allergic rhinitis and asthma in the 'atopic march' (7), it seems reasonable that current wheeze more significantly correlates with current allergic rhinoconjunctivitis than current eczema. In other reports, allergic diseases were reported to be associated with a family history of allergic disease (21-23). Recently, overweight was reported to be associated with asthma in adults and children (24-26).
There are some controversies about the association between smoking and asthma. In some reports, young smokers had better lung function and less airway responsiveness than non-smokers, because those with airway hyperresponsiveness tended to quit smoking before it became a habit, the so-called 'healthy smoker effect' (27). However, many smokers reported wheezing more frequently, and wheezing and airway responsiveness abated after smoking cessation (28, 29). Among young adults in the Swiss military, the incidence of current wheeze was higher among current smokers than former smokers or non-smokers (16%, 11%, and 7%, respectively) (30). Among 55-64 yr old Koreans, current smoking was found to be significantly related to current asthma and airway hyperresponsiveness, although smoking was positively associated with FEV1 (15).
There are some limitations in the present study. Current wheeze was based on self-reporting, allowing for possibly overestimating the prevalence of asthma. However, 27%-54% of subjects with current wheeze were confirmed to have asthma by PFT and MCT in other studies (14, 15), compared with 67.9% in our study. Thus, the validity of the questionnaire was apparently not inferior to that of other studies. Furthermore, worldwide studies of asthma prevalence have used the same method. Nevertheless, we evaluated MCT among only small number of subjects, therefore it could not represent current asthma of all subjects. It is also one of limitations of our study. Also, not all risk factors for asthma were fully evaluated among the young adults in the Korean military. It can be another limitation that the prevalence of allergic diseases among young soldiers in Korean military cannot represent that of all young adults in Korea. Young Korean adults are exempted from military conscription when severe allergic disease is presented. In addition, there are some factors not only associated with allergic diseases but also with exemption from military conscript such as low educational background and so on. The last point is that young soldiers could exaggerate their symptoms in order to fall in their duty. Therefore we could overestimate the prevalence of allergic diseases and their severity.
In conclusion, the prevalence of allergic diseases in young adults of Korean military is not low. Risk factors for wheezing include family history of allergic disease, overweight, current smoking, current allergic rhinoconjunctivitis, and current eczema. This is the first study on the prevalence of allergic diseases among young conscripts in East Asia.
ACKNOWLEDGMENTS
We thank Dae Kyeong Kim and Seung Han Park in the Armed Forces Capital Hospital for their contribution to collection and analysis of data. We also thank Yong Seok Park, Jae Deok Sim and Sang Min Rhee for their contribution in recruiting study subjects. And special thank goes to Wayne, a native speaker of English for proofreading our article.
Footnotes
This work was supported by the Korean Military Medical Research Project funded by the ROK Ministry of National Defense (ROK-MND-2009-KMMRP-011).
AUTHOR SUMMARY
Prevalence of Allergic Diseases and Risk Factors of Wheezing in Korean Military Personnel
Sang Min Lee, Jong Seong Ahn, Chang Suk Noh, and Sei Won Lee
The objective of this study was to evaluate the prevalence of asthma, allergic rhinitis, and atopic dermatitis, as well as the risk factors of wheezing among young adults in the Korean military. Of 3,359 subjects that completed a modified International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire, 354 (10.5%) had current wheeze, 471 (14.0%) had current allergic rhinitis, and 326 (9.7%) had current eczema. Current wheeze was associated with family history of allergic disease, overweight, current smoking, allergic rhinitis, and atopic dermatitis. Of 36 subjects with current wheeze who underwent PFT with or without MCT in the Anyang area, 24 (66.7%) were confirmed to have current asthma. In conclusion, the prevalence of allergic disease in young adults of Korean military is not low, and the risk factors of wheezing include family history of allergic disease, overweight, current smoking, allergic rhinitis, and atopic dermatitis.
References
- 1.Global strategy for asthma management and prevention: NHLIB/WHO workshop report. Global Initiative for Asthma (GINA), National Institutes of Health, National Heart, Lung and Blood Institute. [accessed on 1 May 2010]. Available at http://www.ginasthma.com Data last updated, 2009.
- 2.Lev-Tzion R, Friedman T, Shochat T, Gazala E, Wohl Y. Asthma and psychiatric disorders in male army recruits and soldiers. Isr Med Assoc J. 2007;9:361–364. [PubMed] [Google Scholar]
- 3.Vizzaccaro A, Cirillo I, Tosca MA, Milanese M, Ciprandi G. Asthma in Italian conscripts: a four year study. Eur Ann Allergy Clin Immunol. 2003;35:125–129. [PubMed] [Google Scholar]
- 4.Ciprandi G, Vizzaccaro A, Cirillo I, Tosca M, Passalacqua G, Canonica GW. Underdiagnosis and undertreatment of asthma: a 9-year study of Italian conscripts. Int Arch Allergy Immunol. 2001;125:211–215. doi: 10.1159/000053818. [DOI] [PubMed] [Google Scholar]
- 5.Haahtela T, Lindholm H, Björkstén F, Koskenvuo K, Laitinen LA. Prevalence of asthma in Finnish young men. BMJ. 1990;301:266–268. doi: 10.1136/bmj.301.6746.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dubois P, Degrave E, Vandenplas O. Asthma and airway hyperresponsiveness among Belgian conscripts, 1978-91. Thorax. 1998;53:101–105. doi: 10.1136/thx.53.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spergel JM, Paller AS. Atopic dermatitis and the atopic march. J Allergy Clin Immunol. 2003;112(6 Suppl):S118–S127. doi: 10.1016/j.jaci.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 8.Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, Williams H ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 9.Lee MH, Hong SC, Kim SH, Bahn JW, Chang YS, Kim TB, Kim YK, Cho SH, Min KU, Kim YY. Prevalence of asthma and atopy in children living in rural areas of Cheju island for an interval of three years. J Asthma Allergy Clin Immunol. 2002;22:85–91. [Google Scholar]
- 10.Son KY, Park KS, Hwang HH, Yun BS, Lee SJ, Kim MA, Park JY, Kim KE, Jang KC. Prevalence of allergic diseases among primary school children in Ilsan, Gyeonggi and Changes of symptoms after environmental control in 2005. Pediatr Allergy Respir Dis. 2007;17:384–393. [Google Scholar]
- 11.Jee HM, Kim KW, Kim CS, Sohn MH, Shin DC, Kim KE. Prevalence of asthma, rhinitis and eczema in Korean children using the international study of asthma and allergies in childhood (ISAAC) questionnaires. Pediatr Allergy Respir Dis. 2009;19:165–172. [Google Scholar]
- 12.Kim SH, Hong SC, Bae JM, Lee MH, Kim YK, Cho SH, Min KU, Kim YY. Distinct effect of sensitization of house dust mite and citrus red mite (Panonychus citri) in the development of allergic diseases in 16-18 year old adolescents living in rural areas of Jeju Island. J Asthma Allergy Clin Immunol. 2002;22:92–99. [Google Scholar]
- 13.Kim BS, Kim HB, Lee SY, Kim JH, Jin HS, Kim BJ, Yu JH, Yoo SM, Hong SJ. Prevalence of allergic diseases in high school students in Korea. Korean J Asthma Allergy Clin Immunol. 2007;27:168–175. [Google Scholar]
- 14.Kim SH, Lee JY, Son SW, Chang YS, Jung JW, Kim YK, Cho SH, Min KU, Kim YY. Prevalence of adult asthma based on questionnaires and methacholine bronchial provocation test in Seoul. J Asthma Allergy Clin Immunol. 2001;21:618–627. doi: 10.1046/j.1365-2222.1997.710839.x. [DOI] [PubMed] [Google Scholar]
- 15.Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Park HW, Jung JW, Bahn JW, Chang YS, Choi DC, Chang SI, Min KU, Kim YY, Cho SH. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002;32:1706–1712. doi: 10.1046/j.1365-2222.2002.01524.x. [DOI] [PubMed] [Google Scholar]
- 16.Kim SH, Kim YK, Lee MH, Hong SC, Bae JM, Min KU, Kim YY, Cho SH. Relationship between sensitization to citrus red mite (Panonychus citri) and the prevalence of atopic diseases in adolescents living near citrus orchards. Clin Exp Allergy. 2002;32:1054–1058. doi: 10.1046/j.1365-2222.2002.01431.x. [DOI] [PubMed] [Google Scholar]
- 17.Landrigan PJ, Trasande L, Thorpe LE, Gwynn C, Lioy PJ, D'Alton ME, Lipkind HS, Swanson J, Wadhwa PD, Clark EB, Rauh VA, Perera FP, Susser E. The National Children's Study: a 21-year prospective study of 100,000 American children. Pediatrics. 2006;118:2173–2186. doi: 10.1542/peds.2006-0360. [DOI] [PubMed] [Google Scholar]
- 18.Strachan DP, Butland BK, Anderson HR. Incidence and prognosis of asthma and wheezing illness from early childhood to age 33 in a national British cohort. BMJ. 1996;312:1195–1199. doi: 10.1136/bmj.312.7040.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buffum WP, Settipane GA. Prognosis of asthma in childhood. Am J Dis Child. 1966;112:214–217. doi: 10.1001/archpedi.1966.02090120082007. [DOI] [PubMed] [Google Scholar]
- 20.Castro-Rodriguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med. 2000;162:1403–1406. doi: 10.1164/ajrccm.162.4.9912111. [DOI] [PubMed] [Google Scholar]
- 21.Vázquez Nava F, Saldívar González AH, Martínez Perales G, Lin Ochoa D, Barrientos Gómez MC, Vázquez Rodríguez EM, Vázquez Rodríguez CF, Beltrán Guzmán FJ. Associations between family history of allergy, exposure to tobacco smoke, active smoking, obesity, and asthma in adolescents. Arch Bronconeumol. 2006;42:621–626. doi: 10.1016/s1579-2129(07)60003-2. [DOI] [PubMed] [Google Scholar]
- 22.Sibbald B, Turner-Warwick M. Factors influencing the prevalence of asthma among first degree relatives of extrinsic and intrinsic asthmatics. Thorax. 1979;34:332–337. doi: 10.1136/thx.34.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horwood LJ, Fergusson DM, Shannon FT. Social and familial factors in the development of early childhood asthma. Pediatrics. 1985;75:859–868. [PubMed] [Google Scholar]
- 24.Camargo CA, Jr, Weiss ST, Zhang S, Willett WC, Speizer FE. Prospective study of body mass index, weight change, and risk of adult-onset asthma in women. Arch Intern Med. 1999;159:2582–2588. doi: 10.1001/archinte.159.21.2582. [DOI] [PubMed] [Google Scholar]
- 25.Nystad W, Meyer HE, Nafstad P, Tverdal A, Engeland A. Body mass index in relation to adult asthma among 135,000 Norwegian men and women. Am J Epidemiol. 2004;160:969–976. doi: 10.1093/aje/kwh303. [DOI] [PubMed] [Google Scholar]
- 26.Young SY, Gunzenhauser JD, Malone KE, McTiernan A. Body mass index and asthma in the military population of the northwestern United States. Arch Intern Med. 2001;161:1605–1611. doi: 10.1001/archinte.161.13.1605. [DOI] [PubMed] [Google Scholar]
- 27.O'Connor GT, Sparrow D, Weiss ST. The role of allergy and nonspecific airway hyperresponsiveness in the pathogenesis of chronic obstructive pulmonary disease. Am Rev Respir Dis. 1989;140:225–252. doi: 10.1164/ajrccm/140.1.225. [DOI] [PubMed] [Google Scholar]
- 28.US Department of Health and Human Services (USDHHS) The health effects of active smoking: a report of the Surgeon General. Washington, DC: US Government Printing Office; 2004. [Google Scholar]
- 29.US Department of Health and Human Services (USDHHS) The health benefits of smoking cessation. A report of the Surgeon General. Washington, DC: U.S. Government Printing Office; 1990. [DHHS Publication Number 90-8416] [Google Scholar]
- 30.Miedinger D, Chhajed PN, Karli C, Lupi GA, Leuppi JD. Respiratory symptoms and smoking behaviour in Swiss conscripts. Swiss Med Wkly. 2006;136:659–663. doi: 10.57187/smw.2006.11544. [DOI] [PubMed] [Google Scholar]