Abstract
Background:
Few studies focus on the fusion rates and outcomes for single-level anterior cervical diskectomy/fusion (1-ACDF) utilizing iliac autograft and dynamic plates.
Methods:
Fusion rates and outcomes were prospectively evaluated in 60 consecutive patients undergoing 1-ACDF utilizing iliac autograft and dynamic plates (ABC; Aesculap, Tuttlingen, Germany). Eighteen patients had radiculopathy, while 42 were myelopathic (average Nurick Score 3.3). Pathology included single-level disc disease/spondylosis (38 patients) and/or ossification of the posterior longitudinal ligament (OPLL, 22 patients). Fusion was assessed at 3, 6, and up to 12 months postoperatively utilizing dynamic X-rays and 2D-CT scans. Outcomes were evaluated up to 24 months postoperatively utilizing Odom's Criteria, Nurick Grades, and Short-Form 36 (SF-36) outcome questionnaires. Patients were followed for an average of 4.8 postoperative years (minimum 2 years).
Results:
Although dynamic X-rays/2D-CT studies documented 100% fusion an average of 3.8 months (range 2.5-8 months] postoperatively, 5 heavy smokers exhibited delayed fusions [6-8 months postoperatively]. Two years postoperatively, the average Nurick Score was 0.3 (mild radiculopathy), while Odom's Criteria revealed 52 excellent, 6 good, and 2 fair outcomes [the latter 8 patients were heavy smokers]). Utilizing SF-36 outcome questionnaires, patients markedly improved (>10.0 point gain) on 5 of 8 Health Scales within 6 months, 7 of 8 within 1 year, and all 8 within 2 postoperative years.
Conclusions:
For 60 patients undergoing 1-ACDF utilizing dynamic plates, ultimately a 100% fusion rate was achieved (5 heavy smokers exhibited delayed fusions). Two years postoperatively, Nurick Grades, Odom's Criteria, and SF-36 questionnaires revealed adequate outcomes.
Keywords: Single-level, Anterior Cervical Diskectomy/Fusion, SF-36 Outcomes, Fusion Rates, Autograft, Dynamic Plates
INTRODUCTION
Few studies document the efficacy of utilizing iliac crest autograft with dynamic plates (ABC; Aesculap, Tuttlingen, Germany) for performing single-level anterior cervical diskectomy and fusion (1-ACDF) addressing disc disease/spondylosis or ossification of the posterior longitudinal ligament (OPLL). One-year fusion rates (dynamic X-rays and 2D-CT studies) and 2-year outcomes (Nurick Grades, Odom's Criteria, and Short-Form (SF-36) questionnaires) were assessed for 60 such patients undergoing single-level anterior cervical diskectomy and fusion (1-ACDF) utilizing iliac crest autograft and dynamic plates.
MATERIALS AND METHODS
Clinical Data
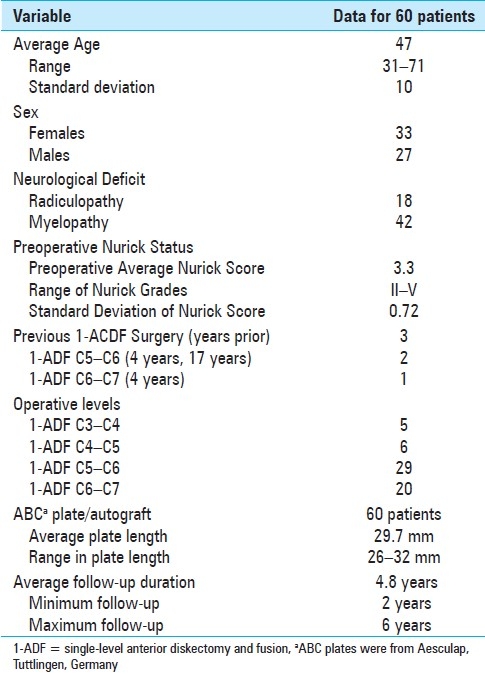
Sixty patients, 33 females and 27 males, underwent 1-ACDF utilizing iliac crest autograft and dynamic ABC plates [Table 1]. Thirty-two of these patients had a history of trauma. Thirty of 60 patients demonstrated various comorbidities which included diabetes (3 patients), hypertension (5 patients), psychiatric/anxiety disorders (3 patients), osteoporosis (5 patients), smoking (12 patients/8 heavy smokers), and obesity (21 patients). The average patient weighed 184 lbs (range 115-320); 21 patients weighed over 200 lbs, and 7 of these weighed over 240 lbs. Preoperative neurological deficits included radiculopathy (18 patients) or myelopathy (42 patients). Prior to surgery, the average Nurick Score was 3.3, consistent with moderate myelopathy (Nurick Grade range II-V).
Table 1.
Clinical data for 60 patients undergoing single-level anterior diskectomy/fusion (1-ACDF)
MR and CT Studies
Preoperatively, both MR and CT studies were obtained to document cervical disc disease/spondylosis (38 patients) or OPLL (22 patients) [Figures 1–2]. MR scans uniquely documented increased signals in the cord consistent with edema/myelomalacia (19 patients), while CT studies best delineated OPLL. Three patients had prior 1-ACDF performed at other levels [Table 1]. Single-level ACDF procedures involved the C5-C6 (29 patients), C6-C7 (20 patients), C4-C5 (6 patients), and C3-C4 (5 patients) levels. Single-level ACDF was performed utilizing iliac crest autograft and dynamic plates [Table 1]. The average operative time was 3.4 h [Table 1]. Patients were followed for an average of 4.8 postoperative years (minimum 2-year follow-up).
Figure 1.
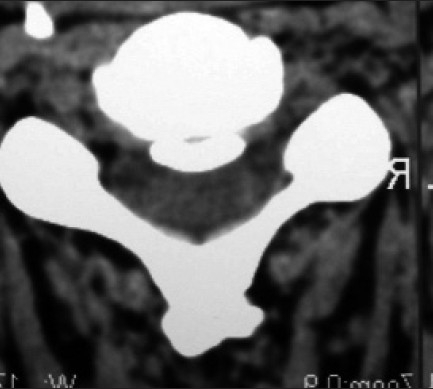
This transaxial CT examination readily demonstrates the “smooth-layer sign” associated with OPLL seen at the disc space level alone. The “smooth-layer sign” is rarely associated with a cerebrospinal fluid fistula during 1-ACDF surgery.
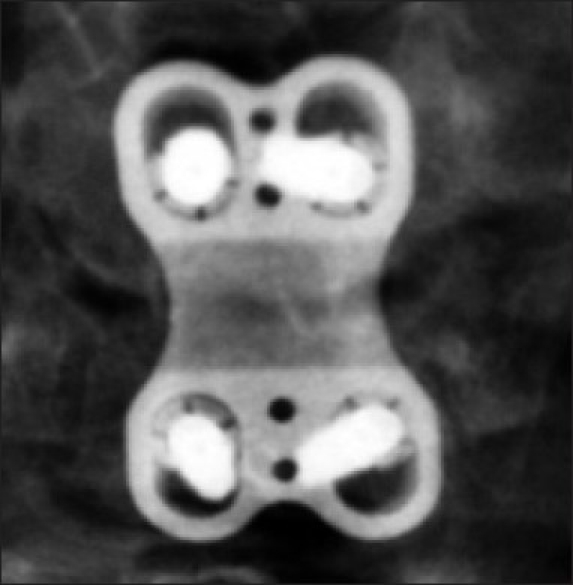
Figure 2.

On this noncontrast axial CT study, at the level of the interspace, a central ossified intradural mass is seen which is separated from the posterior margin of the vertebral body by the interposed hypodense dura. This is the classical image of the “double-layer sign” for OPLL that is highly associated with cerebrospinal fluid fistulas during anterior cervical surgery. This patient developed an intraoperative CSF fistula which was effectively treated with a sewn-in [7-0 Gortex Sutures] dural graft, fibrin sealant, and microfibrillar collagen
Documentation of Fusion
Postoperative fusion rates, assessed by two independent neuroradiologists blinded to the study design, were based upon both dynamic X-ray and 2D-CT studies obtained at 3, 4.5, 6, and up to 12 months postoperatively and/or until fusion occurred [Figures 3–5]. Dynamic X-ray fusion criteria included the lack of active motion/translation, < 0-1 mm of motion between adjacent spinous processes, and <15° of angulation. 2D-CT fusion criteria included the presence of bony trabeculation, and the lack of lucency at the graft/vertebral body interface.
Figure 3.

This lateral cervical plain X-ray demonstrates adequate dynamic plate and graft localization. The interbody graft appears incorporated, as there is bony trabeculation and no lucency at the graft/vertebral body interface. Note the 3-4 mm superior and inferior migration of the plate over the vertebral body screw heads
Figure 5.

The sagittal midline 2D-CT study obtained 6 months postoperatively following iliac autograft and dynamic ABC plate placement documented an adequate fusion. Observe the lack of lucency and the presence of bony trabeculation at the graft/vertebral body interfaces superiorly and inferiorly. A further fusion criterion is the lack of lucency surrounding the vertebral screws. Also note the 3-4 mm of cephalad and caudad screw migration within the plate minimizing stress shielding and allowing for graft settling/fusion.
Figure 4.
This AP cervical plain X-ray demonstrates maximal cephalad and caudad migration of the screws within the slots of the dynamic plate
Outcome Assessment
Outcomes were analyzed utilizing Nurick Grades, Odom's Criteria, and the SF-36 questionnaires. Nurick Grades and SF-36 questionnaires were assessed preoperatively, and at 3, 6, 12, and 24 months postoperatively, while Odom's Criteria were evaluated over these same intervals but only postoperatively. To simplify the presentation of SF-36 results, data were divided into three categories of “improvement.” At each time interval, data were compared with preoperative baselines, e.g., minimal improvement (± 0−5 points), moderate improvement (± 6−10 points), and marked improvement (>10 points).
RESULTS
Outcome Measures
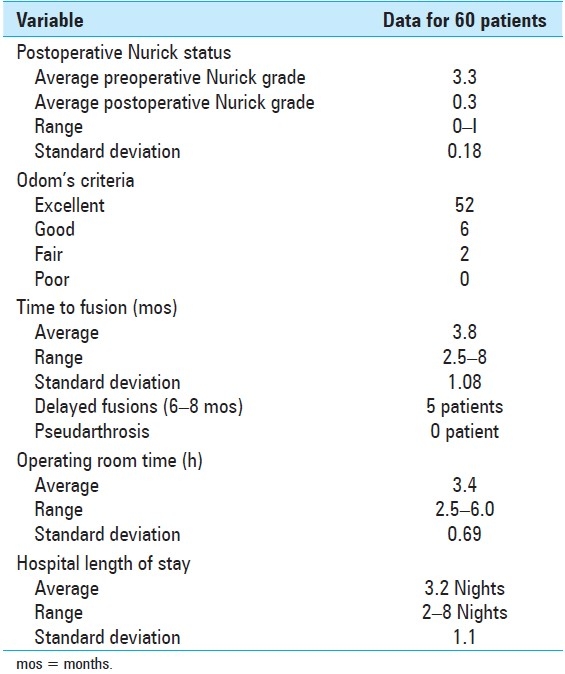
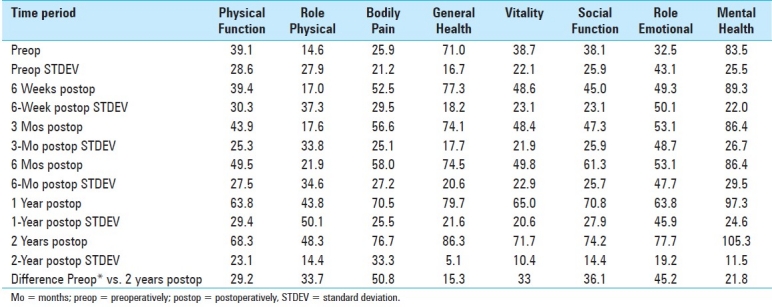
Outcomes were assessed utilizing Nurick Grades/Scores, Odom's Criteria, and SF-36 questionnaires up to 2 years postoperatively. By the second postoperative year, patients improved an average of 3.0 Nurick Grades; the average preoperative Nurick Score was 3.3 (moderate myelopathy), while the mean postoperative Nurick Score was 0.3 (mild radiculopathy) [Table 2]. At two postoperative years, Odom's Criteria revealed 52 excellent, 6 good, 2 fair, and 0 poor outcomes [Table 2]. Of interest, all eight patients in the good/fair groups were heavy smokers, and five of these patients exhibited delayed fusions occurring between 6 and 8 months postoperatively. Analysis of 6-week postoperative SF-36 data revealed minimal improvement on two (Physical Function [PF] and Role Physical [RP]), moderate improvement on four (General Health [GH], Vitality [V], Social Function [SF], and Mental Health [MH]), and marked improvement on two Health Scales (Role Emotional [RE] and Bodily Pain [BP]). At three postoperative months, mild improvement was observed on four (PF, RP, GH, and MH), moderate improvement on two (SF and V), and marked improvement on the remaining two Health Scales (BP and RE). At six postoperative months, two had mild (GH and MH), one had moderate (RP), but five showed marked improvement (PF, BP, V, SF, and RE) on various Health Scales. At 1 year, one had mild (GH), but now seven showed marked improvement (PF, RP, BP, V, SF, RE, and MH) on the varied Health Scales. Finally, at 2 years postoperatively, patients demonstrated marked improvement on all eight Health Scales; presented in descending order these included BP (50.8), RE (45.2), SF (36.1), RP (33.7), V (33), PF (29.2), MH (21.8), and GH (15.3).
Table 2.
Surgeon-based outcome data (Nurick Grades, Odom's Criteria), time to fusion, and length of stay
Of interest, patients demonstrated the greatest postoperative improvement on the BP health scale by the sixth postoperative week; BP increased from the preoperative baseline of 25.9 to 52.5. Although further increases were observed between 3 months and 2 years postoperatively (56.6 at 3 months, 58.0 at 6 months, 70.5 at 1 year, and 76.7 at 2 years), the largest gains occurred early on (6 weeks; Table 3).
Table 3.
Short-Form 36 (SF-36) outcome data for 60 patients undergoing single-level anterior diskectomy and fusion
Fusion Rates
Utilizing both dynamic X-rays and 2D-CT studies, the average time to fusion was 3.8 months (range 2.5-8 months) [Table 2; Figures 3–5]. Although pseudarthrosis was not documented, five (8.3%) patients who had been heavy smokers (2 packs/day > 10 years) exhibited delayed fusions occurring between 6 and 8 months postoperatively: three at 6 months, one at 7 months, and one at 8 months respectively. Of note, all five patients remained braced (cervicothoracic orthoses) until fusion was documented on both 2D-CT and dynamic X-ray studies.
Complications
There were two major and three minor complications in this series. Major complications included one vertebral artery injury (successfully embolized without sequelae) and one cerebrospinal fluid fistula (adequately treated with duragen/fibrin sealant without shunting); both occurred in patients with OPLL. Three minor complications occurred: [1] an obese patient required elective plate revision 3 weeks postoperatively due to low positioning of inferior screws, [2] a second patient developed a transient deltoid paresis which spontaneously resolved within 3 months, and [3] one patient was minimally symptomatic from a mild pulmonary embolism which was successfully managed with an inferior vena cava [IVC] filter without anticoagulation.
DISCUSSION
High fusion rates have been observed for 1-ACDF utilizing different grafts and/or fixed and dynamic plates. In Fraser et al.'s meta-analylsis of the literature, which included 21 papers [involving at least 25 cases/study with a minimum 1-year follow-up], the overall fusion rate was 89.5% (2682 patients).[6] The fusion rate for single-level anterior diskectomy alone was 84.9%, for 1-ACDF was 92.1%, and for plated 1-ACDF was 97.1%. In Kaiser et al.'s study, the fusion rate for single-level fixed-plated ACDF (Orion and Atlantis Plates [Medtronic, Memphis, TN, USA] and Codman Plates [Codman and Shurtleff, Inc., Raynham, MA, USA]) was 96% compared with a lesser 90% fusion rate for nonplated 1-ACDF.[7] In the Samartzis et al. series, the fusion rate was 100% for patients undergoing 1-ACDF using fixed plates (Orion; Medtronic) with allograft compared with a 90.3% fusion rate for fixed plate/autograft (note that the difference in fusion rates was not considered significant).[10] In a 1-ACDF study, utilizing dense cancellous allograft and dynamic ABC plates (Aesculap), which utilized a slotted plate design to allow for 10 mm of cephalad/caudad screw migration, a 96% fusion rate was achieved (66 patients).[1] In a prospective randomized study that included 1-ACDF (28 patients) and 2- to 3-level ACDF (38 patients), half of the patients received dynamic plates, while the other half received static plates; the plate type (static versus dynamic) did not impact fusion rates for 1-ACDF, while dynamic plates appeared to contribute (although not significantly) to higher fusion rates for the multilevel group.[9] In this study, utilizing dynamic ABC plates with autograft, a fusion rate of 100% was achieved utilizing both dynamic X-ray and 2D-CT studies. Statistically, there was no significant difference in the fusion rates for this study compared with the others cited.
Outcomes
Typically, comparable outcomes have been reported utilizing varied grafts and/or plating systems for performing 1-ACDF. Good/excellent outcomes were observed in 91.3% of patients undergoing 1-ACDF with (31 patients) or without (38 patients) fixed/semiconstrained plates.[10] Comparable good/excellent outcomes were achieved: excellent 19.7%, good 71.2%, and fair 9.1%.[10] Although comparable long-term outcomes were also observed following 1-ACDF performed utilizing rhBMP-2 (Medtronic's AMPILFY rhBMP-2 [INFUSE])/ polyetheretherketone (PEEK) cages (Depuy Spine, Raynham, MA, USA), in 22 patients and allograft spacers/demineralized bone matrix (DBM), in 24 patients, the threefold greater cost and incidence of severe postoperative dysphagia (1–6 postoperative weeks) associated with rhBMP-2/PEEK cages prompted the authors to abandon this construct.[11] In another study, comparable 1-year postoperative outcomes (visual analog scale [VAS], and SF-12 (12 physical and mental health scales of SF-36)) results were reported utilizing four different constructs to perform 1-ACDF: (1) fixed plates and autograft, (2) fixed plate, cage, and bone substitute, (3) cage only, and (4) disc arthroplasty.[2] In this 1-ACDF dynamic-plated series, adequate 2-year postoperative outcomes were demonstrated. Patients exhibited only mild residual radiculopathy (Nurick Score of 0.3), while they improved utilizing Odom's Criteria (58 of 50 excellent/good) [Table 2]. SF-36 data at 6 weeks and 3 months revealed marked improvement on two Health Scales (RE and BP; Table 3). By six postoperative months, patients demonstrated marked improvement on five Health Scales (PF, BP, V, SF, and RE), which increased to seven at 1 year (PF, RP, BP, V, SF, RE, and MH), and all eight at 2 years. These outcome measures did not indicate statistical superiority to results attained in the other studies cited.
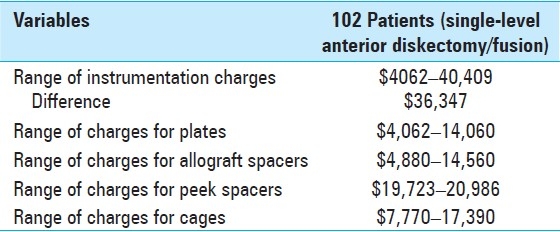
Cost Data
Although 1-ACDF is one of the most frequently performed cervical operations in the USA, few studies focus on the cost-effectiveness of different types of plates, spacers (autograft, allograft, wire mesh, and PEEK), and bone graft supplements (bone morphogenic protein [BMP], DBM, and beta tricalcium phosphate [B-TCP]). One series determined comparable costs for three different types of 1-ACDF spacers/constructs ((1) plate/cage/bone substitute, (2) cage alone, and (3) disc arthroplasty); the fourth plate/iliac autograft construct, although utilizing less costly instrumentation, proved to be less cost-effective due to a longer length of stay (LOS; 5 days).[2] In a second 1-ACDF study, the costs/effectiveness of autograft spacer/cervical spine locking plates (CSLP; Synthes North America, West Chester, PA, USA), placed in 26 patients, were compared with the the Syncage C (Titanium Box, Synthes, Paoli, PA, USA) filled with autograft cancellous bone/CSLP, utilized in 27 patients; the higher cost for the cages was counterbalanced by the shorter operative times and shorter LOS for these constructs compared with autograft/CSLP.[8] In a third 1-ACDF study utilizing cage/mesh/autograft cancellous bone/plate (27 patients) versus iliac autograft spacer/plate (27 patients), operative costs proved comparable; the operative time saved by avoiding iliac crest bone harvesting was negated by the increased cost of the cage.[4] Two other studies documented that utilizing BMP/INFUSE as a bone graft supplement for 1-ACDF spacers was not cost-effective, as it markedly exacerbated postoperative dysphagia, prolonged the LOS, and increased operative costs.[3,11]
In a separate study, Epstein et al. analyzed instrume-ntation charges (charges to the insurer by the hospital; not the actual original costs of these items) for performing 102 single-level ACDF performed by 15 different surgeons at a single institution in 2008.[5] All patients had a single diagnosis related group (DRG 473), a single principal procedure code (81.02), and had either myelopathy (22 patients; 722.72) or radiculopathy (80 patients; 722.3) without comorbidities. Instrumentation charges for these 102 patients ranged from $4062 to $40,409, a 10-fold difference in charges (a difference of $36,347; Table 4).[5] The instrumentation charge for the author's single patient in that series was the lowest at $4062 for a dynamic plate and four screws accompanied by an autograft. Other surgeons utilized various combinations of plates and spacers (allograft, PEEK, cages), which contributed to the near 10-fold difference in operative charges [Table 4].[15]
Table 4.
Summary of cost data from series of 102 patients undergoing single-level anterior diskectomy and fusion at one institution[11]
SUMMARY OF CONTROVERSY
As society focuses on the rising costs of medical care, we as spine surgeons should more actively participate in correlating costs of the different instrumentation systems/constructs with fusion rates and outcomes. The aim of this study was to reaffirm the value of iliac crest autograft and dynamic plates in performing 1-ACDF, a construct which produced more than adequate outcomes and fusion rates but at a lesser cost. Although major economic interests may promote other more expensive plates (constrained [fixed] or semiconstrained) and spacers, the focus should remain on quality of outcomes, fusion rates, and cost containment.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/9/76146
REFERENCES
- 1.Balabhadra R, Kim DH, Zhang HY. Anterior cervical fusion using dense cancellous allografts and dynamic plating. Neurosurgery. 2004;54:1405–11. doi: 10.1227/01.neu.0000125543.38952.87. [DOI] [PubMed] [Google Scholar]
- 2.Bhadra AK, Raman AS, Casey AT, Crawford RJ. Single-level cervical radiculopathy: Clinical outcome and cost-effectiveness of four techniques of anterior cervical discectomy and fusion and disc arthroplasty. Eur Spine J. 2009;18:232–7. doi: 10.1007/s00586-008-0866-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buttermann GR. Prospective nonrandomized comparison of an allograft with bone morphogenetic protein versus an iliac-crest autograft in anterior cervical diskectomy and fusion. Spine J. 2008;8:426–35. doi: 10.1016/j.spinee.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Castro FP, Jr, Holt RT, Maid M, Whitecloud TS., 3rd A cost analysis of two anterior cervical fusion procedures. J Spinal Disord. 2000;13:511–4. doi: 10.1097/00002517-200012000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Epstein NE, Schwall GS, Reilley T, Insinna T, Bahnken A, Hood DC. Surgeon choices, and the choice of surgeons, affect total hospital charges for single-level anterior cervical surgery. Spine. 2010 doi: 10.1097/BRS.0b013e3181e6c4d8. [in press] [DOI] [PubMed] [Google Scholar]
- 6.Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: A meta-analysis of fusion rates. J Neurosurg Spine. 2007;6:298–303. doi: 10.3171/spi.2007.6.4.2. [DOI] [PubMed] [Google Scholar]
- 7.Kaiser MG, Haid RW, Jr, Subach BR, Barnes B, Rodts GE., Jr Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:229–36. doi: 10.1097/00006123-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Kandziora F, Pflugmacher R, Scholz M, Schnake K, Putzier M, Khodadadyan-Klostermann C, et al. Treatment of traumatic cervical spine instability with interbody fusion cages: A prospective controlled study with 2-year follow-up. Injury. 2005;36:27–35. doi: 10.1016/j.injury.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 9.Nunley PD, Jawahar A, Kerr EJ, 3rd, Cavanaugh DA, Howard C, Brandao SM. Choice of plate may affect outcomes for single versus multilevel ACDF: Results of a prospective randomized single-blind trial. Spine J. 2009;9:121–7. doi: 10.1016/j.spinee.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Samartzis D, Shen FH, Goldberg EJ, An HS. Is autograft the gold standard in achieving radiographic fusion in one-level anterior cervical discectomy and fusion with rigid anterior plate fixation? Spine. 2005;30:1756–61. doi: 10.1097/01.brs.0000172148.86756.ce. [DOI] [PubMed] [Google Scholar]
- 11.Vaidya R, Carp J, Sethi A, Bartol S, Craig J, Les CM. Complications of anterior cervical diskectomy and fusion using recombinant human bone morphogenetic protein-2. Eur Spine J. 2007;16:1257–65. doi: 10.1007/s00586-007-0351-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


