Abstract
Background:
Pituitary abscess is an extremely rare finding. The abscess may arise as a primary pituitary lesion or be associated with parasellar pathology. It is important for pituitary abscess treatments to perform early diagnosis. In this report, we describe a case of pituitary adenoma in which MRI findings changed during the follow-up period and strongly suggested progression to pituitary abscess arising from adenoma.
Case Description:
In a 73-year-old female, pituitary adenoma had been incidentally detected; MRI showed typical findings of pituitary adenoma, and we had followed up the pituitary lesion and clinical symptoms. Six months later, she had oculomotor nerve palsy and symptoms of hypopituitarism. Hematological examination revealed inflammation and hypopituitarism. MRI showed striking changes in the signal intensity of the pituitary lesion, and strongly suggested occurrence of sinusitis and pituitary abscess ascribed to pituitary adenoma. She was admitted and endoscopic transsphenoidal surgery was performed. The sellar floor was destroyed, and yellowish-white creamy pus was observed. A histopathological study using hematoxylin-eosin staining showed adenoma and inflammatory cells. Aerobic, anaerobic, and fungal cultures were negative. Antibiotics were administered and hormonal replacement was started. Neurological and general symptoms were improved, and postoperative MRI revealed complete evacuation of abscess and removal of tumor.
Conclusions:
Pituitary abscess within invasive pituitary adenoma is a rare entity, and shows high mortality. Early diagnosis of pituitary abscess is very important for the prompt surgery and initiation of treatment with antibiotics. In our case, changes in MRI findings were helpful to diagnose pituitary abscess, and endoscopic transsphenoidal surgery was an optimal surgical treatment.
Keywords: Endoscopic transsphenoidal surgery, pituitary abscess, MRI findings
INTRODUCTION
Pituitary abscess is an extremely rare finding. Some reports described finding pituitary abscess as a primary pituitary lesion or be associated with an underlying parasellar pathology, such as pituitary adenomas,[1–13,19–21] Rathke's cleft cyst,[1,9,14,17–19] and craniopharyngioma.[15,19] But there were few cases that confirmed changes in MRI findings before and after abscess formation.[11] In this report, we described a case of abscess formation within invasive pituitary adenoma. In our case, typical findings of pituitary adenoma were detected on MRI before abscess formation, and it useful for diagnosis of pituitary abscess that changes of MRI findings and clinical symptoms.
CASE REPORT
In a 73-year-old female, pituitary adenoma had been incidentally detected, and she had been followed up as an outpatient at our neurosurgery department. Magnetic resonance imaging (MRI) showed solid intra- and suprasellar lesions with hypoenhancement after the administration of the contrast medium [Figure 1]. We had followed up the pituitary lesion and clinical symptoms because she refused surgical treatment at first.
Figure 1.
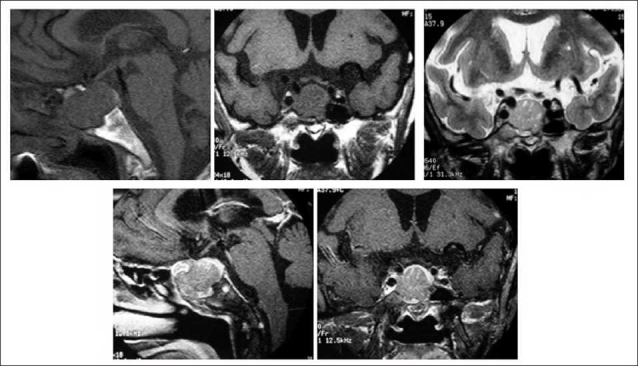
Magnetic resonance images obtained for the initial diagnostic determination of pituitary adenoma. Upper left and center: T1-weighted images, upper right: T2-weighted image, lower right and center: T1-weighted images after administration of contrast medium.
Six months later, she had bilateral ophthalmoplegia, and ptosis and diplopia in the right eye. Symptoms were worsened, and she started to have general fatigue. She had no history of diabetes mellitus, immunosuppression, malignancy, or head trauma.
Neurological examination revealed ptosis and restricted eye movement in the right eye caused by oculomotor and abducens nerve paralysis. Pupils were equal (3 mm), and light reflex was bilaterally prompt. Papilledema was not seen on examination of the fundi. Impairment of visual acuity and bitemporal hemianopsia were detected. She had no sensory or motor deficit, or meningeal signs.
Hematological examination showed that hemoglobin and hematocrit were normal, and white blood cells were 11.7 (1000/μl) with 88.84% neutrophils and 8.19% lymphocytes. C-reacted protein was 14.3 mg/dl. Endocrinological examination revealed 4.8 pg/ml adrenocorticotropic hormone (ACTH), 0.274 μIU/ml thyroid stimulating hormone (TSH), 0.74 pg/ml free T3, 0.74 ng/ml free T4, 0.05 ng/ml growth hormone (GH), 40 ng/ml insulin-like growth factor-1 (IGF-1), and 9.79 ng/ml prolactin (PRL).
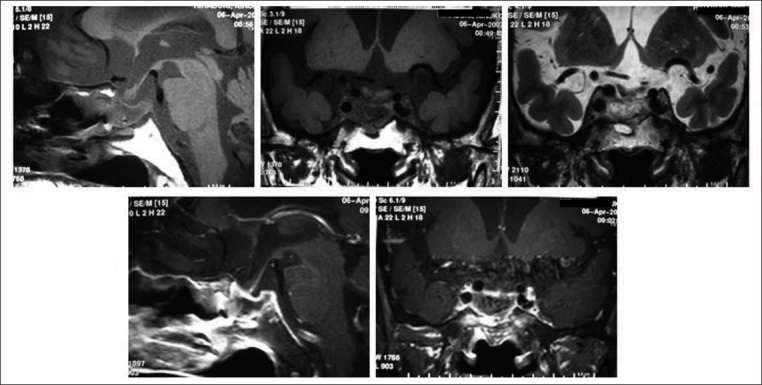
The X-ray craniogram showed ballooning of the sella turcica and cloudiness of the sphenoid sinus. Computed tomography (CT) revealed the intra- and suprasellar enhanced mass lesion, and the bone image showed a defect of the sellar floor and extension of the pituitary lesion toward the sphenoid sinus. MRI showed striking changes in the signal intensity of the pituitary enhanced lesion: low intensity on the T1-weighted image and isointensity on the T2-weighted image. After the administration of the contrast medium, the prominent rim enhancement extending toward the sphenoid sinus was seen [Figure 2]. These findings differed from those of previous MRI. Clinical symptoms and the result of laboratory examinations and MRI findings strongly suggested of sinusitis and pituitary abscess associated with pituitary adenoma.
Figure 2.
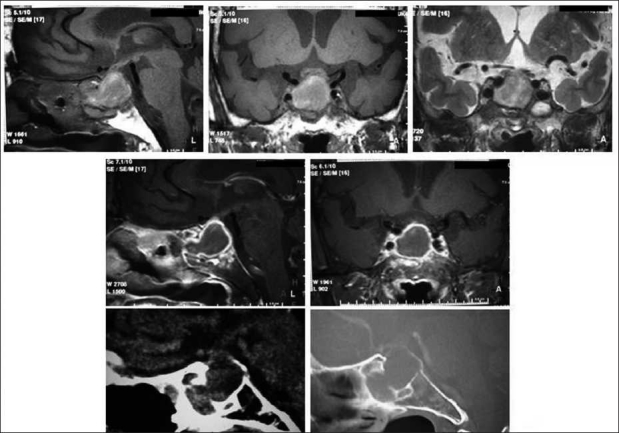
Magnetic resonance images and CT images after neurological and hormonal symptoms appeared. Upper left and center: T1-weighted images, upper right: T2-weighted image. Middle left and center: T1 weighted images after administration of contrast medium showing enhancement of the outline of sellar lesion. Lower left and center: CT image showing intra- and supra-sellar enhanced mass lesions, defect of the sella floor, and extension of the pituitary lesion toward the shpenoid sinus.
Transsphenoidal surgery was performed. The intrasphenoidal mucosa was thickened, and purulent materials were seen. The sellar floor was destroyed and yellowish-white creamy pus was observed [Figure 3]. The pus was taken for cultures, and the abscess and tumor were almost totally excised.
Figure 3.
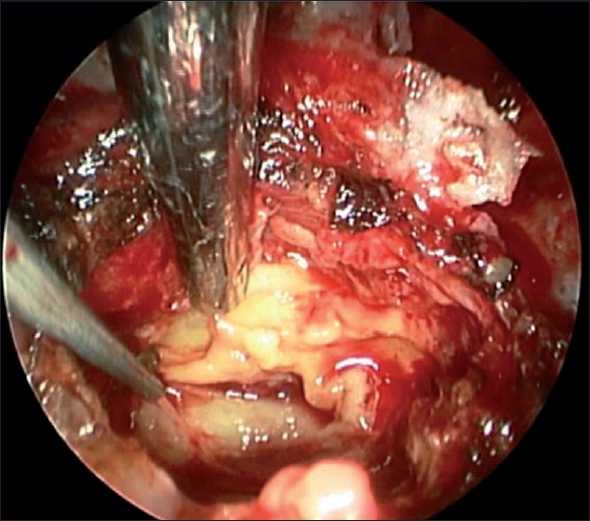
Intra-operative endoscopic view. The lesion consisted of the yellowish-white thick creamy pus extending toward the sphenoid sinus through the defect of sellar floor.
A histopathological study with hematoxylin and eosin staining revealed hypostaining adenoma cells with round nuclei and acidophilic cytoplasm, and inflammatory cells [Figure 4]. Pathological diagnosis was null cell adenoma, because immunohistochemistry was negative for ACTH, FSH, LH, PRL, TSH, and GH. Aerobic, anaerobic, and fungal cultures were negative. Antibiotics were administered before surgery and were continued for 4 weeks. She also received hormonal replacement therapy. Neurological and general findings were improved, and MRI revealed complete evacuation of abscess and removal of the tumor [Figure 5].
Figure 4.
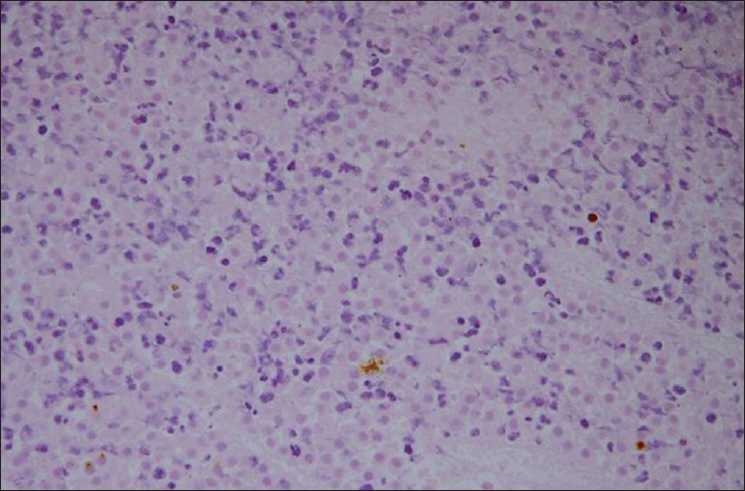
Microphotogram: Histopathology suggestive of pituitary adenoma with inflammatory cells. Hormonal immunohistochemistry was negative (H & E, ×200).
Figure 5.
Magnetic resonance images after treatment. Upper right and center: T1-weighted images, upper left: T2-weighted image, lower right and center: T1-weighted images after administration of contrast medium. Abscess and tumor were almost totally excised.
DISCUSSION
Pituitary abscess is a rare clinical entity. The abscess may arise as a primary pituitary lesion or be associated with an underlying parasellar pathology, such as pituitary adenomas,[1–13,19–21] Rathke's cleft cyst,[1,9,14,17–19] and craniopharyngioma.[15,19] The first report of pituitary abscess associated with pituitary adenoma was described by Whalley[20] in 1952 as an autopsy finding. In 1998 Jadhav[8] first described abscess formation in invasive pituitary adenoma in the MRI era. The abscess presented as a sellar lesion with a low-intensity signal on a T1-weighted image and a high-intensity signal on a T2-weighted image which indicated a cystic lesion, but other lesions such as necrotic lesions can also show this presentation. Therefore, diagnosis of pituitary abscess is difficult, even with the help of MRI. However, retrospective analysis in our case may offer useful information to diagnose the abscess formation correctly. The finding on MRI was the enhancement of the outline of the sellar lesion after the administration of the contrast medium. Ten previous reports[1–3,6,8,10,11,16,17,19] have described this MRI finding within a preexisting sellar lesion supporting our impression for an abscess formation in our case.
In our case, typical findings of pituitary adenoma were detected on MRI before abscess formation, and changes in MRI findings and clinical symptoms strongly suggested the occurrence of inflammatory changes at the parasellar lesion. In addition, the finding of the destruction of the sellar floor on CT indicated inflammation spread from the sphenoid sinus. Kroppenstedt et al.[11] reported changes in MRI findings before and after abscess formation. To our knowledge, our case was the second report, and was more valuable because changes in MRI findings before and after inflammatory findings of pituitary abscess could have been observed.
The recommendations of pituitary abscess management are surgical drainage, administration of antibiotics, and hormonal replacement.[19] Most of the reported cases have been treated by transsphenoidal surgery. Transsphenoidal surgery is considered to be the preferred approach, because it provides a line for prolonged drainage from the infected area, decompression of the optic chiasma, and management of an associated sinusitis if present.[1–4,12–14,21] We used an endoscopic endonasal transsphenoidal approach to treat pituitary abscess. This approach permitted a direct look into surgical anatomy, and gave better magnification and visualization of the hidden zone using a 30° or 70° angled scope. Craniotomy was considered to increase the risk of contaminating the cerebrospinal fluid causing intracranial inflammation.
The administration of antibiotics should be started preoperatively if pituitary abscess is suspected. An appropriate and more specific antibiotic or antifungal agent should be administered and continued for 4-6 weeks.[19]
Panhypopituitarism is usually seen in patients with pituitary abscess. The replacement of hormones, particularly corticosteroids, is necessary.[9] Diabetes insipidus may complicate the management of patients with pituitary abscess, but its presentation is usually transient if it is not preexisting.
In conclusion, pituitary abscess within invasive pituitary adenoma is a rare entity and shows high mortality. Early diagnosis of pituitary abscess is very important for prompt surgery and initiation of treatment with antibiotics. In our case, changes in MRI findings were helpful to diagnose pituitary abscess, and endoscopic transsphenoidal surgery was an optimal surgical treatment.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/3/76140
Contributor Information
Atsushi Kuge, Email: akuge@med.id.yamagata-u.ac.jp.
Shinya Sato, Email: sinsato@med.id.yamagata-u.ac.jp.
Sunao Takemura, Email: stakemur@med.id.yamagata-u.ac.jp.
Kaori Sakurada, Email: kasakura@med.id.yamagata-u.ac.jp.
Rei Kondo, Email: rkondo@saiseikan.jp.
Takamasa Kayama, Email: nouge@mws.id.yamagata-u.ac.jp.
REFERENCES
- 1.Bognar L, Szeifert T, Fedorcsak I, Pasztor E. Abscess formation in Rathke's cleft cyst. Acta Neurochir (Wien) 1992;117:70–3. doi: 10.1007/BF01400640. [DOI] [PubMed] [Google Scholar]
- 2.Bossard D, Himed A, Badet C, Lapras V, Mornex R, Fisher G, et al. MRI and CT in a case of pituitary abscess. J Neuroradiol. 1992;19:139–44. [PubMed] [Google Scholar]
- 3.Ciappetta P, Calace A, D'Urso PI, Candia ND. Endoscopic treatment of pituitary abscess: Two case reports and literature review. Neurosurg Rev. 2008;31:237–46. doi: 10.1007/s10143-007-0096-2. [DOI] [PubMed] [Google Scholar]
- 4.Domingue JN, Wilson CB. Pituitary abscess. J Neurosurg. 1977;46:601–8. doi: 10.3171/jns.1977.46.5.0601. [DOI] [PubMed] [Google Scholar]
- 5.Hammann HV. Abscess formation in the pituitary fossa associated with a pituitary adenoma. J Neurosurg. 1956;13:208–10. doi: 10.3171/jns.1956.13.2.0208. [DOI] [PubMed] [Google Scholar]
- 6.Hatiboglu MA, Iplikcioglu A, Ozcan D. Abscess formation within invasive pituitary adenoma. J Clin Neurosci. 2006;13:774–7. doi: 10.1016/j.jocn.2005.11.031. [DOI] [PubMed] [Google Scholar]
- 7.Holck S, Laursen H. Prolactinoma coexistent with granulomatous hypophysitis. Acta Neuropathol (Berl) 1983;61:253–7. doi: 10.1007/BF00691994. [DOI] [PubMed] [Google Scholar]
- 8.Jadhav RN, Dahiwadkar HV, Palande DA. Abscess formation in invasive pituitary adenoma case report. Neurosurgery. 1998;43:616–9. doi: 10.1097/00006123-199809000-00124. [DOI] [PubMed] [Google Scholar]
- 9.Jain KC, Varma A, Mahapatra AK. Pituitary abscess: A series of six cases. Br J Neurosurg. 1997;11:139–43. doi: 10.1080/02688699746492. [DOI] [PubMed] [Google Scholar]
- 10.Jaiswal AK, Mahapatra AK, Sharma MC. Pituitary abscess associated with prolactinoma. J Clin Neurosci. 2004;11:533–4. doi: 10.1016/j.jocn.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Kroppenstedt SN, Liebig T, Mueller W, Graf KJ, Lanksch WR, Unterberg AW. Secondary abscess formation in pituitary adenoma after tooth extraction , J Neurosurg. 2001;94:335–8. doi: 10.3171/jns.2001.94.2.0335. [DOI] [PubMed] [Google Scholar]
- 12.Lindholm J, Rasmussen P, Korsgaard O. Intrasellar or pituitary abcess. J Neurosurg. 1973;38:616–9. doi: 10.3171/jns.1973.38.5.0616. [DOI] [PubMed] [Google Scholar]
- 13.Nelson PB, Haverkos H, Martinez AJ, Robinson AG. Abscess formation within pituitary adenoma. Neurosurgery. 1983;12:331–3. doi: 10.1227/00006123-198303000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Obenchain TG, Becker DP. Abscess formation in a Rathke's cleft cyst case report. J Neurosurg. 1972;36:359–62. doi: 10.3171/jns.1972.36.3.0359. [DOI] [PubMed] [Google Scholar]
- 15.Obrador S, Blazquez MG. Pituitary abscess in a craniopharyngioma case report. J Neurosurg. 1972;36:785–9. doi: 10.3171/jns.1972.36.6.0785. [DOI] [PubMed] [Google Scholar]
- 16.Shono T, Nishio S, Muratani H, Yasuda T, Fukui M, Moutai K. Pituitary abscess secondary to isolated spheoid sinusitis. Minim Invas Neurosurg. 1999;42:204–6. doi: 10.1055/s-2008-1053400. [DOI] [PubMed] [Google Scholar]
- 17.Takayasu T, Yamasaki F, Tominaga A, Hidaka T, Arita K, Kurisu K. A pituitary abscess showing high signal intensity on diffuision-weighted imaging. Neurosurg Rev. 2006;29:246–8. doi: 10.1007/s10143-006-0021-0. [DOI] [PubMed] [Google Scholar]
- 18.Thomas N, Wittert GA, Scott G, Reilly PL. Infection of an Rathke's cleft cyst: A rare cause of pituitary abscess. J Neurosurg. 1998;89:682. doi: 10.3171/jns.1998.89.4.0682. [DOI] [PubMed] [Google Scholar]
- 19.Vates GE, Berger MS, Wilson CB. Diagnosis and management of pituitary abscess: A review of twenty-four cases. J Neurosurg. 2001;95:233–41. doi: 10.3171/jns.2001.95.2.0233. [DOI] [PubMed] [Google Scholar]
- 20.Whalley N. Abscess formation in a pituitary adneoma. J Neurol Neurosurg Psychiat. 1952;15:66–7. doi: 10.1136/jnnp.15.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zorub DS, Martinez AJ, Nelson PB, Lam MT. Invasive pituitary adenoma with abscess formation: Case report. Neurosurgery. 1979;5:718–22. doi: 10.1227/00006123-197912000-00014. [DOI] [PubMed] [Google Scholar]


