Abstract
This randomized controlled pilot study compared a cognitive-behavioral therapy (Seeking Safety; SS) plus treatment-as-usual (TAU) to TAU-alone in 49 incarcerated women with substance use disorder (SUD) and posttraumatic stress disorder (PTSD; full or subthreshold). Seeking Safety consisted of a voluntary group treatment during incarceration and individual treatment after prison release. TAU was required in the prison and comprised 180 to 240 hours of individual and group treatment over 6 to 8 weeks. Assessments occurred at intake, 12 weeks after intake, and 3 and 6 months after release from prison. There were no significant differences between conditions on all key domains (PTSD, SUD, psychopathology, and legal problems); but both conditions showed significant improvements from intake to later time points on all of these outcomes across time. Secondary analyses at follow-up found trends for SS participants improving on clinician-rated PTSD symptoms and TAU participants worsening on self-reported PTSD symptoms. Also, SS demonstrated continued improvement on psychopathology at 3 and 6 months, whereas TAU did not. However, alcohol use improved more for TAU during follow-up. Satisfaction with SS was high, and a greater number of SS sessions was associated with greater improvement on PTSD and drug use. Six months after release from prison, 53% of the women in both conditions reported a remission in PTSD. Study limitations include lack of assessment of SS outcomes at end of group treatment; lack of blind assessment; omission of the SS case management component; and possible contamination between the two conditions. The complex needs of this population are discussed.
In 2005, the number of women incarcerated in state and federal prisons was 106,174, with an increase of 6.1% from 1995 and a 3.4% increase from 2004 (Bureau of Justice Statistics, 2005). Rates of incarceration for women continue to rise faster than for men (Bureau of Justice Statistics, 2005). In part, drug offenses have contributed to the rise in incarceration of women (Bureau of Justice Statistics, 2002). Furthermore, half of incarcerated women were under the influence of alcohol or drugs at the time of their criminal offense (Bureau of Justice Statistics, 2000), and studies have shown substantially higher prevalence rates of substance use disorder (SUD) among women in prison than women in the community (Jordan, Schlenger, Fairbank, & Caddell, 1996). In addition to SUD, many women offenders also meet criteria for a mental disorder (Jordan et al., 1996; Pelissier & O’Neil, 2000; Teplin, Abram, & McClelland, 1996) and report histories of trauma (Alexander, 1996). Many women in prison-based substance abuse treatment meet criteria for current (50%) or lifetime (60%) posttraumatic stress disorder (PTSD) (Kubiak, 2004; Zlotnick, Najavits, Rohsenow, & Johnson, 2003).
In general, prison-based treatment programs, including cognitive-behavioral programs, have been found to reduce posttreatment recidivism and drug use (Knight, Simpson, & Hiller, 1999; Pelissier, Motivans, & Rounds-Bryant, 2005). Unfortunately, most treatment studies have focused exclusively on men. Several authors have expressed concerns that substance abuse programs for women prisoners may not target the unique needs of incarcerated women or address their pervasive experience of abuse and victimization (e.g., Bloom, Owen, & Covington, 2003; Mosher & Phillips, 2006).
Although the needs of incarcerated women with PTSD and SUD are profound, few treatments for this population have been developed or tested (Battle, Zlotnick, Najavits, & Winsor, 2002). One of the only studies to examine the efficacy of a prison-based treatment program in women with comorbid PTSD and SUD was an open, uncontrolled pilot trial of Seeking Safety (SS) as an adjunct to treatment-as-usual (TAU) (Zlotnick et al., 2003). In that study, 17 incarcerated women with PTSD and SUD who received SS showed significant improvement in PTSD symptoms at the end of treatment, which was maintained 3 months after release from prison; moreover, their severity of substance use and legal problems showed significant improvements at 6 weeks after release from prison. The women also reported a high degree of satisfaction with treatment. Although this treatment approach appears promising for incarcerated women with comorbid PTSD and SUD, there is a need for further scientific testing. For example, without a control condition, it is not possible to determine whether gains from SS are higher than among women who do not receive it. To address this issue, the current randomized controlled pilot trial (RCT) compared the efficacy of SS as an adjunct to TAU compared to TAU-alone in a sample of incarcerated women with current comorbid PTSD and SUD. This study extended the treatment to the period after release from prison because post-release participation in mental health treatment has been found to decrease women’s substance use (Pelissier et al., 2001). Inmates newly released from prison are known to face multiple challenges, such as simultaneous recovery and reentry into society, return to high-risk drug neighborhoods, and families that may offer little support for continued involvement in treatment (Barthwell et al., 1995; Peters, Strozier, Murrin, & Kearns, 1997), all of which place these women at high risk for relapse (Osher, Steadman, & Barr, 2003). Although aftercare appears to be crucial for individuals who have received in-prison drug treatment, Pelissier, Jones, and Cadigan (2007), in a review of drug treatment aftercare in the criminal justice system, concluded that much more research is needed to support this claim. Furthermore, this research should include multiple outcome measures and specify the exact nature of the aftercare services.
We elected to test SS for two reasons. First, it evidenced positive results in our earlier prison-based pilot trial, including high acceptability among both clients and the prison warden and staff (Zlotnick et al., 2003). Second, it is the only model that is established as effective for comorbid PTSD and SUD (per the criteria of Chambless & Hollon, 1998, for example). It has outperformed TAU in all four trials in which it has been compared to that treatment condition (Desai, Harpaz-Rotem, Najavits, & Rosenheck, 2008; Gatz et al., 2007; Hien, Cohen, Miele, Litt, & Capstick, 2004; Najavits, Gallop, & Weiss, 2006). One of these was a multisite trial (Desai et al.), and two were RCTs (Hien et al., 2004; Najavits et al., 2006). It has also evidenced positive outcomes in a wide variety of uncontrolled pilot studies. In every study thus far (both pilot studies and controlled trials), it has evidenced significant reductions in substance use, PTSD or trauma-related symptoms, as well as other domains (for a review see Najavits, 2007). Most of these were studies represented vulnerable populations, such as clients in community treatment, low-income urban clients, homeless persons, and veterans).
The current study thus had two main goals: (1) to evaluate outcomes of SS plus TAU to TAU-alone in an incarcerated sample on key variables (PTSD diagnosis, substance use, prison recidivism, legal problems, and psychopathology), and (2) to understand more about treatment outcomes for women in prison with PTSD and SUD. This is the first known study to address both questions using a prospective design.
Method
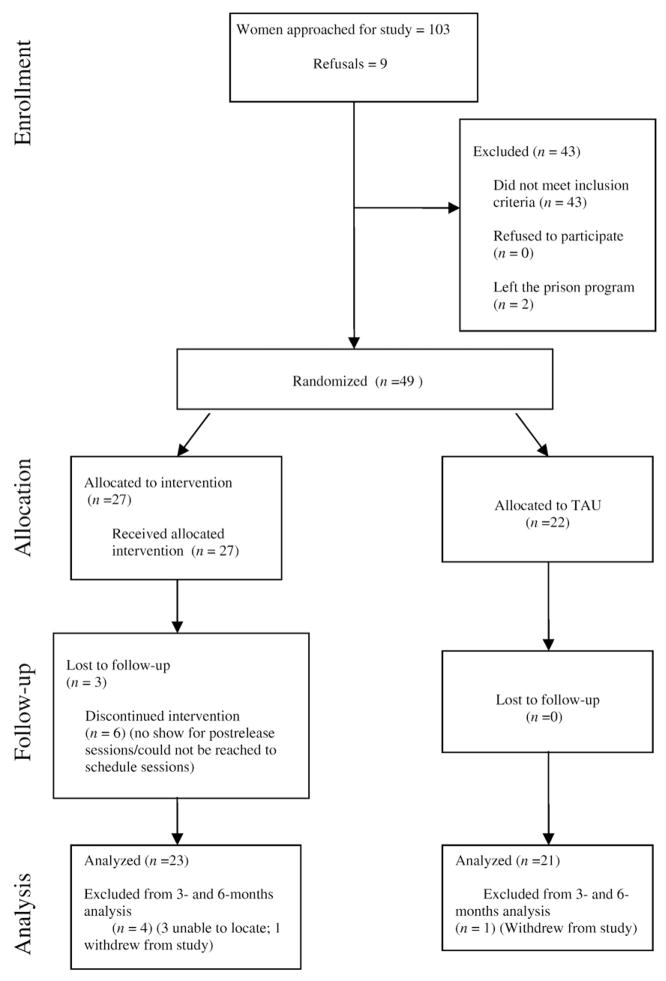
Women were recruited from a residential substance abuse treatment program in a minimum security wing of a women’s prison. Admission to the in-prison treatment program is voluntary and those admitted to the program are female inmates who request intensive substance abuse treatment. All participants provided informed consent to participate in the study. The study was approved by the Institutional Review Board (IRB) of Butler Hospital, the IRB of the prison’s substance use treatment provider, and the prison’s Medical Research Advisory Group. Women who were scheduled to be released from prison within 12 to 16 weeks were approached to be in the study. Of the 103 women approached, 94 women (91%) consented to participate in the study. Of these 94 women, 45 (48%) women were excluded (see Fig. 1). Two women left the substance abuse treatment program prior to randomization. The remaining 43 did not meet inclusion criteria, that is, DSM-IV criteria for current PTSD or subthreshold PTSD (i.e., had at least one symptom from all three clusters that were associated with impairment/distress) within the previous month as determined by the Clinician-Administered Posttraumatic Stress Disorder Scale-I (CAPS-I; Blake et al., 1990) or did not meet DSM-IV criteria for substance dependence one month prior to entering prison per the Structured Clinical Interview for DSM-IV—Patient Version (SCID; First, Spitzer, Gibbon, & Williams, 1996). Women were also excluded if they were actively psychotic (hallucinating or delusional) at the time of recruitment, could not understand English well enough to understand the consent form or measures, or were diagnosed with organic brain impairment. The remaining 49 (52%) of the women were individually randomized to one of the two conditions, after the completion of all study intake measures (see below for details). A simple randomization procedure was used for each cohort of participants (i.e., group of participants who entered the randomized phase of the study at the same time). Each cohort of participants consisted of 5 to 11 women, and there were 7 cohorts of participants.
FIGURE 1.
Flow of Participants through Each Stage of the Study.
SEEKING SAFETY
SS sessions were provided on a voluntary basis (i.e., joining the treatment per se and attendance at sessions). It was offered in addition to required TAU; SS sessions were conducted when TAU sessions were not meeting. (TAU is described below in more detail.) Study participants were paid for completing assessments but not for attending treatment sessions. Clinicians were substance use counselors in the prison (not hired or selected specifically for SS) with varying levels of prior training. Three female clinicians conducted SS under supervision by an associate of Lisa Najavits (who authored Seeking Safety, 2002, and who consulted with the associate during the trial). An additional female clinician served as co-leader for one group cohort. The supervisor conducted twice-monthly telephone supervision and reviewed one taped session for each phone call. The primary goals of SS are psychoeducation and the development of coping skills to help clients attain safety from both PTSD and SUD; it is present-focused, abstinence-oriented, and emphasizes an empowering, compassionate approach (for a detailed description of the treatment see Najavits, 2002, and www.seekingsafety.org). SS was conducted in group modality for 90 min, typically three times a week for 6 to 8 weeks while the women were in prison, with three to five women per group. After release from prison, each woman in SS was offered weekly individual 60-min “booster” sessions for 12 weeks to reinforce material from the group sessions. The clinician and client decided which topic from SS to cover at each booster session. Except for one cohort of women, the clinician who conducted the group conducted the individual booster sessions. These individual sessions were mostly conducted in person. On a few occasions when women were unable to attend in-person sessions, the sessions were conducted by telephone.
TREATMENT AS USUAL
All participants in this study were enrolled in a 28-bed residential substance use treatment program in the minimum security wing (approximately 30 hours per week). Women typically attend this program for 3 to 6 months, depending on the length of their sentences. Substance use treatment was abstinence-oriented, focused on the 12-step model (Alcohol Anonymous, Cocaine Anonymous, Narcotics Anonymous), and took place in a psychoeducational large-group format, with weekly individual case management and drug counseling. To remain in the TAU program, the women had to attend all components of the treatment. Psychoeducational groups included attention to women’s health, domestic violence, affect management, relapse prevention, career exploration, anger management, and parenting, conducted by the same clinicians who conducted the SS treatment. This program did not offer any treatment specifically for trauma. Prior to prison release, the women received case management services, although this discontinued once the women were released from prison. All women leaving prison were referred for further substance use treatment. The TAU program was similar to other state prison substance use programs in that more than 75% of states offer programs in therapeutic community settings, in day treatment settings, teach relapse prevention, and offer substance use education (Taxman et al., 2005), suggesting that findings from this study will be generalizable to other state prisons.
MEASURES
Unless otherwise noted, all measures were collected at study intake, 12 weeks later (which was approximately 1 week prior to prison release), and at 3 and 6 months after release from prison. Women’s projected release dates could change after study intake, and some women left earlier than anticipated. We attempted to assess all women close to their release from prison to obtain a uniform pre-release assessment. A trained bachelor’s-level research assistant administered all measures. She knew all participants’ treatment assignment.
PTSD
The CAPS-I provided the diagnosis of PTSD and level of PTSD symptoms (a composite score of frequency and severity of PTSD symptoms; Blake et al., 1995). The self-report Trauma Symptom Checklist 40 (TSC-40; Briere, 1996) was also used as it addresses broader trauma-related symptoms. Both measures have strong psychometric properties (e.g., Weathers, Keane, & Davidson, 2001; Zlotnick et al., 1996). To assess for the presence of trauma, a self-report measure, the Trauma History Questionnaire (THQ; Greene, 1995), was administered. The THQ measures the frequency of physical/sexual, general disaster, and crime-related traumas.
Substance use
The SCID was conducted to obtain SUD diagnoses, at intake only. The Addiction Severity Index (ASI; McLellan et al., 1992) composite scores for alcohol and drugs were used to measure severity of use in the prior 30 days. The Time Line Follow Back (TLFB; Sobell, Vanderspek, & Saltman, 1980) addressed frequency of drug and alcohol use in the prior 30 days. Note, however, that for study intake, both substance-related measures were administered for the 30-day time period prior to entering prison to obtain an accurate gauge on the women’s substance use outside of a controlled environment. However, for all follow-up assessments it was assessed for the prior 30 days. The ASI and TLFB have excellent reliability and validity (Fals-Stewart, O’Farrell, Freitas, McFarlin, & Rutigliano, 2000; McLellan et al., 1992; Sobell, Maisto, Sobell, & Cooper, 1979). Reports of drug and alcohol use on the TLFB were summarized into the ratio of days using to days not in a controlled environment (i.e., prison, residential treatment, or detoxification). Ratios were calculated for each of the specified time intervals and for days using drugs or alcohol and days using drugs only. Urine drug screens and breath alcohol tests were completed at 3- and 6-month follow-ups to detect recent use.
Psychopathology
The self-report Brief Symptom Inventory (Derogatis, 1983) was used to obtain an overall evaluation of mental health problems. We used the positive symptom total, which offers strong psychometric properties (Derogatis).
Legal problems
The legal composite score of the ASI assessed for criminal activity in the prior 30 days, including arrests, incarceration, and engagement in criminal activity. At intake, legal problems were assessed for the 30 days prior to entering prison; for both follow-up assessments, they were assessed for the prior 30 days. The score was calculated for all time points except 12 weeks. We also calculated recidivism (return to prison after release), based on the participants’ self-report and the prison’s census.
Treatment utilization
Treatment utilization was assessed at 3- and 6-month follow-ups on the Treatment Services Review (TSR; McLellan et al., 1992), a brief interview with excellent reliability and validity when compared to clinical records.
Seeking Safety measures
SS participants additionally completed the following measures. The Client Satisfaction Questionnaire (Attkisson & Zwick, 1982; scaled 1 to 6, with 6 the highest satisfaction) was given at the end of the SS group treatment (about 6 to 8 weeks after it began) and at the end of the booster sessions (approximately 3 months after release from prison). The End-of-Treatment Questionnaire (Najavits, 2002; to rate the helpfulness of treatment components; scaled −3 to +3) was given twice (after the last group session and after the last individual booster session). The Evaluation of Treatment Interview (Carroll, Kadden, Donovan, Zweben, & Rounsaville, 1994) was given after the last group session to address satisfaction with the clinician and the number of sessions and to identify helpful aspects of the treatment.
To measure clinicians’ adherence to SS, the Seeking Safety Adherence Scale (Najavits & Liese, 2000) was completed by the supervisor based on audiotaped sessions. It assesses clinician performance for adherence (amount of the behavior) and helpfulness (impact of the behavior), scaled 0 to 3. Forty randomly selected SS Adherence Scales were completed by the supervisor.
DATA ANALYSIS
We analyzed all outcomes in two ways. First was the primary outcome analysis. We conducted two versions of this: analyses of covariance (ANCOVA) at 12 weeks, 3 months post-release, and 6 months post-release; and generalized estimating equations (GEE) analysis from intake through 6-months post-release. Covariates were intake scores and age (the latter was covaried because it differed significantly between the two conditions at intake). We were not able to locate 5 women for any of the post-release follow-up assessments; these women’s data were excluded from the ANCOVA and GEE analyses, leaving a sample of 44 women for these analyses. In addition, to better understand the pattern of results, we also conducted paired-samples t-tests (two tailed) for continuous measures and chi-square tests for categorical ones. We focused on total scores for all measures and only report significant results or trends. We include trends due to the relatively small sample size, the likelihood of type II error, and the exploratory nature of this trial given that it is the first in this area. Because substance use rates are affected when women return to prison, substance use outcomes were calculated for the entire sample and for the subsample of women who were not reincarcerated during the follow-up period.
Results
Our sample of 49 women had an average age of 34.6 (SD=7.4), with 46.9% Caucasian, 32.7% African-American, 14.2% Hispanic, and 6.1% other races/ethnicities. Half were high school graduates (53.1%), half had never married (55.1%), and most had been in prison before (89.8%). They had an average of 6.5 previous convictions (SD=6.8), and the felony rate for their current offense was 42.9%. Women had been incarcerated for a mean of 2 months (range 0 – 7) prior to study intake. All of the women reported repeated trauma, with a 93.9% rate of sexual abuse, 89.8% physical abuse, and average age at first trauma of 7.5 (SD=3.2). The mean age of first onset of PTSD was 15.6 (SD=6.7), with 83.5% meeting criteria for full PTSD and 16.5% for subthreshold PTSD. In the month prior to incarceration, the majority of women (87.8%) met criteria for alcohol dependence; another 4.1% met criteria for lifetime alcohol abuse. The percentages of women who had ever used a single substance at a level typically indicating dependence (10 or more times in one month) were 93.9% for cocaine, 75.5% for cannabis, 59.2% for heroin or other opioids, 38.8% for sedatives/hypnotics/anxiolytics, 30.6% for hallucinogens/PCP, and 26.5% for stimulants. Average age of first onset for SUD was 16.9 (SD=4.0) and an average number of months for their longest period of abstinence was 26.7 (SD=37.9) months. Data on interrater reliability were not collected.
Chi-square and independent samples t-tests showed that women in the two treatment conditions did not differ at intake on total CAPS score or the ASI alcohol or drug composite scores. Women in the two conditions also did not differ on any of the variables described in the previous paragraph, except age. Women in SS were 4 years older, on average, than women in TAU (M=36.5 years, SD=7.6 years for SS women vs. M=32.2 years, SD = 6.61 years for TAU women; t[47] = 2.0, p = .046); thus, age served as a covariate in subsequent analyses.
Follow-up data were available for 21 women in TAU and 23 women in SS for a sample of 44 for both the 3- and 6-month post-prison release analyses. Fifteen percent of women in SS and 5% in TAU were unavailable for assessments within the 6 months after release from prison.
COMPLIANCE/SATISFACTION WITH SS
There was a high degree of acceptance of the treatment. Of the women who were approached to participate in the study, 91% agreed to participate. All of the women who were offered SS began it. Some women were unexpectedly released early or transferred to other prison wards before the end of the 6- to 8-week SS treatment; thus, some women did not have access to all 25 SS group sessions and 12 individual booster sessions. The 27 women in SS voluntarily attended an average of 15.6 (SD=6.2, range 4 – 25) group sessions while in prison and an average of 3.3 (SD=3.8, range 0 –12) individual booster sessions after release from prison, for an average total of 18.9 (SD=8.5, range 5 – 37) SS sessions. Nine (33%) of the women had an individual booster session that extended beyond the first month after prison release.
The mean ratings for each item on the End-of-Treatment Questionnaire indicated a high level of satisfaction. Ratings can range from −3 to +3, and mean scores on most (48 out of 51) items were 2.0 or higher, e.g., the clinician overall M=2.7 (SD=0.7), the treatment overall M=2.6 (SD=1.0), focus on the relationship between PTSD and SUD M=2.8 (SD=0.5), helpfulness of the treatment for PTSD M=2.9 (SD=0.3), and helpfulness of the treatment for SUD M=2.7 (SD=0.5). Mean scores on the Client Satisfaction Questionnaire were also high. Of a maximum score of 56, the mean at 12 weeks was 48.9 (SD=6.1), the 3-month follow-up mean was 49.1 (SD=5.3), and the 6-month follow-up mean was 47.3 (SD=6.3).
We also analyzed scores from the final End-of-Treatment Questionnaire (after completion of the booster sessions), which was completed by the 17 women in SS who had received at least one SS booster session after release from prison. Ratings could range from 1 to 5. None of the women reported dissatisfaction with the clinician as a reason for leaving treatment. The women reported that on average: they were “very satisfied” with the treatment they received (M=4.7, SD=0.47), they were between “a little” and “much” better than when they began treatment (M=4.4, SD=0.94), they believed the change was “probably” due to the treatment (M=3.9, SD=1.56), they were “moderately satisfied” with the number of treatment sessions they received (M=4.2, SD=1.01), “very satisfied” with the clinicians they saw (M=4.9, SD=0.49), they would “definitely” return to the treatment program again in the future (M=4.8, SD=0.56), and the program had met “most” of their needs (M=4.0, SD=1.12).
Clinician adherence
Clinicians’ total mean adherence score was 2.1 (SD=0.4) as measured by the SS Adherence Scale (Najavits & Liese, 2000), which is scaled from 0 (not done) to 3 (done thoroughly). The total mean helpfulness score was 2.0 (SD=0.4), on a scale from 0 (harmful) to 3 (extremely effective).
Clinical differences
One clinician had significantly lower adherence, t(38)=5.3, p<.001, and competence, t(38)=4.9, p<.001, scores than did the others. Excluding this clinician raised the mean adherence score slightly to 2.2 (SD=0.3) and the mean helpfulness score to 2.2 (SD=0.4). To rule out the possibility that the lack of significant differences between study treatments was due to one problematic clinician, we reran all outcome analyses excluding this clinician’s four patients (see below). The pattern of results from the 40 women who had adherent clinicians was the same as when data were used from all 44 women, so the results below include all 44 women.
OUTCOME
Specific outcomes are detailed below and in Table 1. Overall, participants’ scores in the two conditions did not differ significantly except in the follow-up period, when there were some advantages for SS over TAU on the paired t-test/chi-square analyses. In general, the consistent pattern was that women in both SS and TAU improved significantly from intake to each subsequent time point (12 weeks, 3- and 6-month follow-ups) on each category of measurement (e.g., PTSD, substance use, psychopathology).
Table 1.
Outcomes of Seeking Safety (n=27) and Treatment-as-Usual (n=22)
| Scale | Seeking Safety M (SD) |
Treatment-as-Usual M (SD) |
||||||
|---|---|---|---|---|---|---|---|---|
| Intake (n=27) | 12 weeks after intake (n=27) | 3 months after release from prison (n=23) | 6 months after release from prison (n=23) | Intake (n=22) | 12 weeks after intake (n=22) | 3 months after release from prison (n=21) | 6 months after release from prison (n=21) | |
| CAPS PTSD total score | 69.4 (16.7) | 57.0 (23.7) **a | 50.9 (32.0) **a | 45.9 (30.7) **a † b | 64.4 (21.3) | 52.5 (24.6) *a | 51.5 (24.6) **a | 46.7 (28.3) **a |
| Trauma Symptom Checklist 40 total score | 9.3 (3.1) | 6.4 (3.9) **a | 6.7 (3.4) ***a | 5.9 (2.4) **a | 8.2 (3.0) | 5.6 (3.2) **a | 7.4 (3.7) † b | 6.7 (3.6) |
| Brief Symptom Inventory-positive symptom score | 40.2 (11.2) | 32.7 (10.3) *a | 27.4 (16.6) **a *b | 27.2 (16.7) **a *b | 42.5 (7.9) | 30.2 (12.0) ***a | 34.5 (16.6) *a | 32.5 (15.6) **a |
| ASI Drug Composite | .23 (.11) | – | .17 (.11) **a | .16 (.14) **a | .27 (.12) | – | .15 (.12) **a | .18 (.11) **a |
| ASI Alcohol Composite | .23 (.24) | – | .13 (.18) | .10 (.17) | .29 (.32) | – | .15 (.21) *a | .20 (.23) |
| ASI Legal Composite | .30 (.23) | – | .15 (.18) **a | .17 (.20) *a | .35 (.20) | – | .15 (.19) **a | .19 (.21) *a |
| Self-report Weeks Abstinent (of 12)1 | – | – | 5.9 (5.5) | 6.3 (5.3) | – | – | 6.3 (5.6) | 7.6 (5.2) |
| PTSD Diagnosis (% yes) | 85 | 48 | 39 | 43 | 82 | 55 | 43 | 38 |
| Return to Prison (% yes)2 | – | – | 4 | 22 † | – | – | 9 | 45 |
Notes. CAPS=Clinician-Administered Posttraumatic Stress Disorder Scale-I; ASI=Addiction Severity Index. All paired t-tests were performed against baseline, exclude women with data missing at the second time point, and are 2-tailed. Sample sizes listed are the maximum per timepoint available; for some measures, the sample size may have been slightly lower. All results are in the direction of clinical improvement, except those that are bolded and italicized (which indicates worsening).
Superscripts:
compared to intake;
compared to 12 weeks;
compared to 3-month follow-up.
Includes weeks of forced abstinence. For results excluding forced abstinence, see the substance use outcome paragraph.
Seeking Safety had a trend for significantly lower return to prison compared to TAU at 6 month follow-up, based on chi square.
p≤.10;
p≤.05;
p≤.01;
p≤.001.
PTSD
Women in both conditions showed a substantial reduction from intake to the 3-month follow-up, i.e., the end of the booster phase for SS, with only 39% of available SS women and only 43% of available TAU women meeting criteria for PTSD 3 months post-release. Six months after prison release, 53% of women who met full criteria for PTSD at intake and were available for follow-up no longer met criteria for PTSD in both the SS and TAU conditions. GEE analysis indicated no significant difference in the odds of meeting criteria for PTSD between the two conditions across all time points (odds ratio for experimental vs. control=1.22, 95% CI=.48 – 3.13, Wald χ2 =.18, p=.67). Per Table 1, for the CAPS total score, women in both SS and TAU improved significantly from intake to each subsequent follow-up point. In addition, there was a trend for improvement for women in SS from 12 weeks to 6 months that did not occur for women in TAU. However, ANCOVA showed that after accounting for age and intake CAPS score, women in the experimental and control conditions did not differ in CAPS total scores across the three posttreatment assessments [Mean difference (experimental – control)=−2.30, 95% CI=−13.81 – 9.21, F(1,40)=0.16, p=.69]. On the TSC-40, there was no significant difference between conditions across time [Mean difference (experimental – control)= −0.43, 95% CI=−2.03 –1.17, F(1,40)=0.30, p=.59]. Women in SS showed significant improvement from intake to each follow-up point, whereas this occurred for women in TAU only at 1 point (12 weeks); moreover, women in TAU showed a trend toward worsening from 12 weeks to 3 month follow-up.
Substance use
Intake ASI drug and alcohol composite scores were not correlated (r=−.06, p=.68), so the ASI drug and alcohol composites were analyzed separately. Repeated measures analyses showed no significant difference between the two conditions on the drug or alcohol composites after accounting for age and intake ASI composite scores [Mean difference (experimental – control)=0.01, 95% CI=−.06 – .08, F(1, 40)=0.14, p=.71 for drug; Mean difference (experimental – control)= −.03, 95% CI=−.13 – .06, F (1, 40)=.52, p=.48 for alcohol]. Results were similar when those who returned to prison were excluded from the analyses. Per Table 1, women in both SS and TAU improved significantly from intake to the two available subsequent time points on the ASI drug composite (3 and 6 month follow-ups). On the alcohol composite, only women in TAU showed a significant decrease and at one time point (intake to 3-month follow-up). Women in the two conditions also did not differ on weeks abstinent from substances [Mean difference (experimental – control)= −1.7, 95% CI=−4.5 – 1.0, F(1, 40)=1.67, p=.20] and rates of total abstinence [χ2(1, N=44)=0.03, p=.86; includes women who returned to prison]. No significant differences were found when women who recidivated were excluded from the analysis. For the TLFB, we excluded women with less than one week outside a controlled environment during the follow-up period, resulting in a sample size of 40 for months 1 to 3 and 41 for months 1 to 6. ANCOVAs with the prior-to-prison substance use ratio as a covariate found no significant differences between conditions (i.e., drug use in months 1 to 3; drug use in months 1 to 6; drug and alcohol use in months 1 to 3; drug and alcohol use in months 1 to 6]. Self-report was consistent with biological tests in 100% of cases.
Psychopathology
In the GEE analysis, there were no significant differences between women in the two conditions on BSI scores across time [Mean difference (experimental – control)= −0.05, 95% CI=−0.42 – 0.31, F(1, 40)=0.09, p=.77]. On the paired t-tests of the BSI positive symptom score, women in both SS and TAU improved significantly from intake to each subsequent follow-up point. In addition, women in SS improved significantly from 12 weeks to each follow-up point (3 and 6 months), whereas women in TAU did not.
Legal
Chi-square analyses showed a trend for women in SS being less likely to have returned to prison by the 6-month follow-up, χ2(1, N=49)=2.98, p=.09, with 10 of 22 women in TAU returning to prison (46%), compared to only 6 of 27 women in SS (22%); when age was covaried this trend no longer approached significance (Wald=2.46, p=.12). ANCOVA of the ASI legal composite showed no differences between the groups across time [Mean difference (experimental – control)=0.02, 95% CI=−0.10 –0.13, F(1, 40)=0.09, p=.76], but women in both conditions showed significant improvement from intake to both 3- and 6-month follow-ups.
Treatment utilization
Chi-square analysis showed a trend toward women in SS being less likely to attend a sober/residential program at some time during the 6 months following treatment (4 of 23 women in Seeking Safety vs. 9 of 21 TAU women attended; χ2(1, N=44)=3.42, p=.06). On the TSR (McLellan et al., 1992), there were no differences between women in SS and TAU on other post-release treatment variables including attending detoxification, taking psychiatric medications, taking drug-related medications, taking medications for medical conditions, talking to a professional about psychological or SUD-related problems, or attending 12-step meetings in the 3 months or 6 months after release from prison. Fifteen women in each group received some form of psychosocial treatment during the 6 months following release from prison.
Association between attendance and outcome
Repeated measures analyses indicated that number of SS group sessions attended was associated with better later CAPS PTSD scores, after accounting for age and intake CAPS score, F(1, 22)=5.51, p=.03. Number of individual SS booster sessions attended was related to better later ASI drug scores, after accounting for age and intake ASI drug scores, F(1, 22)=6.58, p=.02. Neither SS group nor individual attendance was associated with subsequent ASI alcohol scores.
Discussion
This study was a pilot RCT comparing SS plus TAU to TAU-alone in a sample of incarcerated women with PTSD and substance use disorder. This is the first known study in a sample of incarcerated women to use a prospective design to address two key questions: differences between the two conditions and level of improvement on key variables. SS is a therapy model designed to treat PTSD and SUD in an integrated fashion and was administered in this study as a voluntary group treatment during prison (up to 25 sessions, with an average of 15.6) and individual booster sessions after prison (up to 12 sessions, with an average of 3). TAU was a required prison-based substance abuse treatment program consisting of 30 hours per week of group and individual treatment. Study results were consistent: there were no significant differences between conditions on any measure in the primary analyses; both conditions showed significant improvements from intake to subsequent time points on measures of each of the key domains (e.g., PTSD, SUD, psychopathology, legal problems). Secondary analyses (i.e., paired t-tests/chi squares) suggest some benefit for SS above TAU, most notably on measures of psychopathology. In contrast to the current study, all other studies that evaluated SS-plus-TAU compared to TAU-alone have found consistent significant differences in favor of SS at end-of-treatment on numerous variables (Desai et al., 2008; Gatz et al., 2007; Hien et al., 2004; Najavits et al., 2006). In the RCT by Hien et al., unlike the current study, only a third of the clients received any services as part of TAU, and in the RCT by Najavits et al. (2006), it is unknown if all clients received services as part of TAU (as means were reported for the sample as a whole for services received). We can also note that the controlled (but nonrandomized) study by Gatz et al. was conducted in a residential substance abuse treatment program. In the Desai et al. study, which was controlled, but non-randomized, some clients received residential treatment and some received unspecified amounts of psychosocial treatment and/or case management. Although none of these studies involved incarcerated women, they did also sample clients who were severe and chronic in their disorders and had multiple co-occurring life problems. However, comparisons are difficult to make given that the TAU condition varied substantially across studies. Future research will, hopefully, be able to address in more detail the differential impact of SS in relation to the amount and exact nature of the TAU received. Moreover, the fact that TAU was required and SS was voluntary may have also affected our results (i.e., the rate of attendance may have been influenced, and this may have affected outcomes). The attendance at SS in this study was an average of 15 sessions during incarceration, and we found a positive association between attendance and outcomes (the more SS sessions attended, the better the improvement on PTSD and drug severity scores (although not alcohol scores). Thus, if clients had been required to attend all sessions of SS (just as they had been required to attend all TAU sessions), we may have seen greater impact on outcomes. Future research would need to verify this, however, to determine whether a more complete dose of SS would improve outcomes, or whether the type of treatment would not make a difference (i.e., whether SS, TAU, or some as yet unspecified treatment would improve outcomes). Also, future research would benefit from a more formal dose-response study in which patients were randomly assigned to different lengths of treatment.
The current study showed SS having significant improvements from 12 weeks or 3 months to subsequent time points on the measures of psychopathology (BSI and TSC-40), whereas TAU showed no improvement on the BSI and a trend toward worsening on the TSC-40. Additionally, although it is important not to make too much of it in the absence of more statistically significant results, the direction of means for continuous measures also indicates SS improving at each time point, whereas various TAU means worsened. This pattern of results is comparable to that of Hien et al. (2004) and, if confirmed by future research, may suggest that SS has potentially greater ability to help participants continue to improve over time. Of course, future studies will need to examine whether any aftercare program or the specific intervention, SS, promotes positive change after release from prison. It is encouraging that overall satisfaction with SS was high and that higher number of SS sessions was associated with greater improvement on PTSD and drug use symptoms.
Several limitations of this study may also have affected our ability to find more differences between the experimental and control conditions. First, there was potential contamination of the treatment and control conditions. In the closed communal setting of a prison wing, it is likely that contamination occurred and blurred the difference between the treatment and the control. The study clinicians also treated women both in SS and TAU, which represents a potential confound by clinician. Although the study clinicians were instructed to refrain from offering SS ideas or materials to the TAU clients, it was unknown if elements of SS were incorporated into their other therapeutic interactions with these women.
Second, the clinicians also did not implement the topic “case management” that is part of SS. They had been instructed not to deliver that topic as there were separate case managers as part of TAU. This may have somewhat reduced the impact of SS, particularly when considering the case management needs of this population during the post-release phase (e.g., Jordan et al., 2002). The inclusion of an expanded and intensive case management component to SS that attends to the women’s multiple transitional needs during the post-release phase, such as securing housing, medical services, parenting services, and a source of income, might enhance the treatment effects of SS with our target population of women. The issue of post-prison aftercare is a crucial one for future research.
A third limitation was that the women were not assessed at the end of the group SS treatment (which was after about 6 to 8 weeks after intake), but instead the first assessment was close to the women’s release from prison (approximately at 12 weeks), which was much further out than a typical RCT (i.e., the first “posttreatment” occurred 4 to 6 weeks after the primary treatment dosage had ended, during which various events may have occurred to diminish treatment effects, such as stressors, the loss of the treatment per se, other life events). Fourth, because of our limited sample size, we did not have adequate power to test for clustering within cohorts or clinicians, nor to detect a difference of 20% in recidivism rates between the two conditions. Finally, clinicians conducting SS were not selected for it by the SS training/supervision team on the study.
We also observed that it was difficult getting the women to attend booster sessions. The women attended only an average of 3 sessions during the booster period rather than the target of 12 that had been planned. This did not appear to be the result of a negative response to SS or to the therapists, which were consistently given highly positive satisfaction ratings in the current study, in the prior study in the same setting (Zlotnick et al., 2003), and in all other prior studies (see Najavits, 2007). Indeed, it is encouraging that SS has such high acceptability within a criminal justice setting and among women with such intense needs. Actually getting to the booster sessions was a challenge, because after release from prison, the women’s lives tended to be chaotic, with many competing needs. Since women who attended more SS booster sessions tended to have a better outcome in terms of their drug use, it would be important that future research explores the obstacles that women face in participating in aftercare.
In general, more research is needed to better understand the needs of women in prison and effective treatment strategies that may help them. Possibly, a longer treatment during prison and increased frequency of treatment during post-release may be helpful. Greater understanding of how PTSD and SUD interact and how treatment of one may impact the other is also needed. This study is promising in indicating that women with comborbid PTSD and SUD can improve when given an in-prison residential substance abuse treatment program. It is heartening that clients of such severity in terms of PTSD, SUD, and legal problems improved significantly from intake through the later time points. That we showed positive impact over the short period of active treatment in this study is quite encouraging. A major question for future research is whether it is necessary to treat PTSD and SUD simultaneously and/or using models specifically for the dual diagnosis. This issue is as yet unresolved in the field at large.
This study had many notable strengths, including use of a range of standardized measures, an attempt to add treatment as well as assessment after the women had left prison, a thorough statistical analysis, low attrition rate, and a lengthy follow-up period (up to 6 months after prison). Other studies that also provided an in-prison program plus aftercare evidenced lower recidivism within 3 years (25%) for those who participated in both compared to those who dropped out of the after-care portion (64%) (e.g., Knight et al., 1999). If SS and/or provision of an aftercare component can potentially reduce recidivism, this may be an important area for future research. Hopefully, the years ahead will see continued progress in evaluating treatments for women in prison, who are so in need of effective services. Both in the prison setting and after release, there is continued need for creative treatment strategies to help improve women’s PTSD and substance abuse.
Acknowledgments
This study was supported by a grant to Caron Zlotnick from the National Institute of Drug Abuse (DA013935-03). Martha Schmitz, Ph.D., and Tracey Rogers, Ph.D., are thanked for their work as supervisors and Marysol Gutierrez, B.A., for her work as research assistant. We would also like to thank the clinicians for their work on this study and the director of the prison residential substance abuse treatment program, Margaret Plunkett, and the prison warden, Carol Dwyer, for their support of this study. Finally, we would like to thank the women prisoners for participating in this study.
Contributor Information
Caron Zlotnick, Butler Hospital/Brown University.
Jennifer Johnson, Brown University.
Lisa M. Najavits, McLean Hospital/Harvard Medical School
References
- Attkisson CC, Zwick R. The Client Satisfaction Questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning. 1982;5:233–237. doi: 10.1016/0149-7189(82)90074-x. [DOI] [PubMed] [Google Scholar]
- Alexander DA. Trauma research: A new era. Journal of Psychosomatic Research. 1996;4:1–5. doi: 10.1016/0022-3999(95)00027-5. [DOI] [PubMed] [Google Scholar]
- Barthwell AG, Bokos P, Bailey J, Nisenbaum M, Devereux J, Senay EC. A continuum of care for substance abusers in the criminal justice system. Journal of Psychoactive Drugs. 1995;27:39–47. doi: 10.1080/02791072.1995.10471671. [DOI] [PubMed] [Google Scholar]
- Battle CL, Zlotnick C, Najavits LM, Winsor C. Posttraumatic stress disorder and substance use disorder among incarcerated women. In: Ouimette P, Brown PJ, editors. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. Washington, DC: American Psychological Association; 2002. pp. 209–226. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney D. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-I. Behavior Therapy. 1990;18:187–188. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995 Jan;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bloom BO, Owen B, Covington S. Gender-responsive strategies: Research, practice, and guiding principles for women offenders. Washington, DC: U.S. Department of Justice; 2003. [Google Scholar]
- Briere J. Psychometric review of the Trauma Symptom Checklist-40. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press; 1996. [Google Scholar]
- Bureau of Justice Statistics. Women offenders. Washington, DC: Bureau of Justice Statistics; 2000. [Google Scholar]
- Bureau of Justice Statistics. Prisoners in 2002, NCJ 200248, July 2003. 2002. [Google Scholar]
- Bureau of Justice Statistics. Prison Statistics, Summary Findings. 2005 June 30; Retrieved September 11, 2003, from http://www.ojp.usdoj.gov/bjs/prisons.htm.
- Carroll KM, Kadden RM, Donovan DM, Zweben A, Rounsaville BJ. Implementing treatment and protecting the validity of the independent variable in treatment matching studies. Journal of Studies on Alcohol. 1994;12(Suppl):149–155. doi: 10.15288/jsas.1994.s12.149. [DOI] [PubMed] [Google Scholar]
- Chambless D, Hollon S. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Desai RA, Harpaz-Rotem I, Najavits LN, Rosenheck RA. Impact of the Seeking Safety Program on Clinical Outcomes Among Homeless Female Veterans With Psychiatric Disorders. Psychiatric Services. 2008;59:996–1003. doi: 10.1176/ps.2008.59.9.996. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The Timeline Followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RI, Gibbon M, Williams JB. User’s Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version. New York, NY: New York State Psychiatric Institute, Biometrics Research Department; 1996. [Google Scholar]
- Gatz M, Brown V, Hennigan K, Rechberger E, O’Keefe M, Rose T, Bjelejac P. Effectiveness of an integrated trauma-informed approach to treating women with co-occurring disorders and histories of trauma. Journal of Community Psychology. 2007;35:863–878. [Google Scholar]
- Greene B. In: Trauma History Questionnaire. Stamm BH, Varra EM, editors. Lutherville, MD: Sidron Press; 1995. [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. American Journal of Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Federman EB, Burns BJ, Schlenger WE, Fairbank JA, Caddell JM. Lifetime use of mental health and substance abuse treatment services by incarcerated women felons. Psychiatric Services. 2002;53:317–325. doi: 10.1176/appi.ps.53.3.317. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Schlenger WE, Fairbank JA, Caddell JM. Prevalence of psychiatric disorders among incarcerated women. II: Convicted felons entering prison. Archives of General Psychiatry. 1996;53:513–519. doi: 10.1001/archpsyc.1996.01830060057008. [DOI] [PubMed] [Google Scholar]
- Knight K, Simpson D, Hiller ML. Three year incarceration outcomes for in-prison therapeutic community treatment in Texas. The Prison Journal. 1999;79:337–351. [Google Scholar]
- Kubiak SP. The Effects of PTSD on treatment adherence, drug relapse, and criminal recidivism in a sample of incarcerated men and women. Social Work Practice. 2004;14:424–433. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Grissom G, Pettinati H, Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Mosher C, Phillips D. The dynamics of a prison-based therapeutic community for women offenders: Retention, completion, and outcomes. The Prison Journal. 2006;86:6–31. [Google Scholar]
- Najavits LM. Seeking Safety: A treatment manual for PTSD and substance abuse. New York: Guilford; 2002. [DOI] [PubMed] [Google Scholar]
- Najavits LM. Seeking Safety: An evidence-based model for substance abuse and trauma/PTSD. In: Witkiewitz KA, Marlatt GA, editors. Therapists’ guide to evidence-based relapse prevention: Practical resources for the mental health professional. San Diego: Elsevier Press; 2007. pp. 141–167. [Google Scholar]
- Najavits LM, Gallop RJ, Weiss RD. Seeking Safety therapy for adolescent girls with PTSD and substance use disorder: A randomized controlled trial. The Journal of Behavioral Health Services and Research. 2006;33:453–463. doi: 10.1007/s11414-006-9034-2. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Liese BS. Seeking Safety Adherence Scale (revised). Unpublished measure. Boston, MA: Harvard Medical School/McLean Hospital; 2000. [Google Scholar]
- Osher F, Steadman HJ, Barr H. A best practice approach to community reentry from jails for inmates with co-occurring disorders: The APIC Model. Crime and Delinquency. 2003;49:79–96. [Google Scholar]
- Pelissier B, Jones N, Cadigan T. Drug treatment aftercare in the criminal justice system: A systematic review. Journal of Substance Abuse Treatment. 2007;32:311–320. doi: 10.1016/j.jsat.2006.09.007. [DOI] [PubMed] [Google Scholar]
- Pelissier B, Motivans M, Rounds-Bryant JL. Substance abuse treatment outcomes: A multi-site study of male and female prison programs. Journal of Offender Rehabilitation. 2005;41:57–80. [Google Scholar]
- Pelissier B, O’Neil JA. Antisocial personality and depression among incarcerated drug treatment participants. Journal of Substance Abuse. 2000;11:379–393. doi: 10.1016/s0899-3289(00)00034-1. [DOI] [PubMed] [Google Scholar]
- Pelissier B, Wallace S, O’Neil J, Gaes G, Camp S, Rhodes W, Saylor W. Federal prison residential drug treatment reduces substance use and arrests after release. American Journal of Drug and Alcohol Abuse. 2001;42:315–337. doi: 10.1081/ada-100103712. [DOI] [PubMed] [Google Scholar]
- Peters RH, Strozier AL, Murrin MR, Kearns WD. Treatment of substance-abusing jail inmates: Examination of gender differences. Journal of Substance Abuse Treatment. 1997;14:339–349. doi: 10.1016/s0740-5472(97)00003-2. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Vanderspek R, Saltman P. Utility of portable breath alcohol testers for drunken driving offenders. Journal of Studies on Alcohol. 1980;41:930–934. doi: 10.15288/jsa.1980.41.930. [DOI] [PubMed] [Google Scholar]
- Taxman F, Young D, Tesluk P, Mitchell S, Wainright J, Ormond J, Decelles K, Carson J, Rhodes A. The National Survey of Criminal Justice Treatment Practices: Preliminary findings of the prevalence of state-based offender services, importance of offender programming, and systems development issues. Washington, DC. Paper presented at the CJ-DATS Steering Committee Meeting.2005. Apr, [Google Scholar]
- Teplin LA, Abram KM, McClelland GM. Prevalence of psychiatric disorders among incarcerated women, I: Pretrial jail detainees. Archives of General Psychiatry. 1996;53:505–512. doi: 10.1001/archpsyc.1996.01830060047007. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Najavits LM, Rohsenow DJ, Johnson DM. A cognitive-behavioral treatment for incarcerated women with substance abuse disorder and posttraumatic stress disorder: Findings from a pilot study. Journal of Substance Abuse Treatment. 2003;25:99–105. doi: 10.1016/s0740-5472(03)00106-5. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Shea MT, Begin A, Pearlstein T, Simpson E, Costello E. The validation of the Trauma Symptom Checklist-40 (TSC-40) in a sample of inpatients. Child Abuse and Neglect. 1996;20:503–510. doi: 10.1016/0145-2134(96)00032-4. [DOI] [PubMed] [Google Scholar]