Abstract
There is growing empirical and clinical interest in purported associations between smoking and the aggravation of cancer symptoms and treatment side effects, such as pain. Both pain and smoking are highly prevalent among persons with cancer, and there is recent evidence to suggest that cancer patients who continue to smoke despite their diagnosis experience greater pain than nonsmokers. Accordingly, the main goal of this cross-sectional study was to examine associations between multiple levels of smoking status and several pain-related outcomes among a sample of 224 cancer patients about to begin chemotherapy. Patients completed self-report measures of pain severity, pain-related distress, and pain-related interference, as well as a demographics questionnaire. Results indicated that persons who continued to smoke despite being diagnosed with cancer reported more severe pain than never smokers, F (2, 215) = 3.47, p < .05. Current smokers also reported greater interference from pain than either former or never smokers, F (2, 215) = 5.61, p < .01. Among former smokers, an inverse relation between pain severity and the number of years since quitting smoking was observed, r (104) = −.26, p < .01. These data suggest that continued smoking despite a cancer diagnosis is associated with greater pain severity and interference from pain; however, future research is warranted to determine the directionality of this relationship.
Keywords: Tobacco, smoking, cancer, pain, recurrent pain, pain severity, pain interference, pain distress, cessation, quitting
The relationship between tobacco smoking and cancer is well established. Smoking accounts for 90% of lung cancer cases and 85% of head and neck cancers. A review of smoking behavior among lung and head and neck cancer patients revealed that approximately 50–75% self-identified as current smokers at the time of diagnosis [7]. Moreover, up to 58% of these smokers endorsed continued smoking post-diagnosis. Persistent smoking despite a cancer diagnosis has been associated with impaired healing, reduced treatment efficacy, increased risk for developing a second primary cancer, and poorer survival [5,9,21,26].
Persistent smoking has also been associated with the exacerbation of commonly reported cancer symptoms and treatment side effects (e.g., pain, dyspnea, fatigue). Pain reporting among persons with cancer is of particular interest because 30–45% of cancer patients with early stage disease experience moderate to severe pain [2], and nearly 75% with advanced stage disease report moderate to very severe pain [27]. There is also emerging evidence of a unique relationship between recurrent pain and tobacco use among smokers in the general population (i.e., smokers who do not have cancer), which may help to elucidate associations between the maintenance of nicotine dependence and the experience of pain among cancer patients [10,11].
Smoking has been associated with the development and aggravation of several chronically painful conditions [1,12,24,33], and smokers who experience situational or recurrent pain tend to report greater motivation to smoke and increased cigarette consumption [10,17,19]. Ditre and Brandon (2008) integrated these findings to conceptualize a reciprocal relationship between pain and tobacco smoking that operates as a positive feedback loop, leading to greater pain, increased cigarette consumption, and the maintenance of nicotine dependence.
Researchers have advocated for the consideration of population-specific issues (e.g., the influence of common cancer-related symptoms and side-effects) in the development of smoking cessation interventions for cancer patients [7,16]. However, despite the prevalence of smoking and pain among cancer patients and the barrier to quitting smoking that recurrent pain may pose, there has been surprisingly little research on this topic. To our knowledge, only one previous study has examined relations between pain and tobacco smoking among persons with cancer [8]. Daniel and colleagues (2009) tested the cross-sectional association between post-diagnosis smoking status and pain ratings among lung cancer patients, and found that current smokers reported greater pain (OR = 1.6, CI = 1.1 – 2.4) than a group comprised of both former smokers and never smokers.
To elucidate important relations between pain and smoking among persons with cancer, and to identify prospective targets for intervention, it is necessary to build upon these nascent findings by examining smoking status and pain reporting in greater detail, across a wider range of cancer patients, and with regard to potential benefits of quitting smoking. Specifically, we hypothesized that, among patients with diverse cancer diagnoses, current smokers would report greater pain, pain interference, and pain-related distress than former smokers and/or never smokers. We also planned to examine associations between pain and other smoking variables (e.g., number of years since quitting) in an exploratory fashion.
Method
Participants
Participants were recruited as part of a larger study investigating the efficacy of interventions designed to improve quality of life during chemotherapy treatment (i.e., stress management and exercise training). Eligibility criteria included: having an existing cancer diagnosis, being at least ≥ 18 years of age, not having received intravenous chemotherapy within the past 2 months, being scheduled to receive outpatient cytotoxic chemotherapy over a period of at least 9 weeks, being capable of speaking and reading English, having no contra-indications to participating in moderate intensity exercise and graded exercise testing, and having an Eastern Cooperative Oncology Group (ECOG) performance status of ≤ 2 (i.e., ambulatory and/or able to walk without assistance).
Procedure
Patients being considered for chemotherapy were seen in consultation by a medical oncologist at Moffitt Cancer Center in Tampa, Florida. Patients for whom chemotherapy was indicated were scheduled to receive an initial infusion at a later date. Patients being seen for consultations were identified through the use of a computerized appointment system. Patient eligibility was initially determined via medical chart review. Final eligibility determination was based on the medical oncologist reviewing and signing a clearance form that excluded patients for whom moderate exercise or graded exercise testing was contraindicated. Those patients meeting eligibility criteria were introduced to the study by a research assistant and provided with an opportunity to ask questions before signing an Institutional Review Board-approved informed consent form. Following screening and consent, and before randomization to intervention condition, participants completed several questionnaires, including those reported herein.
Measures
Demographic characteristics
Demographic information was obtained prior to initiation of chemotherapy treatment. Variables assessed included gender, education level, race and ethnicity, and marital status. A quarter of the sample (24.9%) opted not to report annual household income. As such, income was excluded from the current report.
Clinical characteristics
Clinical information was obtained via review of patients’ medical charts. Variables assessed included cancer type, disease stage, pre-chemotherapy body mass index (BMI), and surgery status.
Smoking status and cigarette consumption
Smoking status and cigarette consumption was determined via self-report at baseline assessment. Never smokers (n = 80) were operationally defined as those patients who reported smoking fewer than 100 cigarettes in their lifetime. Accordingly, smokers were defined as those patients who reported smoking more than 100 cigarettes in their lifetime. Smokers were then asked to indicate the number of cigarettes smoked in the last month, the total number of years smoked, whether they had quit smoking, or whether they were currently still smoking. Former smokers (n = 108) were operationally defined as those patients who reported having quit smoking and not having smoked any cigarettes in the past month. Current smokers (n = 36) were operationally defined as those patients who reported having smoked in the past month. Current smokers were further queried regarding the number of cigarettes they currently smoked per day.
Pain severity and pain interference
Two items that comprise the SF-36 (Medical Outcomes Survey 36-item Short Form) Bodily Pain subscale were employed to assess past week pain severity and pain interference, respectively [31,32]. The SF-36 is a widely used self-report measure of physical and mental wellbeing. Respondents were asked to rate their perceived severity of bodily pain (1 = “none” to 6 = “very severe”) and the degree to which pain interfered with their daily routine (1 = “not at all” to 5 = “extremely”).
Pain-related distress
The Memorial Symptom Assessment Scale-Short Form (MSAS-SF; [6]) is a self-report measure of the severity of 32 symptoms commonly experienced by cancer patients. Respondents were asked to rate, for the past week, the extent to which they experienced distress associated with pain (0 = “not at all” to 4 = “very much”). Previous research has demonstrated the reliability and validity of the MSAS-SF with cancer patients [6].
Data Analytic Strategy
As seen in Table 1, significant variability was observed for age, gender, cancer diagnosis, disease stage, surgery status, and education across the categorical variable smoking status. Therefore, analysis of covariance (ANCOVA) was employed to statistically control for the influence of these variables (covariate-adjusted means and standard errors are reported throughout). Three separate ANCOVAs were conducted with smoking status (i.e., never, former, and current smokers) as the fixed factor, and pain severity, pain interference, and pain-related distress as the respective dependent variables. Correlational analyses were then conducted to examine associations between pain variables and (a) number of years since quit smoking among former smokers, and (b) number of cigarettes smoked per day among former and current smokers, respectively.
Table 1.
Demographic and Clinical Characteristics of Participants by Smoking Status
| (a) Never Smokers n (%) | (b) Former Smokers n (%) | (c) Current Smokers n (%) | Total Sample n (%) | |
|---|---|---|---|---|
| Gender | ||||
| Male | 17 (21.3%)b | 45 (45.4%)a | 16 (44.4%)a | 82 (36.6%) |
| Female | 63 (78.8%)b | 59 (54.6%)a | 20 (55.6%)a | 142 (63.4%) |
| Education | ||||
| < College Degree | 41 (51.3%) | 66 (61.1%) | 24 (66.7%) | 131 (58.5%) |
| ≥ College Degree | 39 (48.8%) | 42 (38.9%) | 12 (33.3%) | 93 (41.5%) |
| Race | ||||
| Caucasian | 67 (83.8%) | 95 (88.0%) | 35 (97.2%) | 197 (87.9%) |
| Not Caucasian | 13 (16.3%) | 13 (12.0%) | 1 (2.8%) | 27 (12.1%) |
| Cancer Diagnosis | ||||
| Breast | 40 (51.3%) | 26 (33.3%) | 12 (15.4%) | 78 (34.8%) |
| Lung | 4 (5.4%) | 51 (68.9%) | 19 (25.7%) | 74 (33.0%) |
| Other | 36 (50%) | 31 (43.1%) | 5 (6.9%) | 72 (32.2%) |
| Disease Stage | ||||
| I | 9 (11.3%) | 11 (10.2%) | 2 (5.6%) | 22 (9.8%) |
| II | 19 (23.8%) | 28 (25.9%) | 11 (30.6%) | 58 (25.9%) |
| III | 35 (43.8%) | 21 (19.4%) | 11 (30.6%) | 67 (29.9%) |
| IV | 17 (21.3%) | 48 (44.4%) | 12 (33.3%) | 77 (34.4%) |
| Surgery Status | ||||
| Had Surgery | 70 (87.5%)b, c | 79 (73.1%)a, c | 16 (44.4%)a, b | 165 (73.7%) |
| No Surgery | 10 (12.5%)b, c | 29 (26.9%)a, c | 20 (55.6%)a, b | 59 (26.3%) |
| Previous Chemotherapy Treatment | ||||
| No | 63 (78.8%) | 91 (84.3%) | 31 (86.1%) | 185 (82.6%) |
| Yes | 17 (21.3%) | 17 (15.7%) | 5 (13.9%) | 39 (17.4%) |
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Age | 51.10 (10.84)b, c | 60.12 (10.80)a, c | 55.67 (9.77)a, b | 56.18 (11.37) |
| Body Mass Index | 26.75 (5.03) | 27.64 (5.62) | 26.59 (4.87) | 27.15 (5.32) |
| Cigarettes Per Day | - | 20.79 (14.21) | 23.99 (13.32) | 21.48 (14.20) |
| # Years Smoked | - | 23.50 (14.18)c | 35.31 (12.36)b | 26.86 (13.95) |
Note. Superscript letters indicate significant pairwise comparisons at p < .05.
Results
Sample Characteristics
Of 316 patients who were deemed eligible, 71% (N = 224) agreed to participate. Although preliminary analyses revealed that patients who declined to participate were in more advanced stages of their disease (χ2 = 5.85, p = .016), the current sample was fairly evenly distributed across disease stages: I (10%), II (26%), III (30%), and IV (34%). Participation was not associated with age, gender, cancer diagnosis, or ECOG score (ps > .05). The distribution of cancer diagnoses across the current sample was as follows: breast (34.82%), lung (33.04%), bladder (6.25%), ovarian (6.25%), colon (4.02%), mesothelioma (3.12%), head and neck (2.68%), testicular (2.23%), endometrial (1.34%), prostate (1.34%), rectal/anal (1.34%), sarcoma (1.34%), and other (2.23%); however, for analytical purposes, cancer diagnoses were categorized as breast (34.82%), lung (33.04), and other (32.14%). Patients were between 0 – 165 months (M = 10.66; SD = 24.23) from their diagnosis. Forty-three (19%) patients were about to begin chemotherapy for a recurrence of a previously-diagnosed cancer; these patients were between 0 – 14 months (M = 1.58; SD = 2.78) from their recurrence. Participants were predominantly female (63%) and Caucasian (88%). The mean age of patients in the current study was 56.2 (range: 22 – 81, SD = 11.4). Former and current smokers consumed an average of 21.5 (SD = 14.2) cigarettes per day for a mean total of 26.9 years (SD = 14.0). Former smokers reported quitting smoking between 1 – 636 months (M = 187.29; SD = 15.93) before their study visit; ninety-one (84.3%) quit before their diagnosis, 11 (10.2%) quit concurrently with their diagnosis, and 6 (5.5%) quit after their diagnosis. For a complete breakdown of demographic, clinical, and smoking characteristics, see Tables 1 & 2.
Table 2.
Cancer Type by Smoking Status
| Never Smokers n | Former Smokers n | Current Smokers n | Total Sample n | |
|---|---|---|---|---|
| Breast | 40 | 26 | 12 | 78 |
| Lung | 4 | 51 | 19 | 74 |
| Bladder | 2 | 9 | 3 | 14 |
| Ovarian | 11 | 2 | 1 | 14 |
| Colon | 6 | 3 | 0 | 9 |
| Mesothelioma | 2 | 5 | 0 | 7 |
| Head & Neck | 1 | 4 | 1 | 6 |
| Testicular | 4 | 1 | 0 | 5 |
| Endometrial | 2 | 1 | 0 | 3 |
| Prostate | 1 | 2 | 0 | 3 |
| Rectal/Anal | 1 | 2 | 0 | 3 |
| Sarcoma | 3 | 0 | 0 | 3 |
| Other | 3 | 2 | 0 | 5 |
Pain Severity
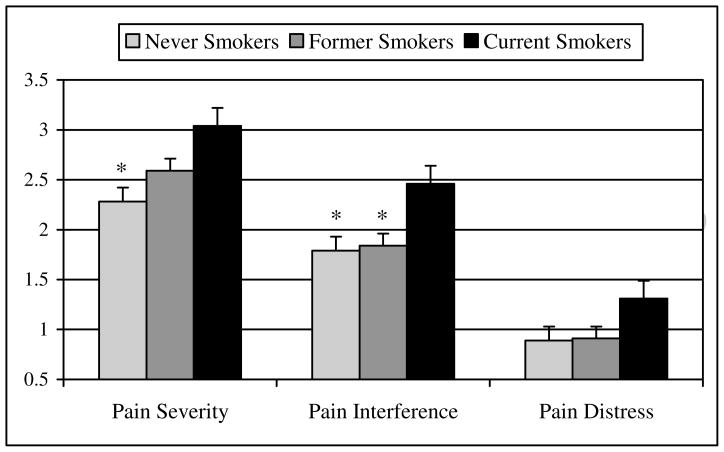
As hypothesized, ANCOVA revealed significant differences in self-reported pain severity as a function of smoking status, F(2, 215) = 3.47; p < .05. Post-hoc pair-wise comparisons indicated that current smokers (M = 3.04, SE = .23) reported experiencing more severe pain than never smokers (M = 2.28, SE = .16), t(114) = 2.68, p < .01. Conversely, there were no differences in severity of pain reporting between former smokers (M = 2.59, SE = .13) and either current smokers or never smokers (both ps > .09) See Figure 1 for a depiction of pain ratings by smoking status.
Figure 1. Covariate-adjusted mean pain ratings (and standard errors) by smoking status.
Note. Asterisks indicate that means are significantly different from Current Smokers at p < .05.
Pain Interference
Also as hypothesized, analysis revealed significant differences in self-reported pain interference with daily routine across groups of smokers and nonsmokers, F (2, 215) = 5.61, p < .01. Post-hoc comparisons indicated that current smokers (M = 2.46, SE = .18) reported having experienced greater interference from pain than did never smokers (M = 1.79, SE = .12), t(114) = 3.10, p < .01, and former smokers (M = 1.84, SE = .10), t(142) = 3.07, p < .01. No differences in pain interference were observed between former smokers and never smokers (p = .79).
Pain-Related Distress
Contrary to expectations, ANCOVA revealed no differences in the degree to which patients experienced distress associated with pain as a function of smoking status, F(2, 215) = 1.63, p = .20. Though this finding did not reach significance, examination of the means indicated that current smokers did report greater pain-related distress (M = 1.31, SE = .21) than former smokers (M = .91, SE = .12) and never smokers (M = .89, SE = .14).
Correlations between Pain and Number of Years since Quitting Smoking
Analyses revealed a significant negative correlation between self-reported pain severity and number of years since quitting smoking among former smokers, r(104) = −.26, p < .01. A similar inverse relation was observed between self-reported interference from pain and number of years since quitting, r(104) = −.24, p = .01. There was, however, no significant correlation between pain-related distress and years since quit, r(103) = −.16, p = .11.
To determine whether the demonstrated negative associations between number of years since quitting and pain severity/interference remained after controlling for potential confounding variables, hierarchical regression analyses were conducted. First, t-tests and correlational analyses were conducted to identify potential confounds. Of the variables examined (i.e., age, gender, education, ethnicity, cancer diagnosis, disease stage, surgery status, previous chemotherapy, BMI, and cigarettes per day), only age was significantly associated with years since quitting, r(105) = .42, p < .001. Hierarchical regression analyses (with age entered first) revealed that number of years since quitting smoking accounted for significant unique variance in pain severity (β = −.23, p < .05) and pain interference (β = −.22, p < .05), above and beyond that accounted for by age.
Correlations between Pain and Cigarettes per Day
Among both current and past smokers, analyses revealed no significant correlations between number of cigarettes smoked per day and either pain severity, pain interference, or pain-related distress (all ps > .36).
Analysis of Pain Severity and Pain Interference Excluding Patients with Lung Cancer
To test whether significant findings for pain severity and pain interference were driven solely by those patients diagnosed with lung cancer (e.g., [8]), a second set of identical ANCOVAs were conducted with all lung cancer patients removed (n = 74). Although some p-values increased due to the reduced statistical power to detect effects, effect sizes tended to be similar to those observed for the full sample. Specifically, the effect size for pain severity was η2 = .031 for the full sample, and η2 = .025 for the sample excluding patients with lung cancer. Similarly, the effect size for pain interference was η2 = .047 for the entire sample, and η2 = .046 without lung cancer patients. Thus, the current results were not driven predominantly by patients diagnosed with lung cancer.
Discussion
The main goal of the current study was to examine associations between smoking status and several indices of pain reporting among groups of nonsmokers, former smokers, and current smokers who were previously diagnosed with cancer. We further sought to explore potential relations between pain and smoking behavior, including number of years since quitting and number of cigarettes smoked per day.
As hypothesized, and consistent with Daniel and colleagues (2009), patients in the current sample who continued to smoke despite their cancer diagnosis reported greater pain severity than patients who were identified as lifetime nonsmokers. Although former smokers’ pain scores did fall between those of nonsmokers and current smokers, they did not differ significantly from either. Due to the cross-sectional nature of these findings, it is unclear whether smoking may have increased pain or been motivated by the pain experience itself. Indeed, there is some empirical support for both causal directions. First, although true causal effects have yet to be established, research indicates that smoking may serve as a marker and/or risk factor for the incidence and severity of chronic nonmalignant pain (for review see [10]). For example, it has been proposed that tobacco smoke may increase pain by reducing blood and oxygen flow to peripheral tissues, or via direct influence on the neurological processing of sensory information. Second, for over two decades researchers have suggested that the avoidance and relief of pain may be a potent reinforcer in the maintenance of tobacco dependence (e.g., [13]). Whereas evidence is mixed regarding the acute pain-inhibitory effects of nicotine (e.g., [14,30]), mounting cross-sectional [17,19] and causal data [10] indicate that pain can nevertheless be a potent motivator of smoking behavior.
Also as predicted, significant associations were observed between smoking status and the degree to which pain interfered with the daily routine of persons with cancer. Specifically, patients who continued to smoke despite their cancer diagnoses reported greater interference from pain than either former smokers or never smokers. No differences in pain interference ratings were observed, however, between former smokers and never smokers. This finding suggests the possibility that pain may be experienced as less obtrusive if cancer patients either quit smoking or never initiated tobacco smoking in the first place.
Contrary to our predictions, results revealed no differences in the extent to which cancer patients experienced psychological distress associated with their pain as a function of smoking status. Examination of the means in Figure 1 indicates that although smokers endorsed somewhat greater pain-related distress than former smokers and never smokers, all patients reported relatively low levels of distress. Another possible explanation for these non-significant findings is that continued smoking may have served as a means for persons with cancer to cope with pain-related distress. Indeed, stress-coping [34] and self-medication [22] models of addiction motivation propose that individuals use substances to cope with distress by regulating affect [4,20], facilitating distraction [3,25], or enhancing performance [18]. An important clinical implication of this consideration is that cancer patients who become increasingly reliant on tobacco for stress-coping and self-medication may become less motivated to quit smoking.
A particularly interesting finding of the current study was the inverse relationship between number of years since quitting smoking and reports of pain severity/pain interference among our sample of former smokers. Although these findings are correlational and modest in magnitude, they could have important clinical implications, particularly if replicated in future studies that are capable of establishing causality. For example, psycho-educational interventions for smokers who have been diagnosed with cancer would likely benefit from conveying scientific evidence that quitting smoking may result in significantly reduced pain over time. However, it is equally plausible that reduced pain preceded and increased the probability successfully quitting smoking. Clearly, additional research is warranted.
The lack of association observed between the number of cigarettes smoked per day and pain severity, pain interference, and pain-related distress may suggest the absence of a dose-response influence of cigarette consumption on pain-related outcomes. However, it is important to note that such presumptions would be limited to the current sample.
Also notable was the finding that a significantly greater percentage of both never smokers (87.5%) and former smokers (73.1%) had undergone surgery than did current smokers (44.4%). Considering that smoking has been associated with increased risk of complications and poorer recovery [23,29], patients may have been instructed to quit smoking as a prerequisite for undergoing surgery. However, this explanation does not address why never smokers were more likely to have undergone surgery. Clearly, this finding requires replication and further examination.
The present study has several important limitations. First the use of cross-sectional data precludes us from making causal inferences. Although these findings have served to identify variables that warrant additional empirical attention, conclusions regarding their relative importance would be premature. Whereas we have made a point of discussing clinically relevant issues germane to the topic of pain and smoking among cancer patients, further deliberation regarding potential clinical implications should be reserved for more conclusive findings. For example, although we detected statistically significant differences between current smokers and never smokers on measures of pain severity and pain interference, the clinical significance of these results remains unclear. Future research would benefit from longitudinally investigating the temporal relation between pain, smoking, and quitting smoking among persons with cancer in naturalistic settings, perhaps using ecological momentary assessment [28].
A second limitation of the current study was that we did not explore mechanistic factors that may underlie the relation between pain and current smoking among persons diagnosed with cancer. Understanding the influence of emotional, physical, and cognitive factors associated with persistent smoking could better inform the development of smoking cessation and relapse-prevention interventions for this population. Given the potential adverse effects of continued smoking on cancer treatment and outcome (e.g., [15]), additional research is clearly warranted.
A third limitation is that these results are not necessarily generalizable to all persons with cancer. For example, 88% of participants in the current study were Caucasian, 74% had already undergone surgery, and this study excluded patients with poor performance statuses. Thus, it is unclear to what extent these findings may be applicable to patients of varied race and ethnicity, those diagnosed at earlier disease stages, and those with greater functional limitations. It should also be noted that our sample of current smokers was relatively small (n = 36), and the extent to which this is representative of all persons with cancer remains unclear. To extend the current findings, future cross-sectional studies into the association between pain and smoking will require larger, more diverse populations of cancer patients.
In summary, the current data indicated that continued smoking despite a cancer diagnosis was associated with increased pain and increased interference from pain, after controlling for age, gender, surgery status, disease stage, and education. A negative correlation between pain ratings and number of years since quitting smoking was also observed. Finally, these findings were obtained among a sample of patients with a range of cancer diagnoses.
Acknowledgments
This research was supported by funding from the American Cancer Society (RSGPB-05-243-01 CPPB), and the National Institute on Drug Abuse (F31 DA023728). Data management services were provided by the Survey Methods Core at Moffitt Cancer Center.
Footnotes
Summary of Conclusion: Among patients with a variety of cancer diagnoses, continued smoking was associated with increased pain and interference from pain, after controlling for demographic and clinical variables.
None of the authors have conflicts of interest to disclose.
Protocol Review and Approval. The data presented in this manuscript were collected through a protocol approved by the Institutional Review Boards at the University of South Florida (Protocol #IRB102390).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Albano SA, Santana-Sahagun E, Weisman MH. Cigarette smoking and rheumatoid arthritis. Sem Arthritis Rheumatism. 2001;31:146–159. doi: 10.1053/sarh.2001.27719. [DOI] [PubMed] [Google Scholar]
- 2.Bonica JJ. The Management of Pain. Philadelphia: Lea & Febiger; 1990. [Google Scholar]
- 3.Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychol Assess. 1991;3:484–491. [Google Scholar]
- 4.Brandon TH, Wetter DW, Baker TB. Affect, expectancies, urges, and smoking: Do they conform to models of drug motivation and relapse? Exp Clin Psychopharmacol. 1996;4:29–36. [Google Scholar]
- 5.Browman GP, Wong G, Hodson I, Sathya J, Russell R, McAlpine L, Skingley P, Levine MN. Influence of cigarette smoking on the efficacy of radiation therapy in head and neck cancer. N Engl J Med. 1993;328:159–163. doi: 10.1056/NEJM199301213280302. [DOI] [PubMed] [Google Scholar]
- 6.Chang VT, Hwang SS, Feuerman M, Kasimis BS, Thaler HT. The memorial symptom assessment scale short form (MSAS-SF) Cancer. 2000;89:1162–1171. doi: 10.1002/1097-0142(20000901)89:5<1162::aid-cncr26>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 7.Cox LS, Africano NL, Tercyak KP, Taylor KL. Nicotine dependence treatment for patients with cancer. Cancer. 2003;98:632–644. doi: 10.1002/cncr.11538. [DOI] [PubMed] [Google Scholar]
- 8.Daniel M, Keefe FJ, Lyna P, Peterson B, Garst J, Kelley M, Bepler G, Bastian LA. Persistent smoking after a diagnosis of lung cancer is associated with higher reported pain levels. J Pain. 2009;10:323–328. doi: 10.1016/j.jpain.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dasgupta P, Rizwani W, Pillai S, Kinkade R, Kovacs M, Rastogi S, Banerjee S, Carless M, Kim E, Coppola D. Nicotine induces cell proliferation, invasion and epithelial-mesenchymal transition in a variety of human cancer cell lines. Intl J Can. 2009;124:36–45. doi: 10.1002/ijc.23894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ditre JW, Brandon TH. Pain as a motivator of smoking: Effects of pain induction on smoking and urge behavior. J Abn Psychol. 2008;117:467–472. doi: 10.1037/0021-843X.117.2.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ditre JW, Heckman BW, Butts EA, Brandon TH. Effects of expectancies and coping on pain-induced motivation to smoke. J Abn Psychol. doi: 10.1037/a0019568. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eriksen WB, Brage S, Bruusgaard D. Does smoking aggravate musculoskeletal pain? Scand J Rheumatol. 1997;26:49–54. doi: 10.3109/03009749709065664. [DOI] [PubMed] [Google Scholar]
- 13.Fertig JB, Pomerleau OF, Sanders B. Nicotine-produced antinociception in minimally deprived smokers and ex-smokers. Addict Behav. 1986;11:239–248. doi: 10.1016/0306-4603(86)90052-3. [DOI] [PubMed] [Google Scholar]
- 14.Girdler SS, Maixner W, Naftel HA, Stewart PW, Moretz RL, Light KC. Cigarette smoking, stress-induced analgesia and pain perception in men and women. Pain. 2005;114:372–385. doi: 10.1016/j.pain.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 15.Gritz ER, Dresler C, Sarna L. Smoking, the missing drug interaction in clinical trials: ignoring the obvious. Can Epidem Biomark Prev. 2005;14:2287–2293. doi: 10.1158/1055-9965.EPI-05-0224. [DOI] [PubMed] [Google Scholar]
- 16.Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment: Smoking cessation in cancer patients. Cancer. 2006;106:17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 17.Hahn EJ, Rayens MK, Kirsh KL, Passik SD. Brief report: Pain and readiness to quit smoking cigarettes. Nicotine Tobacco Res. 2006;8:473–480. doi: 10.1080/14622200600670355. [DOI] [PubMed] [Google Scholar]
- 18.Heishman SJ. Behavioral and cognitive effects of smoking: Relationship to nicotine addiction. Nicotine Tobacco Res. 1999;1:S143–S147. doi: 10.1080/14622299050011971. [DOI] [PubMed] [Google Scholar]
- 19.Jamison RN, Stetson BA, Parris WCV. The relationship between cigarette smoking and chronic low back pain. Addict Behav. 1991;16:103–110. doi: 10.1016/0306-4603(91)90002-y. [DOI] [PubMed] [Google Scholar]
- 20.Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 21.Kawahara M, Ushijima S, Kamimori T, Kodama N, Ogawara M, Matsui K, Masuda N, Takada M, Sobue T, Furuse K. Second primary tumours in more than 2-year disease-free survivors of small-cell lung cancer in Japan: The role of smoking cessation. Br J Cancer. 1998;78:409–412. doi: 10.1038/bjc.1998.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harv Rev Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- 23.Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: A randomised clinical trial. The Lancet. 2002;359:114–117. doi: 10.1016/S0140-6736(02)07369-5. [DOI] [PubMed] [Google Scholar]
- 24.Pamuk ÖN, Dönmez S, Çakir N. The frequency of smoking in fibromyalgia patients and its association with symptoms. Rheumatol Int. 2009;29:1311–1314. doi: 10.1007/s00296-009-0851-5. [DOI] [PubMed] [Google Scholar]
- 25.Steele CM, Josephs RA. Alcohol myopia: Its prized and dangerous effects. Am Psychol. 1990;45:921–933. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- 26.Stevens MH, Gardner JW, Parkin JL, Johnson LP. Head and neck cancer survival and life-style change. Arch Otolaryngology. 1983;109:746–749. doi: 10.1001/archotol.1983.00800250040009. [DOI] [PubMed] [Google Scholar]
- 27.Stjernsward J, Teoh N. The scope of the cancer pain problem. Advanc Pain Res Ther. 1990;16:9. [Google Scholar]
- 28.Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavorial medicine. Ann Behav Med. 1994;16:199–202. [Google Scholar]
- 29.Tonnesen H, Nielsen PR, Lauritzen JB, Moller AM. Smoking and alcohol intervention before surgery: Evidence for best practice. Br J Anaesth. 2009;102:297–306. doi: 10.1093/bja/aen401. [DOI] [PubMed] [Google Scholar]
- 30.Unrod M, Kassel JD, Robinson M. Effects of smoking, distraction, and gender on pain perception. Beh Med. 2004;30:133–140. doi: 10.3200/BMED.30.3.133-140. [DOI] [PubMed] [Google Scholar]
- 31.Ware JE, Kosinski M, Keller SD. SF-36 physical and mental health summary scales: A user’s manual. Boston, MA: The Health Institute; 1994. [Google Scholar]
- 32.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey: Manual and interpretation guide. Boston, MA: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- 33.Weingarten TN, Moeschler SM, Ptaszynski AE, Hooten WM, Beebe TJ, Warner DO. An assessment of the association between smoking status, pain intensity, and functional interference in patients with chronic pain. Pain Physician. 2008;11:643–653. [PubMed] [Google Scholar]
- 34.Wills TA, Shiffman S. Coping and substance use: A conceptual framework. Coping Subst Abuse. 1985:3–24. [Google Scholar]