Abstract
Objectives.
We aimed to examine the effects of 2 factors of familism (Familial Obligations and Expected Support from the Family) and Cultural Justification on caregivers’ mental and physical health as mediated by coping style.
Methods.
We used a probability sample of 95 African American and 65 White family caregivers for people with dementia to test hypotheses based on the updated sociocultural stress and coping model using path analysis. Main outcome measures included depressive symptomatology, various psychological symptoms, and subjective physical health.
Results.
Both Familial Obligations and Cultural Justification had an indirect effect on poor mental health and subjective physical health via avoidant coping. Expected Support from the Family had no effect on caregivers’ health outcomes.
Discussion.
These findings suggest that feelings of obligation may be accounting for a significant proportion of the negative effects of familism on caregivers’ mental and subjective physical health. Expectations of familial social support may be relatively inconsequential in this process.
Keywords: Caregiver burden, Caregiving, Culture, Ethnicity, Familism, Stress and coping
A substantial literature documents that providing care for a family member with dementia is associated with detrimental mental and physical health consequences (e.g., Schulz, O’Brien, Bookwala, & Fleissner, 1995; Vitaliano, Zhang, & Scanlan, 2003). As the elderly population in the United States is expected to surge, the number of people with dementia is also expected to grow rapidly as is the number of family members providing care for these individuals (Hebert, Scherr, Bienias, Bennett, & Evans, 2003). Given that the number of older adults from minority cultures is predicted to increase at a significantly greater rate than that of White Americans (U.S. Bureau of the Census, 2000), the need to understand crosscultural differences in caregiving experiences and outcomes is becoming more pressing. As such, literature reviews on ethnicity and caregiving have highlighted the need to directly measure and evaluate the effect that cultural values have on caregiving experiences rather than simply relying on group membership to assess ethnic and cultural differences in caregiving (Dilworth-Anderson, Williams, & Gibson, 2002; Janevic & Connell, 2001).
Knight and Sayegh (2010) recently updated the sociocultural stress and coping model for caregivers, which provides a conceptual framework for better understanding and conceptualizing caregiving across culturally diverse groups. This model, which is based on the stress and coping model originally developed by Lazarus and Folkman (1984), posits that the effects of negative stress on individuals are mediated by several variables, including appraisals of burden, coping styles, and social support. This model emphasizes the role of cultural and ethnic dimensions within the stress and coping process rather than simply viewing ethnic group membership as a proxy for presumed differences in cultural values that may affect the caregiving experience. Chun, Knight, and Youn (2007), Kim, Knight, and Flynn Longmire (2007), and Sörensen and Pinquart (2005) suggested a common core model for caregiver distress that has been consistently found in various ethnic groups. This model views behavior problems in the individual with dementia as stressors for family caregivers and includes the caregivers’ appraisal of burden as a key mediator of those stressors, with higher levels of burden appraisal being associated with worse mental and physical health outcomes for caregivers. The updated sociocultural model adds to this common core model by providing a framework with which to look for the influence of cultural values on this common core model and also for variations on components of the stress and coping model by ethnic group. The model posits that cultural values operate through influences on coping resources such as social support and coping styles rather than through caregivers’ appraisals of burden when they are associated with emotional or physical health outcomes at all.
One cultural value that has been examined across diverse ethnic and cultural groups in the context of caregiving is familism. Familism refers to the strong normative feelings of loyalty, dedication, reciprocity, and attachment of family members to their family and familial relationships, both nuclear and extended, as well as strong identification and solidarity with their family members (Heller, 1970; Sabogal, Marin, Otero-Sabogal, Marin, & Perez-Stable, 1987). Kim and colleagues (2007) developed path models based on the sociocultural stress and coping model and hypothesized that familism would have protective effects against detrimental health outcomes for caregivers as mediated by its association with active coping. They also hypothesized that the effects of familism on health outcomes would be mediated by caregivers’ burden appraisals and coping styles, with familism being negatively associated with burden and higher levels of burden being associated with avoidant coping. Contrary to their hypotheses, the authors reported that familism was in fact associated with avoidant coping, which resulted in poorer outcomes for mental and subjective physical health. However, the authors did find that burden was associated with poorer mental and subjective physical health outcomes through avoidant coping as hypothesized.
These surprising findings suggested that familism may not have protective effects on caregivers’ health and may in fact result in worse outcomes. Kim and colleagues (2007) proposed a possible explanation for these findings, suggesting that “familism, as measured in caregivers by the Bardis (1959) scale, may represent obligation more than positive feelings about family support” (p. 573). The Bardis familism scale has been applied indiscriminately to describe both nuclear and extended familial relationships, and it consists of two distinct subscales assessing nuclear and extended familism, which intercorrelate with one another (see McClendon Baumann, 2007). Thus, the Bardis familism scale may not be best suited as a measure of familism.
The Sabogal and colleagues (1987) familism scale differs from the Bardis scale in that it taps more specific components of familism involving both attitudinal and behavioral aspects of familism. Sabogal and colleagues conducted an exploratory factor analysis of this scale that revealed three different factors: Familial Obligations, Perceived Support from the Family, and Family as Referents. The Familial Obligations factor was described as the perception of obligation to provide financial and emotional support to extended family members. One item belonging to this factor is “aging parents should live with their relatives.” The Perceived Support from the Family factor assesses the extent to which individuals expect to receive adequate material and emotional support from their family. This factor is hereafter referred to as “Expected Support from the Family,” as the items that compose this factor appear to represent expectations rather than perceptions of familial support. A sample item belonging to this factor is “One can count on the help from his/her relatives to solve most problems.” Zarit, Orr, and Zarit (1985) hypothesized that the distress linked with caregiving among primary caregivers could be lessened by social support, such as having other relatives pay visits to them. In line with this conjecture, several studies have reported that the receipt of social support from others can reduce the detrimental effects of caregiving on physical health outcomes (e.g., Barusch & Spaid, 1989; Pinquart & Sörensen, 2007). The third factor, Family as Referents, measures the view of relatives as behavioral and attitudinal referents. An example of an item belonging to this factor is” the family should consult close relatives concerning its important decisions.” These findings provide a more specific understanding of familism by providing three distinct factors addressing different dimensions of this cultural value, which can be more useful and illuminating in family dementia caregiving research than the more broad dimensions of familism that the Bardis scale measures.
In addition to familism, several other cultural values have been proposed to explain why individuals decide to provide care for a family member, including filial obligation (Silverstone, 1978), reciprocity between adult children and their parents (John, Hennessy, Dyeson, & Garret, 2001; Wallace, Witucki, Boland, & Tuck, 1998), role modeling of caregiving behavior for one's own children (Nkongho & Archbold, 1995), and religious and spiritual values emphasizing an ethic to care for family members (Levkoff, Levy, & Weitzman, 1999). The Cultural Justifications for Caregiving Scale (CJCS; Dilworth-Anderson, 1995) assesses these kinds of cultural values with regard to the caregiving experience by measuring attitudes about cultural reasons and expectations for providing care. The Traditional Caregiving Ideology (TCI) subscale of the Lawton Caregiving Appraisal measure (Lawton, Kleban, Moss, Rovine, & Glicksman, 1989) assesses traditional attitudes toward the caregiving role assumed to incorporate cultural values concerning caregiving, including both family and religious tradition, modeling for one’s children, and reciprocity as motivation for caregiving.
An exploratory factor analysis aimed at identifying potential factors involving these two measures of cultural values associated with caregiving revealed a 12-item factor, Cultural Justification, composed of all 10 items from the CJCS as well as 2 items from the TCI subscale. McClendon Baumann (2007) defined this factor as “caregiving based on a broad collection of values learned within the family … exclusively comprised items describing explicitly stated cultural reasons for caregiving (e.g., caregiving based on religious beliefs, based on role modeling, based on duty).” The items included in this factor constitute a more appropriate cultural values scale with more defined cultural components that can be useful for examining cultural differences in dementia caregiving. Having strong cultural reasons for providing care would appear to be protective against poor outcomes for caregivers based on a stress and coping framework that would view such justifications for caregiving as a caregiving resource in the face of caregiving demands (Dilworth-Anderson, Goodwin, & Williams, 2004).
The overall objective of this research investigation is to provide a more detailed examination of how specific factors of familism and Cultural Justification, as mediated by burden and coping, affect the caregiving process and outcomes for African American and White family caregivers of people with dementia. This report reanalyzes the Kim and colleagues (2007) data using path models that substitute more specific components of familism in addition to Cultural Justification in the context of the stress and coping process for caregivers. This study thereby aims to better understand the surprising finding from the study by Kim and colleagues that familism was associated with avoidant coping, which resulted in poorer health outcomes for caregivers. Using the updated sociocultural stress and coping model (Knight & Sayegh, 2010) as a foundation, we hypothesized the following:
Hypothesis 1: Higher scores on the Familial Obligation factor will result in higher levels of use of avoidant coping, which will result in poorer mental and physical health outcomes for family caregivers of people with dementia.
Hypothesis 2: Higher scores on the Expected Support from the Family factor will result in higher levels of use of active coping, which will result in better mental and physical health outcomes for family caregivers of people with dementia.
Hypothesis 3: Higher scores on the Cultural Justification factor will result in higher levels of use of active coping, which will result in better mental and physical health outcomes for family caregivers of people with dementia.
We made no hypotheses involving the Family as Referents factor of familism in this study as its potential role in the context of the stress and coping process for caregivers was not conceptually clear. We also emphasize that we did not make hypotheses regarding ethnic differences in this study because previous studies using the same sample (Kim et al., 2007; Knight, Flynn Longmire, Dave, Kim, & David, 2007) have found ethnic differences in terms of mean levels of familism, yet no direct effects of ethnicity on outcomes. Thus, ethnicity was included in this study as a control variable rather than a mediating variable.
DESIGNS AND METHODS
Participants
This community-based sample of caregivers included 95 African American and 65 White family caregivers of individuals with dementia from the Stress and Ethnicity Caregiving Study who were recruited by multistage sample collection. The Kim and colleagues (2007) study examined how familism affected these outcomes among caregivers differentially across ethnic groups by applying the sociocultural stress and coping model (Aranda & Knight, 1997; Knight, Silverstein, McCallum, & Fox, 2000). The current study differs from the Kim and colleagues study in that it aimed to examine how more specific cultural values (the Familial Obligations and Expected Support from the Family factors of familism and the Cultural Justification factor) affect caregivers’ mental and physical health outcomes in the context of the updated sociocultural stress and coping model (Knight & Sayegh, 2010).
Participants were recruited through phone contacts in census tracts known to contain a high percentage of residents aged 65 years and older (10% or greater) and known to be largely African American or non-Hispanic White (60% or greater). Neighborhoods that had average household incomes below the median for Los Angeles County, California, were selected in order to minimize potential confounds resulting from socioeconomic status (SES). This technique served to prevent the comparison of primarily lower SES African Americans with Whites from predominantly higher SES brackets. Age for the sample was restricted to individuals aged 18 years or older.
Project telephone interviewers then contacted these randomly selected households and questioned an adult residing in the household to determine if anyone in the household was aged 50 years or older and had memory problems or was a caregiver of an older relative with memory problems who resided in another household. Individuals were considered primary caregivers if they had a family member with dementia and either resided with the person with dementia or provided at least 8 hr of care per week. If more than one potential caregiver lived in the household, the one who managed personal care or supervision was selected. A brochure describing the purpose of the study was mailed to those households in which a caregiver was identified. After receipt of the brochure, the project telephone interviewers contacted the potential participants again to determine whether they would be willing to participate in the study and to obtain the diagnosis of dementia and its source. Only caregivers of those who had a professional diagnosis of dementia were recruited. Approximately one third of the obtained sample was providing care for an individual diagnosed with Alzheimer's disease, whereas 30.5% were diagnosed with dementia without further specification. The remainder were nearly equally divided between various vascular dementias and Parkinson’s-related dementias.
In-person interviews with the participants were then arranged by a graduate student research assistant. The interviews, which lasted about 70–100 min, were conducted by ethnically diverse research assistants who were randomly assigned to interview the participants. The participants received $20 as compensation. The majority (greater than 90%) of the interviews took place in the participants’ homes, whereas the rest occurred on the University of Southern California campus. Table 1 provides demographic and descriptive information for the caregivers included in this study.
Table 1.
Mean Demographic, Caregiving, and Key Variable Information of Caregivers (N = 160)
| M (SD) | % | |
| Demographic characteristic | ||
| Age (years) | 56.70 (15.85) | |
| Gender | ||
| Male (coded 0) | 31.2 | |
| Female (coded 1) | 68.8 | |
| Ethnicity | ||
| White (coded 0) | 40.6 | |
| African American (coded 1) | 59.4 | |
| Incomea | 3.31 (1.67) | |
| Educationb | 4.06 (0.88) | |
| Caregiving-related characteristics | ||
| Living with care recipient | ||
| Yes (coded 0) | 80.0 | |
| No (coded 1) | 20.0 | |
| Length of time in caregiving (years)c | 4.35 (3.08) | |
| Caregiving hours per week | 17.95 (11.61) | |
| Care recipients’ problems with ADLd | 9.48 (3.32) | |
| Care recipients’ problems with IADLd | 20.45 (3.37) | |
| Key variable | ||
| Care recipients’ behavioral problems | 8.33 (6.76) | |
| Familial Obligations | 16.97 (3.70) | |
| Expected Support from the Family | 7.37 (2.68) | |
| Cultural Justification | 36.67 (8.03) | |
| Burden | 30.92 (15.70) | |
| Active coping | 58.50 (10.85) | |
| Avoidant coping | 31.04 (7.55) | |
| Depression (CES-D) | 10.89 (6.71) | |
| Psychological symptoms (GSI) | 0.50 (0.53) | |
| Subjective physical health | 2.16 (0.79) | |
Notes: ADL = activities of daily living; IADL = instrumental activities of daily living; CES-D = Center for Epidemiological Studies-Depression Scale; GSI = General Symptom Index.
Income was measured using the following scale: 1 = under $10,000, 2 = $10,000–$19,999, 3 = $20,000–$29,999, 4 = $30,000–$39,999, 5 = $40,000–$49,999, and 6 = $50,000 or more.
Highest level of education was measured using the following scale: 1 = elementary school, 2 = middle school/junior high, 3 = high school, 4 = some college, 5 = undergraduate degree, and 6 = master’s degree or beyond.
The mean and SD of the length of time in caregiving are presented after dropping four outliers.
ADL and IADL were measured using the following scale: 1 = no help, 2 = some help, and 3 = a lot of help. Total possible scores ranged from 5 to 15 and 8 to 24, respectively.
Measures: Independent Variables
Familism factors.—
The scores on the two factors of familism (Familial Obligations and Expected Support from the Family) derived from the 14-item Sabogal and colleagues (1987) familism scale were measured by calculating participants’ total scores from the six items that create the Familial Obligations factor and the three items that compose the Expected Support from the Family factor. This scale presents hypothetical situations involving family crises or events (e.g., “A person should always help his/her parents with the support of his/her younger brothers and sisters if necessary, When one has problems, one can count on the help of relatives”), which respondents score on a scale of 0–4, with higher scores indicating greater levels of the familism factors. The Cronbach’s α values for these two factors are .69 (African American) and .80 (Whites) for Familial Obligations and .82 (African American) and .88 (Whites) for Expected Support from the Family in this sample of caregivers.
Cultural justification.—
The Cultural Justification factor was measured by calculating participants’ total scores on the 10 items from the CJCS (Dilworth-Anderson, 1995) as well as the 2 items from the TCI (Lawton et al., 1989) that combine to create this factor. The CJCS requires respondents to indicate the degree to which they agree with reasons to provide care for older family members (e.g., “By giving care to the elderly dependent family members, I am giving back what has been given to me”) on a scale from 1 to 4, with higher scores representing more cultural justifications for caregiving. The two items from the TCI pertain to cultural reasons for caregiving, including caregiving based on religious beliefs and role modeling for one’s children (e.g., “A strong reason to care for a family member is to provide a good model for your own children to follow”). Respondents indicate the degree to which they agree or disagree with each item on a scale from 0 to 4, with higher scores representing greater amounts of cultural reasons for caregiving. The α values are .88 for African Americans and .87 for Whites.
Caregiver burden.—
Subjective burden was measured with the 22-item Zarit Burden Interview (Zarit, Reeves, & Bach-Peterson, 1980). Items are scored 0–4, with higher scores indicating greater caregiver burden. The α values are .95 for African Americans and .92 for Whites.
Coping style.—
Sixty items of the COPE scale (Carver, 1997) were used as a measure of coping styles. Caregivers were asked to respond to each item while focusing specifically on caregiving. The response choices were 1 (I haven’t been doing this at all), 2 (I have been doing this a little bit), 3 (I have been doing this a medium amount), and 4 (I have been doing this a lot). The Active Coping factor was composed of items such as “I make a plan of action” and “I look for something good in what is happening.” The Avoidant Coping factor contained items such as “I just give up trying to reach my goal” and “I act as though it hasn’t even happened.” The α values are .82 (African Americans) and .81 (Whites) for Active Coping and .73 (African Americans and Whites) for Avoidant Coping.
Care recipient behavioral problems.—
The behavioral problems of the care recipients, which represent a caregiver stressor, were measured with nine items of the Revised Memory and Behavior Problems Checklist (Teri et al., 1992). Responses were scored from 0 (not at all) to 4 (always), with higher scores representing increased caregiving demands. The α values are .88 in African Americans and .78 in Whites.
Measures: Dependent Variables
Caregiver mental health: Depression.—
Caregivers’ depression was measured in this data set using the Center for Epidemiological Studies-Depression Scale (Radloff, 1977), which is a 20-item self-report scale that was created to screen for depressive symptoms in the general population. Responses to each of the items are scored from 0 to 3 and total scores range from 0 to 60, with higher scores representing higher numbers of depressive symptoms. The α values are .80 in African Americans and .77 in Whites.
Caregiver mental health: Psychological symptoms.—
Psychological symptoms were measured using the 53-item Brief Symptom Inventory (BSI), which covers a wide range of symptoms categorized into nine dimensions: somatization, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid anxiety, and psychoticism (Derogatis & Spencer, 1985). The BSI is a short measure used to calculate a global measure of such symptoms referred to as the General Symptom Index (GSI). The α values for the GSI for both African Americans and Whites are the same (.97).
Caregiver physical health: Subjective physical health.—
Caregivers’ subjective physical health was measured by a one-item measure of current physical health. The item was rated on a 4-point Likert scale (1 = excellent, 2 = good, 3 = fair, and 4 = poor). Several previous studies have reported that subjective physical health is highly correlated with physician ratings of health and mortality (Benyamini, Blumstein, Lusky, & Modan, 2003; George, 2001). Therefore, subjective physical health measures are regarded as valuable proxy measures of physical health status.
Measures: Control Variables
Age, ethnicity, and education level were included as background variables as they are known to be highly correlated with physical health. Ethnicity was measured by asking participants how they described their ethnic background/heritage, which has then categorized as either African American or White. We define ethnicity as belonging to a group that possesses a specific heritage and set of beliefs, customs, and values (Phinney, 1996). Education level was assessed using six categories: elementary school, middle school/junior high, high school, some college, undergraduate degree, and master’s degree or beyond (scored from 1 to 6). Although income level has been demonstrated to be an important factor affecting physical health, it was not included as a control variable as it was found to be highly correlated with education level. In addition, the familial relationship of the caregiver to the care recipient and coresidence were not included because analyses revealed that correlations between both of these factors and caregiver burden and physical health were low (r < .20).
Analysis
In order to test the study hypotheses, path models were assessed using the statistical software AMOS 17.0 by examination of the statistical significance of estimated path coefficients and various statistics indicating goodness of fit for the models as a whole, including comparative fit indices (CFI), chi square to degrees of freedom ratio (χ2/df), and root mean square error of approximation (RMSEA). Models with a better fit generally have higher CFI and lower χ2/df and RMSEA values. The rules for establishing goodness of fit for models vary. However, Bentler (1992) stated that values greater than .90 for CFI represent well-fitting models as do χ2/df values of less than 3.0 (e.g., Hu & Bentler, 1999). Browne and Cudeck (1993) reported that RMSEA values of up to 0.1 signify reasonable approximation errors in the population.
We ran unique path models for each cultural value variable (Familial Obligations, Expected Support from the Family, and Cultural Justification) for both outcomes (mental and subjective physical health) separately, resulting in a total of six final models. All unidirectional paths excluding paths from the three cultural values were freely estimated. The direct paths from these variables to the outcome variables were omitted from the models for theoretical reasons as the effects of these factors are viewed as being mediated by coping as opposed to being directly associated with the outcomes of interest. We estimated the disturbance terms for each of the mental health outcomes (depression and psychological symptoms) to acknowledge that various factors other than the exogenous (i.e., independent) variables in our models account for these outcomes. In addition, the covariances between the disturbance terms of the mental health outcome variables were estimated, and the disturbance terms were allowed to be correlated in the model to account for the high correlation (r = .805, p < .01) among them. This procedure allowed us to recognize the operation of other unmeasured factors that account for the correlation between these two variables without giving them a central focus in our conceptually based hypothesized models (Jaccard & Jacoby, 2010). Correlations among the exogenous variables were examined before restricting the covariances between them to zero. Zero-order correlations among model variables are reported in Table 2.
Table 2.
Correlation Coefficients Among Key Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| 1 | 1.000 | |||||||||||
| 2 | .153 | 1.000 | ||||||||||
| 3 | –.052 | –.046 | 1.000 | |||||||||
| 4 | –.323** | –.097 | –.122 | 1.000 | ||||||||
| 5 | –.180* | –.020 | –.197* | .671** | 1.000 | |||||||
| 6 | .065 | –.046 | –.037 | .390** | .310** | 1.000 | ||||||
| 7 | –.006 | .077 | .459** | –.191* | –.218** | –.100 | 1.000 | |||||
| 8 | .061 | .058 | .096 | .072 | .046 | .281** | .030 | 1.000 | ||||
| 9 | –.158 | –.095 | .147 | .127 | .064 | .150 | .433** | .026 | 1.000 | |||
| 10 | –.026 | –.084 | .140 | .062 | –.032 | .013 | .448** | –.123 | .431** | 1.000 | ||
| 11 | –.182* | –.031 | .096 | –.006 | –.023 | .029 | .391** | –.061 | .423** | .805** | 1.000 | |
| 12 | .153 | –.097 | –.117 | –.049 | –.171* | .071 | .129 | –.029 | .256** | .291** | .148 | 1.000 |
Note: 1 = caregivers’ age; 2 = caregiver's education; 3 = care recipients’ behavioral problems; 4 = Familial Obligations; 5 = Expected Support from the Family; 6 = Cultural Justification; 7 = caregiver burden; 8 = active coping; 9 = avoidant coping; 10 = depression (Center for Epidemiological Studies-Depression Scale); 11 = psychological symptoms (General Symptom Index); and 12 = subjective physical health.
*p < .05; **p < .01.
Less than 10% of the cases in this data set had item-level missing values. Prorated scores were calculated when there were fewer than three missing items on scales with multiple items. With the inclusion of these interpolated values, scale scores were missing in less than 5% of cases for all scales and single-item variables.
RESULTS
Analyses of the hypothesized path models revealed that in all cases, the fit statistics indicated acceptable levels of model fit. Final models were then estimated after nonsignificant paths were deleted from the originally proposed models in the interest of parsimony. The fit statistics of the reduced models also suggested that the data fit these models well. CFI and RMSEA values for all the reduced models fell within the acceptable range, so the reduced models were accepted as the final models. The reduced models were not significantly different in comparison with the originally proposed models, as indicated by the changes in the chi-square values (Familial Obligations models: Δχ2(23) = 30.998 for the mental health model, Δχ2(17) = 22.574 for the subjective physical health model, Expected Support from the Family models: Δχ2(24) = 39.887 for the mental health model, Δχ2(18) = 31.228 for the subjective physical health model, Cultural Justification models: Δχ2(23) = 29.884 for the mental health model, and Δχ2(17) = 20.805 for the subjective physical health model).
Fit statistics for both the first and the reduced models involving both Familial Obligations and Cultural Justification with the mental and subjective physical health outcomes are presented in Table 3. The unstandardized path coefficients and their significance levels for the originally proposed models that included these two cultural values with the mental and subjective physical health outcomes are reported in Tables 4–5. The final path models with standardized path coefficients for these two cultural values with the mental and subjective physical health outcomes are presented in Figures 1–4. The fit statistics, unstandardized path coefficients, and final models with standardized path coefficients for the Expected Support from the Family models are omitted as the main findings for this cultural value were nonsignificant.
Table 3.
Goodness of Model Fit Statistics of the First and Reduced Models
| First model | χ2 | df | p | χ2/df | CFI | RMSEA (90%) |
| Familial Obligations and mental health | 18.902 | 9 | .026 | 2.100 | .969 | .083 (.023, .136) |
| Familial Obligations and subjective physical health | 11.494 | 8 | .175 | 1.437 | .973 | .052 (.000, .115) |
| Cultural Justification and mental health | 7.421 | 9 | .593 | .825 | 1.000 | .000 (.000, .078) |
| Cultural Justification and subjective physical health | 7.060 | 8 | .530 | .883 | 1.000 | .000 (.000, .086) |
| Reduced model | ||||||
| Familial Obligations and mental health | 49.900 | 32 | .023 | 1.559 | .945 | .059 (.023, .090) |
| Familial Obligations and subjective physical health | 34.068 | 25 | .106 | 1.363 | .930 | .048 (.000, .085) |
| Cultural Justification and mental health | 37.305 | 32 | .238 | 1.166 | .983 | .032 (.000, .070) |
| Cultural Justification and subjective physical health | 27.865 | 25 | .314 | 1.115 | .975 | .027 (.000, .071) |
Note: CFI = comparative fit index; RMSEA = root mean square error of approximation.
Table 4.
Unstandardized Regression Coefficients Estimated From Fully Recursive Path Models With Familial Obligations and Cultural Justification Predicting Caregivers’ Burden, Coping Style, and Mental Health (N = 160)
| Independent variable | Endogenous variable | |||||
| Familial Obligations | Burden | Active coping | Avoidant coping | CES-D | GSI | |
| Exogenous | ||||||
| Age | –0.07*** | –0.06 | 0.08 | –0.04 | 0.01 | –0.01* |
| Education | –0.05 | 1.27 | 1.37 | –0.89 | –0.78 | –0.02 |
| Ethnicity | 1.16* | –3.65 | 4.68* | 0.37 | –1.05 | –0.14 |
| Behavioral problem | — | 1.04*** | 0.16 | –0.08 | –0.04 | –0.01 |
| Mediating | ||||||
| Familial Obligations | — | –0.48 | 0.27 | 0.34* | — | — |
| Burden | — | — | 0.01 | 0.24** | 0.15*** | 0.01*** |
| Active coping | — | — | — | — | –0.08 | 0.00 |
| Avoidant coping | — | — | — | — | 0.25*** | 0.02*** |
| Independent variable | Endogenous variable | |||||
| Cultural Justification | Burden | Active coping | Avoidant coping | CES-D | GSI | |
| Exogenous | ||||||
| Age | 0.04 | –0.01 | 0.05 | –0.07* | 0.01 | –0.01* |
| Education | –0.20 | 1.28 | 1.32 | –0.87 | –0.79 | –0.02 |
| Ethnicity | 1.56 | –4.02 | 4.42* | 0.50 | –1.05 | –0.14 |
| Behavioral problem | — | 1.08*** | 0.14 | –0.10 | –0.04 | –0.01 |
| Mediating | ||||||
| Familial Obligations | — | –0.12 | 0.35** | 0.17* | — | — |
| Burden | — | — | 0.02 | 0.24*** | 0.15*** | 0.01*** |
| Active coping | — | — | — | — | –0.08 | 0.00 |
| Avoidant coping | — | — | — | — | 0.25*** | 0.02*** |
Note: Dashes indicate the regression coefficients were not estimated because the paths were not hypothesized in the model. CES-D = Center for Epidemiological Studies-Depression Scale; GSI = General Symptom Index.
*p < .05; **p < .01; ***p < .001.
Table 5.
Unstandardized Regression Coefficients Estimated From Fully Recursive Path Models With Familial Obligations and Cultural Justification Predicting Caregivers’ Burden, Coping Style, and Subjective Physical Health (N = 160)
| Independent variable | Endogenous variable | ||||
| Familial Obligations | Burden | Active coping | Avoidant coping | Subjective physical health | |
| Exogenous | |||||
| Age | –0.07*** | –0.05 | 0.08 | –0.04 | 0.01** |
| Education | –0.05 | 1.29 | 1.42 | –0.88 | –0.06 |
| Ethnicity | 1.16* | –3.64 | 4.72* | 0.32 | –0.32* |
| Behavioral problem | — | 1.04*** | 0.17 | –0.08 | –0.03** |
| Mediating | |||||
| Familial Obligations | — | –0.50 | 0.31 | 0.35* | — |
| Burden | — | — | 0.00 | 0.24*** | 0.01 |
| Active coping | — | — | — | — | 0.00 |
| Avoidant coping | — | — | — | — | 0.02** |
| Independent variable | Endogenous variable | ||||
| Cultural Justification | Burden | Active coping | Avoidant coping | Subjective physical health | |
| Exogenous | |||||
| Age | 0.04 | –0.01 | 0.05 | –0.07* | 0.01** |
| Education | –0.19 | 1.30 | 1.36 | –0.86 | –0.06 |
| Ethnicity | 1.57 | –4.02 | 4.49* | 0.45 | 0.32** |
| Behavioral problem | — | 1.07*** | 0.15 | –0.10 | –0.03** |
| Mediating | |||||
| Familial Obligations | — | –0.12 | 0.35*** | 0.17* | — |
| Burden | — | — | 0.01 | 0.24*** | 0.01 |
| Active coping | — | — | — | — | –0.01 |
| Avoidant coping | — | — | — | — | 0.02** |
Note: Dashes indicate that the regression coefficients were not estimated because the paths were not hypothesized in the model.
*p < .05; **p < .01; ***p < .001.
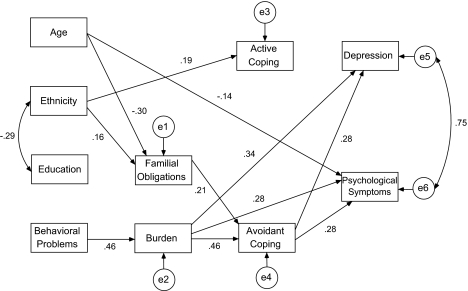
Figure 1.
Fitted path model of Familial Obligations, burden, coping style, and mental health of caregivers (standardized path coefficients).
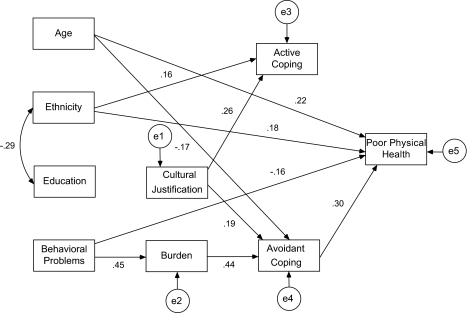
Figure 4.
Fitted path model of Cultural Justification, burden, coping style, and subjective physical health of caregivers (standardized path coefficients).
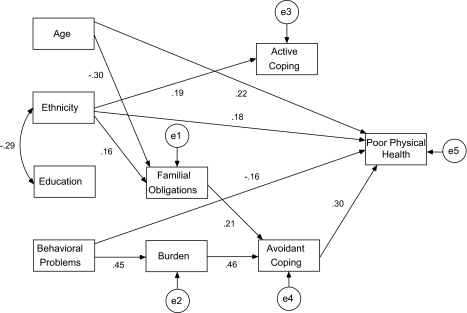
Hypothesis 1 predicted that Familial Obligations would be associated with higher levels of use of avoidant coping, which would result in negative mental and physical health outcomes among family caregivers. This hypothesis received partial support (Figures 1–2) in that Familial Obligations was in fact associated with avoidant coping in all of the models. Moreover, avoidant coping was associated with both poor mental and subjective physical health outcomes.
Figure 2.
Fitted path model of Familial Obligations, burden, coping style, and subjective physical health of caregivers (standardized path coefficients).
Hypothesis 2, that Expected Support from the Family would be related to higher levels of use of active coping that would in turn result in better mental and physical health outcomes among caregivers was not supported at all. Unexpectedly, this cultural value did not have any direct or indirect effects on any of the variables examined in the models in which it was included.
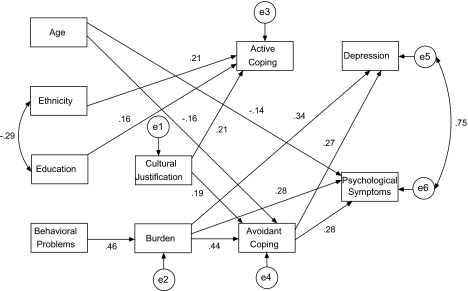
Hypothesis 3 predicted that Cultural Justification would be associated with higher levels of use of active coping, which would lead to better mental and physical health outcomes among caregivers. This hypothesis was partially supported (Figures 3–4) in that Cultural Justification was significantly associated with active coping, yet active coping did not have a significant effect on any of the mental and physical health outcomes in these models. Interestingly, Cultural Justification was also significantly related to avoidant coping, which was in turn related to poor mental and subjective physical health outcomes.
Figure 3.
Fitted path model of Cultural Justification, burden, coping style, and mental health of caregivers (standardized path coefficients).
DISCUSSION
The findings of this study suggest that only one of the two factors of familism—Familial Obligations—affects the mental and physical health of African American and White family caregivers of individuals with dementia. This factor detrimentally affected both the mental and the subjective physical health of the caregivers in this study through avoidant coping. This finding supports the conjecture by Kim and colleagues (2007) that familism scales may tap values of obligation to provide care rather than more than positive feelings about family support. This result is also similar to the finding in a recent study by Losada and colleagues (2010) that found that Familial Obligations was associated with dysfunctional thoughts, which in turn led to depressive symptomatology among their sample of 334 Spanish caregivers. Indeed, it appears as though the Familial Obligations factor accounts for a large proportion of the harmful effects of familism on caregivers’ mental and physical health that has been reported in previous studies.
Interestingly, the Expected Support from the Family factor of familism had neither direct nor indirect effect on this sample of African American and White caregivers’ health outcomes. Although it is conceptually appealing to view positive expectations of familial social support as protective against poor health outcomes for caregivers, this hypothesis did not receive any empirical support in this study. Because this factor is in fact measuring expectations of or beliefs about social support, it is likely that the belief or expectation that family members should provide support to caregivers may lead to poor outcomes if the actual support obtained does not meet expectations. It should be noted that despite the finding that this factor was highly correlated (r = .67, p < .01) with the Familial Obligations factor, it had no significant effects on caregivers’ mental or subjective physical health outcomes. One possible explanation for this finding is that the associations of this factor with other variables in these models are quite different than those of Familial Obligations, especially with regard to the mediating coping variables. Specifically, Familial Obligations was positively associated with avoidant coping in our models, whereas Expected Support from the Family was not significantly associated with either coping style. Given that these two factors tap different aspects of familism and are composed of their own unique items, it does not appear unreasonable that their results differed despite their positive correlation.
The findings regarding the effects of Cultural Justification were mixed and only partially supported the hypothesis. For example, this cultural value was significantly associated with both active and avoidant coping, whereas it was hypothesized that it would only be related to active coping. This finding suggests that high levels of Cultural Justification values motivate high use of both active and avoidant coping styles. This result is analogous to findings that high levels of perceived stress lead to higher use of all coping styles (e.g., Haley et al., 1996; Lazarus & Folkman, 1984). The finding that Cultural Justification was associated with avoidant coping, which in turn led to poor mental and subjective physical health outcomes among these caregivers, was unanticipated. However, this finding partially supports research of Dilworth-Anderson and colleagues (2004) with African American caregivers showing that cultural justifications for caregiving (measured by the CJCS) had a curvilinear effect on caregivers’ psychosocial health. Both very weak and very strong cultural justifications for caregiving predicted poor psychosocial health for the caregivers in this study. The authors suggested that caregivers who provide care due to a strong identification with cultural values and beliefs may be driven to do so out of a sense of obligation. This suggestion may extend to the findings of our study regarding the negative effects of Cultural Justification on caregivers’ mental and subjective physical health.
Other findings from this study warrant comparison with the findings from the Kim and colleagues (2007) study. For example, Kim and colleagues found that higher levels of education were inversely related to familism in their path models. In the current study, education was not associated with either of the factors of familism. Caregivers with higher levels of education may have weaker ties with extended family members. Thus, use of the Bardis (1959) familism scale by Kim and colleagues may account for the inverse relation between education and familism reported in their study. The current study, which used the Sabogal and colleagues (1987) familism scale to derive the familism factors, may be a more appropriate and useful measure of familism as it taps more specific factors of familism involving both attitudinal and behavioral elements of this cultural value.
Our study found that ethnicity was positively associated with Familial Obligations in the path models, a finding that somewhat diverges from the finding of Kim and colleagues (2007) that ethnicity was not associated with familism in their models. In this sample, African American caregivers were more likely to perceive caregiving more as an obligation than were White caregivers. Future research with this measure should seek to understand what this difference means and how it relates to other differences between African American and White caregivers as reported in the literature. Interestingly, in contrast to Familial Obligations, Cultural Justification was not associated with ethnicity in the models. Perhaps, both ethnic groups (African American and White) are motivated by similar cultural explanations for caring for dependent elders.
Limitations
This study has certain limitations that suggest that caution should be used in the interpretation of these results. First, it employed a cross-sectional design and involved a relatively small sample size, which limits the power of the models to assess smaller effects and discern changes in small effects. Second, these models are not causal; instead, they should be regarded as consistent with the observed multivariate covariance structure of this caregiver sample’s data. For both of these reasons, replication with a larger and more diverse sample is needed to clarify the most likely paths in these models. In addition, a longitudinal analysis of the influence of these cultural values on caregivers’ health outcomes would allow for a better understanding of the relation among the variables examined in this study. However, this study does have the benefit of having used probability sampling methods that resulted in a population-based sample recruited from tracts with roughly similar SES backgrounds. Finally, this sample included only African American and White family caregivers. Thus, these findings may not necessarily extend to caregivers belonging to other ethnic groups.
Conclusions
In conclusion, the results of this study make several important contributions to the cultural values and caregiving literature. For example, this study examined some of the specific underlying dimensions that compose the cultural value of familism rather than simply examining familism as a unitary construct, which resulted in a richer understanding of how familism operates to affect African American and White caregivers’ mental and physical health outcomes in the updated sociocultural stress and coping model (Knight & Sayegh, 2010). As a result, it is evident that Familial Obligations account for a substantial proportion of the negative mental and subjective physical health outcomes that caregivers experience as an indirect result of familism. Similar findings were found with the Cultural Justification factor, which may be attributable to providing care out of a sense of duty based on firm cultural values and beliefs. In contrast, Expected Support from the Family had no significant effect on caregivers’ health outcomes in these models. It appears as though cultural values that emphasize feelings of obligation rather than familial solidarity or support tend to have adverse health effects for caregivers. Therefore, a broader finding that can be derived from these results is that it should not be assumed that cultural values have positive effects on the caregiving stress and coping process or health outcomes. Some cultural values may have negative or null effects for certain caregivers. Future research should focus on examining the effects of these cultural values on caregivers’ health outcomes across diverse ethnic groups and search for other cultural values with positive effects for caregivers.
Finally, these findings point to practical implications. Cultural values that have a negative impact on caregivers’ health should be studied further in order to identify therapeutic tools to assist caregivers in highlighting the positive effects of cultural values and decreasing the impact of their negative effects on caregivers’ health. Caregivers’ cultural values should be evaluated to determine whether they tend to emphasize feelings of obligation, which we showed were associated with detrimental mental and physical health outcomes. Cognitive restructuring might be effective for modifying feelings of obligation in the context of caregiving. However, if feelings of obligation stemming from deep-seated cultural values are difficult to modify, interventions aimed at changing an avoidant coping style may prove useful in ameliorating the negative health effects associated with caregiving.
FUNDING
This work was supported by a grant from the National Institute on Aging (R01 AG 16307).
Acknowledgments
We gratefully acknowledge Margaret Gatz, Mara Mather, Brian Lickel, Cecilia Poon, and Jennifer Kellough for their helpful input and feedback on this project.
References
- Aranda MP, Knight BG. The influences of ethnicity and culture on the caregiver stress and coping process: A sociocultural review and analysis. The Gerontologist. 1997;37:342–354. doi: 10.1093/geront/37.3.342. [DOI] [PubMed] [Google Scholar]
- Bardis PD. A familism scale. Marriage and Family Living. 1959;21:340–341. [Google Scholar]
- Barusch AS, Spaid WM. Gender differences in caregiving: Why do wives report greater burden? The Gerontologist. 1989;29:667–676. doi: 10.1093/geront/29.5.667. [DOI] [PubMed] [Google Scholar]
- Bentler PM. On the fit of models of covariance and methodology to the Bulletin. Psychological Bulletin. 1992;112:400–404. doi: 10.1037/0033-2909.112.3.400. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Blumstein T, Lusky A, Modan B. Gender differences in the self-rated health-mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? The Gerontologist. 2003;43:396–405. doi: 10.1093/geront/43.3.396. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit in the analysis of covariance structure. Psychological Bulletin. 1993;88:588–606. [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Chun M, Knight BG, Youn G. Differences in stress and coping models of emotional distress among Korean, Korean-American and White-American caregivers. Aging & Mental Health. 2007;11:20–29. doi: 10.1080/13607860600736232. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Spencer PM. The brief symptoms inventory. Baltimore, MD: Johns Hopkins University; 1985. [Google Scholar]
- Dilworth-Anderson P. Cultural justifications for caregiving scale. 1995 doi: 10.1093/geronb/60.5.s257. Unpublished manuscript. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Goodwin PY, Williams SW. Can culture help explain the physical health effects of caregiving over time among African American caregivers? Journal of Gerontology: Social Sciences. 2004;59:S138–S145. doi: 10.1093/geronb/59.3.s138. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000) The Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- George LK. The social psychology of health. In: Binstock RH, George LK, editors. Handbook of aging and the social sciences. San Diego, CA: Academic Press; 2001. pp. 217–237. [Google Scholar]
- Haley WE, Roth DL, Coleton MI, Ford GR, West CA, Collins RP, Isobe TL. Appraisal, coping, and social support as mediators of well-being in Black and White family caregivers of patients with Alzheimer's disease. Journal of Consulting and Clinical Psychology. 1996;64:121–129. doi: 10.1037//0022-006x.64.1.121. [DOI] [PubMed] [Google Scholar]
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA. Alzheimer disease in the U.S. population: Prevalence estimates using the 2000 census. Archives of Neurology. 2003;60:1119–1122. doi: 10.1001/archneur.60.8.1119. [DOI] [PubMed] [Google Scholar]
- Heller P. Familism scale: A measure of family solidarity. Journal of Marriage and the Family. 1970;32:73–80. [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Jaccard J, Jacoby J. Theory construction and model-building skills: A practical guide for social scientists. New York: Guilford Press; 2010. [Google Scholar]
- Janevic MR, Connell CM. Racial, ethnic, and cultural differences in the dementia caregiving experience: Recent findings. The Gerontologist. 2001;41:334–347. doi: 10.1093/geront/41.3.334. [DOI] [PubMed] [Google Scholar]
- John R, Hennessy CH, Dyeson TB, Garret MD. Toward the conceptualization and measurement of caregiver burden among Pueblo Indian family caregivers. The Gerontologist. 2001;41:210–219. doi: 10.1093/geront/41.2.210. [DOI] [PubMed] [Google Scholar]
- Kim J, Knight BG, Flynn Longmire CV. The role of familism values in stress and coping processes among African American and White dementia caregivers: Effects on mental and physical health. Health Psychology. 2007;26:564–576. doi: 10.1037/0278-6133.26.5.564. [DOI] [PubMed] [Google Scholar]
- Knight B, Silverstein M, McCallum T, Fox L. A sociocultural stress and coping model for mental health outcomes among African American caregivers in Southern California. Journal of Gerontology: Psychological Sciences. 2000;55B:P142–P150. doi: 10.1093/geronb/55.3.p142. [DOI] [PubMed] [Google Scholar]
- Knight BG, Flynn Longmire CV, Dave J, Kim JH, David S. Mental health and physical health of family caregivers for persons with dementia: A comparison of African American and white caregivers. Aging & Mental Health. 2007;11:538–546. doi: 10.1080/13607860601086561. [DOI] [PubMed] [Google Scholar]
- Knight BG, Sayegh P. Cultural values and caregiving: The updated sociocultural stress and coping model. Journal of Gerontology: Psychological Sciences. 2010;65B:5–13. doi: 10.1093/geronb/gbp096. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Kleban MH, Moss M, Rovine M, Glicksman A. Measuring caregiving appraisal. Journal of Gerontology: Psychological Sciences. 1989;44:P61–P71. doi: 10.1093/geronj/44.3.p61. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Levkoff SE, Levy BR, Weitzman PE. The role of religion and ethnicity in the help seeking of family caregivers of elders with Alzheimer's disease and related disorders. Journal of Cross-Cultural Gerontology. 1999;14:335–356. doi: 10.1023/a:1006655217810. [DOI] [PubMed] [Google Scholar]
- Losada A, Márquez-González M, Knight BG, Yanguas J, Sayegh P, Romero-Moreno R. Psychosocial factors and caregivers’ distress: Effects of familism and dysfunctional thoughts. Aging & Mental Health. 2010;14:193–202. doi: 10.1080/13607860903167838. [DOI] [PubMed] [Google Scholar]
- McClendon Baumann VA. Measurement of cultural values regarding dementia caregiving. 2007. Doctoral dissertation. Available from ProQuest Dissertations and Theses database. (UMI No. 3291828) [Google Scholar]
- Nkongho NO, Archbold PG. Reasons for caregiving in African American families. Journal of Cultural Diversity. 1995;2:116–123. [PubMed] [Google Scholar]
- Phinney JS. When we talk about U.S. ethnic groups, what do we mean? American Psychologist. 1996;51:918–927. [Google Scholar]
- Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: A meta-analysis. Journals of Gerontology: Psychological Sciences. 2007;62B:P126–P137. doi: 10.1093/geronb/62.2.p126. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Sabogal F, Marin G, Otero-Sabogal R, Marin BV, Perez-Stable EJ. Hispanic familism and acculturation: What changes and what doesn’t? Hispanic Journal of Behavioral Sciences. 1987;9:397–412. [Google Scholar]
- Schulz R, O’Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- Silverstone B. An overview of research on informal social supports: Implications for policy and practice. Aged Care and Services Review. 1978;1:23–35. [Google Scholar]
- Sörensen S, Pinquart M. Racial and ethnic differences in the relationship of caregiving stressors, resources, and sociodemographic variables to caregiver depression and perceived physical health. Aging & Mental Health. 2005;9:482–495. doi: 10.1080/13607860500142796. [DOI] [PubMed] [Google Scholar]
- Teri L, Truax P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP. Assessment of behavioral problems in dementia: The revised memory and behavior problems checklist. Psychology and Aging. 1992;7:622–629. doi: 10.1037//0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of the Census. Projections of the total resident population by 5-year age groups, race, and Hispanic origin with special age categories: Middle series 1999–2000; middle series 2050–2070. 2000. Retrieved March 13, 2008, from http://www.census.gov/population/projections/nation/summary/np-t4-a.txt. [Google Scholar]
- Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? A meta-analysis. Psychological Bulletin. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- Wallace DC, Witucki JM, Boland CS, Tuck I. Cultural context of caregiving with elders. Journal of Multicultural Nursing and Health. 1998;4:42–48. [Google Scholar]
- Zarit SH, Orr NK, Zarit JM. Families under stress: Caring for the patient with Alzheimer's disease and related disorders. New York: University Press; 1985. [Google Scholar]
- Zarit SH, Reeves KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]