How did the study come about?
The Mauritius Child Health Project is a prospective longitudinal study of child health and development based on a 1969 birth cohort of 1795 children. Originally set up by Professors P.V., S.M. and Fini Schulsinger in 1972, it has its conceptual origins in the successful High-Risk for Schizophrenia Project initiated in Denmark.1 Following the success of this project, the World Health Organization (WHO) Scientific Group on Neurophysiological Research in Psychiatry2 met in 1967 to assess whether neurophysiological methods could be applied to further high-risk studies. The WHO Group outlined the advantages of examining high-risk individuals early in childhood prior to the onset of clinical disorders, and recommended early experimental interventions to alter neurophysiological risk factors for psychopathology. The importance of malnutrition as well as poverty as stressors was highlighted, together with the potential benefits of enhancing educational and health services in a developing country.
The recommendations of the Scientific Group's 1968 report that formed the basis for the Mauritius study were: (i) conduct the study in a developing country; (ii) investigate 3-year-old children; (iii) establish nursery schools as settings for the study; and (iv) use psychophysiological methods to identify children at risk. The initial aim of the study, which would distinguish it from other high-risk studies, was to investigate the possibility of primary prevention of psychopathology by random assignment of 100 children to an environmental enrichment set up in nursery schools, involving better nutrition, more physical exercise and cognitive stimulation.3 P.V. has been the Principal Investigator (PI) of the project from 1972 to 1987, whereas A.R. has been PI from 1987 to the present date.
Where is Mauritius?
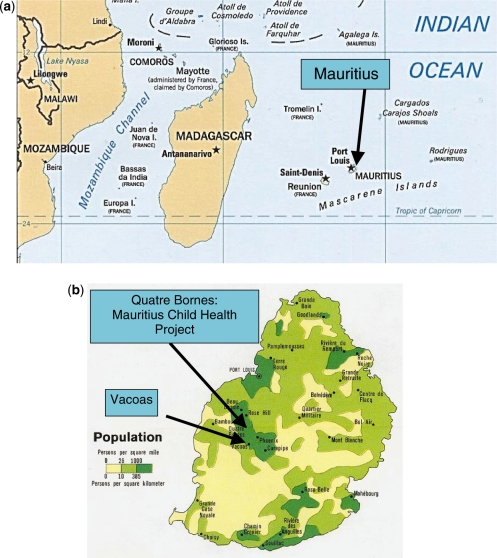
Mauritius is a small tropical island in the Indian Ocean just inside the tropic of Capricorn, lying to the east of Madagascar (Figure 1a). It extends 38 miles (61 km) from north to south and 29 miles (47 km) from east to west (Figure 1b). Part of the African sub-continent, it is a multi-racial democratic nation that gained independence from British rule in 1968, becoming a Republic in 1992. With a population of 1,284,264 as of July 2009, it is the third most densely populated country in the world.
Figure 1.
(a) The location of the African volcanic island of Mauritius in the Indian Ocean, lying west of Madagascar and Mozambique, and making up one of the Mascarene islands. (b) The locations of Quatre Bornes and Vacoas, the two towns making up the original birth cohort in the densely populated central-west area of Mauritius. Dark green areas have more than 1000 people per square kilometre. Population densities are based on data from 1972, the year data collection began in the cohort study [see online for colour version]
Why Mauritius?
The project was initiated in Mauritius because Dr Raman, who was the Medical Director of Brown Sequard Hospital in Mauritius, suggested to the WHO that Mauritius would be a suitable location for their recommended study. The WHO report2 (pp. 33) had initially targeted India as a possible site, but Raman successfully argued for the geographical advantage of Mauritius based on the island's small size and low emigration, permitting subjects to be contacted more readily than in India.
How was it funded?
The initial priming grant ($4000) for a feasibility study was made by WHO in August 1969, based on the recommendations of the Scientific Group on Neurophysiological Research in Psychiatry.2 In April 1970, the Danish State Department for Technical Collaboration with Developing Counties awarded a grant to establish and run the two nursery schools where the environmental enrichment prevention programme would take place. In 1971, the British Medical Research Council (MRC) awarded additional funding to the project to allow psychophysiological examination of 1,795 3-year-old children. Since then the project has been funded by the Government of Mauritius, the Danish International Aid Organization (DANIDA), the MRC (UK), the Wellcome Trust (UK), the Leverhulme Trust (UK), the Mental Health Foundation (UK), the Ford Foundation (USA), the Scottish Rite (USA), the National Institute of Mental Health (NIMH; USA), the National Institute of Alcohol and Alcohol Abuse (NIAAA; USA), and most recently the National Institute of Child Health and Development (NICHD; USA).
What does the study cover?
This longitudinal study covers early child health and development and the identification of early risk factors for later psychopathology, as well as early primary prevention. Because the initial sample recruited all children born in two towns on the island (see below), this community birth cohort has the ultimate potential to cover a wide range of outcomes. In the past two decades the study has focused on outcomes for antisocial/violent behaviour and schizotypal personality, using early psychophysiological, temperamental, health and cognitive predictors. Outcome data are also available on alcoholism, depression, anxiety and personality disorders for future analyses. Early factors that shape later cognitive functioning as well as developmental processes in psychophysiological functioning have been a secondary focus. More recently, the study has additionally covered positive outcomes in life, including curiosity, exploration, achievement and happiness. A randomized controlled trial of the effects of omega-3 fatty acids in reducing childhood behaviour problems and improving cognitive ability in the offspring of the original birth cohort is currently underway.
Who are in the sample?
The original birth cohort consists of 1,795 3-year-old children drawn from polio vaccination records, making up almost the entire population of children born in 1969 in two major towns in a densely populated part of the mid-west of the island (Quatre Bornes and Vacoas; Figure 1b). These towns were chosen due to their central locality to the research laboratory in Quatre Bornes, and because they contained a racial mix very similar to the racial distribution of the island as a whole. The ethnic make up of the sample is Indian (68.5%), Creole (African origin) 25.7%, Chinese 1.8% and others 3.9%, and very closely matches that of the country as a whole. The sample consists of both males (51.4%) and females (48.6%). The Indian group is comprised largely of descendants of indentured labourers brought to the island when it was under British rule, whereas the Creole group is largely comprised of descendants of slaves brought to the island in the 18th and 19th centuries to work on sugar plantations. Hindu makes up the largest religious group (48%), followed by Roman Catholic (23.6%) and Muslim (16.6%). Although the official language is English, the large majority of the population (80.5%) speak Creole (based largely on French, with English, Hindi, Chinese and Malagasy contributions). Since the time of the initiation of the project to date, the medium of teaching in the schools has been mainly English and French, with examinations being held in English.
Although the primary focus has been on the 1,795 children (referred to as generation 2; G2), psychosocial and psychiatric data have also been collected on their parents (G1). In recent years the project has shifted its attention to G3—the offspring of the 1,795 G2 cohort—in an attempt to understand the intergenerational transmission of antisocial behaviour across three generations. Approximately 650 of these G3 children have been enrolled to date.
Significant social and economic changes have taken place in Mauritius since the project's inception. In 1972 Mauritius was still a developing country with a limited infrastructure. Today the country is fully developed with an excellent infrastructure, and is widely viewed as a model African country, with a GDP per capita of $12,100 (2008). One important change is the economic diversification from a mono-crop sugarcane economy to a more diversified employment sector that includes textiles, financial services and tourism, with current expansion into fish processing and information/communications technology. The country's current standings on basic health indicators (with world rankings in parentheses) are as follows: birth rate 14.41/1000 births (146); death rate 6.59/1000 (148); infant mortality rate 12.2 deaths/1000 live births (145); fertility rate 1.81 (156); HIV/AIDS prevalence rate 1.7% (36) and life expectancy 74 years (93).4 School-life expectancy (primary to tertiary education) is 14 years, with a secondary school enrollment ratio of 64.2% (72).5
At the time of the study's inception there were no government preschools on the island. One lasting infrastructure contribution made by the Mauritius Child Health Project, embodied in the 1984 Pre-School Trust Fund Act, has been the establishment of Government preschools based on the two model nursery schools set up by the project in 1972.6 Currently, 183 such schools are running in five educational zones in Mauritius.
How often have they been followed up?
The main birth cohort of 1,795 3-year-old children (G2) have been followed up at ages 8, 11, 17, 23, 28 and 35 years, with a current follow-up at age 40 years. Pregnancy and birth complications data were also collected on this cohort from hospital records.
A total of 200 G2 children were more intensively studied—the 100 who were placed into an environmental enrichment and 100 matched controls. These children were reassessed at ages 4, 5, 6 and 8 years on psychophysiological functioning, height and weight.
The parents (G1) were originally assessed on psychosocial variables when the study began in 1972 and have been followed up when the G2 children were aged 28 years. The G3 offspring of the original G2 birth cohort have been assessed at ages 3–6 and 7–11 years on a wide range of functioning. Some of these G3 children, as well as others not previously tested, are currently involved in an intervention study.
What has been measured?
The study involves three generations of subjects. Relatively little data have been collected on the original G1 parents of the main birth cohort, whereas much more extensive longitudinal data have been collected on the G2 birth cohort itself. Data have been collected on some of the G3 offspring of the birth cohort.
Parents of the birth cohort (G1)
This first generation was interviewed in 1972 when their children (G2) were aged 3 years. Social workers visited the homes of all G1 parents to obtain detailed assessments of home circumstances and demographic information. When their offspring (G2) were aged 28 years, they were interviewed using the Family History-Research Diagnostic Criteria7 to assess psychiatric disorders in the G1 parents, allowing for assessment of the intergenerational transmission of psychiatric disorder.
The birth cohort (G2)
The 1,795 male and female birth cohort was assessed on a wide range of psychophysiological, cognitive, temperamental, behavioural, nutritional, health and psychosocial measures when aged 3 years. Extensive autonomic assessments (skin conductance and heart rate) of arousal, orienting and fear conditioning were conducted.8 Cognitive functioning and intelligence were assessed using the Boehm Test of Basic Concepts.9 Inhibited and disinhibited temperament styles were assessed from observations of the children in the laboratory with their mother and other children,10 as well as fearlessness and stimulation seeking.11 Paediatricians conducted a physical assessment of all children to assess for the seven signs of malnutrition, while blood samples were taken to assess haemoglobin levels.12 At this time, birth record information was also coded from hospital records to assess birth complications.13 Exposure to the 1969 Hong Kong influenza epidemic was also retrospectively assessed in the G1 mothers when pregnant with their G2 offspring in the second and third trimesters of pregnancy.14 From age 3 to 8 years, 200 of the children (100 in the environmental enrichment group and 100 controls) were retested on autonomic functioning every year, using the same paradigm employed at age 3 years, to assess for developmental trajectories of basic information-processing ability, including orienting, habituation and classical conditioning.15
At age 8 years, 1,299 of the original children were rated by their teachers on a checklist for behaviour problems, including antisocial behaviour, aggression, hyperactivity and anxiety.16,17 Psychosocial and demographic data were collected, while height, weight and chest measurements were collected from school medical examinations.
At age 11 years, a major psychophysiological retest was conducted. In addition to repeating the autonomic data collected at age 3 years, additional data were collected on smooth-pursuit eye movements and also electroencephalogram (EEG) and event-related potentials, both at rest and during a continuous performance task.18 Cognitive functioning was assessed using the wechsler scale for children [Wechsler Intelligence Scale for Children (WISC)] and the trail-making test.19 Social workers visited the homes of the parents to collect detailed information on demographics, living conditions and siblings. During this visit parents completed the Child Behavior Checklist (CBCL),20 measuring childhood internalizing and externalizing behaviour problems.
At age 17 years, the sample was assessed on the Revised Behaviour Problem Checklist,21 assessing conduct disorder, socialized aggression, attention problems, motor excess, anxiety/withdrawal and psychotic behaviour, together with a measure of schizotypal personality.22 A computerized neuropsychological tests battery was also administered,23 including the continuous performance task,24 span of apprehension,25 mazes and reaction-time measures.
At age 23 years, assessments were made on self-report crime,3 depression using the Beck Depression Inventory,26 schizotypal personality using the schizotypal personality questionnaire (SPQ),27 alcohol use using the Michigan Alcohol Screening Test28 (MAST), head injury and handedness. All district courts on the islands were searched to track official crime records on the 1,795 participants.
At age 28 years, diagnostic interviews were conducted using SCID I and II (structured clinical interview for axis I and II DSM-IV disorders) to access all axis I and II disorders. Other measures included the stimulant and sedative effects of alcohol, child abuse, handedness and demographic information.
At age 35 years, the new intergenerational phase of the study on G3 (see below) also involved the original cohort of G2 parents. Parents were assessed on parenting skills (see below), daily hassles and uplifts, major life events, suicide ideation, spouse abuse, neighbourhood social cohesion, state and trait anxiety, impulsivity, stimulation seeking, positive and negative affect, a 7-day log of sleep and consumption of alcohol, caffeine, cigarettes and drugs, history of head injury, adult attention deficit hyperactivity disorder (ADHD), and adult attachment and happiness, both across the life-span and also in different social contexts.
At age 40 years, participants are currently engaged in another self-report test wave that repeats some of the negative outcome measures previously obtained, covering reactive and proactive aggression (reactive–proactive questionnaire; RPQ),29 schizotypal personality (SPQ-B),30 psychopathic personality (PSI),31 self-report crime, spouse and child abuse (conflict tactics scale; CTS),32 adult ADHD, alcohol use (Alcohol Use Disorders Scale; AUDIT),33 state-trait anxiety (STAI)34 and depression (Beck Depression Inventory, Beck).26 In addition, positive psychology measures are being taken in order to both assess early life factors that shape positive outcome, and also to assess how they may act as protective factors against negative adult outcome. Measures include achievement, interest and effort,35 life satisfaction, happiness, curiosity and exploration, hope, inspiration, personal growth and income. Basic demographic measures covering income and occupation are also derived.
Offspring of the birth cohort (G3)
The new G3 offspring of the original cohort have been assessed at age 3–4 years, the same age that their parents had been originally tested in the same laboratory ∼30 years earlier. The same autonomic arousal, orienting and habituation measures that had been originally assessed on the parents were included, together with new measures of vagal tone, EEG, event-related potentials and startle blink. New psychophysiological paradigms were added to induce emotions of empathy, fear, reward expectancy and frustration. Comprehensive behavioural test batteries in the laboratory setting included seven measures of inhibitory control and rule-breaking behaviour.36,37 Observational measures were also made of the children interacting with their caregiver in 10 different contexts to derive measures of parenting skills and also children's reactivity to parenting.38,39 Parents also completed measures of child behaviour problems [Child Behavior Checklist(CBC)], 10 dimensions of conscience,40 15 dimensions of temperament,41 parenting hassles and child-rearing agreements.42 Intelligence was assessed using the (Wechsler Preschool and Primary Scale of Intelligence – Revised). Research assistants visited the mother and child at their homes and completed the Home Observation for Measurement of the Environment, which assesses eight dimensions of the quality of the child's home environment,43 together with detailed demographic and psychosocial adversity measures.
At age 7–11 years, another G3 test phase was introduced, which included both older G3 children of the original G2 birth cohort, as well as a retest of some of the G3 children already assessed at age 3 years. Psychophysiological testing was repeated. Parents also completed a demographic interview. Neuropsychological testing was conducted, covering the areas of executive functioning, memory, verbal fluency, colour trails and visuo-spatial functions. Intelligence was also assessed using the WISC-III. Parents again completed the CBC, together with the RPQ.29
What is the attrition?
The original sample consists of 1,795 3-year olds, with data very largely complete on all measures. Sample sizes in later phases are as follows: age 8 years (1,299), age 11 years (1,217), age 17 years (615), age 23 years (1,264–1,795), age 28 years (1,023), age 35 years (652) and age 40 years (763; ongoing). Attrition at age 11 years was due to the fact that a major cyclone brought the testing to a halt after two-thirds of the sample had been tested. Attrition at ages 8 and 17 years was due to both lack of financial resources and also at age 8 years to the difficulty in accessing teachers to rate the children. Attrition at later ages (≥23 years) was due predominantly to lack of funding, subject refusals and inability to locate some participants, as well as loss due to study abroad and emigration. Nevertheless, those tested have not been found to differ from those not tested on gender, ethnicity, IQ, social/demographic factors, antisocial behaviour, temperament, autonomic functioning and body size.11,12,17,44,45. One analysis did find an over-representation of Indians and males in the tested group compared to the non-tested group, but neither variable was found to act as a mediator or confounder.46
What has been found? Key findings and publications
To date there have been 63 journal articles and book chapters published on the Mauritius project, focusing on the development of psychopathology, including externalizing behaviour problems (conduct disorder, aggression, psychopathy and crime) and schizotypal personality. Use has also been made of the data to examine more basic science questions, including the development of intelligence, temperament and autonomic measures of basic information-processing. Table 1 lists selected journal article publications dealing with developmental issues, classified by ‘predictor’ variables and ‘outcome’ variables, together with a brief summary of the main findings. We highlight below a few of the study's main findings to date.
Table 1.
Selected findings from Mauritius Child Health Project
| Outcome | Authors | Predictors | Key findings |
|---|---|---|---|
| Antisocial behaviour | |||
| Aggression | Raine et al. (1997)44 | Resting heart rate | Low resting heart rate at age 3 years predisposes to childhood aggression at age 11 years |
| Aggression | Raine et al. (1998)11 | Temperament and body size | Fearlessness, stimulation-seeking and large body size at age 3 years predispose to childhood aggression at age 11 years |
| Antisocial behaviour | Raine et al. (2002)17 | Cognitive functioning | Spatial but not verbal cognitive deficits at age 3 years predict persistently antisocial behaviour at age 17 years |
| Externalizing behaviour | Liu et al. (2004)46 | Nutritional status | Malnutrition at age 3 years predisposes to externalizing behaviour problems at ages 8, 11 and 17 years |
| Externalizing behaviour | Liu et al. (2009)13 | Birth complications | Birth complications are associated with increased externalizing behaviour at age 11 years |
| Conduct disorder | Venables (1989)58 | Autonomic arousal | Low skin conductance levels at age 11 years characterize those with high conduct disorder scores at age 17 years, particularly girls |
| Crime | Gao et al. (in press)49 | Fear conditioning | Poor autonomic fear conditioning at age 3 years is associated with crime at age 23 years |
| Psychopathy | Glenn et al. (2007)52 | Temperament and psychophysiology | Children aged 3 years with reduced fear, increased stimulation-seeking and increased autonomic arousal and orienting score higher on psychopathy at age 28 years |
| Temperament | |||
| Temperament | Scerbo et al. (1995)10 | Temperament | Inhibited and uninhibited behaviour remains stable from ages 3 to 11 years |
| Temperament | Scarpa et al. (1997)53 | Heart rate, skin conductance | Reduced heart rate and skin conductance at age 3 years characterizes behaviourally disinhibited children |
| Schizotypal personality | |||
| Schizotypal personality | Raine et al. (2002)50 | Autonomic arousal and orienting | Increased psychophysiological arousal and orienting at ages 3 and 11 years characterizes persistently schizotypal adults |
| Schizotypal personality | Venables (1996)14 | Prenatal influenza exposure | Prenatal influenza exposure is associated with increased positive symptom schizotypal personality at age 17 years |
| Psychophysiology | |||
| Autonomic orienting and habituation | Gao et al. (2007)15 | Age (3–8 years) | Electrodermal orienting increases across age but shows a rapid increase from 5 to 6 years when children enter school |
| Autonomic fear conditioning | Gao et al. (in press)51 | Age (3–8 years) | Children at age 3 years evidence fear conditioning and show a substantial increase from 5 to 6 years |
| Autonomic functioning | Venables (1997)47 | Prenatal Influenza exposure | Influenza exposure in the second trimester predicts reduced autonomic functioning at age 3 years |
| Autonomic and central nervous system functioning | Raine et al. (2001)18 | Experimental enhancement of early environment | Better nutrition, more physical exercise and more cognitive stimulation at age 3–5 years increases autonomic and central nervous system arousal and orienting at age 11 years |
| Cognition | |||
| Intelligence | Liu et al. (2003)46 | Nutritional status | Malnutrition at age 3 years is associated with lower cognitive ability at age 11 years, independent of social adversity |
| Intelligence | Raine et al. (2002)19 | Stimulation seeking | Stimulation seeking at age 3 years predicts higher intelligence at age 11 years |
| Intelligence | Lynn et al. (2005a)54 | Gender | Girls at age 3 years score higher than boys on spatial IQ and total IQ |
| Intelligence | Lynn et al. (2005b)55 | Gender | Boys at age 11 years score higher than girls on spatial IQ and total IQ |
| Intelligence | Venables (1983)59 | Autonomic orienting | Boys with an absence of skin conductance orienting at age 3 years have lower verbal IQs at age 6 years |
| Obstetrics | |||
| Delivery complications | Venables et al. (2007)57 | Prenatal influenza exposure | Prenatal influenza exposure increases the risk of delivery complications |
Early prevention of child and adulthood psychopathology
The study has shown that early environmental enrichment in the preschool years both reduces adult psychopathology and also improves brain functioning. Using a stratified, randomized design, we demonstrated that children who received a nutritional, educational and physical exercise enrichment at ages 3–5 years showed reduced conduct disorder at age 17 years and reduced criminal offending at age 23 years.3
The beneficial effects of the intervention tended to be greater for children who had poor nutrition at age 3 years, particularly with respect to conduct disorder at age 17 years. Taking into account early nutritional status, the enrichment resulted in a 53% reduction in conduct disorder (age 17 years), a 41% reduction in hyperactivity (age 17 years), a 34.6% reduction in self-report crime (age 23 years) and a 63.6% reduction in official crime (age 23 years). The moderating effect of early nutritional status suggests (but does not prove) that better nutrition was an active ingredient of the prevention programme. The prevention programme also reduced schizotypal personality at age 17 years, particularly in the malnourished group who showed a 43.2% reduction in psychotic behaviour at age 17 years, a 32.4% reduction in cognitive disorganization, together with a 23.0% reduction in schizotypal personality at age 23 years.3
The facts that the prevention programme reduced crime in a period extending over 20 years and using two different measures of outcome (self-report and objective measures) indicates the robustness of the effects. Results could not be attributed to pre-prevention group differences in temperament, cognitive ability, nutritional status, autonomic reactivity or demographic variables.3 This programme constituted the first attempt at primary prevention of schizotypal personality, a forerunner of schizophrenia, and one of the very few studies to show that prevention efforts in the preschool years can reduce adult crime. Findings have potential public health implications for the prevention of crime and violence, particularly in underserved populations at risk for poor nutrition.
Early health risk factors for childhood and adulthood psychopathology
We have observed significant effects of early nutritional status on later psychopathology. Preschool children at age 3 years who showed signs of protein deficiency, riboflavin deficiency and iron deficiency, showed increased externalizing behaviour (antisocial, aggressive, hyperactive, attention problems) at ages 8, 11 and 17 years. A dose–response relationship was shown between the degree of malnutrition and degree of externalizing behaviour at ages 8 and 17 years.46 Malnutrition at this age was also found to result in poorer cognitive functioning at ages 3 and 11 years,12 and low IQ was found to moderate the malnutrition–antisocial behaviour relationship. These are the first findings to show prospectively that malnutrition assessed in the early postnatal years is associated with externalizing behaviour problems from childhood to late adolescence and also to show the mediating effects of cognitive ability. Findings in turn have potential nutritional implications for public health attempts to prevent the occurrence of externalizing behaviour problems in children and adolescents, particularly since poor nutrition mediated outcome findings in the prevention programme.
Obstetric risk factors for child behaviour problems have also been observed. Babies with birth complications are more likely to develop externalizing behaviour problems at age 11 years.46 Low IQ was associated with birth complications and was found to mediate the link between early predictors and later externalizing behaviour. This is the first large prospective longitudinal study to show a direct effect of birth complications on later childhood externalizing behaviour, and the first to show the mediating effect of low IQ on this relationship.
By chance, some of the participants in the study were in utero at the time of the 1968–72 Hong Kong/A2 influenza virus epidemic that reached Mauritius in January 1970.14 Because maternal exposure to the influenza virus has been associated with the development of schizophrenia in the offspring, use was made of this natural experiment to assess associations between influenza exposure and schizotypal personality. It was shown that those children whose mothers were exposed to the virus in the second or third trimester of pregnancy had elevated schizotypal personality at age 17 years,14 as well as increased electrodermal orienting at age 3 years.47
Early psychophysiological risk factors for childhood and adulthood psychopathology
We have been finding autonomic nervous system (ANS) risk factors for later child and adult psychopathology as early as age 3 years. Children with low resting heart rates at age 3 years were more aggressive at age 11 years, independent of possible confounders such as body size, health and socio-economic conditions.44 Low resting heart rate has become the best-replicated biological risk factor for antisocial behaviour in children and adolescents,48 and is unusual in that it is diagnostically specific—no other form of psychopathology has been associated with low resting heart rate.
More recently, we have demonstrated that poor autonomic fear conditioning at age 3 years is associated with criminal offending 20 years later at age 23 years.49 This is the first longitudinal study to demonstrate an early deficit in autonomic fear conditioning as a predisposition to adult criminality. Findings implicate amygdala and ventral prefrontal dysfunction and a lack of fear to socializing punishments in preschool children who grow up to become criminals, and give rise to a neurodevelopmental theory of crime causation.
Schizotypal personality has also been found to have early psychophysiological underpinnings. Individuals who were persistently schizotypal at both ages 17 and 23 years were found to have increased electrodermal arousal and orienting at both ages 3 and 11 years, as well as reduced slow-wave EEG [i.e. increased Central Nervous System (CNS) arousal] at age 11 years.50 The fact that increased arousal and orienting are found in schizotypal individuals across two early ages and across different psychophysiological measures attests to the robustness of the findings.
Early influences on later cognitive functioning
Although the cohort study has focused on psychopathology, early temperamental, health and environmental influences have also been found for later cognitive functioning. Children who were stimulation seekers at age 3 years as measured through laboratory behavioural tests scored 12 points higher on total IQ at age 11 years, and also performed better on standardized educational tests at age 11 years.11 Findings are the first to show a prospective link between stimulation seeking and intelligence and suggest that young stimulation seekers create for themselves an enriched environment that stimulates cognitive development.
We also observed that children with poor nutrition at age 3 years had lower IQ at age 11 years, together with poorer neuropsychological functioning and poorer school performance.12 Children with three indicators of poor nutrition showed a 15.3-point reduction in IQ at age 11 years. These results remained after controlling for multiple indicators of psychosocial adversity. Findings indicate that early child malnutrition is a risk factor for later cognitive impairments and that from a paediatric standpoint improving nutrition could enhance children's long-term cognitive development.
The early environmental enrichment that reduced adult psychopathology also produced long-term improvements in brain functioning and information-processing. Children who experienced the environmental enrichment at age 3 years showed more alert and aroused EEGs at age 11 years, both at rest and also during performance of a sustained attention task.18 They also showed larger skin conductance responses to orienting stimuli, an indicator of greater allocation of attentional resources to processing environmental stimuli. This is believed to be the first study to show that early environmental enrichment is associated with long-term increases in psychophysiological orienting and arousal in humans.
What are the main strengths and weaknesses?
The Mauritius Child Health Project is a unique birth cohort that incorporates three generations of longitudinal data. The prospective longitudinal design, large sample size, equal representation of males and females and ethnic diversity are all methodological strengths. The fact that data collection spans 37 years, with follow-up from age 3 (as well as birth) to age 40 years is unusual. The small size of the island, the location of research facilities in Quatre Borne in the centre of the island and low emigration rate facilitates subject tracking for multi-wave data collection and future follow-ups. It is also the largest and most comprehensive prospective longitudinal study on ANS and CNS psychophysiological measures in the world. To our knowledge, it is probably the largest, most comprehensive and longest-running longitudinal study on child health and development from Africa.
The strong methodological design has resulted in several first findings: (i) the demonstration that an experimental environmental enrichment in young children improves brain and autonomic functioning 8 years later;18 (ii) the finding that this early prevention programme reduces schizotypal personality (as well as crime) in adulthood;3 (iii) the first longitudinal study showing sustained effects of early malnutrition on externalizing behaviour throughout childhood and adolescence;46 (iv) the linking of prenatal influenza exposure to teenage schizotypal personality;14 (v) the first establishment of poor fear conditioning in childhood as a risk factor to adult crime;49 and (vi) the first to document the development trajectory of psychophysiological information-processing in early childhood.45,51
These strengths should be balanced with several limitations. First, as with many longitudinal studies, there is attrition in later data collection phases, although we are still able to recruit relatively large numbers that give sufficient power for statistical analyses, with little evidence of selection bias. Secondly, do findings from Mauritius in Africa generalize to other African and Western countries? Perhaps surprisingly, to date we find that with very few exceptions results from Mauritius parallel those from Western countries in terms of risk factors for antisocial behaviour,44 psychopathy,52 schizotypal personality,50 nutrition,46 temperament,11,53 intelligence,54,55 fear conditioning,51 psychophysiology8 and personality.56 These findings indicate cross-cultural generalizability of prior Western findings, and also show that theoretical conceptualizations of the aetiology of psychopathology from the West find substantiation in Mauritius. A third limitation is that, as with all lengthy longitudinal studies, there is a question of whether findings from a prior generation apply to today's research participants, although to date we have found theoretical commonalities in findings from the Mauritius cohort to current-day populations.
Can I get access to the data? Where can I find out more?
Mechanisms for data sharing are under development. Institutional Review Board approval would be required for accessing data. To obtain more information on the research project and to explore potential collaborations, contact the PI, A.R. (araine@sas.upenn.edu). A comprehensive annotated bibliography of all findings from all sources is also available from the first author, which includes reports in book chapters, conference proceedings and conference presentations in addition to the journal articles publications listed in Table 1.
Funding
World Health Organization (WHO), the Danish State Department for Technical Collaboration with Developing Counties, the British Medical Research Council (MRC) the Ministries of Health and Education in Mauritius, the Danish International Aid Organization (DANIDA), the Medical Research Council (UK), the Wellcome Trust (UK), the Leverhulme Trust (UK), the Mental Health Foundation (UK), the Ford Foundation (USA), the Scottish Rite (USA), the National Institute of Mental Health (NIMH; USA), the National Institute of Alcohol and Alcohol Abuse (NIAAA; USA) and the National Institute of Child Health and Development (NICHD; USA).
Acknowledgements
The authors wish to thank all the participants and staff of the Joint Child Health Project for making this research possible.
Conflicts of Interest: None declared.
References
- 1.Mednick SA, Schulsinger F. Some pre-morbid characteristics related to breakdown in children with schizophrenic mothers. In: Rosenthal D, Kety SS, editors. The Transmission Of Schizophrenia (267–291) New York: Pergamon Press; 1968. [Google Scholar]
- 2.WHO Scientific Group. WHO Technical Report No. 381. Geneva: World Health Organization; 1968. Neurophysiological and Behavioural Research in Psychiatry. [PubMed] [Google Scholar]
- 3.Raine A, Mellingen K, Liu J, Venables PH, Mednick SA. Effects of environmental enrichment at 3–5 years on schizotypal personality and antisocial behavior at ages 17 and 23 years. Am J Psych. 2003;160:1627–35. doi: 10.1176/appi.ajp.160.9.1627. [DOI] [PubMed] [Google Scholar]
- 4.Central Intelligence Agency: The World Factbook. http://www.cia.gov/library/publications/the-world-factbook/geos/mp.html (13 November 2009, date last accessed)
- 5.NationMaster. http://www.nationmaster.com/graph/edu_enr_rat_sec_lev-education (13 November 2009, date last accessed)
- 6.UNESCO. EFA Global Monitoring Report 2007: Strong Foundations: Early Childhood Care and Education. Paris: UNESCO Publishing; 2007. [Google Scholar]
- 7.Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Arch Gen Psych. 1977;34:1229–35. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- 8.Venables PH. Psychophysiology and psychometrics. Psychophysiology. 1978;15:302–15. doi: 10.1111/j.1469-8986.1978.tb01383.x. [DOI] [PubMed] [Google Scholar]
- 9.Boehm A. Boehm Test of Basic Concepts—Preschool Version. San Antonio: Psychological Corporation; 1986. [Google Scholar]
- 10.Scerbo A, Raine A, Venables PH, Mednick SA. The stability of inhibited/uninhibited temperament from ages 3 to 11 years in Mauritian children. J Abnormal Child Psychology. 1995;23:607–18. doi: 10.1007/BF01447665. [DOI] [PubMed] [Google Scholar]
- 11.Raine A, Reynolds C, Venables PH, Mednick SA, Farrington DP. Fearlessness, stimulation-seeking, and large body size at age 3 years as early predispositions to childhood aggression at age 11 years. Arch Gen Psychiatry. 1998;55:745–51. doi: 10.1001/archpsyc.55.8.745. [DOI] [PubMed] [Google Scholar]
- 12.Liu J, Raine A, Venables PH, Dalais C, Mednick SA. Malnutrition at age 3 years and lower cognitive ability at age 11: Independence from social adversity. Arch Pediat Adolesc Med. 2003;157:593–600. doi: 10.1001/archpedi.157.6.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu J, Raine A, Wuerker A, Venables PH, Mednick SA. The association of birth complications and externalizing behavior in early adolescents: Direct and mediational effects. J Res Adolesc. 2009;19:93–111. doi: 10.1111/j.1532-7795.2009.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Venables PH. Schizotypy and maternal exposure to influenza and to cold temperature: The Mauritius study. J Abnormal Psychology. 1996;105:53–60. doi: 10.1037//0021-843x.105.1.53. [DOI] [PubMed] [Google Scholar]
- 15.Gao Y, Raine A, Dawson ME, Venables PH, Mednick SA. Development of skin conductance orienting, habituation, and reorienting from ages 3 to 8 years: a longitudinal latent growth curve analysis. Psychophysiology. 2007;44:855–63. doi: 10.1111/j.1469-8986.2007.00564.x. [DOI] [PubMed] [Google Scholar]
- 16.Venables PH, Fletcher RP, Dalais JC, Mitchell DA, Schulsinger F, Mednick SA. Factor structure of the Rutter Children's Behavior Questionnaire in a primary school population in a developing country. J Child Psychology Psychiatry. 1983;24:213–22. doi: 10.1111/j.1469-7610.1983.tb00570.x. [DOI] [PubMed] [Google Scholar]
- 17.Raine A, Yaralian PS, Reynolds C, Venables PH, Mednick SA. Spatial but not verbal cognitive deficits at age 3 years in persistently antisocial individuals. Dev Psychopathology. 2002;14:25–44. doi: 10.1017/s0954579402001025. [DOI] [PubMed] [Google Scholar]
- 18.Raine A, Venables PH, Dalais C, Mellingen K, Reynolds C, Mednick SA. Early educational and health enrichment at age 3–5 years is associated with increased autonomic and central nervous system arousal and orienting at age 11 years: evidence from the Mauritius Child Health Project. Psychophysiology. 2001;38:254–66. [PubMed] [Google Scholar]
- 19.Raine A, Reynolds C, Venables PH, Mednick SA. Stimulation-seeking and intelligence: A prospective longitudinal study. J Person Soc Psychology. 2002;82:663–674. [PubMed] [Google Scholar]
- 20.Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1983. [Google Scholar]
- 21.Quay HC, Peterson DR. Manual for the Revised Behavior Problem Checklist. Coral Gables, FL: Department of Psychology: University of Miami; 1987. [Google Scholar]
- 22.Venables PH, Wilkins S, Mitchell DA, Raine A. Bailes, K. A scale for the measurement of schizotypy. Person Individual Diff. 1990;11:481–95. [Google Scholar]
- 23.Levander S. Evaluation of cognitive impairment using a computerized neuropsychological test battery. Nordic. J Psychiatry. 1987;41:417–422. [Google Scholar]
- 24.Cornblatt BA, Lenzenweger MF, Erlenmeyer-Kimling L. The Continuous Performance Test, Identical Pairs Version: II. Contrasting attentional profiles in schizophrenic and depressed patients. Psychiatry Res. 1989;29:65–85. doi: 10.1016/0165-1781(89)90188-1. [DOI] [PubMed] [Google Scholar]
- 25.Asarnow RF, Nuechterlein KH, Marder SR. Span of apprehension performance, neuropsychological functioning, and indices of psychosis-proneness. J Ner Men Dis. 1983;171:662–69. doi: 10.1097/00005053-198311000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Beck AT. Depression: Clinical, Experimental and Theoretical Aspects. New York: Harper and Row; 1967. [Google Scholar]
- 27.Raine A. The Schizotypal Personality Questionnaire (SPQ): a measure of schizotypal personality based on DSM-III-R criteria. Schizo Bull. 1991;17:555–64. doi: 10.1093/schbul/17.4.555. [DOI] [PubMed] [Google Scholar]
- 28.Selzer ML. The Michigan alcoholism screening test: the quest for a new diagnostic instrument. Am J Psychiatry. 1971;127:89–94. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- 29.Raine A, Dodge K, Loeber R, Gatzke-Kopp L, Lynam D, Reynolds C, Stouthamer-Loeber M, Liu J. The Reactive-Proactive Aggression Questionnaire: differential correlates of reactive and proactive aggression in adolescent boys. Aggr Behav. 2006;32:159–171. doi: 10.1002/ab.20115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raine A, Benishay D. The SPQ-B: a brief screening instrument for schizotypal personality disorder. J Person Dis. 1995;9:346–55. [Google Scholar]
- 31.Lilienfeld SO, Andrews BP. Development and preliminary validation of a self-report measure of psychopathic personality traits in noncriminal populations. J Person Assess. 1996;66:488–524. doi: 10.1207/s15327752jpa6603_3. [DOI] [PubMed] [Google Scholar]
- 32.Straus MA, Gelles RJ. Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8145 Families. New Brunswick: Transaction Publishers; 1990. [Google Scholar]
- 33.Allen JP, Reinert DF, Volk RJ. The Alcohol Use Disorders Identification Test: an aid to recognition of alcohol problems in primary care patients. Prev Med. 2001;33:428–33. doi: 10.1006/pmed.2001.0910. [DOI] [PubMed] [Google Scholar]
- 34.Spielberger CD, Gorusch RL, Lushene RE. Manual for the State-Trait Anxiety Scale. Palo Alto: Consulting Psychologists Press; 1970. [Google Scholar]
- 35.Duckworth AL, Quinn PD. Development and validation of the Short Grit Scale (Grit-S) J Person Assess. 2009;91:166–74. doi: 10.1080/00223890802634290. [DOI] [PubMed] [Google Scholar]
- 36.Kochanska G, Aksan N, Koenig AL. A longitudinal study of the roots of preschoolers' conscience: committed compliance and emerging internalization. Child Dev. 1995;66:1752–69. [PubMed] [Google Scholar]
- 37.Kochanska G, Murray K, Jacques TY, Koenig AL. Inhibitory control in young children and its role in emerging internalization. Child Dev. 1996;67:490–507. [PubMed] [Google Scholar]
- 38.Belsky J, Rovine M, Fish M. The developing family system. In M Gunnar, E Thelen (eds) Systems and Development, Vol. 22. Minnesota Symposia on Child Psychology. 1989:119–66. [Google Scholar]
- 39.Belsky J, Youngblade L, Rovine M, Volling B. Patterns of marital change and parent–child interaction. J Marriage Family. 1991;53:487–98. [Google Scholar]
- 40.Kochanska G, DeVet K, Goldman M, Murray K, Putnam SP. Maternal reports of conscience development and temperament in young children. Child Dev. 1994;65:852–68. [PubMed] [Google Scholar]
- 41.Rothbart MK, Ahadi SA, Hershey KL, Fisher P. Investigations of temperament at three to seven years: The children's behavior questionnaire. Child Dev. 2001;72:1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- 42.Jouriles EN, Murphy CM, Farris AM, Smith DA, Richters JE, Waters E. Martial adjustment, parental disagreements about child rearing, and behavior problems in boys: Increasing the specificity of the martial assessment. Child Dev. 1991;62:1424–33. [PubMed] [Google Scholar]
- 43.Caldwell BM, Bradley RH. Home Observation for Measurement of the Environment (revised edition) Little Rock: U Arkansas, Center for Child Development and Education; 1984. [Google Scholar]
- 44.Raine A, Venables PH, Mednick SA. Low resting heart rate at age 3 years predisposes to aggression at age 11 years: Findings from the Mauritius Joint Child Health Project. J Am Acad Child Adolesc Psychiatry. 1997;36:1457–64. doi: 10.1097/00004583-199710000-00029. [DOI] [PubMed] [Google Scholar]
- 45.Gao Y, Raine A, Dawson ME, Venables PH, Mednick SA. Development of skin conductance orienting, habituation, and reorienting from ages 3 to 8 years: A longitudinal latent growth curve analysis. Psychophysiology. 2007;44:855–63. doi: 10.1111/j.1469-8986.2007.00564.x. [DOI] [PubMed] [Google Scholar]
- 46.Liu JH, Raine A, Venables PH, Mednick SA. Malnutrition at age 3 years and externalizing behavior problems at ages 8, 11 and 17 years. Am J Psychiatry. 2004;161:2005–13. doi: 10.1176/appi.ajp.161.11.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Venables PH. Maternal exposure to influenza and cold in pregnancy, and electrodermal activity in offspring: The Mauritius study. Psychophysiology. 1997;34:427–35. doi: 10.1111/j.1469-8986.1997.tb02386.x. [DOI] [PubMed] [Google Scholar]
- 48.Ortiz J, Raine A. Heart rate level and antisocial behavior in children and adolescents: A meta-analysis. J Am Acad Child Adolesc Psychiatry. 2004;43:154–62. doi: 10.1097/00004583-200402000-00010. [DOI] [PubMed] [Google Scholar]
- 49.Gao Y, Raine A, Venables PH, Mednick SA. Poor fear conditioning at age 3 years predisposed to adult crime at age 23. Am J Psychiatry. doi: 10.1176/appi.ajp.2009.09040499. (in press) [DOI] [PubMed] [Google Scholar]
- 50.Raine A, Venables PH, Mednick SA, Mellingen K. Increased physiological arousal and orienting at ages 3 and 11 years in persistently schizotypal adults. Schizophrenia Research. 2002;54:77–85. doi: 10.1016/s0920-9964(01)00354-1. [DOI] [PubMed] [Google Scholar]
- 51.Gao Y, Raine A, Venables PH, Dawson ME, Mednick SA. The development of electrodermal fear conditioning in children from ages 3 to 8 years. Dev Science. doi: 10.1111/j.1467-7687.2009.00874.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Glenn AL, Raine A, Venables PH, Mednick SA. Early temperamental and psychophysiological precursors of adult psychopathic personality. J Abnormal Psychology. 2007;116:508–18. doi: 10.1037/0021-843X.116.3.508. [DOI] [PubMed] [Google Scholar]
- 53.Scarpa A, Raine A, Venables PH, Mednick SA. Heart rate and skin conductance in behaviorally inhibited Mauritian children. J Ab Psychology. 1997;106:182–190. doi: 10.1037//0021-843x.106.2.182. [DOI] [PubMed] [Google Scholar]
- 54.Lynn R, Raine A, Venables PH, Mednick SA. Sex differences in 3-year-olds on the Boehm Test of Basic Concepts: Some data from Mauritius. Person Individ Diff. 2005;39:683–88. [Google Scholar]
- 55.Lynn R, Raine A, Venables PH, Mednick SA, Irwing P. Sex differences on the WISC-R in Mauritius. Intelligence. 2005;33:527–34. [Google Scholar]
- 56.Reynolds CA, Raine A, Mellingen K, Venables PH, Mednick SA. Three factor model of schizotypal personality: Invariance across culture, gender, religious affiliation, family adversity, and psychopathology. Schizophrenia Bulletin. 2000;26:603–618. doi: 10.1093/oxfordjournals.schbul.a033481. [DOI] [PubMed] [Google Scholar]
- 57.Venables PH, Liu J, Raine A, Mednick SA. Prenatal influenza exposure and delivery complications: Implications for the development of schizophrenia. Fam Comm Health. 2007;30:151–59. doi: 10.1097/01.fch.0000264412.28389.89. [DOI] [PubMed] [Google Scholar]
- 58.Venables PH. The Emanuel Miller Memorial Lecture 1987: childhood markers for adult disorders. J Child Psychology Psychiatry. 1989;30:347–64. doi: 10.1111/j.1469-7610.1989.tb00251.x. [DOI] [PubMed] [Google Scholar]
- 59.Venables PH. Outcome at age nine of psychophysiological selection at age three for risk of schizophrenia: a Mauritian study. British J Dev Psychology. 1983;1:21–30. [Google Scholar]