Abstract
Background.
Higher protein diets are promoted for effective weight loss. Striated tissues in omnivorous diets contain high-quality protein, but limited data exist regarding their effects on bone.
Methods.
To examine the effects of energy restriction–induced weight loss with higher protein omnivorous diets versus lower protein vegetarian diets on bone mineral density in overweight postmenopausal women, two randomized controlled feeding studies were conducted. In Study 1, 28 women consumed 750 kcal/day energy deficit diets with 18% energy from protein via lacto-ovo vegetarian sources (normal protein, n = 15) or 30% energy from protein with 40% of protein from lean pork (higher protein, n = 13, omnivorous) for 12 weeks. In Study 2, 54 women consumed their habitual diet (control, n = 11) or 1,250 kcal/day diets with 16% energy from nonmeat protein sources (n = 14) or 26% energy from protein, including chicken (n = 15) or beef (n = 14) for 9 weeks.
Results.
Study 1: With weight loss (normal protein −11.2%, higher protein −10.1%), bone mineral density was not significantly changed in normal protein (−0.003 ± 0.003 g/cm2, −0.3%) but decreased in higher protein (−0.0167 ± 0.004 g/cm2, −1. 4%, group-by-time p < .05). Study 2: The control, nonmeat, chicken, and beef groups lost 1.5%, 7.7%, 10.4%, and 8.1% weight and 0.0%, 0.4%, 1.1%, and 1.4% bone mineral density, respectively. The change of bone mineral density was significant for chicken and beef compared with the control (group-by-time, p < .05). Markers of calcium metabolism and bone homeostasis in blood and urine were not changed over time or differentially affected by diet.
Conclusion.
Consumption of higher protein omnivorous diets promoted decreased bone mineral density after weight loss in overweight postmenopausal women.
Keywords: Protein, Weight loss, Bone mineral density
WEIGHT loss is recommended for overweight and obese adults to promote health, including improved insulin sensitivity and cardiovascular function (1). However, weight loss increases the rate of bone mineral density (BMD) loss (2). Moderately higher protein (22%–29% of energy) or higher protein (>30% of energy) diets are popular for weight loss, in part, because they may help preserve lean body mass (3,4). The impact of dietary protein on bone remains controversial. Some researchers observed that inadequate or excessive protein intakes adversely affected BMD (5,6), whereas adequate protein intake helped minimize BMD loss in older persons (7). Other researchers reported no association between protein intake and bone (8). Some (9,10), but not all (7), researchers also found that animal protein, compared with plant protein, was more detrimental to bone due to increased urinary calcium excretion.
Data are limited on the potential impact of dietary protein on bone during weight loss. In premenopausal women and similarly aged men, ingestion of an energy-restricted diet with 25% versus 12% energy from protein diminished the loss of bone mineral content after 6 months (11). Overweight participants who consumed energy-restricted diets with 27% versus 16% of energy from protein for 4 months did not experience adverse changes in markers of bone turnover (4). In middle-aged men and women who consumed an energy-restricted diet with 34% protein for 12 weeks, markers of bone resorption (urinary deoxypyridinoline) and bone formation (plasma osteocalcin) increased, indicating higher bone turnover (12). The changes in these markers were blunted when the protein was dairy based compared with an isonitrogenous diet from mixed protein sources (12). Recent research (13) suggested that achieving a higher protein intake (1.4 vs 0.8 g·kg−1·day−1), mainly from dairy, attenuated BMD loss after a 4-month period of energy restriction–induced weight loss.
Collectively, these data document that weight loss and the quantity and source of dietary protein may influence BMD and bone turnover markers. The paucity of data, the contradiction of results, and the popularity and potential enhanced efficacy of higher protein intake during energy restriction and weight loss underscore the need for additional research on the impact of protein quantity and source on BMD and markers of bone formation and resorption. The purposes of this research are to assess the influence of higher protein intake and the inclusion of striated tissue in the diet (ie, an omnivorous diet) during energy restriction on BMD and markers of bone turnover in overweight and moderately obese postmenopausal women, a population at high risk for osteoporosis, from two controlled feeding studies.
METHODS
Study 1 and Study 2: Ethics and Protocol Registration
The Purdue University Institutional Review Board approved the protocols and procedures for both studies. All participants provided written informed consent and received monetary reimbursement.
Study 1: Experimental Design
This 13-week protocol included a 1-week baseline and a 12-week dietary intervention with energy restriction. The participants were randomly assigned to one of two energy-restricted diets that differed in macronutrient distribution. Testing was conducted at baseline and postintervention.
Study 1: Experimental Participants
The exclusion criteria were men; aged <20 years; body mass index <25 and >37 kg/m2 at screening; clinically abnormal kidney, liver, or heart function; clinically abnormal protein or hematological status; diagnosed diabetes mellitus or receiving insulin replacement therapy; and smoker. Fifty-four women were eligible and started the intervention; 46 women completed the study (Supplementary Figure 1). Data from all 46 women were used to assess the effects of higher protein intake on body composition and satiety (3). The current analyses utilized data from the 28 postmenopausal women (higher protein: n = 13, normal protein: n = 15) to avoid potential confounding effects of menstrual status on weight loss–induced changes in bone.
Study 1: Energy-Restricted Diet Intervention
All participants consumed a diet with 750 kcal/day less than their estimated energy requirement and contained either the recommended dietary allowance of 0.8 g·kg−1·day−1 (normal protein group) or 175% of the recommended dietary allowance (1.4 g·kg−1·day−1, higher protein group) for protein based on the participants’ screening body masses. The higher protein diet contained 30% of energy from protein, 45% carbohydrate, and 25% fat; the normal protein diet contained 18% protein, 57% carbohydrate, and 25% fat.
The participants were counseled to follow 7-day menus with specified quantities of typical and brand-specific food items to purchase and consume. These menus were void of animal flesh foods (ie, striated tissues). The higher protein group was provided with portioned quantities of cooked pork (loin, ham, or Canadian bacon) products comprising 40% of their total protein intake, whereas the normal protein group was given portioned quantities of milk comprising 13% of their total protein intake. Thus, the higher protein diet was omnivorous, and the normal protein diet was lacto-ovo vegetarian. This study was not designed to compare sources of protein (meat vs dairy). Milk was given to the normal protein group to equalize the interactions and contact time with the higher protein group. The higher protein and normal protein diets had comparable amounts of protein from dairy: 42 and 36 g/day, respectively, based on a typical 1,550 kcal/day diet. All participants consumed daily a multivitamin/mineral tablet (Centrum; Wyeth Consumer Healthcare, Madison, NJ) and two calcium citrate tablets (400 mg calcium/tablet consumed in the morning and evening, total 800 mg calcium/day). For more detailed descriptions of the dietary intervention, see Leidy and colleagues (3).
Study 2: Experimental Design
This 11-week protocol included a 2-week baseline and a 9-week dietary intervention. The participants were randomly assigned to a nonintervention control group (CONTROL) or one of three energy-restricted groups (CARB, CHICKEN, BEEF). Testing was conducted at baseline and postintervention.
Study 2: Experimental Participants
The exclusion criteria were men; age <50 or >80 years; <2-year postmenopausal; body mass index <25 and >34 kg/m2 at screening; clinically abnormal kidney, liver, or heart functions; clinically abnormal protein or hematological status; diagnosed diabetes mellitus or receiving insulin replacement therapy; smoker; and use of antiinflammatory steroid medications. Fifty-seven women who were eligible started the protocol and were randomized to one of the four groups. Fifty-four women completed the study (CONTROL n = 11; CARB n = 14; CHICKEN n = 15; and BEEF n = 14; Supplementary Figure 2).
Study 2: Diet Intervention
The women in the three energy-restricted groups were counseled to consume the same 1,000 kcal/day lacto-ovo vegetarian basal diet (5-day fixed rotation menu consisting of three meals plus two snacks) and were provided with 250 kcal/day of shortbread cookies and sugar-coated chocolates (CARB), cooked breast meat chicken (CHICKEN; plus 10 g butter to match the total and saturated fat contents of the beef), or beef tenderloin (BEEF). Thus, the CARB diet was vegetarian, and the CHICKEN and BEEF diets were omnivorous. Details of the counseling and food preparation procedures are published (14). The 1,250 kcal/day diet of the CARB group was designed to contain 58% of energy from carbohydrate, 16% protein, and 26% fat, whereas the CHICKEN and BEEF group’s diets contained 48% carbohydrate, 26% protein, and 26% fat. The CONTROL participants continued to consume their usual diets and did not purposefully alter their eating behavior or change body mass. At baseline and post, each participant’s energy and macronutrient intakes were estimated from 3-day food records (Nutritionist Pro software; First databank, San Bruno, CA).
Each woman was requested to stop using nutritional supplements that were not recommended by a physician, nonprescription medications, and alcohol 3 weeks prior to and throughout the study. Twenty-nine of the 54 women who completed the study used calcium supplements (8 CARB, 9 CHICKEN, 8 BEEF, and 4 CONTROL) during the study. For more details of the dietary intervention, see Mahon and colleagues (14).
Study 1 and Study 2: Body Composition Measures
Each participant’s fasting-state mass and height were measured, and body mass index (kg/m2) was calculated. Body composition, whole body BMD (g/cm2), bone mineral content (g), and bone area (cm2) were measured using a dual-energy x-ray absorptiometer (GE LUNAR Prodigy with EnCORE software version 5.60, Madison, WI). The participant was asked to lie still on an x-ray table for less than 30 min while the measurements were being taken.
Blood and Urine Sampling and Analyses
For Study 1, fasting-state venous blood samples taken postintervention were analyzed for blood urea nitrogen using a photometric assay (Chemistry Immuno Analyzer aU5700; Olympus, Center Valley, PA) by MidAmerica Clinical Laboratories.
For Study 2, fasting-state venous blood samples were collected at baseline and postintervention, processed to obtain plasma and serum, and aliquots stored at −20°C. Measurements of serum osteocalcin (marker of bone formation), bone alkaline phosphatase (marker of bone formation), parathyroid hormone (marker of calcium homeostasis), and insulin-like growth factor 1 (IGF-1, associated with BMD in older humans) were made. The analytical methods used were osteocalcin—enzyme-linked immunosorbent assays (ELISA), Quidel Corp., San Diego, CA; bone alkaline phosphatase—ELISA, Quidel Corp.; parathyroid hormone—immunoradiometric assay, Nichols Institute, San Juan Capistrano, CA; and IGF-1—radioimmunoassay, Diagnostics Systems Laboratories, Webster, TX.
For Study 2, 24-hour urine collections were made at baseline and postintervention. Aliquots were stored at −20°C and N-telopeptide cross-links, free deoxypyridinoline (markers of bone resorption rate), creatinine, calcium, phosphorous, and total nitrogen were measured. The analytical methods used were N-telopeptide cross-links—ELISA, Ostex International, Seattle, WA; free deoxypyridinoline—ELISA, Quidel Corp.; creatinine—Cobas Mira with Jaffe Kinetic assay, Roche Diagnostics, Indianapolis, IN; calcium—Cobas Mira with Arsenazo III assay, Roche Diagnostics; phosphorous—Cobas Mira with ammonium molybdate assay, Roche Diagnostics; and total nitrogen—Leco model FP-528, Leco, St. Joseph, MI.
Potential Renal Acid Load Estimations
Participants’ micronutrient intakes were estimated using Nutrition Data System for Research 2008 software (University of Minnesota Nutrition Data System for Research). Potential renal acid load (PRAL, mEq/day) of the diets was estimated as follows (15):
For Study 1, PRAL was evaluated using representative menus from the normal protein and higher protein diets at three energy levels (1,200, 1,500, and 1,700 kcal/day). For Study 2, PRAL was estimated for the BEEF, CHICKEN, and CARB diets.
Statistical Analyses
Data were analyzed using PROC GLM (SAS version 9.1.2; SAS Institute Inc, Cary, NC). Repeated measures ANOVA was performed to access the main effects of group and time, and the group-by-time interaction. In Study 1, t tests were used for post hoc analyses to detect differences within (paired t test; pre vs post) and between (independent t test) the normal protein and higher protein groups. In Study 2, Dunnett’s test of multiple comparisons was used for post hoc analyses to detect differences between treatment groups and the control group. Paired t test was used to examine the difference within groups (pre vs post). Data are presented as mean ± SEM. Statistical significance was accepted at p < .05.
RESULTS
Study 1: Participant Characteristics and Body Composition
There was no difference at baseline or differential change over time in height, body mass, body mass index, fat mass, and fat-free mass between the normal protein and higher protein groups (Table 1).
Table 1.
Study 1: Participant Characteristics and Body Composition at Baseline and Post*
| Parameter | Group | Baseline | Post | Change |
| Age†(y) | Normal protein | 60 ± 3 | ||
| Higher protein | 51 ± 2 | |||
| Height (cm) | Normal protein | 164 ± 2 | ||
| Higher protein | 163 ± 2 | |||
| Weight‡ (kg) | Normal protein | 80.0 ± 2.9 | 71.0 ± 2.6 | −9.1 ± 0.8 |
| Higher protein | 82.5 ± 4.2 | 74.3 ± 4.0 | −8.2 ± 0.5 | |
| Body mass index‡ (kg/m2) | Normal protein | 30.0 ± 0.9 | 26.4 ± 0.8 | −3.4 ± 0.3 |
| Higher protein | 30.8 ± 1.1 | 27.7 ± 1.1 | −3.1 ± 0.2 | |
| Fat mass‡ (kg) | Normal protein | 35.6 ± 1.8 | 28.7 ± 1.8 | −6.9 ± 0.6 |
| Higher protein | 36.8 ± 2.5 | 30.2 ± 2.6 | −6.6 ± 0.5 | |
| Fat-free mass‡ (kg) | Normal protein | 41.8 ± 1.3 | 39.7 ± 1.1 | −2.2 ± 0.4 |
| Higher protein | 43.2 ± 1.8 | 41.6 ± 1.7 | −1.6 ± 0.3 | |
| Total bone mineral density§ (g/cm2) | Normal protein | 1.165 ± 0.028 | 1.161 ± 0.029 | −0.003 ± 0.003 |
| Higher protein | 1.183 ± 0.025 | 1.165 ± 0.024 | −0.017 ± 0.004 | |
| Total bone mineral content (g) | Normal protein | 2606 ± 93 | 2574 ± 96 | −32 ± 24 |
| Higher protein | 2523 ± 119 | 2517 ± 130 | −6 ± 18 | |
| Total bone area (cm2) | Normal protein | 2234 ± 49 | 2212 ± 49 | −22 ± 20 |
| Higher protein | 2123 ± 64 | 2144 ± 70 | 21 ± 20 |
Notes: *Mean ± SEM; normal protein, n = 15; higher protein, n = 13.
Significant difference between groups, p = .007.
Significant change over time (pre to post), p < .001.
Significant group-by-time interaction, p < .01. p Values of paired Student’s t test for change over time in the normal protein and higher protein groups are 0.216 and 0.003, respectively.
Study 1: Diet Composition, Protein Intake, and PRAL
Energy intake was lower during the intervention than baseline for both groups (p < .001; Supplementary Table 1). As designed, during energy restriction, the normal protein group consumed less protein, more carbohydrate, and the same fat compared with the higher protein group. The absolute amount of protein (g/day) consumed during the 12-week intervention was constant for the normal protein and higher protein groups, but the relative protein intakes (grams per kilogram per day) increased as body mass loss occurred. At intervention Week 1, protein intakes for the normal protein and higher protein groups were 0.81 ± 0.03 and 1.39 ± 0.04 g·kg−1·day−1, respectively. Postintervention, the protein intakes were 0.91 ± 0.04 and 1.55 ± 0.04 g·kg−1·day−1, respectively. The group-specific protein intakes were supported by differential blood urea nitrogen postintervention (normal protein 12.6 ± 0.9 and higher protein 16.5 ± 0.8 mg/dL; p < .05). The sources of dietary protein are presented in Supplementary Table 2. During energy restriction, total calcium intake (diet + supplement) was >2,000 mg/day for both groups.
At 1,200–1,700 kcal/day energy intakes, PRAL ranged from 6.4–13.7 and 29.1–42.2 mEq/day for the normal protein and higher protein groups, respectively.
Study 1: Bone Parameters
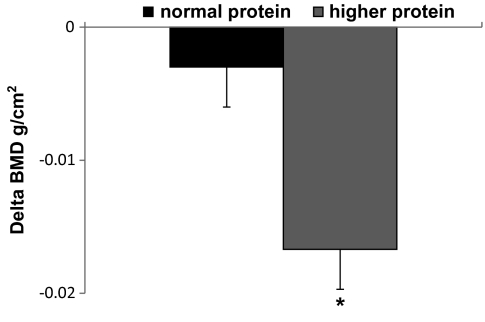
At baseline, total body BMD, bone mineral content, and bone area were not different between the normal protein and higher protein groups (Table 1). After weight loss, BMD was not changed in normal protein (–0.3% ± 0.2%) but decreased in higher protein (−1.4% ± 0.4%, p < .01; Figure 1, group-by-time p < .05). Bone mineral content and bone area were not changed after weight loss, independent of diet.
Figure 1.
Study 1: Changes in total body BMD. *p < .01. BMD: bone mineral density.
Study 2: Participant Characteristics and Body Composition
There were no differences in age, height, body mass, body mass index, or body composition among the four groups at baseline (Table 2). Compared with CONTROL, the CARB, CHICKEN, and BEEF groups lost body mass, fat mass, and fat-free mass and lowered body mass index.
Table 2.
Study 2: Participant Characteristics at Baseline and Post*
| Parameter | Group | Baseline | Post | Change |
| Age (y) | CONTROL | 54 ± 5 | ||
| CARB | 59 ± 2 | |||
| CHICKEN | 60 ± 2 | |||
| BEEF | 58 ± 2 | |||
| Height (cm) | CONTROL | 163 ± 2 | ||
| CARB | 164 ± 1 | |||
| CHICKEN | 162 ± 1 | |||
| BEEF | 164 ± 1 | |||
| Body mass† (kg) | CONTROL | 79.8 ± 3.4 | 79.1 ± 3.7 | −1.2 ± 0.4 |
| CARB | 75.9 ± 2.4 | 70.3 ± 2.4 | −5.6 ± 0.5‡ | |
| CHICKEN | 76.2 ± 2.8 | 67.3 ± 2.6 | −7.9 ± 0.7‡ | |
| BEEF | 81.0 ± 2.5 | 74.4 ± 2.6 | −6.6 ± 0.7‡ | |
| Body mass index† (kg/cm2) | CONTROL | 30.1 ± 1.1 | 29.8 ± 1.2 | −0.3 ± 0.2 |
| CARB | 28.4 ± 0.9 | 26.3 ± 0.9 | −2.1 ± 0.2‡ | |
| CHICKEN | 29.1 ± 1.1 | 26.1 ± 1.0 | −3.0 ± 0.3‡ | |
| BEEF | 30.1 ± 0.8 | 27.6 ± 0.9 | −2.5 ± 0.3‡ | |
| Fat mass† (kg) | CONTROL | 35.3 ± 2.9 | 35.9 ± 3.2 | 0.6 ± 1.1 |
| CARB | 33.5 ± 2.0 | 29.6 ± 2.0 | −3.9 ± 0.4‡ | |
| CHICKEN | 32.9 ± 1.9 | 27.3 ± 1.7 | −5.6 ± 0.6‡ | |
| BEEF | 35.4 ± 2.1 | 31.1 ± 2.2 | −4.3 ± 0.6‡ | |
| Fat-free mass† (kg) | CONTROL | 44.5 ± 1.0 | 44.5 ± 0.9 | 0.0 ± 0.3 |
| CARB | 42.4 ± 0.8 | 40.7 ± 0.7 | −1.7 ± 0.3‡ | |
| CHICKEN | 43.3 ± 1.2 | 41.0 ± 1.1 | −2.3 ± 0.3‡ | |
| BEEF | 45.5 ± 0.9 | 43.3 ± 0.8 | −2.2 ± 0.3‡ | |
| Total bone mineral density† (g/cm2) | CONTROL | 1.166 ± 0.028 | 1.166 ± 0.028 | −0.0000 ± 0.004 |
| CARB | 1.111 ± 0.026 | 1.107 ± 0.026 | −0.0038 ± 0.003 | |
| CHICKEN | 1.143 ± 0.024 | 1.131 ± 0.024 | −0.0123 ± 0.003‡ | |
| BEEF | 1.140 ± 0.026 | 1.126 ± 0.025 | −0.0145 ± 0.003‡ | |
| Total bone mineral content (g) | CONTROL | 2542 ± 88 | 2548 ± 95 | 7 ± 21 |
| CARB | 2377 ± 81 | 2354 ± 88 | −23 ± 20 | |
| CHICKEN | 2242 ± 76 | 2445 ± 81 | 3 ± 18 | |
| BEEF | 2463 ± 78 | 2480 ± 84 | 18 ± 19 | |
| Total bone area (cm2) | CONTROL | 2170 ± 48 | 2176 ± 53 | 6 ± 21 |
| CARB | 2140 ± 44 | 2127 ± 49 | −12 ± 20 | |
| CHICKEN | 2130 ± 41 | 2152 ± 45 | 23 ± 18 | |
| BEEF | 2165 ± 43 | 2205 ± 47 | 40 ± 19 |
Notes: *Mean ± SEM; BEEF = moderate protein beef group (n = 14), CHICKEN = moderate protein chicken group (n = 15), CARB = lower protein, lacto-ovo vegetarian group (n = 14), and CONTROL = nonintervention control group (n = 11).
Significant group-by-time interaction p < .05.
Significant difference compared with control p < .05.
Study 2: Diet Composition, Protein Intake, and PRAL
At baseline, energy, protein, carbohydrate, fat, and calcium intakes were not different among the four groups (Supplementary Table 3). During the intervention, energy intake was lower in the three energy-restricted groups compared with CONTROL. Protein intake was lower in the CARB (0.73 ± 0.12 g protein·kg−1·day−1) but not different in the CHICKEN (0.99 ± 0.08 g protein·kg−1·day−1) and BEEF (0.90 ± 0.09 g protein·kg−1·day−1) compared with CONTROL (0.89 ± 0.11 g protein·kg−1·day−1). These protein intake results were supported by 24-hour urinary total nitrogen excretion, which was lower for CARB, but not CHICKEN and BEEF compared with CONTROL: 4.8 ± 0.3, 8.3 ± 0.3, 8.6 ± 0.9, and 7.8 ± 0.7 g nitrogen·kg−1·day−1, respectively (14). The sources of dietary protein among the three energy-restricted groups are provided in Supplementary Table 2. Average dietary calcium intake among all participants was 732 ± 46 mg/day.
PRAL for BEEF and CHICKEN diets were 5.4 and 6.9 mEq/day, respectively. PRAL for CARB diet was −5.5 mEq/day.
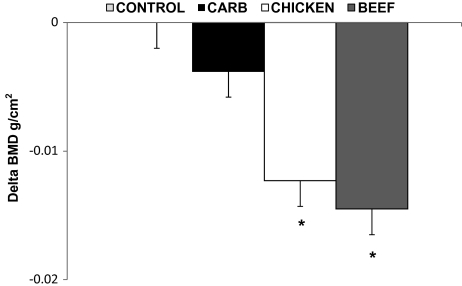
Study 2: Bone Parameters
At baseline, BMD, bone mineral content, and bone area were not different among the four groups (Table 2). After intervention, BMD decreased in CHICKEN (−1.1 ± 0.3%) and BEEF (−1.4 ± 0.2%) from baseline and was not changed in CARB (−0.4 ± 0.3%) and CONTROL (0.0 ± 0.3%; Figure 2, group-by-time p < .05). The BMD changes in the BEEF and CHICKEN groups were different from CONTROL. Bone mineral content and bone area were not changed over time or differentially influenced by diet.
Figure 2.
Study 2: Changes in total body BMD. *p < .05: Change of bone mineral density in CHICKEN and BEEF were different from CONTROL. CONTROL: nonintervention control group, CARB: lower protein lacto-ovo vegetarian group, CHICKEN: higher protein chicken group, BEEF: higher protein beef group, and BMD: bone mineral density.
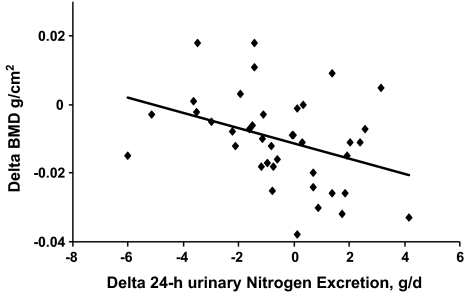
Among the energy-restricted participants, the change in BMD was related to the change in 24-hour urinary total nitrogen excretion (R2 = 0.137, p < .05; Figure 3) but not related to the change in body mass.
Figure 3.
Study 2: Correlation between the change in whole body bone mineral density and the change in 24-hour urinary nitrogen excretion. BMD: bone mineral density.
Study 2: Markers of Calcium Metabolism and Bone Homeostasis
The blood and urinary markers of calcium metabolism and bone turnover were not different among groups at baseline except serum parathyroid hormone or changed over time (Supplementary Table 4).
DISCUSSION
These results indicate that dietary protein is an important factor influencing BMD changes in conjunction with weight loss in postmenopausal women and that energy-restricted diets with higher amounts of dietary protein, mainly from animal flesh sources, promoted greater BMD loss than lower protein diets void of animal flesh foods. Past research showed that a higher protein diet either did not influence BMD (11,12) or helped preserve BMD (13) after weight loss. In one study (11), no significant BMD loss occurred in participants consuming either a higher protein (25% of energy from protein) or a normal protein diet for 6 month. Another 12-week study (12) with participants consuming a higher protein (34% of energy from protein), energy-restricted diet from different sources showed no change in BMD from baseline or interactions with diet. A recent study (12) found that whole body BMD was higher by 1.6% in the higher protein (30% of energy from protein) group compared with a normal protein diet, after 4-month of weight loss followed by 8-month of weight maintenance. These investigators (11–13) indicated that dairy was the predominant source of protein, although the sources of protein were not quantified. In the current research, participants in Study 1 and Study 2 assigned to the higher protein diets consumed 36% and 24% of protein from dairy, respectively, but BMD loss still occurred. Neither study was intended to compare protein from meat versus dairy. We are not able to distinguish between the effect of protein source and protein quantity on BMD loss in the current studies.
The combination of higher protein and calcium intakes might promote bone mineral accrual in older people (16). With regard to weight loss, participants who consumed a high dairy high calcium (2,400 mg Ca/day) diet apparently had slower bone turnover (assessed using blood markers of bone formation and resorption) than those who consumed a comparable high protein diet from mixed protein sources (500 mg Ca/day) (12). In Study 1, all the participants consumed calcium supplements. Despite calcium intakes >2,000 mg/day, the higher protein group lost BMD after weight loss, whereas the normal protein group did not. In Study 2, although about one half of the participants consumed calcium supplements, this use did not influence the BMD responses to weight loss. Collectively, higher calcium intakes from supplements do not appear to prevent or influence the loss of BMD when overweight and obese postmenopausal women lose weight while consuming a higher protein omnivorous diet.
A common explanation for bone loss with a higher protein diet is elevated endogenous acid production (9). Increased bone resorption may occur to help balance endogenous acidity, which may result in a negative calcium balance and higher risk of osteoporosis (10). In the current research, the higher protein intakes of the omnivorous groups translated into higher dietary PRALs, which could theoretically promote reduced BMD. This interpretation should be drawn with caution. Although the BMD losses of the higher protein groups were comparable (Study 1, higher protein −1.4%; Study 2, CHICKEN −1.1%, BEEF −1.4%), the PRALs were fivefold higher in Study 1 than in Study 2. Although speculative, these observations support the notion that humans with normal kidney function possess the metabolic capacity to buffer diet-related acidity without the mobilization of bone (17), and PRAL is not a significant factor with regard to BMD changes with weight loss.
Dietary protein-induced increases in IGF-1 may stimulate bone formation. Serum IGF-1 was higher in participants who consumed higher protein provided from milk (18,19), and IGF-1 concentration was positively associated with dairy protein (20). The specificity of dairy-based proteins to increase IGF-1 is not firmly established because other researchers found no association between dairy protein intake and IGF-1 (21). Meat protein intake has (21) and has not (20) been positively associated with IGF-1. In Study 2, serum IGF-1 was not changed over time in all four groups, which suggests that IGF-1 may not have influenced the differential BMD responses to weight loss among the different energy-restricted diets.
The novel observation that the change in BMD was negatively correlated with the change in 24-hour urinary total nitrogen excretion suggests that older women who increase their total protein intake during the period of energy restriction may be at higher risk for BMD loss, whereas a reduction in total protein intake may help preserve BMD. Future studies should document how much protein a person regularly consumes before starting a weight loss program and whether women who usually consume a higher protein diet do not experience greater BMD loss with energy restriction.
Results from research when both bone turnover markers and BMD were measured are inconsistent. In one study (22), bone turnover was increased, but BMD was unchanged. In another study (23), C-telopeptide of Type I collagen (bone resorption marker) was increased when weight loss was achieved using either energy restriction or exercise, but hip BMD was decreased in the energy-restricted group only. In Study 2, the post-weight loss reductions in BMD observed in the BEEF and CHICKEN groups occurred without any apparent changes in bone turnover markers. In terms of assessing the risk of osteoporosis, BMD data obtained from dual-energy X-ray absorptiometry scans are more relevant than bone turnover markers because the technique has less variation (24), is non-invasive and is a direct measure of changes in bone. The combination of increased bone turnover markers with decreased BMD indicates higher risk of osteoporosis than any of them alone (24).
Strengths of the current studies include using randomized repeated measures experimental designs, using blood urea nitrogen or 24-hour urinary total nitrogen excretion as independent markers to confirm differential protein intakes and using a control group in Study 2. One limitation is the short-term length of the interventions and the possibility that the BMD changes reflect transient bone remodeling (25). Future longer term interventions are needed to fully understand the impacts of dietary protein on bone in conjunction with weight loss. Another limitation is the possibility that BMD changes after weight loss are not physiological but may be an artifact because the dual-energy x-ray absorptiometer lacks sensitivity when body weight and composition are changed (26). However, within the two current studies, the lower and higher protein groups lost comparable amounts of body mass and fat mass, yet only the higher protein groups reduced BMD significantly. Thus, the differential BMD responses attributable to dietary protein were measurable despite possible instrument insensitivity. A dual-energy x-ray absorptiometer uses bone mineral content and bone area to calculate BMD. A potential confounder of dual-energy x-ray absorptiometry measurement is body water, which may alter with higher protein diets (27). Change in body water may affect the precision of bone mineral content measurement and as a result affect BMD.
In summary, a higher protein energy-restricted diet with protein predominantly from animal flesh sources promoted total body BMD loss in overweight and obese postmenopausal women during weight loss compared with a lower protein energy-restricted diet void of animal flesh foods. Our results suggested that for postmenopausal women, choosing a higher protein omnivorous diet for effective weight loss, may decrease BMD and increase the risk of osteoporosis.
FUNDING
Study 1 was supported by the National Pork Board. Study 2 was supported by the Cattlemen’s Beef Board and the National Cattlemen’s Beef Associationand National Institutes of Health (grant number M01 RR00750).
SUPPLEMENTARY MATERIAL
Supplementary material can be found at: http://biomed.gerontologyjournals.org/
Supplementary Material
Acknowledgments
The abstract of Study 1 was presented at the Experimental Biology Conference 2009. The abstract of Study 2 was presented at the Obesity Society’s Annual Scientific Meeting 2006.
References
- 1.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894 i–xii: 1–253. [PubMed] [Google Scholar]
- 2.Ricci TA, Heymsfield SB, Pierson RN, Jr., Stahl T, Chowdhury HA, Shapses SA. Moderate energy restriction increases bone resorption in obese postmenopausal women. Am J Clin Nutr. 2001;73:347–352. doi: 10.1093/ajcn/73.2.347. [DOI] [PubMed] [Google Scholar]
- 3.Leidy HJ, Carnell NS, Mattes RD, Campbell WW. Higher protein intake preserves lean mass and satiety with weight loss in pre-obese and obese women. Obesity (Silver Spring) 2007;15:421–429. doi: 10.1038/oby.2007.531. [DOI] [PubMed] [Google Scholar]
- 4.Farnsworth E, Luscombe ND, Noakes M, Wittert G, Argyiou E, Clifton PM. Effect of a high-protein, energy-restricted diet on body composition, glycemic control, and lipid concentrations in overweight and obese hyperinsulinemic men and women. Am J Clin Nutr. 2003;78:31–39. doi: 10.1093/ajcn/78.1.31. [DOI] [PubMed] [Google Scholar]
- 5.Kerstetter JE, O’Brien KO, Insogna KL. Low protein intake: the impact on calcium and bone homeostasis in humans. J Nutr. 2003;133:855S–861S. doi: 10.1093/jn/133.3.855S. [DOI] [PubMed] [Google Scholar]
- 6.Barzel US, Massey LK. Excess dietary protein can adversely affect bone. J Nutr. 1998;128:1051–1053. doi: 10.1093/jn/128.6.1051. [DOI] [PubMed] [Google Scholar]
- 7.Hannan MT, Tucker KL, Dawson-Hughes B, Cupples LA, Felson DT, Kiel DP. Effect of dietary protein on bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res. 2000;15:2504–2512. doi: 10.1359/jbmr.2000.15.12.2504. [DOI] [PubMed] [Google Scholar]
- 8.Feskanich D, Willett WC, Stampfer MJ, Colditz GA. Protein consumption and bone fractures in women. Am J Epidemiol. 1996;143:472–479. doi: 10.1093/oxfordjournals.aje.a008767. [DOI] [PubMed] [Google Scholar]
- 9.Sellmeyer DE, Stone KL, Sebastian A, Cummings SR. A high ratio of dietary animal to vegetable protein increases the rate of bone loss and the risk of fracture in postmenopausal women. Study of Osteoporotic Fractures Research Group. Am J Clin Nutr. 2001;73:118–122. doi: 10.1093/ajcn/73.1.118. [DOI] [PubMed] [Google Scholar]
- 10.Thorpe M, Mojtahedi MC, Chapman-Novakofski K, McAuley E, Evans EM. A positive association of lumbar spine bone mineral density with dietary protein is suppressed by a negative association with protein sulfur. J Nutr. 2008;138:80–85. doi: 10.1093/jn/138.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skov AR, Haulrik N, Toubro S, Molgaard C, Astrup A. Effect of protein intake on bone mineralization during weight loss: a 6-month trial. Obes Res. 2002;10:432–438. doi: 10.1038/oby.2002.60. [DOI] [PubMed] [Google Scholar]
- 12.Bowen J, Noakes M, Clifton PM. A high dairy protein, high-calcium diet minimizes bone turnover in overweight adults during weight loss. J Nutr. 2004;134:568–573. doi: 10.1093/jn/134.3.568. [DOI] [PubMed] [Google Scholar]
- 13.Thorpe MP, Jacobson EH, Layman DK, He X, Kris-Etherton PM, Evans EM. A diet high in protein, dairy, and calcium attenuates bone loss over twelve months of weight loss and maintenance relative to a conventional high-carbohydrate diet in adults. J Nutr. 2008;138:1096–1100. doi: 10.1093/jn/138.6.1096. [DOI] [PubMed] [Google Scholar]
- 14.Mahon AK, Flynn MG, Stewart LK, et al. Protein intake during energy restriction: effects on body composition and markers of metabolic and cardiovascular health in postmenopausal women. J Am Coll Nutr. 2007;26:182–189. doi: 10.1080/07315724.2007.10719600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Remer T, Manz F. Potential renal acid load of foods and its influence on urine pH. J Am Diet Assoc. 1995;95:791–797. doi: 10.1016/S0002-8223(95)00219-7. [DOI] [PubMed] [Google Scholar]
- 16.Dawson-Hughes B. Interaction of dietary calcium and protein in bone health in humans. J Nutr. 2003;133:852S–854S. doi: 10.1093/jn/133.3.852S. [DOI] [PubMed] [Google Scholar]
- 17.Bonjour JP. Dietary protein: an essential nutrient for bone health. J Am Coll Nutr. 2005;24:526S–536S. doi: 10.1080/07315724.2005.10719501. [DOI] [PubMed] [Google Scholar]
- 18.Cadogan J, Eastell R, Jones N, Barker ME. Milk intake and bone mineral acquisition in adolescent girls: randomised, controlled intervention trial. BMJ. 1997;315:1255–1260. doi: 10.1136/bmj.315.7118.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heaney RP, McCarron DA, Dawson-Hughes B, et al. Dietary changes favorably affect bone remodeling in older adults. J Am Diet Assoc. 1999;99:1228–1233. doi: 10.1016/S0002-8223(99)00302-8. [DOI] [PubMed] [Google Scholar]
- 20.Budek AZ, Hoppe C, Michaelsen KF, Bugel S, Molgaard C. Associations of total, dairy, and meat protein with markers for bone turnover in healthy, prepubertal boys. J Nutr. 2007;137:930–934. doi: 10.1093/jn/137.4.930. [DOI] [PubMed] [Google Scholar]
- 21.Larsson SC, Wolk K, Brismar K, Wolk A. Association of diet with serum insulin-like growth factor I in middle-aged and elderly men. Am J Clin Nutr. 2005;81:1163–1167. doi: 10.1093/ajcn/81.5.1163. [DOI] [PubMed] [Google Scholar]
- 22.Bowen JB, Noakes M, Clifton PM. A high dairy protein, high calcium diet minimizes bone turnover in overweight adults during weight loss. J Nutr. 2004;134:568–573. doi: 10.1093/jn/134.3.568. [DOI] [PubMed] [Google Scholar]
- 23.Villareal DT, Fontana L, Weiss EP, et al. Bone mineral density response to caloric restriction-induced weight loss or exercise-induced weight loss: a randomized controlled trial. Arch Intern Med. 2006;166:2502–2510. doi: 10.1001/archinte.166.22.2502. [DOI] [PubMed] [Google Scholar]
- 24.Seibel MJ, Lang M, Geilenkeuser WJ. Interlaboratory variation of biochemical markers of bone turnover. Clin Chem. 2001;47:1443–1450. [PubMed] [Google Scholar]
- 25.Heaney RP. The bone remodeling transient: interpreting interventions involving bone-related nutrients. Nutr Rev. 2001;59:327–334. doi: 10.1111/j.1753-4887.2001.tb06957.x. [DOI] [PubMed] [Google Scholar]
- 26.Van Loan MD, Johnson HL, Barbieri TF. Effect of weight loss on bone mineral content and bone mineral density in obese women. Am J Clin Nutr. 1998;67:734–738. doi: 10.1093/ajcn/67.4.734. [DOI] [PubMed] [Google Scholar]
- 27.Baba NH, Sawaya S, Torbay N, Habbal Z, Azar S, Hashim SA. High protein vs high carbohydrate hypoenergetic diet for the treatment of obese hyperinsulinemic subjects. Int J Obes Relat Metab Disord. 1999;23:1202–1206. doi: 10.1038/sj.ijo.0801064. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.