Abstract
Background
Long-term immune recovery in older patients given hematopoietic cell transplantation after non-myeloablative conditioning remains poorly understood. This prompted us to investigate long-term lymphocyte reconstitution and thymic function in 80 patients given allogeneic peripheral blood stem cells after non-myeloablative conditioning.
Design and Methods
Median age at transplant was 57 years (range 10–71). Conditioning regimen consisted of 2 Gy total body irradiation (TBI) with (n=46) or without (n=20) added fludarabine, 4 Gy TBI with fludarabine (n=6), or cyclophosphamide plus fludarabine (n=8). Stem cell sources were unmanipulated (n=56), CD8-depleted (n=19), or CD34-selected (n=5) peripheral blood stem cells. Immune recovery was assessed by signal-joint T-cell receptor excision circle quantification and flow cytometry.
Results
Signal-joint T-cell receptor excision circle levels increased from day 100 to one and two years after transplantation in patients under 50 years of age (n=23; P=0.02 and P=0.04, respectively), and in those aged 51–60 years (n=35; P=0.17 and P=0.06, respectively), but not in patients aged over 60 (n=22; P=0.3 and P=0.3, respectively). Similarly, CD4+CD45RA+ (naïve) T-cell counts increased from day 100 to one and two years after transplantation in patients aged 50 years and under 50 (P=0.002 and P=0.02, respectively), and in those aged 51–60 (P=0.4 and P=0.001, respectively), but less so in patients aged over 60 (P=0.3 and P=0.06, respectively). In multivariate analyses, older patient age (P<0.001), extensive chronic GVHD (P<0.001), and prior (resolved) extensive chronic graft-versus-host disease (P=0.008) were associated with low signal-joint T-cell receptor excision circle levels one year or more after HCT.
Conclusions
In summary, our data suggest that thymic neo-generation of T cells occurred from day 100 onwards in patients under 60 while signal-joint T-cell receptor excision circle levels remained low for patients aged over 60. Further, chronic graft-versus-host disease had a dramatic impact on thymic function, as observed previously in patients given grafts after myeloablative conditioning.
Keywords: thymus, hematopoietic cell transplantation, non-myeloablative, graft-versus-host disease, immunity, age
Introduction
It is well established that the thymus undergoes a physiological involution with aging that affects its structure and cytokine environment.1,2 However, studies by Steinman et al. in the 1980s documented lymphocytic thymic tissue in adults up to 107 years of age.1 Further, several studies have suggested that the human thymus could continue to mature new T cells throughout life, exporting signal-joint T-cell receptor excision circle (sjTREC) bearing T cells into the peripheral blood even in elderly patients.3–5
Non-myeloablative conditioning regimens followed by allogeneic hematopoietic cell transplantation (HCT) have opened the way to performing allogeneic HCT in patients with hematologic malignancies aged up to 70–75 years.6–9 This approach has relied on optimization of pre- and post-transplant immunosuppression to overcome graft-versus-host disease (GVHD) reactions,10 thereby allowing engraftment and eradication of tumors nearly exclusively via immune-mediated graft-versus-tumor effects.11–13
T-cell recovery after allogeneic HCT following high-dose (myeloablative) conditioning depends on both peripheral expansion of mature T cells contained in the graft (thymo-independent pathway), and T-cell neo-production from donor hematopoietic stem cells (thymo-dependent pathway).14–17 In young patients given myeloablative allogeneic HCT, most circulating T cells during the first 3–6 months following HCT are the progeny of T cells infused with the grafts,18 while neogeneration of T cells by the thymus plays an important role in reconstituting the T-cell pool beyond day 100 after HCT.19–24
We recently analyzed immune recovery after non-myeloablative conditioning the first year after non-myeloablative conditioning.25,26 Main observations were that unrelated donor status and donor age affected early immune recovery,25 while sjTREC levels significantly increased from day 100 to day 365 in a cohort of 16 patients,26 suggesting that the thymic pathway might play a role in immune recovery in these older patients given non-myeloablative conditioning. Here, we analyzed long-term (one year or more) immune recovery and thymic function in 80 patients given non-myeloablative conditioning regimen.
Design and Methods
Patients and donors
Data from 80 patients transplanted between March 2000 and April 2008 at the University of Liège were included in the study. Results were analyzed as of July 29, 2009. Patients’ characteristics are summarized in the Online Supplementary Table S1. Median patient age was 57 (range 10–71) years. Thirty-three of the 80 patients received grafts from HLA-matched related donors, 22 from HLA-matched unrelated donors, and 25 from HLA-mismatched related or unrelated donors. Stem cell sources were unmanipulated (n=56), CD8-depleted (n=19), or CD34-selected (n=5) peripheral blood stem cells (PBSC). CD8-depletion and CD34-selection of PBSC were carried out as previously reported.26,27 Nine patients given grafts from HLA-mismatched donors were enrolled in a trial of mesenchymal stem cell co-transplantation as a potential way to prevent severe GVHD28. Immune recovery in 35 of the 80 patients for the first six (n=14)27 or 12 (n=21)26 months after HCT has been reported previously. Written informed consent was obtained from each patient to undergo non-myeloablative HCT and to collect, store and analyze blood samples for research purposes. The Ethics Committee of the University of Liège approved the consent form as well as the current research study protocol.
Treatment and evaluation
The non-myeloablative conditioning regimens consisted of 2 Gy total body irradiation (TBI) alone (n=20; patients with low risk of graft rejection given PBSC from HLA-identical siblings), 2 Gy TBI with 90 mg/m2 fludarabine (n=46; standard regimen), 4 Gy TBI with 90 mg/m2 fludarabine (n=6; patients at high risk of early disease progression and/or graft rejection), or fludarabine 90 mg/m2 with cyclophosphamide 3 g/m2 (n=8, patients with previous irradiation precluding the use of TBI). Post-grafting immuno-suppression combined mycophenolate mofetil (MMF) with a calcineurin inhibitor for all patients, as previously described.26,27
Clinical management
Twenty-four patients received at least one unmanipulated (n=18) or CD8-depleted (n=6) pre-emptive donor lymphocyte infusion (DLI) the first year after HCT (including the 5 patients given CD34-selected PBSC who received CD8-depleted preemptive DLI). G-CSF (5 μg/kg/d) was administered when the granulocyte count declined below 1.0×109/L. The diagnosis, clinical grading, and treatment of acute GVHD were performed according to established criteria.29 Treatment was usually given for grade II–IV acute GVHD and for extensive chronic GVHD. Initial treatment of acute GVHD usually consisted of prednisolone, 2 mg/kg/day, with tapering initiated within 14 days. In addition, the calcineurin inhibitor was usually resumed at full doses. Steroid-refractory acute GVHD was treated as per available investigational protocols or standard practice. Treatment of chronic GVHD consisted of methylprednisolone (1 mg/kg) with alternate-day calcineurin inhibitor. Steroid-refractory chronic GVHD was generally treated with rapamycin, mycophenolate mofetil, or photophoresis.
Infection prophylaxis generally consisted of acyclovir (400 mg t.i.d. orally), oral itraconazole solution (200 mg b.i.d.) or oral fluconazole (200 mg b.i.d.), and trimethoprim sulfamethoxazole or aerosolized pentamidine. Polymerase chain reaction (PCR) for cytomegalovirus (CMV) was performed weekly until day 100 and every 2–4 weeks thereafter. Patients with a positive PCR received preemptive i.v. ganciclovir.
Disease evaluations were routinely carried out on days 40, 100, 180 and 365 after HCT.
Chimerism
Chimerism levels among peripheral T cells were assessed on days 28, 40, 100, 180 and 365 after HCT using fluorescence in situ hybridization to detect X and Y chromosomes for recipients of sex-mismatched transplants and PCR-based analysis of polymorphic microsatellite regions (AmpFlSTR® Identifiler®, Applied Biosystems, Lennik, Belgium) for recipients of sex-matched transplants.26,27 CD3 (T cell) selection was carried out with the RosetteSepR human T-cell enrichment kit (StemCell Technologies, Vancouver, Canada). Graft rejection was defined as the occurrence of less than 5% T cells of donor origin after HCT, as previously described.30,31
Immune recovery
Immune recovery was prospectively assessed as previously described.27 Briefly, patients’ peripheral white blood cells were phenotyped on days 28, 42, 60, 80, 100, 120, 180, 365, 540, 730 and yearly thereafter using 4 color flow cytometry after treatment with a red blood cell lyzing solution. The analyzed cell subsets were T cells (CD3+), CD4+ T cells (CD3+CD4+ lymphocytes), CD8+ T cells (CD3+CD8+ lymphocytes), naïve CD4+ T cells (CD4+CD45RAhigh double positive lymphocytes), memory CD4+ T cells (CD4+CD45RO+ double positive lymphocytes), NK cells (CD3-CD56+ lymphocytes) as well as B cells (CD19+ lymphocytes). The percentage of positive cells was measured relative to total nucleated cells, after subtraction of non-specific staining. Absolute counts were obtained by multiplying the percentages of positive cells by the white blood cell counts (Advia 120 hematology analyzer, Bayer Technicon, Tarrytown, USA). Lower and higher limits of normal values for each cell subset were defined respectively as 5 and 95 percentiles of values obtained in 47 age-matched healthy volunteer donors.
More detailed T- and B-cell phenotyping was retrospectively performed using cryopreserved PBMC from 33 patients obtained two years after transplantation using 6 color flow cytometry. The different populations were defined as follows: naïve CD4+ T cells, CD4+CD45RA+CCR7+CD27+ lymphocytes; central memory CD4+ T cells, CD4+CD45RA−CCR7+CD27+ lymphocytes; effector memory CD4+ T cells, CD4+CD45RA-CCR7−CD27+ lymphocytes; late differentiation effector memory CD4+ T cells, CD4+CD45RA−CCR7−CD27− lymphocytes; naïve CD8+ T cells, CD8+CD45RA+CCR7+ lymphocytes; central memory CD8+ T cells, CD8+CD45RA−CCR7+ lymphocytes; effector memory CD8+ T cells, CD8+CD45RA−CCR7− lymphocytes; effector memory RA+ CD8+ T cells, CD8+CD45RA+CCR7− lymphocytes; naïve B cells, CD19+CD27− lymphocytes; memory B cells, CD19+CD27+ lymphocytes; IgM+IgD+ memory B cells, CD19+CD27+IgM+IgD+ lymphocytes; switched memory B cells, CD19+CD27+IgM−IgD− lymphocytes. Absolute counts were calculated by multiplying the percentage of positive cells in the lymphoid gate by the absolute lymphocyte count of the patient the day of PBMC collection.
CDR3 spectratyping (immunoscope)
T-cell receptor beta chain (TCRB) CDR3 spectratyping analyses were performed between two and nine (median three) years after HCT in 21 patients. RNA was extracted from 10×106 cells by Tripure (Roche) according to the manufacturer’s protocol. The quality of the extracted RNA was controlled using the Experion RNA StdSens Starter Kit (Bio-Rad, Nazareth Eke, Belgium) in a gel electrophoresis experiment (Experion Automated Electrophoresis System, Bio-Rad). RNA optical density measurements were performed on a Nanodrop ND1000 (Isogen, Sint-Pieters Leeuw, Belgium). First-strand cDNA was generated from 1 μg total RNA using Transcriptor 1st strand cDNA synthesis kit (Roche) according to the manufacturer’s protocol. Each TCRB segment was amplified with one of the 24 TCRBV family-specific primers (Vβ1–Vβ24) and a TCRBC primer conjugated to fluorescent dye 6-FAM (Applied Biosystems, Lennik, Belgium) for CDR3 analysis. The size distribution of each fluorescent PCR product was determined by electrophoresis on an ABI 3730 automatic capillary sequencer (Applied Biosystems, Foster City, CA, USA) and data were analyzed by Genemapper v4.0 (Perkin Elmer Cetus Instruments, Emeryville, CA, USA). The overall complexity within a T-cell receptor Vbeta subfamily was determined by counting the number of peaks (intervals of 3 nucleotides) per subfamily. The overall spectratyping complexity (T-cell receptor Vbeta score) was calculated as the sum of the numbers of peaks in the 24 subfamilies. The median T-cell receptor Vbeta score in 20 age-matched volunteer blood donors was 239 (range 179–251) peaks. Further, in order to measure the deviation from normality of a repertoire, we measured its quadratic distance to the average of 2 normalized repertoires that were each artificially created by mixing in comparable amounts the cDNAs of the PBMC of 6 age-matched volunteer blood donors, as previously reported.32
T-cell receptor excision circles (TREC) assay
Blood samples were collected on days 40, 100, 180, 365, 540 and then yearly after HCT. TREC assays were performed on samples collected on days 100, 365, 540 and then yearly after HCT as previously described. Briefly, peripheral blood mononuclear cells (PBMC) were isolated using Ficoll-Hypaque (Amersham Pharmacia Biotech, Uppsala, Sweden) gradient centrifugation and then cryopreserved. SjTREC were quantified for each sample by nested real time PCR, as previously described.26,33 Briefly, thawed PBMC were lysed 30 min at 56°C with Tween-20 (0.05%), NP-40 (0.05%) and Proteinase K (100 μg/mL). Cell lysis was stopped by incubating 15 min at 99°C. Multiplex PCR amplification was achieved for sjTREC together with the CD3gamma/chain, used as a housekeeping gene, with specific 3’/5’ outer primers for each amplicon. Cycle conditions and primer/probe sequences have been reported elsewhere.33–35 PCR products were 10-fold diluted prior to PCR quantification using the Lightcycler™ technology. Quantitative PCR conditions were: 5 min initial denaturation at 95°C followed by 40 cycles of amplification (5 second at 95°C, 15 seconds at 60°C, 10 seconds at 72°C). Fluorescence emissions were assessed after the hybridization steps. Each PCR product was run for both sjTREC and CD3/gamma chain in 2 separate Lightcycler experiments. Every sample was run in at least 2 independent experiments. The results were first calculated as absolute numbers of sjTREC per 105 PBMC; because each PBMC contains 2 CD3/gamma chain copies, sjTREC/105 PBMC=(sjTREC/CD3gamma) x 2 105. Because sjTREC are only present in lymphocytes, and because PBMC composition can be variable, sjTREC concentration in peripheral blood was computed using the formula: (sjTREC/105 PBMC x PBMC/μL) /100 where PBMC/μL=(white blood cells /μL x (%lympho + %mono))/100. Similar adjustments for calculating absolute T-cell subset counts from their frequencies in PBMC have been made previously by other groups of investigators.36 The nested character of this quantitative PCR allows high sensitivity (detection of one copy of sjTREC per PCR reaction). SjTRECs were also measured in 47 age-matched healthy volunteers.
Statistical analyses
Wilcoxon’s matched pair test was used to compare sjTRECs concentrations and CD4+CD45RA+ T cells at day 100 after HCT with values obtained in the same patients on days 365 and 730 after HCT. Spearman’s correlation coefficient was used to analyze potential associations between lymphocyte subset counts and sjTRECs levels after HCT. The Mann-Whitney test was used to compare lymphocyte subset counts after HCT in patients under 57 years of age or 57 years and over at HCT. To determine factors affecting the counts of CD3+ T cells, CD4+ T cells, CD4+CD45RA+ (naïve) T cells, CD8+ T cells, B cells, and sjTREC levels at one year or more after HCT, multivariable linear regression models for the different MNC counts one year or more year after HCT were fitted using stepwise selection. Potential factors examined were: patient age, donor age, donor type (related vs. unrelated), HLA-compatibility (10/10 HLA-matched vs. other), number of CD3+ T cells transplanted, day post-HCT, extensive chronic GVHD at the time of analysis, limited chronic GVHD at the time of analysis, and prior (resolved, defined as discontinuation of systemic immunosuppressive therapy) extensive chronic GVHD. Logarithmic transformation of the responses was used for all models. Patients were censored at the time of graft rejection and/or disease progression. The comparison of the probability of chronic GVHD in patients with day 100 sjTREC levels above or below the median was made with the log rank test. The probability of infection from one to two years after HCT according to one year sjTREC levels was calculated using the cumulative incidence method, using death, and graft rejection and progression as competitive risks. Cox’s regression models were applied to fit risk of dying from infection. Results were significant at the 5% critical level (P<0.05). Statistical analyses were carried out with Graphpad Prism (Graphpad Software, San Diego, CA, USA) and SAS version 9.1 for Windows (SAS Institute, Cary, NC, USA).
Results
Reconstitution of thymic function (sjTRECs)
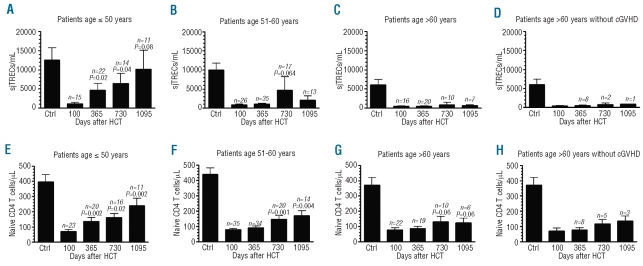
Confirming previous observations by our group in a cohort of 16 patients,26 thymic function assessed by sjTREC/mL of blood increased from day 100 to one and two years after transplantation. Specifically, sjTREC concentrations were 786±1,207 sjTREC/mL on day 100, 1,890±4,784 sjTREC/mL one year after HCT (P=0.0066 in comparison to day 100), and 4,333±1,1131 sjTREC/mL two years after HCT (P=0.0015 in comparison to day 100 and P=0.0422 in comparison to one year after HCT), respectively. However, as shown in Figure 1A–D, thymic recovery did not occur in patients over 60 years of age. Specifically, sjTREC concentrations increased from day 100 to one and two years after transplantation in patients aged 50 years and under (P=0.0245 and P=0.0371, respectively), and in those 51–60 years of age (P=0.17 and P=0.064, respectively), but not in patients over 60 years old (P=0.3 and P=0.3, respectively), even censored at onset of chronic GVHD. Similar results were observed when taking into consideration only patients for whom we had data on each day 100, one year, two years and three years after transplantation (Online Supplementary Figure 1A).
Figure 1.
Impact of patient age (at HCT) on sjTREC (A–D) and naïve CD4 T cell (E–H) recovery. (D and H) Patients were censured at time of occurrence of chronic GVHD. P values are given for comparison with day 100 values.
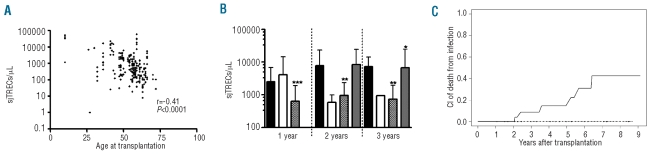
An inverse correlation was observed between sjTREC concentrations one year or more after HCT and recipient (R=−0.41, P<0.0001) and donor (R=−0.25, P=0.0002) ages (Figure 2A). In addition, chronic GVHD had a profound negative impact on sjTREC concentrations one year or more year after HCT. Specifically, sjTREC concentrations were 5,018±9,331 sjTREC/mL in patients without chronic GVHD, 2,493±7,383 sjTREC/mL (P=0.0078) in patients with limited chronic GVHD, 1,209±5,029 sjTREC/mL (P<0.0001) in patients with extensive chronic GVHD, and 4,166±12,436 sjTREC/mL (P=0.0021) in patients with resolved extensive chronic GVHD, respectively. The same results were observed when the impact of chronic GVHD presence / severity was assessed separately one year, two years and three years after transplantation (Figure 2B). As shown in the Online Supplementary Figure 1C-E, sjTREC concentrations one year after transplantation were not statistically affected by PBSC manipulation, donor lymphocyte infusion, or by the type of the non-myeloablative conditioning regimen administered. Further, mean±SD sjTREC concentration one year after HCT were 2,396±5,963 sjTREC/mL in patients given unmanipulated PBSC and no MSC, versus 1,303±2,860 sjTREC/mL (P=0.5) in those given unmanipulated PBSC and MSC.
Figure 2.
(A) Correlation between patient age at HCT and sjTREC levels one year or more after HCT. (B) Impact of chronic GVHD on sjTREC concentration (mean ± standard deviation) 1–3 years after HCT. Black bars, no chronic GVHD; white bars; limited chronic GVHD, black and white bars, extensive chronic GVHD; gray bars, resolved extensive chronic GVHD. P values (obtained with the Mann-Whitney test) are given in comparison to patients without chronic GVHD. (C) Cumulative incidence of dying from infection in patients with sjTREC levels on day 365 below (continuous line) or above (broken line) the median.
We then performed a multivariate analysis of factors affecting long-term thymic function, taking together sjTREC data from each patient at any time point one year or more after HCT (Table 1). In multivariate analysis, high patient age (P<0.0001), extensive chronic GVHD (P<0.0001), and resolved extensive chronic GVHD (P=0.0075) were independently associated with low sjTREC concentrations (Table 1).
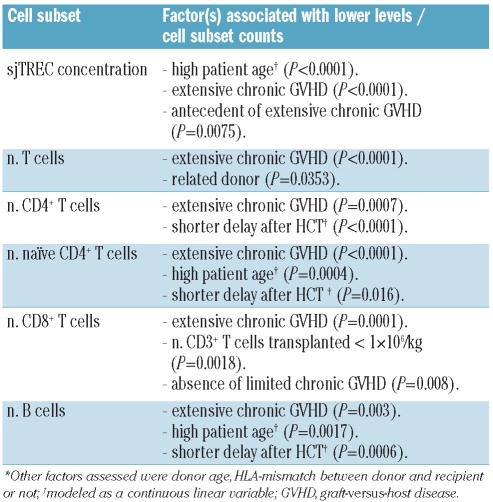
Table 1.
Multivariable analyses of factors affecting immune recovery one year or more after non-myeloablative conditioning (n=242)*.
Reconstitution of peripheral lymphocyte subsets
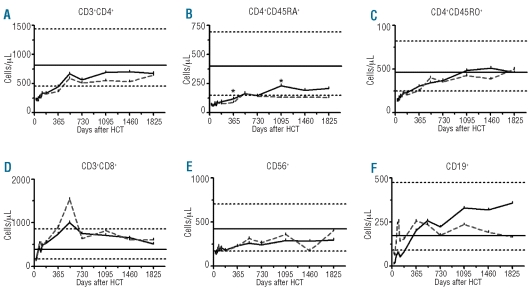
T cells
CD4+ T-cell counts remained below normal values during the first 540 days after HCT, then reached the 5th percentile of normal values on day 540 after HCT. This was mainly due to recovery of memory CD4+ T cells that reached the 5th percentile of normal values on day 365 after HCT, while CD4+CD45RA+ (naïve) T cells remained below normal values for the first three years after HCT (Figure 3). Recovery of lymphocyte subset counts were similar in patients under 57 years of age or 57 years and over, except for CD4+CD45RA+ (naïve) T-cell recovery that was lower in older than in younger recipients. Specifically, CD4+CD45RA+ T-cell counts increased from day 100 to one and two years after transplantation in patients aged 50 years and under (P=0.002 and P=0.02, respectively), and in those 51–60 years of age (P=0.4 and P=0.001, respectively), but less so in patients over 60 years old (P=0.3 and P=0.06, respectively), even when censored at onset of chronic GVHD (Figure 1E–H). Similar results were observed when taking into consideration only patients for whom we had data on each day 100, one year, two years and three years after transplantation (Online Supplementary Figure 1B).
Figure 3.
Mean MNC-subset cell counts after nonmyeloablative conditioning in patients under 57 years of age or 57 years and over at HCT. Horizontal lines show the 5th and 95th percentiles in 47 age-matched healthy volunteer donors. *, P<0.05.
As reported by other investigators,37 we observed a close correlation between sjTREC concentrations and CD4+CD45RA+ T-cell counts (R=0.47, P<0.0001) one year or more after HCT. In contrast to that observed in the CD4+ T-cell compartment, CD8+ T cells normalized quickly, reaching the 5th percentile of normal values as soon as two months after HCT. This indicates that peripheral expansion of mature T cells contained in the graft was more efficient for CD8+ T cells than for CD4+ T cells, as previously reported by other groups of investigators.15 As shown in the Online Supplementary Figure 1C–E, CD3+ T cell and CD4+CD45RA+ T-cell counts one year after transplantation were not statistically affected by PBSC manipulation, donor lymphocyte infusion, or by the type of the non-myeloablative conditioning regimen administered. Furthermore, mean ± SD CD3+ T-cell counts one year after HCT were 1,350±1,409 cells/μL in patients given unmanipulated PBSC and no MSC versus 1,867±1,544 cells/μL (P=0.3) in those given unmanipulated PBSC and MSC.
B and NK cells
CD19+ B-cell counts reached normal values at one year after HCT, while the counts of NK cells reached normal values around six months after HCT.
Multivariate analysis
We then performed a multivariate analysis of factors affecting long term T- and B-cell immune recovery, taking together data from each patient at any time point one year or more after HCT (Table 1). Extensive chronic GVHD was associated with lower counts of T cells (P<0.001), CD8+ T cells (P<0.001), CD4+ T cells (P<0.001), CD4+CD45RA+ T cells (P<0.001), and B cells (P=0.003); higher patient age was associated with lower counts of CD4+CD45RA+ T cells (P<0.001) and B cells (P=0.002) while longer delay after transplantation was associated with higher counts of CD4+ T cells (P<0.001), CD4+CD45RA+ T cells (P=0.016), and B cells (P<0.001). Further, patients given grafts containing less than 1×106 T cells/kg had lower CD8+ T-cell (P=0.002) counts.
Correlation between thymic function and T- and B-cell phenotypes two years after HCT
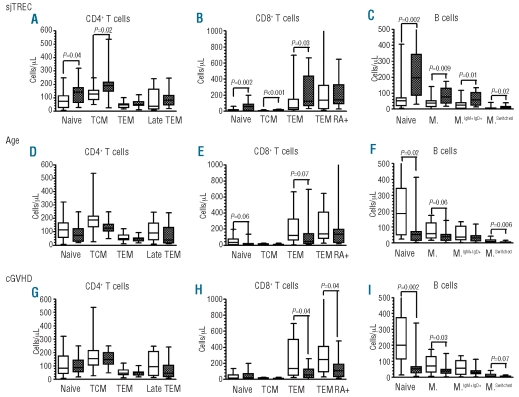
We then analyzed the correlation between sjTREC levels two years after HCT and detailed T- and B-cell phenotypes two years after HCT in a cohort of 33 patients for whom we had cryopreserved PBMC at that time point. There was a statistically significant correlation between 2-year sjTREC levels and patient age (inverse correlation, R=−0.54, P=0.001) as well as with 2-year counts of naïve CD4+CD45RA+CCR7+ T cells (positive correlation, R=0.43, P=0.012), central memory CD4+ T cells (positive correlation, R=0.38, P=0.028), naïve CD8+ T cells (positive correlation, R=0.59, P<0.001), central memory CD8+ T cells (positive correlation, R=0.55, P=0.001), effector memory CD8+ T cells (positive correlation, R=0.39, P=0.025), naïve B cells (positive correlation, R=0.53, P=0.001), memory B cells (positive correlation, R=0.45, P=0.008), IgM+IgD+ memory B cells (positive correlation, R=0.43, P=0.012) and switched memory B cells (positive correlation, R=0.45, P=0.008) (Figure 4A–C).
Figure 4.
CD4+ T-cell (A), CD8+ T-cell (B) and B-cell (C) phenotypes two years after HCT in patients with sjTREC levels below (white bars) or above (black bars) median (1,000 sjTREC/μL) at that time (n=33). CD4+ T-cell (D), CD8+ T-cell (E) and B-cell (F) subtype phenotypes two years after HCT in patients (white bars) or (black bars) under 57 years of age or 57 years and over at HCT. CD4+ T-cell (G), CD8+ T-cell (H) and B-cell (I) subtype phenotypes two years after HCT in patients without (white bars) or with (black bars) extensive chronic GVHD at that time. TCM, central memory T cells; TEM, effector memory T cells; TEM RA+, TEM RA+ CD8+ T cells; M., memory; M.IgM+IgD+ IgM+IgD+ memory B cells; M.Switched, switched memory B cells.
We also analyzed the impact of patient age and extensive chronic GVHD on T- and B-cell phenotypes. Patients aged 57 years and over (n=15) had lower counts of naïve CD8+ T cells (P=0.06), naïve B cells (P=0.02), memory B cells (P=0.06) and switched memory B cells (P=0.006) than those under 57 years of age at HCT (n=18) (Figure 4D–F). Finally, patients who had extensive chronic GVHD two years after HCT had lower counts of effector memory CD8+ T cells (P=0.04), effector memory RA+ CD8+ T cells (P=0.04), naïve B cells (P=0.002), memory B cells (P=0.04), and switched memory B cells (P=0.07) than those who did not (Figure 4G–I).
Correlation between thymic function and T-cell Vbeta repertoire diversity
In order to assess the impact of thymic function on Vbeta repertoire diversity, T-cell receptor Vbeta repertoire CDR3 spectratyping analyses were performed between two and nine (median three) years after HCT in 21 patients with low (<500 sjTREC/mL; n=9) or high (>500 sjTREC/mL; n=12) sjTREC levels, measured on the same day as the spectratyping analysis. As illustrated in the Online Supplementary Figure 2, the Vbeta repertoire was relatively complex even in patients with low thymic function, probably reflecting the fact that peripheral expansion of T cells contained in the graft eventually allowed a relatively diverse T-cell receptor Vbeta repertoire, although some oligoclonal T-cell receptor Vbeta families were observed, and particularly so in patients with low sjTREC levels. Specifically, median T-cell receptor Vbeta score was 239 (range 179–251) peaks in age-matched controls, 207 (range 173–246) peaks in patients with low sjTREC levels (P=0.038 in comparison to controls), and 218 (range 182–252) in patients with high sjTREC levels (NS in comparison to controls and to patients with low sjTREC). Furthermore, we quantified the deviation from normality of each repertoire by measuring its quadratic distance to an average repertoire measured in healthy donors (see Design and Methods section).32 The quadratic distance was 4.5 (range 3.2–6.5) in age-matched controls, 8.1 (range 3.8–11.3) in patients with low sjTREC levels (P=0.003 in comparison to controls), and 5.3 (range 4.5–9.1) in patients with high sjTREC levels (P=0.016 in comparison to controls, P=0.22 in comparison to patients with low sjTREC).
Correlation between thymic function and clinical events
Day 100 sjTREC levels were similar in patients who had grade II–IV acute GVHD before day 100, as compared to those who did not (687±947 vs. 824±1,303 sjTREC/mL, P=0.5). Day 100 sjTREC levels was not associated with the occurrence of chronic GVHD: the 1-year probability of chronic GVHD was 57% in patients with day 100 sjTREC levels below the median (323 sjTREC/mL) versus 52% in those with higher sjTREC levels on day 100 (P=0.5).
We then studied infections occurring between day 365 to 730 based on day 365 sjTREC levels. The probabilities of bacterial, fungal and viral infections were 40%, 9%, and 13%, respectively, in patients with day 365 sjTREC levels below the median (523 sjTREC/mL) versus 31% (P=0.3), 5% (P=0.6) and 17% (P=0.6), respectively, in those with higher levels. The 7-year probability of dying from infection was 40% in patients with day 365 sjTREC levels below the median versus 0% in those with higher values (P=0.01, Figure 2C). However, 6 of 7 patients who died from infections had extensive chronic GVHD at the time of death. Further, the association between 1-year sjTREC levels and the subsequent risk of dying from infection was no longer statistically significant (P=0.17) after adjustment for the presence of extensive chronic GVHD one year after HCT in a Cox’s model where sjTREC levels were modeled as a continuous linear variable.
Discussion
Late infections (with or without chronic GVHD) are the first causes of non-relapse death beyond one year after HCT in young patients given myeloablative conditioning.38,39 They have been attributed to slow recovery of CD4+ T cells.38,40 Nevertheless, despite the well established association between higher patient age and impaired immune recovery following allogeneic HCT,14 HCT after non-myeloablative conditioning has been successful treatment for many patients aged up to between 60 and 70 years of age, most of whom were without evidence of severe infection once systemic immunosuppression was discontinued.31,41 This apparent paradox prompted us to assess long-term immune recovery after non-myeloablative conditioning. Several observations were made.
First and most importantly, while patients below 50 years of age at the time of HCT had evidence of thymic recovery from day 100 to three years after HCT, thymic recovery was much slower in patients aged 50 to 60 years, and was virtually absent in patients over 60, even in those without chronic GVHD. These results mirror those reported by Hakim et al. in patients given autologous HCT where the authors observed a significant thymic rebound in approximately 80% of patients younger than 40 years, 45% of those aged 40 to 50 years, but in less than 15% of those aged 50 years and older.42
Recovery of naïve CD4 T cells after HCT in current patients somewhat mirrored recovery of thymic function assessed by sjTREC levels. Specifically, recovery of naïve T cells was observed by day 365 in patients below 50 years of age, but only at two years after HCT (and to a lesser extent) in patients above 50–60 years of age. Further, sjTREC levels correlated with those of CD4+CD45RA+ T cells one year and over after HCT, and we observed a strong correlation between sjTREC levels and naïve CD4+CD45RA+CCR7+ T-cell and naïve CD8+ T-cell counts two years after HCT. These observations are in agreement with previous reports showing that new naïve T cells originate mainly from the thymic pathway after HCT.43,44
Given the slow or absent thymic recovery in patients above 50 or 60 years, respectively, immune recovery in those patients should have depended mainly on peripheral expansion of mature T cells contained in the graft. Consistent with this possibility, recovery of CD8+ T cells occurred earlier than recovery of CD4+ T cells, and T-cell recovery was derived from memory rather than naïve T cells.15 Interestingly, peripheral expansion was sufficient to produce an efficient immune system in the majority of patients without GVHD. Indeed, TCRB repertoires were relatively complex both in patients with low compared to high sjTREC levels, and incidences of viral, bacterial and fungal infections were similar in patients with low or high sjTREC levels. The risk of death from infection was significantly higher in patients with low sjTREC levels, although all but one patient who died from infection had extensive severe chronic GVHD at the time of death suggesting that GVHD or GVHD treatment might also have played an important role in the risk of mortality from infection in the current study. The observation that late immunity in older patients mainly depends on mature T cells contained in the graft has important implications since it suggests that long-term immune function after HCT might be affected by techniques of in vitro or in vivo T-cell depletion of the graft in these patients. Analysis of long-term immune recovery in older patients given PBSC after alemtuzumab-based reduced-intensity conditioning45 would be particularly interesting to confirm this hypothesis.
Another observation of our study was the dramatic impact of chronic GVHD on immune recovery. Specifically, extensive chronic GVHD was significantly associated with low sjTREC levels, as well as low counts of CD4+ T cells, CD4+CD45RA+ (naïve) T cells, CD8+ T cells and B cells one year and over after HCT, and was significantly associated with lower counts of effector memory CD8+ T cells, effector memory RA+ CD8+ T cells, naïve B cell and memory B cells two years after HCT. The negative impact of chronic GVHD on immune recovery is probably multi-factorial.46 First, the negative impact of chronic GVHD on thymus architecture46 and function47–52 has been well demonstrated, and has been attributed to direct donor T-cell alloreactivity towards recipient thymus,53 and to a negative impact of immunosuppressive drugs (and particularly of glucocorticosteroids) on the thymus.54,55 Secondly, chronic GVHD has been shown to impair peripheral expansion of mature T cells, and the same is obviously true for immunosuppressive drugs given in the treatment of patients with chronic GVHD. Thirdly, chronic GVHD has been associated with reduced B-cell lymphopoiesis perhaps because of B-cell inhibitory cytokines produced by activated T cells in chronic GVHD patients or because of GVHD treatments.56
In summary, our data suggest that thymic neo-generation of T cells occurs from day 100 onwards in patients under 60 years of age. In contrast, the levels of sjTREC remain low for patients over 60 who depended nearly exclusively on peripheral expansion of mature donor T cells contained in the graft to reconstitute their T-cell compartment. This suggests that long-term immune function after HCT might be negatively impacted by techniques of in vitro or in vivo T-cell depletion of the graft in older patients given allogeneic HCT.
Acknowledgments
We thank Y Henrotin and M Mathy for helpful discussions about PCR analyses, V Dhennin from the Genotranscriptomics Platform of the GIGA, for help with T-cell spectratyping, and S Ormenese from the Imaging and Flow Cytometry Platform of the GIGA for help with flow cytometry analyses. The authors are also grateful to O Dengis and C Daulne for excellent technical assistance, to physicians and clinical staff for their dedicated care of the patients, and to N Schaaf-Lafontaine from the laboratory of Hematology.
Footnotes
Funding: MH is Télévie Research Fellow, SHB Postdoctoral Researcher, FB Senior Research Associate, and VG Research Director at the National Fund for Scientific Research (FNRS) Belgium. The study was in part supported by funds from the FNRS, the Belgian Foundation against Cancer (FBC), the anti-cancer foundation from the ULg, the CHU of Liège, the Terry Fox foundation, and by grants CA 78902, CA 18029 and HL 36444 from the National Institutes of Health, Bethesda, MD.
The online version of this article has a supplementary Appendix.
Authorship and Disclosures
The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Steinmann GG, Klaus B, Muller-Hermelink HK. The involution of the ageing human thymic epithelium is independent of puberty. A morphometric study. Scand J Immunol. 1985;22(5):563–75. doi: 10.1111/j.1365-3083.1985.tb01916.x. [DOI] [PubMed] [Google Scholar]
- 2.Fry TJ, Mackall CL. Current concepts of thymic aging. Springer Semin Immunopathol. 2002;24(1):7–22. doi: 10.1007/s00281-001-0092-5. [DOI] [PubMed] [Google Scholar]
- 3.Douek DC, McFarland RD, Keiser PH, Gage EA, Massey JM, Haynes BF, et al. Changes in thymic function with age and during the treatment of HIV infection. Nature. 1998;396(6712):690–5. doi: 10.1038/25374. [DOI] [PubMed] [Google Scholar]
- 4.Jamieson BD, Douek DC, Killian S, Hultin LE, Scripture-Adams DD, Giorgi JV, et al. Generation of functional thymocytes in the human adult. Immunity. 1999;10(5):569–75. doi: 10.1016/s1074-7613(00)80056-4. [DOI] [PubMed] [Google Scholar]
- 5.Haynes BF, Markert ML, Sempowski GD, Patel DD, Hale LP. The role of the thymus in immune reconstitution in aging, bone marrow transplantation, and HIV-1 infection (Review) Annu Rev Immunol. 2000;18:529–60. doi: 10.1146/annurev.immunol.18.1.529. [DOI] [PubMed] [Google Scholar]
- 6.Sandmaier BM, Mackinnon S, Childs RW. Reduced intensity conditioning for allogeneic hematopoietic cell transplantation: current perspectives. Biol Blood Marrow Transplant. 2007;13(1 Suppl 1):87–97. doi: 10.1016/j.bbmt.2006.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baron F, Storb R. Allogeneic hematopoietic cell transplantation following nonmyeloablative conditioning as treatment for hematologic malignancies and inherited blood disorders (Review) Molecular Therapy. 2006;13(1):26–41. doi: 10.1016/j.ymthe.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Barrett AJ, Savani BN. Stem cell transplantation with reduced-intensity conditioning regimens: a review of ten years experience with new transplant concepts and new therapeutic agents. Leukemia. 2006;20(10):1661–72. doi: 10.1038/sj.leu.2404334. [DOI] [PubMed] [Google Scholar]
- 9.Baron F, Storb R, Storer BE, Maris MB, Niederwieser D, Shizuru JA, et al. Factors associated with outcomes in allogeneic hematopoietic cell transplantation with non-myeloablative conditioning after failed myeloablative hematopoietic cell transplantation. J Clin Oncol. 2006;24(25):4150–7. doi: 10.1200/JCO.2006.06.9914. [DOI] [PubMed] [Google Scholar]
- 10.Storb R, Yu C, Wagner JL, Deeg HJ, Nash RA, Kiem H-P, et al. Stable mixed hematopoietic chimerism in DLA-identical littermate dogs given sublethal total body irradiation before and pharmacological immunosuppression after marrow transplantation. Blood. 1997;89(8):3048–54. [PubMed] [Google Scholar]
- 11.McSweeney PA, Niederwieser D, Shizuru JA, Sandmaier BM, Molina AJ, Maloney DG, et al. Hematopoietic cell transplantation in older patients with hematologic malignancies: replacing high-dose cytotoxic therapy with graft-versus-tumor effects. Blood. 2001;97(11):3390–400. doi: 10.1182/blood.v97.11.3390. [DOI] [PubMed] [Google Scholar]
- 12.Baron F, Maris MB, Sandmaier BM, Storer BE, Sorror M, Diaconescu R, et al. Graft-versus-tumor effects after allogeneic hematopoietic cell transplantation with nonmyeloablative conditioning. J Clin Oncol. 2005;23(9):1993–2003. doi: 10.1200/JCO.2005.08.136. [DOI] [PubMed] [Google Scholar]
- 13.Baron F, Petersdorf EW, Gooley T, Sandmaier BM, Malkki M, Chauncey TR, et al. What is the role for donor natural killer cells after nonmyeloablative conditioning? Biol Blood Marrow Transplant. 2009;15(5):580–8. doi: 10.1016/j.bbmt.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Storek J, Witherspoon RP. Immunological reconstitution after hemopoietic stem cell transplantation. In: Atkinson K, Champlin R, Ritz J, Fibbe WE, Ljungman P, Brenner MK, editors. Clinical Bone Marrow and Blood Stem Cell Transplantation. Cambridge, UK: Cambridge University Press; 2004. pp. 194–226. [Google Scholar]
- 15.Crooks GM, Weinberg K, Mackall C. Immune reconstitution: from stem cells to lymphocytes. Biol Blood Marrow Transplant. 2006;12(1 Suppl 1):42–6. doi: 10.1016/j.bbmt.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 16.Peggs KS. Reconstitution of adaptive and innate immunity following allogeneic hematopoietic stem cell transplantation in humans. Cytotherapy. 2006;8(5):427–36. doi: 10.1080/14653240600851938. [DOI] [PubMed] [Google Scholar]
- 17.Gress RE, Emerson SG, Drobyski WR. Immune reconstitution: how it should work, what’s broken, and why it matters. Biol Blood Marrow Transplant. 2010;16(1 Suppl):S133–7. doi: 10.1016/j.bbmt.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Storek J, Dawson MA, Maloney DG. Correlation between the numbers of naive T cells infused with blood stem cell allografts and the counts of naive T cells after transplantation. Biol Blood Marrow Transplant. 2003;9(12):781–4. doi: 10.1016/j.bbmt.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Douek DC, Vescio RA, Betts MR, Brenchley JM, Hill BJ, Zhang L, et al. Assessment of thymic output in adults after haematopoietic stem-cell transplantation and prediction of T-cell reconstitution. Lancet. 2000;355(9218):1875–81. doi: 10.1016/S0140-6736(00)02293-5. [DOI] [PubMed] [Google Scholar]
- 20.Weinberg K, Blazar BR, Wagner JE, Agura E, Hill BJ, Smogorzewska M, et al. Factors affecting thymic function after allogeneic hematopoietic stem cell transplantation. Blood. 2001;97(5):1458–66. doi: 10.1182/blood.v97.5.1458. [DOI] [PubMed] [Google Scholar]
- 21.Hochberg EP, Chillemi AC, Wu CJ, Neuberg D, Canning C, Hartman K, et al. Quantitation of T-cell neogenesis in vivo after allogeneic bone marrow transplantation in adults. Blood. 2001;98(4):1116–21. doi: 10.1182/blood.v98.4.1116. [DOI] [PubMed] [Google Scholar]
- 22.Lewin SR, Heller G, Zhang L, Rodrigues E, Skulsky E, van den Brink MR, et al. Direct evidence for new T-cell generation by patients after either T-cell-depleted or unmodified allogeneic hematopoietic stem cell transplantations. Blood. 2002;100(6):2235–42. [PubMed] [Google Scholar]
- 23.Jimenez M, Martinez C, Ercilla G, Carreras E, Urbano-Ispizua A, Aymerich M, et al. Clinical factors influencing T-cell receptor excision circle (TRECs) counts following allogeneic stem cell transplantation in adults. Transpl Immunol. 2006;16(1):52–9. doi: 10.1016/j.trim.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 24.Hazenberg MD, Otto SA, de Pauw ES, Roelofs H, Fibbe WE, Hamann D, et al. T-cell receptor excision circle and T-cell dynamics after allogeneic stem cell transplantation are related to clinical events. Blood. 2002;99(9):3449–53. doi: 10.1182/blood.v99.9.3449. [DOI] [PubMed] [Google Scholar]
- 25.Baron F, Storer B, Maris MB, Storek J, Piette F, Metcalf M, et al. Unrelated donor status and high donor age independently affect immunologic recovery after nonmyeloablative conditioning. Biol Blood Marrow Transplant. 2006;12(11):1176–87. doi: 10.1016/j.bbmt.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 26.Castermans E, Baron F, Willems E, Schaaf-Lafontaine N, Meuris N, Gothot A, et al. Evidence for neo-generation of T cells by the thymus after non-myeloablative conditioning. Haematologica. 2008;93(2):240–7. doi: 10.3324/haematol.11708. [DOI] [PubMed] [Google Scholar]
- 27.Baron F, Schaaf-Lafontaine N, Humblet-Baron S, Meuris N, Castermans E, Baudoux E, et al. T-cell reconstitution after unmanipulated, CD8-depleted or CD34-selected nonmyeloablative peripheral blood stem-cell transplantation. Transplantation. 2003;76(12):1705–13. doi: 10.1097/01.TP.0000093987.11389.F7. [DOI] [PubMed] [Google Scholar]
- 28.Baron F, Lechanteur C, Willems E, Bruck F, Baudoux E, Seidel L, et al. Cotransplantation of mesenchymal stem cells might prevent death from graft-versus-host disease (GVHD) without abrogating graft-versus-tumor effects after HLA-mismatched allogeneic transplantation following nonmyeloablative conditioning. Biol Blood Marrow Transplant. 2010;16(6):838–47. doi: 10.1016/j.bbmt.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 29.Sullivan KM. Graft-vs-host disease. In: Blume KG, Forman SJ, Appelbaum FR, editors. Thomas' Hematopoietic Cell Transplantation. Oxford, UK: Blackwell Publishing Ltd; 2004. pp. 635–64. [Google Scholar]
- 30.Baron F, Sandmaier BM. Chimerism and outcomes after allogeneic hematopoietic cell transplantation following nonmyeloablative conditioning. Leukemia. 2006;20(10):1690–700. doi: 10.1038/sj.leu.2404335. [DOI] [PubMed] [Google Scholar]
- 31.Willems E, Baron F, Baudoux E, Wanten N, Seidel L, Vanbellinghen JF, et al. Non-myeloablative transplantation with CD8-depleted or unmanipulated peripheral blood stem cells: a phase II randomized trial. Leukemia. 2009;23(3):608–10. doi: 10.1038/leu.2008.248. [DOI] [PubMed] [Google Scholar]
- 32.Baron V, Bouneaud C, Cumano A, Lim A, Arstila TP, Kourilsky P, et al. The repertoires of circulating human CD8(+) central and effector memory T cell subsets are largely distinct. Immunity. 2003;18(2):193–204. doi: 10.1016/s1074-7613(03)00020-7. [DOI] [PubMed] [Google Scholar]
- 33.Dion ML, Poulin JF, Bordi R, Sylvestre M, Corsini R, Kettaf N, et al. HIV infection rapidly induces and maintains a substantial suppression of thymocyte proliferation. Immunity. 2004;21(6):757–68. doi: 10.1016/j.immuni.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 34.Poulin JF, Sylvestre M, Champagne P, Dion ML, Kettaf N, Dumont A, et al. Evidence for adequate thymic function but impaired naive T-cell survival following allogeneic hematopoietic stem cell transplantation in the absence of chronic graft-versus-host disease. Blood. 2003;102(13):4600–7. doi: 10.1182/blood-2003-05-1428. [DOI] [PubMed] [Google Scholar]
- 35.Morrhaye G, Kermani H, Legros JJ, Baron F, Beguin Y, Moutschen M, et al. Impact of growth hormone (GH) deficiency and GH replacement upon thymus function in adult patients. PLoS One. 2009;4(5):e5668. doi: 10.1371/journal.pone.0005668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Storek J, Dawson MA, Storer B, Stevens-Ayers T, Maloney DG, Marr KA, et al. Immune reconstitution after allogeneic marrow transplantation compared with blood stem cell transplantation. Blood. 2001;97(11):3380–9. doi: 10.1182/blood.v97.11.3380. [DOI] [PubMed] [Google Scholar]
- 37.Cavazzana-Calvo M, Carlier F, Le Deist F, Morillon E, Taupin P, Gautier D, et al. Long-term T-cell reconstitution after hematopoietic stem-cell transplantation in primary T-cell-immunodeficient patients is associated with myeloid chimerism and possibly the primary disease phenotype. Blood. 2007;109(10):4575–81. doi: 10.1182/blood-2006-07-029090. [DOI] [PubMed] [Google Scholar]
- 38.Storek J, Gooley T, Witherspoon RP, Sullivan KM, Storb R. Infectious morbidity in long-term survivors of allogeneic marrow transplantation is associated with low CD4 T cell counts. Am J Hematol. 1997;54:131–8. doi: 10.1002/(sici)1096-8652(199702)54:2<131::aid-ajh6>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 39.Robin M, Porcher R, De Castro AR, de Latour RP, Devergie A, Rocha V, et al. Risk factors for late infections after allogeneic hematopoietic stem cell transplantation from a matched related donor. Biol Blood Marrow Transplant. 2007;13(11):1304–12. doi: 10.1016/j.bbmt.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 40.Roux E, Dumont-Girard F, Starobinski M, Siegrist CA, Helg C, Chapuis B, et al. Recovery of immune reactivity after T-cell-depleted bone marrow transplantation depends on thymic activity. Blood. 2000;96(6):2299–303. [PubMed] [Google Scholar]
- 41.Maris MB, Sandmaier BM, Storer BE, Maloney DG, Shizuru JA, Agura E, et al. Unrelated donor granulocyte colony-stimulating factor-mobilized peripheral blood mononuclear cell transplantation after non-myeloablative conditioning: the effect of postgrafting mycophenolate mofetil dosing. Biol Blood Marrow Transplant. 2006;12(4):454–65. doi: 10.1016/j.bbmt.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 42.Hakim FT, Memon SA, Cepeda R, Jones EC, Chow CK, Kasten-Sportes C, et al. Age-dependent incidence, time course, and consequences of thymic renewal in adults. J Clin Invest. 2005;115(4):930–9. doi: 10.1172/JCI22492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heitger A, Neu N, Kern H, Panzer-Grumayer ER, Greinix H, Nachbaur D, et al. Essential role of the thymus to reconstitute naive (CD45RA+) T-helper cells after human allogeneic bone marrow transplantation. Blood. 1997;90(2):850–7. [PubMed] [Google Scholar]
- 44.Mackall CL, Fleisher TA, Brown MR, Andrich MP, Chen CC, Feuerstein IM, et al. Age, thymopoiesis, and CD4+ T-lymphocyte regeneration after intensive chemotherapy. N Engl J Med. 1995;332(3):143–9. doi: 10.1056/NEJM199501193320303. [DOI] [PubMed] [Google Scholar]
- 45.D'Sa S, Peggs K, Pizzey A, Verfuerth S, Thuraisundaram D, Watts M, et al. T- and B-cell immune reconstitution and clinical outcome in patients with multiple myeloma receiving T-cell-depleted, reduced-intensity allogeneic stem cell transplantation with an alemtuzumab-containing conditioning regimen followed by escalated donor lymphocyte infusions. Br J Haematol. 2003;123(2):309–22. doi: 10.1046/j.1365-2141.2003.04612.x. [DOI] [PubMed] [Google Scholar]
- 46.Krenger W, Hollander GA. The immunopathology of thymic GVHD. Semin Immunopathol. 2008;30(4):439–56. doi: 10.1007/s00281-008-0131-6. [DOI] [PubMed] [Google Scholar]
- 47.Noel DR, Witherspoon RP, Storb R, Atkinson K, Doney K, Mickelson EM, et al. Does graft-versus-host disease influence the tempo of immunologic recovery after allogeneic human marrow transplantation? An observation on 56 long-term survivors. Blood. 1978;51:1087–105. [PubMed] [Google Scholar]
- 48.Atkinson K, Incefy GS, Storb R, Sullivan KM, Iwata T, Dardenne M, et al. Low serum thymic hormone levels in patients with chronic graft-versus-host disease. Blood. 1982;59(5):1073–7. [PubMed] [Google Scholar]
- 49.Dulude G, Roy DC, Perreault C. The effect of graft-versus-host disease on T cell production and homeostasis. J Exp Med. 1999;189(8):1329–42. doi: 10.1084/jem.189.8.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Clave E, Busson M, Douay C, Peffault de Latour R, Berrou J, Rabian C, et al. Acute graft-versus-host disease transiently impairs thymic output in young patients after allogeneic hematopoietic stem cell transplantation. Blood. 2009;113(25):6477–84. doi: 10.1182/blood-2008-09-176594. [DOI] [PubMed] [Google Scholar]
- 51.Bahceci E, Epperson D, Douek DC, Melenhorst JJ, Childs RC, Barrett AJ. Early reconstitution of the T-cell repertoire after non-myeloablative peripheral blood stem cell transplantation is from post-thymic T-cell expansion and is unaffected by graft-versus-host disease or mixed chimaerism. Br J Haematol. 2003;122(6):934–43. doi: 10.1046/j.1365-2141.2003.04522.x. [DOI] [PubMed] [Google Scholar]
- 52.Fallen PR, McGreavey L, Madrigal JA, Potter M, Ethell M, Prentice HG, et al. Factors affecting reconstitution of the T cell compartment in allogeneic haematopoietic cell transplant recipients. Bone Marrow Transplant. 2003;32(10):1001–14. doi: 10.1038/sj.bmt.1704235. [DOI] [PubMed] [Google Scholar]
- 53.Hauri-Hohl MM, Keller MP, Gill J, Hafen K, Pachlatko E, Boulay T, et al. Donor T-cell alloreactivity against host thymic epithelium limits T-cell development after bone marrow transplantation. Blood. 2007;109 (9):4080–8. doi: 10.1182/blood-2006-07-034157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yamada K, Gianello PR, Ierino FL, Fishbein J, Lorf T, Shimizu A, et al. Role of the thymus in transplantation tolerance in miniature swine: II. Effect of steroids and age on the induction of tolerance to class I mismatched renal allografts. Transplantation. 1999;67(3):458–67. doi: 10.1097/00007890-199902150-00020. [DOI] [PubMed] [Google Scholar]
- 55.Hattori A, Kunz HW, Gill TJ, 3rd, Shinozuka H. Thymic and lymphoid changes and serum immunoglobulin abnormalities in mice receiving cyclosporine. Am J Pathol. 1987;128(1):111–20. [PMC free article] [PubMed] [Google Scholar]
- 56.Storek J, Wells D, Dawson MA, Storer B, Maloney DG. Factors influencing B-lymphopoiesis after allogeneic hematopoietic cell transplantation (Brief Report) Blood. 2001;98(2):489–91. doi: 10.1182/blood.v98.2.489. [DOI] [PubMed] [Google Scholar]