Abstract
The present study evaluated methods for training mental health providers (N=46) in exposure therapies (ETs) for anxiety disorders. A pilot randomized controlled trial compared: 1) an interactive, multimedia online training (ET OLT), 2) the ET OLT plus a brief Motivational Interviewing-based intervention (ET OLT + MI), and 3) a placebo control OLT. Assessments were completed at baseline, post-training, and one week following training. Both ET OLT and ET OLT + MI received high satisfaction ratings and were comparably effective at increasing knowledge of ETs as well as clinicians’ overt efforts to learn and use the treatment. ET OLT + MI was the most effective method for improving clinicians’ attitudes toward ETs. Results indicate that OLT is effective for disseminating knowledge about ETs to clinicians, and suggest that supplementing OLT with a brief MI-based intervention may be a promising direction to address potential attitudinal barriers to adopting these highly efficacious treatments.
Keywords: Dissemination, Online Training, Exposure Therapy, Motivational Interviewing
Anxiety disorders are the most common psychological disorder in the United States and are estimated to affect 28.8% of the population over a lifetime (Kessler, 2005). Anxiety disorders tend to start at a young age (Kessler, 2005), have a chronic course (Bruce et al., 2005; Keller et al., 1994), and result in significant disability (Buist-Bowman et al., 2006). Despite the widespread and often disabling nature of anxiety disorders, most individuals suffering from these disorders receive no or inadequate treatment (Wang, Berglund, & Kessler, 2000; Wang, Demler, & Kessler, 2002; Wang et al., 2005). Exposure therapies (ETs) include a family of highly effective psychosocial treatments that utilize exposure procedures to resolve anxiety disorders through repeated and prolonged contact of the client with the stimuli that are presumed to cause anxiety (Richard & Lauterbach, 2007). The basic premise of ETs is that individuals with anxiety disorders need to be exposed to anxiety-provoking stimuli in the absence of aversive consequences to learn that these stimuli are in fact not dangerous, they can tolerate anxiety, and anxiety will decrease over time through a process of habituation.
Efficacy of ETs has been well-documented in hundreds of clinical trials involving thousands of patients who suffer from anxiety disorders. Meta-analyses of this extensive research have found ETs to yield large effect sizes for pre- to post-treatment changes in panic disorder (Bakker, van Balkom, Spinhoven, Blauuw, & van Dyck, 1998; Gould, Otto, & Pollack, 1995), obsessive compulsive disorder (OCD; Abramowitz, 1996), social phobia (Fedoroff & Taylor, 2001; Feske & Chambless, 1995), post-traumatic stress disorder (PTSD; Bradley, Greene, Russ, Dutra, & Westen, 2005), and generalized anxiety disorder (GAD; Gould, Otto, Pollack, & Yap, 1997). Meta-analytic research has also shown that ETs are superior to waitlist and supportive control conditions and produce equivalent results as other, often more complex, psychosocial treatments (e.g., Bradley et al., 2005; Feske & Chambless, 1995). Moreover, ETs are tolerated as well as other psychosocial treatments, as evidenced by research indicating that rates of attrition do not differ across treatments (Feske & Chambless, 1995; Hembree et al., 2003). Studies comparing ETs to pharmacological treatments have generally found that both treatments have comparable short-term effects in the treatment of anxiety disorders, but ETs are superior in terms of longer-term outcome and tolerability (Gould, Buckminster, Pollack, Otto, & Yap, 1997; Gould et al., 1995).
Despite extensive research that overwhelmingly supports efficacy of ETs for anxiety disorders, as well as their relatively straightforward rationale and associated treatment strategies, very few mental health professionals use or are familiar with exposure procedures. Surveys of treatment providers have found that very few utilize ETs in their treatment of anxiety disorder clients (7–38%; Becker, Zayfert, & Anderson, 2004; Freiheit, Vye, Swan, & Cady, 2004; Rosen et al., 2004). Similarly, very few individuals with anxiety disorders report having received ETs (7–21%; Goisman, Warshaw, & Keller, 1999; Marcks, Weisberg, & Keller, 2009). Underutilization of ETs in routine clinical practice appears to be primarily due to a lack of training opportunities. A U.S. survey of psychologists found that the most commonly endorsed reason for not using exposure to treat PTSD was limited training; 12–28% of psychologists reported having received training in ETs for PTSD or other anxiety disorders (Becker et al., 2004). Similarly, a European survey of trauma experts found that imaginal exposure was the least used treatment for PTSD, and participants reported that they had received less training in imaginal exposure than other psychosocial treatments (van Minnen, Hendriks, & Olff, in press). However, even among clinicians who are trained in exposure procedures, many do not regularly use the treatment with their anxiety disorder patients. Additional perceived barriers to using ETs to treat PTSD include a preference for individualized treatment over manualized therapy, a concern that patients will decompensate or drop out of treatment, and a belief that ETs are contraindicated for many clients (Becker et al., 2004; van Minnen et al., in press). These findings correspond to some of the common myths that exist about ETs among mental health professionals, including beliefs that the treatment is insensitive, overly rigid, ineffective, potentially iatrogenic, not generalizable to “real-world” clients and clinical settings, and perhaps even unethical (Feeny, Hembree, & Zoellner, 2003; Olatunji, Deacon & Abramowitz, 2009; Richard & Gloster, 2007). Taken together, these findings suggest that another significant barrier to the dissemination of ETs is clinicians’ beliefs that they will be unsafe, unacceptable, or not well tolerated by patients – beliefs that are not supported by either the research data or surveys of potential consumers (see Olatunji et al., 2009 for a review).
The primary aim of the present study was to evaluate methods for overcoming barriers to disseminating ETs for anxiety disorders, including lack of training and negative attitudes toward the treatment. To that end, we conducted a pilot randomized controlled trial (RCT) examining the comparative efficacy of two active training conditions and a placebo control condition. The first training condition utilized an online training (OLT) course that was designed to cover foundational knowledge about ETs as well as to address many of the common misconceptions about ETs. OLT was chosen as the training method because it possesses a number of advantages over traditional treatment manuals and instructor-led trainings (ILTs), such as a user-friendly design, the ability to elicit greater learner engagement via dynamic interactivities, the provision of realistic models of simulated therapist-client interactions, and improved accessibility (Weingardt, 2004). Moreover, OLT has been found to be an effective method of training mental health providers in evidence-based treatments in a number of RCTs (Dimeff, Beadnell, Woodcock, & Harned, in press; Dimeff et al., 2009; Sholomskas & Carroll, 2006; Sholomskas et al., 2005).
To further address potential attitudinal barriers to adopting ETs, a second training condition supplemented the ET OLT with a brief intervention that incorporated strategies from Motivational Interviewing (MI; Miller & Rollnick, 1991). MI is a brief yet powerful intervention for increasing motivation to change a variety of behavioral and health problems and is often used as a precursor to another active treatment to improve engagement and outcome in the subsequent intervention (Hettema, Steele, & Miller, 2005). In the present study, clinicians in this training condition (ET OLT + MI) participated in brief phone calls before and after completing the ET OLT that focused on discussing their beliefs about ETs and addressing any ambivalence they may have felt about learning and using ETs as a result of these beliefs. This approach is consistent with previous research indicating that supplementing a standard training workshop with a brief psychological intervention (Acceptance and Commitment training) improved clinicians’ subsequent willingness to use the newly learned treatment (Varra, Hayes, Roget, & Fisher, 2008).
We hypothesized that the ET OLT and ET OLT + MI would result in comparable increases in knowledge as well as ratings of usability and acceptability. Further, we hypothesized that ET OLT + MI would outperform ET OLT in terms of improving clinicians’ self-efficacy, motivation, attitudes toward exposure, and their use of exposure procedures in clinical practice. Finally, we hypothesized that both active training conditions would outperform the placebo control OLT on all outcomes except usability of the training course.
1. Method
1.1. Procedures
1.1.1. Recruitment and Screening
All procedures were approved by the University of Washington Institutional Review Board (IRB) and the Western IRB. Participant enrollment began in October 2008 and the final follow-up assessment occurred in December 2008. Participants were recruited via a Dialectical Behavior Therapy email listserv via an email that requested help evaluating an online training course in exposure therapies. Interested individuals completed a phone screen to determine eligibility. Inclusion criteria were: (1) at least 18 years of age, (2) currently employed as a treatment provider at a mental health agency or were students working to obtain a professional degree in a mental health-related field, (3) currently treating clients with anxiety disorders or were engaged in an educational curriculum that provided training in the treatment of anxiety disorders, (4) has access to a computer with a sound card and an internet connection, and (5) minimal prior exposure to ETs. To ensure that participants had minimal prior exposure to ETs, individuals were excluded from participation if they had: (1) read any portion of published treatment manuals on an empirically-supported ET or (2) attended a lecture, workshop, or intensive training on ET. Overall, 75 individuals contacted the study and were screened for participation. 24 did not meet inclusion criteria (17 had more than minimal prior exposure to ET, 2 were not currently treating clients, 1 had completed the control OLT in a previous study, 4 declined participation).
1.1.2. Randomization
Following the screening, eligible participants (n=51) were assigned to one of the three study conditions by the Participant Coordinator (PC) via a randomization minimization procedure (White & Freedman, 1978). Participants were matched on educational degree (1=MD/PhD or doctoral candidate; 2=MA/MS/RN or current graduate student; 3= BA/BS level; 4=High School/AA) and clinical experience (1=7 plus years; 2=2–6 years; 3=less than 2 years).
1.1.3. Assessment Procedures
Following randomization, participants were emailed a copy of the informed consent form and were scheduled for an experimental session. The experimental session involved sending participants an internet link to a secured, encrypted assessment site to complete the baseline assessment. Once done, they were sent internet links to their respective OLT course as well as to the post-training assessment. There was no time limit for completing the training, although participants were encouraged to set aside two hours for its completion. Technical support was available should participants have had difficulties accessing the program. Upon completing the post-training assessment, participants were scheduled for the one-week follow-up assessment. At the scheduled follow-up assessment time, the PC sent participants an internet link to the final assessment. Participants in the ET OLT + MI condition also had up to two brief (up to 20-minute) MI-based phone calls: (1) after completing the baseline assessment and within 72 hours of starting the OLT, and (2) within 24 hours of completing the OLT and post-training assessment and prior to the follow-up assessment. Participants were paid for study participation and no adverse events occurred. All participants were allowed to view the OLT for the condition they were not assigned to upon study completion.
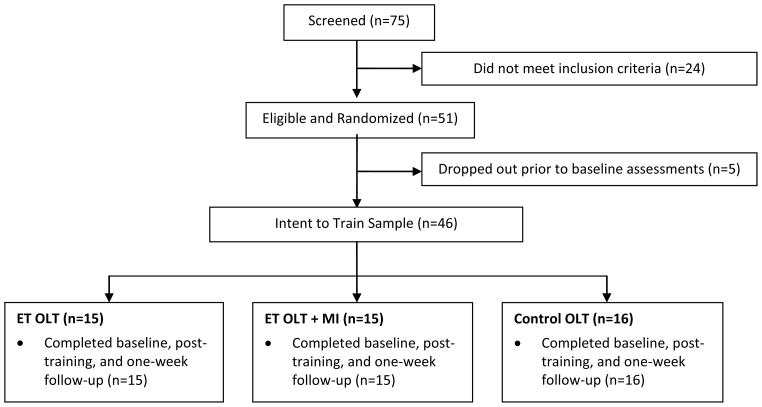
1.2. Subject Flow and Retention
Subject flow from initial phone screening through the one-week follow-up assessment is provided in Figure 1. Of the 51 individuals who were eligible and randomized to a condition, 5 did not complete the baseline assessments. There was no association between failure to complete baseline assessment and experimental condition (χ2(2) = 0.44, p = .80). Of the 46 subjects who completed the baseline assessment (i.e., the “intent-to-train” sample), 100% completed at least one measure at both post-training and one-week follow-up.
Figure 1.
Subject flow from screening through the one-week follow-up assessment.
1.3 Training Conditions
1.3.1. Exposure Therapy Online Training (ET OLT; n=15)
The ET OLT was developed by the first two authors during a formative evaluation phase, which used an iterative process of development to ensure usability, acceptability, and relevance of course content. During this formative phase, feedback on all elements of the OLT was obtained via extensive usability testing with our target audience (i.e., clinicians without prior training in ETs) as well as input from an advisory panel of ET experts. Feedback on the course was obtained via focus groups and individual interviews with clinicians. The final course that was used in the present study included a video montage Introduction and four content modules. (1) Setting the Stage, (2) Step 1: Presenting the Feared Stimulus, (3) Step 2: Corrective Learning, (4) Step 3: Avoid Avoidance. Setting the Stage reviews the empirical and theoretical foundations of ETs (e.g., theories of fear acquisition and maintenance). Step 1 describes the three primary types of exposure (in vivo, imaginal, and interoceptive) and learners engage in an interactivity in which they construct an exposure hierarchy for a fictional client. Step 2 focuses on how best to achieve corrective learning (e.g., using prolonged, repeated exposure across multiple contexts) and includes an interactivity in which learners must decide how long to continue an exposure task. Finally, Step 3 highlights the importance of minimizing avoidance during exposure and provides tips and practice exercises for recognizing and addressing avoidance when it occurs. The course also included an optional Design Your Own Exposure Treatment module, a Resources section providing supplementary information (e.g., a list of treatment manuals for further training), and a Bonus Features section including videos of ET experts discussing clinical cases and addressing concerns related to therapist anxiety about doing ET. A fictional anxiety disorder client appeared throughout the program, which allowed learners to observe and apply course concepts in a risk-free environment with a hypothetical client via clinical simulations. Each module included interactive exercises, knowledge checks to assess learner understanding, and content designed to address common myths about ET. The program was built in Flash and utilized both audio and visual material to create a highly interactive and engaging training.
1.3.2. Exposure Therapy Online Training plus Motivational Interviewing (ET OLT + MI; n=15)
In addition to receiving the ET OLT course (described above), participants in this condition participated in 1–2 brief (up to 20-minute) MI-based phone calls with either the first or second author. These semi-structured interviews were based on MI principles and utilized a variety of motivation-enhancing strategies in an effort to decrease ambivalence about adopting ETs due to attitudinal barriers. In pre-training phone calls, interviewers focused on eliciting self-motivational statements (e.g., by asking participants about the pros and cons of their current approach to treating anxiety disorders), assessing participants’ ratings of the importance of learning about ETs and their confidence in their ability to use ETs as well as their reasons for choosing those ratings, and summarizing self-motivational statements and any areas of ambivalence or concern about adopting ETs. Post-training calls focused on re-assessing participants’ importance and confidence ratings, discussing whether any concerns raised in the pre-training call had changed, summarizing their statements, asking about next steps, and helping to problem-solve ways of achieving these next steps. Throughout the phone calls, interviewers responded to participants via empathic reflection, affirmation, and reframing. The protocol for the phone calls was developed in consultation with a certified MI trainer and expert.
1.3.3 Control Online Training (Control OLT; n=16)
The control OLT was entitled “DBT Validation Principles and Strategies” and was previously developed by the second author. This OLT was intended to function as a placebo attention control that would appeal to the sample recruited for this study as it focused on teaching providers how to actively validate a client in therapy using DBT. The control OLT was comparable in quality, length, and design to the ET OLT and contained no overlapping content.
1.4 Measures
The primary outcome measures in this study were gains in knowledge of ET principles and procedures, attitudes toward ET, self-efficacy, and motivation to apply ET techniques with anxiety disorder clients. Secondary outcomes included satisfaction with the training and utilization of the course content in clinical practice. Because all measures involved self-report, there were no blinded assessments. All outcome measures were administered at baseline, post-training, and one-week follow-up with the exception of the satisfaction survey (post-training only) and the skills use measure (baseline and one-week follow-up only).
1.4.1. Phone screen
This 18-item measure was administered via telephone by the PC to determine participant eligibility and assessed demographics, professional characteristics, experience treating anxiety disorders, and prior formal and informal training in ETs.
1.4.2. Knowledge test
A 27-item multiple choice instrument (with 4–5 response choices per item) was developed to assess knowledge of course content as well as ability to apply knowledge in hypothetical clinical scenarios. All items were developed by study investigators and multiple iterations were piloted to naïve respondents, and then refined, before the final version was created for the research trial. The score used for analysis was the proportion of items correct.
1.4.3. Self-efficacy
A 30-item measure assessing participants’ confidence in their ability to use ET with clients was created for the purposes of this study. All items began with “I feel confident in my ability to” and an example item is “Conduct imaginal exposure.” Items were rated on a 5-point Likert scale ranging from 1 = “Not Confident” to 5 = “Very Confident.” The score used for analysis was the mean across items (Cronbach’s alpha ranged from 0.98 to 0.99).
1.4.4. Motivation
A 4-item measure was created for the purposes of this study to assess participants’ motivation to learn and use ETs. All items began with “I am motivated to” and an example item is “Use exposure procedures with my clients who have anxiety disorders.” Items were rated on a 5-point Likert scale with 1 = “Strongly Disagree” and 5 = “Strongly Agree.” The score used for analysis was the mean across items (Cronbach’s alpha ranged from 0.76 to 0.84).
1.4.5. Credibility scale (CS)
This scale was adapted from a measure created by Addis and Carpenter (1999) and included a brief description of ET followed by 7 items assessing its perceived credibility. The CS has shown good internal consistency in a number of studies of treatment preference (e.g., Zoellner, Feeny, Cochran, & Pruitt, 2003). The items were adapted to refer to “exposure therapy” and “anxiety disorders” and the description of ET was adapted from two previous studies (Tarrier et al., 2006; Zoellner et al., 2003). An example item is: “How scientific does exposure therapy seem to you?” Items were rated on a 7-point scale from 1 = “Not at all” to 7 = “Extremely.” A total score was created by summing all items with higher scores indicating greater perceived credibility (Cronbach’s alpha ranged from 0.84 to 0.92).
1.4.6. Attitudes toward exposure therapy (ATET)
A 21-item measure of clinician attitudes toward ET was developed for the present study. Items were generated by study investigators based on the scientific literature on clinician beliefs about ET (Becker et al., 2004; Feeny et al., 2003; Tarrier, Liversidge, & Gregg, 2006) and interviews with treatment providers. Items included a mixture of positive and negative beliefs about ET (e.g., “Exposure therapy is effective for real-world patients with complex problems” and “Exposure therapy is too emotionally distant or “cold” for my liking”). Items were rated on a 5-point Likert scale ranging from 1= “Not at all” or “Strongly disagree” to 5 = “Very much so” or “Strongly agree”. A total score was created by reverse-scoring positively-phrased items and then averaging all items such that higher scores represent more negative attitudes toward ET. This measure demonstrated strong internal consistency (Cronbach’s alpha ranged from 0.76 to 0.87) as well as evidence for convergent validity as it correlated highly with the CS (r’s ranged from −0.54 to −0.69, all p’s < .001).
1.4.7. Satisfaction survey
This measure assessed participants’ satisfaction with their assigned training condition. An Acceptability subscale (7 items) assessed course relevance, appropriateness, and usefulness for learning ETs (Cronbach’s alpha ranged from .83 to .91). Items were rated on a 5-point Likert scale ranging from 1 = “Not enjoyable/helpful/relevant/likely” or “Didn’t hold my interest” to 5 = “Extremely enjoyable/helpful/relevant/likely” or “Completely held my interest”. An example item is: “How relevant was this topic to your treatment of individuals with anxiety disorders?” A Usability subscale (5 items) assessed the usability of the training for learning ETs (Cronbach’s alpha ranged from .82 to .88). Items were assessed using a 7-point Likert Scale from 1 = “Very boring/difficult” or “Not at all” to 7 = “Very interesting/easy/informative.” An example item is: “How easy was the material to understand?” Subscale scores were created by averaging items.
1.4.8. Readiness to change questionnaire (RCQ)
This 12-item scale was adapted from the original RCQ (Rollnick, Heather, Gold, & Hall, 1992) that was developed for problem drinkers and is based on the transtheoretical stages of change model (Prochaska, DiClemente, & Norcross, 1992). The RCQ assesses the precontemplation, contemplation, and action stages of change and has been shown to demonstrate internal reliability as well as concurrent and predictive validity (Rollnick et al., 1992). The RCQ was modified to assess efforts to learn and use ET and an example item is “I am trying to use exposure therapy more than I used to” (Action). Items were rated on a 5-point Likert scale ranging from 1 = “Strongly disagree” to 5 = “Strongly agree.” Analysis focused on the 4-item Action subscale (i.e., overt efforts to change behavior; Cronbach’s alpha ranged from 0.62 to 0.79). A categorical variable was also created for descriptive purposes that assigned participants to the stage on which they had the highest score.
1.4.9. Skills use
Four self-report items assessed participants’ application of the course content in their clinical practice. An example item is: “In the past week, how many times did you teach or apply exposure therapy in your clinical work?” Items were averaged for analysis. (Cronbach’s alpha was 0.84 for all timepoints).
1.5. Analysis Strategy
Longitudinal outcome measures were examined via Hierarchical Linear Modeling (HLM) using PROC MIXED models in SAS 9.2. HLM has the advantages of allowing for the additional clustering of repeated measures within individuals as well as the specification of the best fitting covariance structure (Raudenbush & Bryk, 2002). Additionally, HLM allowed inclusion of all 46 intent-to-train participants (even those without complete data on all measures at the follow-up assessments). Predictors in the analyses were experimental Condition, Time, and the Time by Condition interaction. The best-fitting covariance structures were selected and then specified based on the Akaike’s Information Criterion (AIC; Hox, 2002). Type III F-tests (omnibus tests to determine if differences existed between conditions) were calculated, and when significant, post-hoc pair-wise comparisons of predicted means from regression estimates were used to identify which conditions differed at each time point. Power analyses indicated that 46 participants would be sufficient to detect medium effect sizes (f = 0.25) for the omnibus time by condition interactions in the HLM models using a two-tailed test (alpha = 0.05) at power = 0.80 (Cohen, 1988). Additionally, follow-up analyses (post-hoc pairwise comparisons) had sufficient power to detect large effect sizes (f = 0.47) using a two-tailed test (alpha= 0.05) at power = 0.80 (Cohen, 1988).
2. Results
2.1. Sample Description
Participants in the intent-to-train sample (N=46) did not significantly differ between conditions on any demographic or professional characteristic (see Table 1).
Table 1.
Sample Characteristics
| Characteristics | ET OLT (n=15) | ET OLT + MI (n=15) | Control OLT (n=16) | Full Sample (N=46) |
|---|---|---|---|---|
| Age M (SD) | 42.20 (9.48) | 40.40 (9.28) | 41.50 | 41.37 (11.47) |
| Gender | ||||
| Female | 86.7% | 86.7% | 75.0% | 82.6% |
| Male | 13.3% | 13.3% | 25.0% | 17.4% |
| Ethnicity | ||||
| Caucasian | 80.0% | 73.3% | 68.8% | 73.9% |
| Native American | 0.0% | 0.0% | 0.0% | 0.0% |
| African American | 6.7% | 0.0% | 12.5% | 6.5% |
| Asian American | 13.3% | 13.3% | 0.0% | 8.7% |
| Hispanic/Latino | 0.0% | 6.7% | 18.8% | 8.7% |
| Other | 0.0% | 6.7% | 0.0% | 2.2% |
| Education | ||||
| BA/BS | 13.3% | 6.7% | 6.3% | 8.7% |
| MA/MS | 60.0% | 60.0% | 50.0% | 56.5% |
| Psy.D./Ph.D./M.D. | 26.7% | 26.7% | 31.3% | 28.3% |
| Ph.D. -dissertation | 0.0% | 6.7% | 12.5% | 6.5% |
| Profession | ||||
| Psychiatrist | 0.0% | 0.0% | 0.0% | 0.0% |
| Psychologist | 26.7% | 13.3% | 31.3% | 23.9% |
| RN/ARNP | 6.7% | 6.7% | 0.0% | 4.3% |
| Social Worker (MSW) | 20.0% | 33.3% | 25.0% | 26.1% |
| Master’s Level Counselor | 26.7% | 26.7% | 25.0% | 26.1% |
| Bachelor’s Level | 6.7% | 0.0% | 6.3% | 4.3% |
| Other | 13.3% | 20.0% | 12.5% | 15.2% |
| Work Setting | ||||
| Private Practice | 20.0% | 13.3% | 18.8% | 17.4% |
| Outpatient CMHC | 33.3% | 40.0% | 25.0% | 32.6% |
| Day Treatment | 6.7% | 6.7% | 6.2% | 6.5% |
| Inpatient Treatment | 0.0% | 13.3% | 25.0% | 13.0% |
| Residential Treatment | 13.3% | 6.7% | 6.3% | 8.7% |
| Corrections Facility | 6.7% | 0.0% | 0.0% | 2.2% |
| Drug Treatment Program | 0.0% | 13.3% | 6.2% | 6.5% |
| School/Training Program | 13.3% | 6.7% | 6.2% | 8.7% |
| Other | 6.7% | 0.0% | 6.2% | 4.3% |
| Experience M (SD) | ||||
| Years worked as a treatment provider | 6.23 (7.59) | 7.27 (7.13) | 8.69 (9.93) | 7.45 (8.24) |
| Theoretical Orientation | ||||
| Cognitive-behavioral | 66.7% | 73.3% | 62.5% | 67.4% |
| Psychodynamic | 13.3% | 6.7% | 6.3% | 8.7% |
| Family systems | 6.7% | 6.7% | 6.3% | 6.5% |
| Interpersonal | 0.0% | 6.7% | 6.3% | 4.3% |
| Behavioral | 0.0% | 0.0% | 6.3% | 2.2% |
| Existential/Humanistic | 6.7% | 0.0% | 0.0% | 2.2% |
| Other | 6.7% | 6.7% | 12.5% | 8.7% |
Note. No between-group differences were statistically significant. Analyses were conducted using ANOVAs and chi-square tests as appropriate. Some categories do not total 100.0% because of rounding. CMHC = community mental health center.
2.2. Preliminary Analyses
2.2.1. Baseline between-condition differences
HLM analyses revealed no significant baseline between-condition differences on any outcome variable.
2.2.2. Time engaged in training
At post-training, participants were asked how many minutes they spent completing their assigned training condition. A cross-sectional HLM revealed no differences between conditions, F (2, 40) = 1.90, p =.16: ET OLT (134.64 ± 48.09), ET OLT + MI (115.36 ± 27.14), and Control OLT (107.33 ± 37.79).
2.3. Primary Outcome Analyses
Table 2 presents descriptive information for each longitudinal outcome at each time-point, by condition, and the associated statistics from the HLM analyses. Between-condition Cohen’s d effects sizes are shown in Table 3.
Table 2.
Means, Standard Deviations, and HLM Results by Condition and Time-point
| Baseline | Post-Training | One-Week Follow-up | Fdf | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ET OLT (n=15) | ET OLT + MI (n=15) | Control OLT (n=16) | ET OLT (n=14–15) | ET OLT + MI (n=15) | Control OLT (n=15–16) | ET OLT (n=14–15) | ET OLT + MI (n=14–15) | Control OLT (n=14–16) | Condition | Time | Condition × Time | |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | ||||
| Knowledge | 0.29 (0.09) | 0.26 (0.11) | 0.33 (0.11) | 0.71 (0.22)a | 0.74 (0.13)b | 0.31 (0.14)ab | 0.65 (0.22)a | 0.67 (0.17)b | 0.34 (0.17)ab | 13.972,43*** | 133.552,86*** | 36.734,86*** |
| Self-efficacy | 2.25 (0.77) | 2.28 (0.87) | 2.47 (0.85) | 3.57 (0.61)a | 3.88 (0.57)b | 2.38 (0.97)ab | 3.42 (0.80)a | 3.94 (0.60)b | 2.37 (1.01)ab | 7.222,42** | 39.952,46*** | 12.514,46*** |
| Motivation | 4.65 (0.57) | 4.73 (0.36) | 4.75 (0.35) | 4.61 (0.34) | 4.59 (0.37) | 4.43 (0.54) | 4.52 (0.36) | 4.58 (0.40) | 4.48 (0.57) | 0.172,43 | 4.762,84* | 0.764,84 |
| Attitudes | 2.29 (0.46) | 2.32 (0.42) | 2.31 (0.43) | 2.08 (0.35) | 2.07 (0.20)a | 2.37 (0.47)a | 2.10 (0.25) | 2.01 (0.28)a | 2.35 (0.44)a | 1.632,43 | 6.242,83** | 2.894,83* |
| Credibility | 39.50 (5.02) | 40.44 (5.33) | 41.31 (4.00) | 41.93 (4.16) | 43.12 (4.57) | 40.20 (5.93) | 41.14 (4.40) | 43.27 (4.40) | 40.87 (4.53) | 0.612,43 | 3.572,83* | 2.574,83* |
| Action | 12.80 (3.30) | 12.40 (2.56) | 11.87 (2.29) | 14.64 (1.55)a | 14.29 (2.73)b | 12.27 (3.26)ab | 15.14 (2.68)a | 15.71 (2.52)b | 11.87 (3.16)ab | 4.322,43* | 12.362,81*** | 3.604,81** |
| Skills use | 0.77 (1.22) | 0.42 (0.61) | 0.52 (0.89) | – | – | – | 0.93 (0.87) | 0.61 (1.00) | 0.54 (0.97) | 1.142,40 | 1.511,37 | 0.442,37 |
p < .05,
p<.01,
p<.001
In a row, when means share the same subscript this means that they are significantly different (in post-hoc comparisons, p < .05)
Table 3.
Cohen’s d Effect Sizes of Raw Means Between-Conditions for each Outcome Measure
| ET OLT vs. ET OLT + MI | ET OLT vs. Control OLT | ET OLT + MI vs. Control OLT | ||||
|---|---|---|---|---|---|---|
| Post-Training | One-Week F/U | Post-Training | One-Week F/U | Post-Training | One-Week F/U | |
| Knowledge | 0.17 | 0.11 | 2.26* | 1.68* | 3.29* | 2.01* |
| Self-efficacy | 0.54 | 0.77 | 1.51* | 1.19* | 1.95* | 1.96* |
| Motivation | 0.06 | 0.16 | 0.41 | 0.09 | 0.36 | 0.21 |
| Attitudes | 0.04 | 0.35 | 0.72 | 0.72 | 0.86* | 0.95* |
| Credibility | 0.28 | 0.50 | 0.35 | 0.06 | 0.57 | 0.56 |
| Action | 0.16 | 0.23 | 0.95* | 1.15* | 0.69* | 1.39* |
| Skills use | – | 0.35 | – | 0.44 | – | 0.07 |
Note. Interpretation of Cohen’s d: .20 small effect, .50 medium, and .80 large (Cohen, 1988). Effect sizes with an asterisk represent statistically significant differences. F/U = follow-up.
2.3.1. Knowledge
As shown in Table 2, participants correctly answered less than one-third of the knowledge test items at baseline. A significant effect for Time indicated that the sample as a whole generally improved on knowledge of ET across time, while a significant Time by Condition interaction revealed differential change between conditions. Post-hoc comparisons showed that the active training conditions (ET OLT and ET OLT + MI) significantly outperformed the Control OLT at post-training and the one-week follow-up with very large between-condition effect sizes (see Table 3). From baseline to post-training, both active conditions more than doubled their knowledge test scores (ET OLT = 29% vs. 71%, ET OLT + MI = 26% vs. 74%), whereas no change in knowledge was found in Control OLT (33% vs. 31%). The two active conditions did not significantly differ at either post-training or one-week follow-up.
2.3.2. Self-efficacy
A significant effect for Time indicated that all conditions generally improved in self-efficacy across time (Table 2). In addition, the Time by Condition interaction was significant and post-hoc comparisons revealed that the two active conditions outperformed the Control OLT at both post-training and one-week follow-up. In addition, medium to large effects (see Table 3) indicated that ET OLT + MI reported higher levels of self-efficacy than ET OLT at post-training and one-week follow-up, but these differences did not reach statistical significance.
2.3.3. Motivation
As seen in Table 2, motivation was high for all three conditions at baseline (Ms = 4.65 – 4.75 on a 5-point scale). The three conditions did not differ in the rate of change in motivation across time. There was a significant effect for Time, indicating that the sample as a whole generally showed a slight decrease in motivation across time. This may not have been a particularly meaningful change, however, as participants remained highly motivated at the one-week follow-up (Ms = 4.48 – 4.58).
2.3.4. Attitudes toward ET
Participants reported somewhat positive attitudes toward ET at baseline (Table 2). All three conditions generally improved in attitudes toward ET across time and a significant Time by Condition interaction indicated a differential rate of change between conditions. Post-hoc comparisons found that ET OLT + MI resulted in significantly more positive attitudes toward ET than Control OLT at both post-training and one-week follow-up. No other between-condition differences were found.
2.3.5. Credibility
At baseline, participants viewed ET as a very credible treatment and the sample as a whole generally increased in ratings of credibility across time (Table 2). Although there was a significant Time by Condition interaction, no post-hoc comparisons reached the level of statistical significance. The significant Time by Condition interaction is likely accounted for by medium effects indicating that ET OLT + MI outperformed Control OLT at post-training and both Control OLT and ET OLT at one-week follow-up (Table 3).
2.4. Secondary Outcome Analyses
2.4.1. Satisfaction
Cross-sectional HLM found a significant difference between conditions at post-training for the acceptability of the training (F (2, 41) = 5.97, p < .01). ET OLT (M = 3.94 ± 0.64) and ET OLT + MI (M = 4.15 ± 0.59) both rated the training as significantly more acceptable for learning ETs than Control OLT (M = 3.30 ± 0.85) (t (41) = 2.45, p < 0.05 and t (41) = 3.33, p < .01, respectively). ET OLT and ET OLT + MI did not significantly differ (t (41) = 0.81, p = .42). The three conditions did not differ in self-reported usability of the training courses (F (2, 41) = 0.39, p = .68), and all rated the trainings as highly usable (Ms = 5.86 – 6.13).
2.4.2. Readiness to change
There was a significant effect for Time and a significant Time by Condition interaction for the Action subscale of the RCQ (Table 2). Post-hoc comparisons revealed that both active conditions outperformed Control OLT in increasing participants’ overt efforts to learn and use ET at both post-training and one-week follow-up. From baseline to one-week follow-up, the number of ET OLT and ET OLT + MI participants in the Action stage of change approximately doubled (33.3% vs. 57.1% and 26.7% vs. 60.0%, respectively), whereas Control OLT remained virtually unchanged (18.8% vs. 20.0%).
2.4.3. Skills use
The results indicated no significant effects for Condition, Time, or their interaction on clinicians’ self-reported use of ET procedures in their clinical practice from baseline to one-week follow-up (Table 2).
3. Discussion
The overarching goal of the present study was to preliminarily evaluate methods for overcoming common barriers to disseminating ETs for anxiety disorders, including lack of training and negative attitudes toward the treatment. To that end, we conducted a pilot RCT examining the efficacy of two methods of training treatment providers in the basic principles and procedures of ETs: (1) ET OLT (an interactive, multimedia online training), and (2) ET OLT + MI (the ET OLT plus a brief MI-based intervention). Participants were randomized to one of these active training conditions or a placebo Control OLT. Overall, our results suggest that OLT can improve knowledge of and attitudes toward ETs, and that supplementing OLT with a brief MI-based intervention may further improve attitudinal barriers to implementation.
ET OLT was highly successful at increasing clinicians’ knowledge of the basic principles and procedures of ETs, with average knowledge test scores in both active conditions more than doubling after receiving the training. As predicted, the two active conditions performed comparably and both outperformed the Control OLT. These findings are consistent with two prior studies that have found computer-aided training to be an effective method of improving knowledge of ET for phobia and panic (Gega, Norman, & Marks, 2006; McDonough & Marks, 2002). In addition, both ET OLT and ET OLT + MI significantly increased clinicians’ confidence in their ability to implement ETs with clients, whereas the Control OLT did not. In contrast to hypotheses, the two active conditions did not significantly differ on self-efficacy although medium to large effects in favor of ET OLT + MI were found. Finally, learners found the ET OLT to be highly usable and helpful in learning ETs. Taken together, these findings suggest that OLT may provide a useful tool to help overcome the portion of the dissemination problem that is due to clinicians’ possessing insufficient knowledge of the basic principles and procedures of ETs for anxiety disorders.
The results also indicated that ET OLT + MI was the most effective method of addressing potential attitudinal barriers to the dissemination of ETs. In particular, ET OLT + MI significantly outperformed the Control OLT in improving attitudes toward ET, whereas ET OLT alone did not. In addition, the three groups differed significantly in terms of changes in the perceived credibility of ET across time. While pairwise comparisons were not helpful in identifying where between-condition differences existed, medium effects indicated that ET OLT + MI clinicians viewed ET as more credible than both Control OLT and ET OLT participants. These findings are consistent with research indicating the efficacy of using MI to prepare clients to make behavioral changes in a subsequent treatment (Burke, Arkowitz, & Menchola, 2003), including several treatments that incorporate MI prior to ETs for anxiety disorders (Maltby & Tolin, 2005; Simpson, Zuckoff, Page, Franklin, & Foa, 2008; Westra, 2004). The present results show that comparable effects may be achieved when preparing clinicians to learn about ETs. More generally, these results confirm and extend prior research indicating the importance of addressing potential attitudinal and psychological barriers to clinicians’ willingness to adopt evidence-based practices (Varra et al., 2008).
While these findings indicate that adding a motivation-enhancing intervention to the ET OLT may be a promising approach to training clinicians in ETs, it is important to note that the specific efficacious elements of the MI-based intervention used in the present study remain unknown. Although the primary goal of the MI-based phone calls was to encourage clinicians to discuss their beliefs, expectancies, and concerns about ETs, during these discussions many participants also asked questions about the course content, and some indicated that being able to get answers to their content-related questions was the most helpful part of the phone calls. Other participants indicated that they primarily appreciated the human contact and sense of being cared for that the MI-based phone calls provided. This feedback is consistent with research on guided self-help, which overwhelmingly supports the importance of brief contact with a therapist or coach in the administration of computerized therapies to facilitate engagement, prevent drop-out, and improve outcomes (e.g., Gellatly et al., 2007; Kenwright, Marks, Graham, Franses, & Mataix-Cols, 2005). Further research is needed to determine whether the MI strategies that were used accounted for the present findings, or whether an unstructured check-in phone call, similar to that used in many guided self-help models, would have yielded the same results.
Contrary to hypotheses, there were no differences between conditions in motivation to learn and use ET. These results likely reflect a ceiling effect, as participants generally began the study already highly motivated. The high level of baseline motivation in this sample is likely due to the fact that participants were recruited from an email listserv for another evidence-based behavioral treatment and were primarily cognitive-behavioral in orientation. Future research is needed to determine whether the predicted between-condition differences in motivation might emerge when using a less motivated sample of clinicians who are perhaps less inclined to use behavioral and evidence-based treatments. More generally, use of a convenience sample of primarily cognitive-behavioral clinicians with experience using web-based technologies (e.g., listservs) may have positively biased the findings. Future research is needed to determine if the present results are maintained when a more representative clinician sample is used.
Hypotheses relating to clinicians’ efforts to apply ET techniques in clinical practice were also not supported or only partially supported. As predicted, ET OLT and ET OLT + MI were both superior to the Control OLT in increasing clinicians’ overt efforts to learn and use the treatment, with the majority of clinicians in these conditions being in the Action stage of change by the one-week follow-up. However, the two active conditions did not differ on this outcome. Moreover, the expected between-condition differences on self-reported use of ET techniques in clinical practice were not found and none of the conditions significantly increased in their use of ET techniques across time. Several factors in the present study may have accounted for this finding. First, the one-week follow-up period was likely too short to adequately evaluate changes in clinicians’ behavior as a result of the training. Second, given that all participants were required to have minimal prior training in ETs and the ET OLT was relatively brief, the course included an advisory warning that encouraged learners to obtain further training and supervision before attempting to apply ET procedures in their clinical practice. Future research with a longer follow-up period and a more in-depth OLT is needed to adequately evaluate changes in clinicians’ use of ET. In addition, future research would benefit from including a measure of observer-rated ability to adherently and competently apply the course content.
In addition to limitations noted above, the present pilot study was underpowered, particularly in terms of the post-hoc pairwise comparisons, and did not detect many between-condition differences that otherwise were seen to have medium effect sizes. Thus, these promising pilot findings require replication in larger samples and we are currently preparing to conduct a larger, sufficiently powered RCT. Finally, although the MI-based intervention was developed in consultation with a certified MI trainer and expert, the MI-based phone calls were not assessed for adherence or competence. Thus, this intervention cannot be assumed to constitute MI, but rather to have incorporated MI-based strategies for enhancing motivation.
In sum, results of the present study support the use of OLT as a method of increasing knowledge of ETs among mental health providers, and suggest that supplementing OLT with a brief MI-based intervention may be an effective method of improving clinicians’ attitudes toward adopting these highly efficacious treatments. Further research is needed to determine whether the additional benefit associated with the MI-based intervention is enough to justify the time and resources needed to provide it or, alternatively, whether there may be more cost-effective methods of delivering it (e.g., as a computerized intervention). It is nonetheless encouraging to find that a brief intervention focused on enhancing motivation had a notable impact on decreasing potential attitudinal barriers to the dissemination of ETs.
Acknowledgments
This research, as well as the development of the online training course, was funded by a Small Business Innovation Research (SBIR) grant from the National Institute of Mental Health (#1R43MH082474-01A1) awarded to the first and second authors. We acknowledge and thank the following individuals and organization for their support and contributions to this research: Brian Knudson and the team at NogginLabs, Inc., Sharon Y. Manning, Ph.D., Marsha M. Linehan, Ph.D., Blair Beadnell, Ph.D., Kathryn E. Korslund, Ph.D., Diana Frey, Ph.D., Stacy Shaw-Welch, Ph.D., Miles Lawrence, Psy.D., Gerald Rosen, Ph.D., John Baer, Ph.D., and our advisory board of exposure therapy experts (Jonathan Abramowitz, Ph.D., Shawn Cahill, Ph.D., Richard Heimberg, Ph.D., Michael Otto, Ph.D., Peter Roy-Byrne, M.D., and Lori Zoellner, Ph.D.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramowitz J. Variants of exposure and response prevention in the treatment of obsessive-compulsive disorder: A meta-analysis. Behavior Therapy. 1996;27:583–600. [Google Scholar]
- Addis ME, Carpenter KM. Why, why, why? Reason-giving and rumination as predictors of response to activation-and insight-oriented treatment rationales. Journal of Clinical Psychology. 1999;55:881–894. doi: 10.1002/(sici)1097-4679(199907)55:7<881::aid-jclp9>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Bakker A, van Balkom AJ, Spinhoven LM, Blauuw B, van Dyck R. Follow-up on the treatment of panic disorder with and without agoraphobia: A quantitative review. Journal of Nervous and Mental Disease. 1998;186:414–419. doi: 10.1097/00005053-199807000-00005. [DOI] [PubMed] [Google Scholar]
- Becker CB, Zayfert C, Anderson E. A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy. 2004;42:277–292. doi: 10.1016/S0005-7967(03)00138-4. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, Shea MT, Keller MB. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: A 12-year prospective study. American Journal of Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buist-Bowman MA, De Graaf R, Vollebergh WAM, Alonso J, Bruffaerts R, Ormel J. Functional disability of mental disorders and comparison with physical disorders: A study among the general population of six european countries. Acta Psychiatrica Scandinavica. 2006;113:492–500. doi: 10.1111/j.1600-0447.2005.00684.x. [DOI] [PubMed] [Google Scholar]
- Burke BB, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Dimeff LA, Beadnell B, Woodcock EA, Harned MS. Can evidence-based therapies be learned in highly structured learning environments? Results from a Dialectical Behavior Therapy randomized controlled dissemination trial. Behavior Therapy. doi: 10.1016/j.beth.2010.06.004. (in press) [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Koerner K, Woodcock EA, Beadnell B, Brown MZ, Skutch JM, Paves AP, Bazinet A, Harned MS. Which training method works best? A randomized controlled trial comparing three methods of training clinicians in dialectical behavior therapy skills. Behaviour Research and Therapy. 2009;47:921–930. doi: 10.1016/j.brat.2009.07.011. [DOI] [PubMed] [Google Scholar]
- Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: A meta-analysis. Journal of Clinical Psychopharmacology. 2001;21:311–324. doi: 10.1097/00004714-200106000-00011. [DOI] [PubMed] [Google Scholar]
- Feeny NC, Hembree EA, Zoellner LA. Myths regarding exposure therapy for PTSD. Cognitive and Behavioral Practice. 2003;10:85–90. [Google Scholar]
- Feske U, Chambless DL. Cognitive behavioral versus exposure only treatment for social phobia: A meta-analysis. Behavior Therapy. 1995;26:695–720. [Google Scholar]
- Freiheit SR, Vye C, Swan R, Cady M. Cognitive-behavioral therapy for anxiety: Is dissemination working? The Behavior Therapist. 2004;27:25–32. [Google Scholar]
- Gega L, Norman IJ, Marks IM. Computer-aided vs. tutor-delivered teaching of exposure therapy for phobia/panic: Randomized controlled trial with pre-registration nursing students. International Journal of Nursing Studies. 2006;44:397–405. doi: 10.1016/j.ijnurstu.2006.02.009. [DOI] [PubMed] [Google Scholar]
- Gellatly J, Bower P, Hennessy S, Richards D, Gilbody S, Lovell K. What makes self-help interventions effective in the management of depressive symptoms? Meta-analysis and meta-regression. Psychological Medicine. 2007;37:1217–1228. doi: 10.1017/S0033291707000062. [DOI] [PubMed] [Google Scholar]
- Goisman RM, Warshaw MG, Keller MB. Psychosocial treatments prescriptions for generalized anxiety disorder, panic disorder, and social phobia, 1991–1996. American Journal of Psychiatry. 1999;156:1819–1821. doi: 10.1176/ajp.156.11.1819. [DOI] [PubMed] [Google Scholar]
- Gould RA, Buckminster S, Pollack MH, Otto MW, Yap L. Cognitive-behavioral and pharmacological treatment for social phobia: A meta-analysis. Clinical Psychology: Science and Practice. 1997;4:291–306. [Google Scholar]
- Gould RA, Otto MW, Pollack MH. A meta-analysis of treatment outcome for panic disorder. Clinical Psychology Review. 1995;15:819–844. [Google Scholar]
- Gould RA, Otto MW, Pollack MH, Yap L. Cognitive behavioral and pharmacological treatment of generalized anxiety disorder: A preliminary meta-analysis. Behavior Therapy. 1997;28:285–305. [Google Scholar]
- Hembree EA, Foa EB, Dorfan NM, Street GP, Kowalski J, Tu X. Do patients drop out prematurely from exposure therapy for PTSD? Journal of Traumatic Stress. 2003;16:555–562. doi: 10.1023/B:JOTS.0000004078.93012.7d. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hox J. Multilevel analyses: Techniques and applications. Mahwah, NJ: Lawrence Erlbaum; 2002. [Google Scholar]
- Keller MB, Yonkers KA, Warshaw MG, Pratt LA, Gollan JK, Massion AO, White K, Swartz AR, Reich J, Lavori PW. Remission and relapse in subjects with panic disorder and panic with agoraphobia: A prospective short interval naturalistic follow-up. Journal of Nervous and Mental Disease. 1994;182:290–296. doi: 10.1097/00005053-199405000-00007. [DOI] [PubMed] [Google Scholar]
- Kenwright M, Marks I, Graham C, Franses A, Mataix-Cols D. Brief scheduled phone support from a clinician to enhance computer-aided self-help for obsessive-compulsive disorder: Randomized controlled trial. Journal of Clinical Psychology. 2005;31:1499–1508. doi: 10.1002/jclp.20204. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Maltby N, Tolin DT. A brief motivational intervention for treatment-refusing OCD patients. Cognitive Behavioural Therapy. 2005;33:176–184. doi: 10.1080/16506070510043741. [DOI] [PubMed] [Google Scholar]
- Marcks BA, Weisberg RB, Keller MB. Psychiatric treatment received by primary care patients with panic disorder with and without agoraphobia. Psychiatric Services. 2009;60:823–830. doi: 10.1176/appi.ps.60.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonough M, Marks IM. Teaching medical students exposure therapy for phobia/panic – randomized, controlled comparison of face-to-face tutorial in small groups vs. solo computer instruction. Medical Education. 2002;36:412–417. doi: 10.1046/j.1365-2923.2002.01210.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York: Guilford Publications; 1991. [Google Scholar]
- Olatunji BO, Deacon BJ, Abramowitz J. The cruelest cure? Ethical issues in the implementation of exposure-based treatments. Cognitive and Behavioral Practice. 2009;16:172–80. [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. American Psychologist. 1992;47:1101–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Richard DCS, Gloster AT. Exposure therapy has a public relations problem: A dearth of litigation amid a wealth of concern. In: Richard DCS, Lauterbach DL, editors. Handbook of exposure therapies. Boston: Academic Press; 2007. pp. 1–28. [Google Scholar]
- Richard DCS, Lauterbach DL. Handbook of exposure therapies. Boston: Academic Press; 2007. [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short “readiness to change” questionnaire for use in brief, opportunistic interventions among excessive drinkers. British Journal of Addiction. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Rosen CS, Chow HC, Finney JF, Greenbaum MA, Moos RH, Sheikh JI, et al. VA practice patterns and practice guidelines for treating posttraumatic stress disorder. Journal of Traumatic Stress. 2004;17:213–222. doi: 10.1023/B:JOTS.0000029264.23878.53. [DOI] [PubMed] [Google Scholar]
- Sholomskas DE, Carroll KM. One small step for manuals: Computer-assisted training in 12 step facilitation. Journal of Studies on Alcohol. 2006;67:939–945. doi: 10.15288/jsa.2006.67.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sholomskas DE, Syracuse-Siewert G, Rounsaville BJ, Ball SA, Nuro KF, Carroll KM. We don’t train in vain: A dissemination trial of three strategies of training clinicians in cognitive-behavioral therapy. Journal of Consulting and Clinical Psychology. 2005;73:106–115. doi: 10.1037/0022-006X.73.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson HB, Zuckoff A, Page JR, Franklin ME, Foa EB. Adding motivational interviewing to exposure and ritual prevention for obsessive-compulsive disorder: An open pilot trial. Cognitive Behaviour Therapy. 2008;37:38–49. doi: 10.1080/16506070701743252. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Liversidge T, Gregg L. The acceptability and preference for the psychological treatment of PTSD. Behaviour Research and Therapy. 2006;44:1643–1656. doi: 10.1016/j.brat.2005.11.012. [DOI] [PubMed] [Google Scholar]
- van Minnen A, Hendriks L, Olff M. When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behaviour Research and Therapy. doi: 10.1016/j.brat.2009.12.003. (in press) [DOI] [PubMed] [Google Scholar]
- Varra AA, Hayes SC, Roget N, Fisher G. A randomized control trial examining the effect of acceptance and commitment training on clinician willingness to use evidence-based pharmacotherapy. Journal of Consulting and Clinical Psychology. 2008;76:449–58. doi: 10.1037/0022-006X.76.3.449. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the United States: Prevalence and conformance with evidence-based recommendations. Journal of General Internal Medicine. 2000;15:284–292. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Demler O, Kessler RC. Adequacy of treatment for serious mental illness in the United States. American Journal of Public Health. 2002;92:92–98. doi: 10.2105/ajph.92.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Weingardt KR. The role of instructional design and technology in the dissemination of empirically supported manual-based therapies. Clinical Psychology: Science and Practice. 2004;11:313–331. [Google Scholar]
- Westra H. Managing resistance in cognitive behavioural therapy: The application of motivational interviewing in mixed anxiety and depression. Cognitive Behavioural Therapy. 2004;33:161–175. doi: 10.1080/16506070410026426. [DOI] [PubMed] [Google Scholar]
- White SJ, Freedman LS. Allocation of patients to treatment groups in a controlled clinical study. British Journal of Cancer. 1978;37:849–857. doi: 10.1038/bjc.1978.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoellner LA, Feeny NC, Cochran B, Pruitt L. Treatment choice for PTSD. Behaviour Research and Therapy. 2003;41:879–886. doi: 10.1016/s0005-7967(02)00100-6. [DOI] [PubMed] [Google Scholar]