Abstract
Background
Improvements in psychosocial status are an important aspect of successful outcomes after bariatric surgery. Relatively few studies have investigated changes in psychosocial functioning at a number of points in the first few postoperative years.
Objectives
The study was undertaken to assess changes in quality of life and body image following gastric bypass surgery.
Setting
The study was performed at an academic medical center.
Methods
Two hundred men and women were enrolled in this study and completed psychometric measures of quality of life and body image prior to surgery and again 20, 40 and 92 weeks postoperatively.
Results
Participants reported significant improvements in several domains of health- and weight-related quality of life, as well as changes in body image, following surgery. These changes were correlated with percent weight loss.
Conclusions
Individuals who undergo gastric bypass surgery experience significant improvements in quality of life and body image within the first few months of surgery. These changes are, with few exceptions, maintained into the second postoperative year.
Introduction
As bariatric surgery has grown in popularity so has interest in the psychosocial issues of individuals with extreme obesity. Much of this research has focused on the psychological characteristics of candidates for bariatric surgery 1–5. Studies have consistently found higher rates of formal psychopathology among candidates for surgery, as well as elevated symptoms of psychosocial distress, such as lower self-esteem and increased depressive symptoms.
Another area of psychosocial functioning—quality of life —also has received a great deal of study. A number of investigations have reported impairments in specific domains of quality of life in persons with extreme obesity 6–8. More specifically, these studies have suggested that both health-related and weight-related quality of life are dramatically impacted by extreme obesity. Encouragingly, both health-related and weight-related quality of life appear to improve following bariatric surgery 9–14. For example, Kolotkin and colleagues recently reported that gastric bypass patients reported experience improvements in both health- and weight-related quality of life as compared to other obese persons who did not undergo bariatric surgery.11
One important area of quality of life is body image. Like quality of life, body image is a multidimensional construct. Body image dissatisfaction has been positively associated with BMI 15–16 and has been shown to improve following weight loss with behavioral, pharmacological, and surgical treatments 15, 17–20. Unfortunately, few studies of have investigated changes in multiple domains of both body image and quality of life at several points within and beyond the first year after bariatric surgery.11, 18 Thus, the present study was designed to investigate changes in quality of life and body image in the first 92 weeks following gastric bypass surgery.
Materials and Methods
Participants
Study participants were 200 individuals who underwent Roux-en-Y gastric bypass surgery at the Hospital of the University of Pennsylvania between November 2001 and June 2004. (We have previously reported on the eating behaviors of these individuals)4. The study was approved by the Institutional Review Board of the University of Pennsylvania; all participants provided informed consent prior to the study.
Measures
Approximately 4 weeks prior to surgery, participants completed a psychosocial/behavioral evaluation to assess their appropriateness for surgery 21. As part of this assessment, patients completed the Weight and Lifestyle Inventory (WALI),22 which provided information on race, employment, education, and self-reported height. Weight was confirmed with a digital scale.
Participants also completed a packet of questionnaires. They were mailed these questionnaires again approximately 20, 40, and 92 weeks following surgery and provided a postage-paid envelope to facilitate return. The packet included the following measures:
The SF-36 Health Survey (SF-36)
The SF-36 is a self-report measure used to assess health-related quality of life. Eight subscales assess separate domains of health and related functioning. Higher scores indicate more positive health-related quality of life 23.
Impact of Weight on Quality of Life
The Impact of Weight on Quality of Life is a 74-item self-report measure that is designed to assess the effect of weight in eight domains of quality of life. Participants respond to each item using a 5-point scale from 1 (“never true”) to 5 (“always true”). High scores on all of the scales, except for the comfort with food scale, reflect lower quality of life in the respective domain 24.
Body Image Quality of Life Inventory (BIQLI)
The BIQLI is a 19-item self-report inventory that is designed to measure the positive and negative impact of body image on various qualities of life. Subjects’ feelings are assessed in regard to beliefs about the self and life in general, emotional states, same and other-sex relationships, eating and exercise, grooming activities, sexual experiences, and family and work/school contexts. Participants respond to 19 items using a 7-point scale ranging from −3 (“Very Negative Effect”) to +3 (“Very Positive Effect”); 0 is labeled “No Effect” 25.
Body Shape Questionnaire
The Body Shape Questionnaire is a 34-item self-report questionnaire designed to evaluate participants’ dissatisfaction with their body shape. Each item is rated on a scale of 1 (“never”) to 6 (“always”) based on how the participant has been feeling over the last 4 weeks. A total score is obtained by calculating the sum of the responses to each item. Higher scores on this measure indicate higher levels of distress about body shape 26.
Surgical Procedure
The gastric bypass surgery was performed as either an open or laparoscopic procedure by one of two surgeons (SER and NNW). Both surgeons performed essentially the same operation. Postoperative weight loss did not differ by surgeon or by technique (open or laparoscopic). Thus, results from both surgeons were combined in all analyses.
Statistical Analysis Plan
All 200 participants completed a baseline packet and at least 1 postoperative packet. We received 198 packets at Week 20, 147 at Week 40, and 112 at Week 92. The declining response occurred despite repeated mailings, telephone calls, and email contacts. These assessment points were selected as this study was conducted in parallel with a study of behavioral treatment for obesity, the results of which are not presented here.
To assess changes over the 3 time points (Weeks 20, 40, and 92) in the mean IWQOL, SF-36, BIQOL and BSQ scores, as well as mean percent change in weight, repeated-measures analyses were conducted using a means model with the SAS Mixed procedure. An unstructured variance-covariance form in repeated measurements was assumed for each outcome. Model based mean (SE) are reported for each outcome at each time point. A significant main effect of time indicates significant changes in the outcomes across the 92 weeks. Using a Bonferroni adjustment for the six pairwise time comparisons, these mixed model analyses also were used to identify significant within mean differences between time points for each outcome (Bonferroni adjusted α =0.008). The relationships between the behavioral outcomes and gender, ethnicity, education, and marital status were examined by adding these covariates in to the mixed models. We also used correlation analyses to examine associations between percent weight loss at week 92 and changes in quality of life and body image from baseline to week 92.
Results
Participants’ Characteristics
Demographic and descriptive variables were presented in Table 1 of our previous report 4. They are briefly summarized here. The entire sample had a mean preoperative age of 42.6 ± 9.9 yrs, weight of 146.9 ± 32.3 kg, height of 167.6 ± 9.4 cm and BMI of 51.4 ± 9.0 kg/m2. One-hundred sixty four participants were women. Approximately 87% of all participants were European-American, 9% were African-American, and the remainder of other ethnic origin. Participants reported 14.0 ± 2.3 years of education. Just under half (49.5%) reported being married, 34.5% were single, and the remainder were separated, divorced, or widowed. Eighty three percent indicated that they were employed.
Changes in Weight
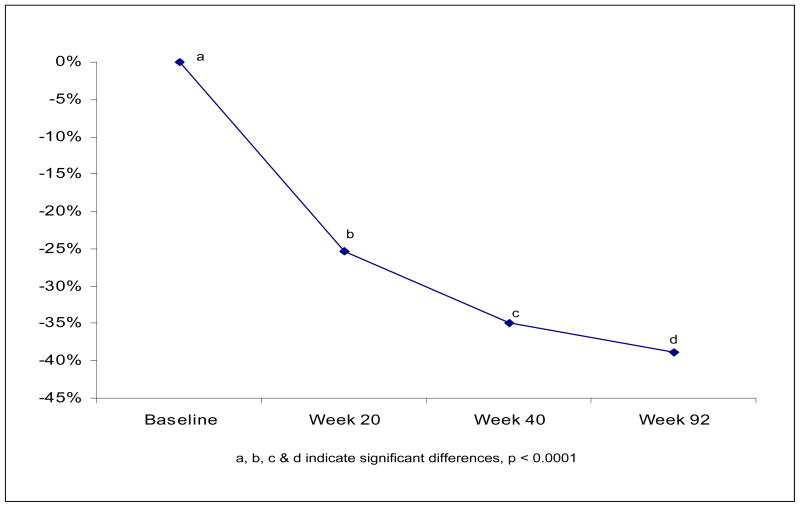
Based on the mixed model analysis that used all available data at each time point (as reported in our initial paper), mean percent weight loss significantly changed over time (See Figure 1, Overall Time F = 223, p <0.0001). Participants, on average, lost approximately 25.4% (95% CI: 24.6, 26.3) of their body weight 20 weeks after surgery; 34.9% (CI: 33.8, 36.1) at 40 weeks; and 38.8% (95% CI: 37.1, 40.6) at 92 weeks. Mean percent weight loss from baseline to each time point (Week 20, 40, 92) is significantly different from percent weight loss at each and every other time point (Overall Time F = 223, p <0.0001).
Figure 1.
Mean weight loss following gastric bypass surgery
Changes in Quality of Life
Tables 1 and 2 display the mixed model based means ± SE of the behavioral variables of interest at baseline (preoperatively) and at the three postoperative assessment points. At postoperative week 20 participants reported significant improvements in both health-related (as measured by the SF-36) and weight-related quality of life (IWQOL) (all p’s < 0.0001). These improvements remained significantly different from baseline at postoperative Week 92 (all p’s < 0.001). The exception was the SF-36 mental health subscale which was no longer significantly different from baseline at Week 92.
Table 1.
Health related quality of life as assessed by the SF-36
| Baseline | Week 20 | Week 40 | Week 92 | |
|---|---|---|---|---|
| n = 200 | n = 198 | n = 147 | N = 112 | |
| General Health | 52.3 ± 1.6a | 71.7 ± 1.5b | 72.0 ± 1.7b | 73.3 ± 1.9b |
| Physical Functioning | 34.2 ± 1.8a | 67.5 ± 1.7b | 74.0 ± 1.8c | 70.8 ± 2.2 b,c |
| Role Physical | 53.5 ± 3.0a | 81.8 ± 2.4b | 84.5 ± 2.5b | 83.1 ± 2.8b |
| Role Emotional | 74.5 ± 2.6a | 84.7 ± 2.3b | 87.8 ± 2.3b | 82.7 ± 3.0 a,b |
| Social Functioning | 65.9 ± 2.1a | 84.8 ± 1.6b | 83.6 ± 2.0b | 81.6 ± 2.5b |
| Bodily Pain | 53.7 ± 1.9a | 75.4 ± 1.8b | 75.8 ± 2.1b | 73.9 ± 2.3b |
| Vitality | 36.3 ± 1.4a | 63.2 ± 1.5b | 64.7 ± 1.7b | 61.4 ± 2.0b |
| Mental Health | 70.7 ± 1.2a | 78.2 ± 1.2b | 77.2 ± 1.4b | 74.6 ± 1.7 a,b |
| Physical Health Summary Measure | 48.7 ± 1.6a | 73.9 ± 1.6b | 76.4 ± 1.7b | 76.5 ± 1.8b |
| Mental Health Summary Measure | 62.0 ± 1.4a | 77.9 ± 1.4b | 78.4 ± 1.6b | 75.7 ± 2.0b |
Values with the same superscript letter do not differ from one another; values which do not share the same letter are significantly different from one another, based on Bonferroni adjustment, significant differences are p < .008.
Table 2.
Quality of life assessed by the IWQOL
| Baseline | Week 20 | Week 40 | Week 92 | |
|---|---|---|---|---|
| n = 200 | n = 198 | n = 147 | n = 112 | |
| Social/Interpersonal | 27.6 ± 0.7a | 20.2 ± 0.7b | 18.8 ± 0.7c | 16.8 ± 0.7d |
| Mobility | 33.4 ± 0.8a | 18.2 ± 0.7b | 15.5 ± 0.6c | 14.2 ± 0.6d |
| Activities of daily living | 24.7 ± 0.5a | 14.6 ± 0.5b | 11.7 ± 0.4c | 10.5 ± 0.4d |
| Sex | 19.9 ± 0.5a | 15.2 ± 0.5b | 14.1 ± 0.6bc | 13.1 ± 0.6c |
| Self-Esteem | 31.2 ± 0.7a | 21.9 ± 0.7b | 19.8 ± 0.7c | 18.4 ± 0.8c |
| Health | 35.6 ± 0.7a | 24.7 ± 0.5b | 23.9 ± 0.6bc | 22.9 ± 0.6c |
| Comfort with Food | 31.7 ± 0.5a | 26.5 ± 0.4b | 27.6 ± 0.5bc | 28.9 ± 0.5c |
| Work | 15.5 ± 0.5a | 12.0 ± 0.5b | 11.5 ± 0.4b | 10.9 ± 0.5b |
| Total | 214.4 ± 4.0a | 151.1 ± 3.5b | 141.7 ± 3.7c | 136.1 ± 3.4c |
Values with the same superscript letter do not differ from one another; values which do not share the same letter are significantly different from one another, based on Bonferroni adjustment, significant differences are p < .008.
Changes in Body Image
We also were interested in how quality of life and body image changed over the first 92 postoperative weeks. Patients reported significant improvement on both BIQOL and BSQ by postoperative Week 20 (both p’s <0.0001), and Week 40 and 92 body image scores remained significantly improved when compared to preoperative score (Table 3). Participants continued to experience improved BIQOL scores at week 40 that leveled off at Week 92. For BSQ, the improvement experienced at Week 20 was maintained through Week 92.
Table 3.
Changes in body image as assessed by the Body Image Quality of Life (BIQOL) and the Body Shape Questionnaire (BSQ)
| Baseline | Week 20 | Week 40 | Week 92 | |
|---|---|---|---|---|
| n = 200 | n = 198 | n = 147 | n = 112 | |
| BIQOL | −0.6 ± 0.1a | 0.7 ± 0.1b | 1.1 ± 0.1c | 1.2 ± 0.1c |
| BSQ | 121.4 ± 2.8a | 87.3 ± 2.5b | 84.2 ± 2.6b | 83.9 ± 3.0b |
Values with the same superscript letter do not differ from one another; values which do not share the same letter are significantly different from one another, based on Bonferroni adjustment, significant differences are p < .008.
Correlations of Quality of Life and Body Image
Changes on the BIQOL were significantly correlated with each of the domains on the IWQOL, with correlations ranging from r = −0.33 to r = −0.61 (p’s < 0.01). The one exception was the correlation between the BIQOL and the Comfort with Food subscale of the IWQOL (r = −0.26, p = 0.047). Changes on the BSQ also were significantly correlated with the domains on the IWQOL, ranging from r = 0.38 to r = 0.63 (p’s < 0.008). Again, the exception was the correlation with the Comfort with Food subscale (r = 0.26, p = 0.04).
Changes in body image also were correlated with several domains of health-related quality of life. Changes on the BIQOL were significantly correlated with changes on the General Health, Role Functioning, and Vitality subscales, as well as the Physical Health Summary Measure of the SF-36 (correlations ranging from r = 0.25 to r = 0.32, p’s < 0.05). Changes on the BSQ were significantly correlated with changes on the Bodily Pain, General Health, Mental Health and Vitality subscales as well as the Physical Health and Mental Health Summary Measures of the SF-36 (correlations ranging from r = −0.27 to r = −0.45, p’s < 0.05).
Correlations with Weight Loss
As shown in Table 4, percent weight loss was significantly correlated with a number of changes in quality of life and body image 92 weeks after surgery. Larger weight losses were associated with significant improvements on the general health (r = −0.27, p = 0.009) and vitality (r = −0.19, p = 0.08) subscales of the SF-36 and on the mobility (r = 0.28, p = 0.009), activities of daily living (r = 0.47, p < 0.0001) and social/interpersonal interactions subscales (r = 0.38, p = 0.0005), as well as the total score (r = 0.30, p = 0.016) on the IWQOL. Larger weight losses also were associated with significant improvements in body image quality of life, as assessed by the BIQOL (r = −0.43, p = 0.0003), but were not associated with changes in body image as assessed by the BSQ.
Table 4.
Correlations Between Percent Weight Loss and Psychosocial Changes at Postoperative Week 92
| Subscales | r | p |
|---|---|---|
| SF-36 – General Health | −0.27 | 0.009 |
| SF-36 – Physical Functioning | −0.11 | 0.30 |
| SF-36 – Role Physical | 0.07 | 0.53 |
| SF-36 – Role Emotional | 0.02 | 0.87 |
| SF-36 – Social Functioning | −0.14 | 0.21 |
| SF-36 – Bodily Pain | −0.03 | 0.77 |
| SF-36 – Vitality | −0.19 | 0.08 |
| SF-36 – Mental health | 0.05 | 0.61 |
| SF-36 – Physical Health Summary Measure | −0.09 | 0.46 |
| SF-36 – Mental Health Summary Measure | −0.09 | 0.48 |
| IWQOL – Social/Interpersonal | 0.38 | 0.0005 |
| IWQOL - Mobility | 0.28 | 0.009 |
| IWQOL – Activities of Daily Living | 0.47 | <0.0001 |
| IWQOL – Sex | 0.14 | 0.22 |
| IWQOL – Self-esteem | 0.18 | 0.10 |
| IWQOL – Health | 0.08 | 0.50 |
| IWQOL – Comfort with food | 0.06 | 0.57 |
| IWQOL – Work | 0.11 | 0.33 |
| IWQOL – Total | 0.30 | 0.02 |
| BIQOL | −0.43 | 0.0003 |
| BSQ | 0.26 | 0.03 |
Demographic Differences in Quality of Life and Body Image
We were also interested in investigating the relationship between several demographic variables and changes in quality of life and body image following bariatric surgery. We found gender differences in SF-36 mental health subscale (interaction time*gender p=0.03) and SF-36 mental health summary score (interaction time*gender p=0.02). Though both males and females had similar preoperative SF-36 mental health scores, the significant interaction term indicates that the trajectory of scores by gender differed over the postoperative period. For SF-36 mental health subscale score, males continued to improve throughout the postoperative period, whereas females improved at Week 20 but by Week 92, the females’ SF-36 score was no longer significantly different from their preoperative score [males, mean ± SE at Week 0, 20, 40, 92 respectively: 72.7 ± 2.8, 77.3 ± 2.8, 79.5 ± 3.3, 83.5 ± 3.7; Females: 70.2 ± 1.4, 78.4 ± 1.3, 76.6 ± 1.5, 72.4 ± 1.9]. The gender-specific trajectories of SF-36 mental health summary scores were similar to this with males improving at Week 20 and continuing to improve at Week 40. By contrast, females improved at Week 20 but then experienced a decline in scores throughout the rest of the postoperative period. There were no significant gender differences in any of the other quality of life or body image outcomes.
Married and non-married individuals experienced significantly different changes in SF-36 role emotional scores (interaction time*marital status p=0.04). Those not married had a mean preoperative score of 70 ± 3.7 and significantly improved at Week 20 (81 ± 3.2) and at Week 40 (87 ± 3.3) but then declined back to a similar baseline score by Week 92 (73 ± 4.1). The married subjects maintained their post-operative improvement in SF-36 role emotional throughout the entire study [mean ± SE at Weeks 0, 20, 40, 92: 79 ± 3.6, 89 ± 3.2, 89 ± 3.2, 92 ± 4.0). There were no other significant interactions between time and marital status for the additional quality of life outcomes. However, collapsed across time, married people had higher scores in SF-36 role physical, social functioning, and mental health summary score (main effect marital status p’s all <0.04).
Although the trajectories of scores based on education status were not significantly different, on average, participants with more education (some college or more as compared to those with a high school degree or less) had significantly better IWQOL self-esteem, work, and total scores, as well as higher SF-36 scores on physical functioning, role physical, social functioning, bodily pain, mental health subscale, and physical health summary score (main effect of high school education, p’s all <0.04). When considering ethnicity (Caucasian vs. Non-Caucasian), there were no significant main effects or interaction terms.
Discussion
Gastric bypass patients reported significant improvements in several domains of quality of life within the first few months of surgery. Both health-related, as well as weight-related, quality of life were well maintained through the second postoperative year and, in many cases, were associated with changes in weight. This replicates the recent findings of Kolotkin et al11 who also found that following a weight loss of 34.2% following gastric bypass surgery patients experienced significant improvements in health-related quality of life. In the present study, the baseline scores of several of the SF-36 subscales were higher than those reported by Kolotkin and colleagues. Following a somewhat larger weight loss of 38.8% (95% CI: 37.1, 40.6) at 92 weeks, we saw a similar magnitude of change in most of the subscales of the SF-36. The present study also expands research in this area by documenting that body image, which is an important aspect of quality of life for many individuals, similarly improves following gastric bypass surgery. Like the changes in quality of life, improvements in body image appear to occur relatively early in the postoperative period, which represents a unique contribution to the literature. After that point, quality of life and body image appear to remain relatively stable.
Larger weight losses were associated with improvements in several domains of quality of life. These included both the physical as well as emotional aspects of quality of life. Greater weight losses also were associated with significant improvements on the BIQOL, which assesses body image quality of life, but not with changes on the BSQ, which assesses more general weight and shape concerns. In some respects, the lack of consistent changes across the body image measures is surprising. However, it may suggest that while larger weight losses are associated with greater improvements in multiple quality of life domains (including body image quality of life), a larger weight loss may not be directly associated with greater improvements in weight and shape concerns, as assessed by the BSQ. Dixon and colleagues similarly found a discrepancy in changes in body image in persons who underwent laparoscopic adjustable gastric banding.18 They found improvements in overall body image satisfaction (as assessed by the Appearance Evaluation subscale of the Multidimensional Body-Self Relations Questionnaire) but not changes in body image investment (as assessed by the Appearance Orientation subscale of the measure).
In general and as anticipated, changes in body image were positively associated with changes in quality of life. However, these relationships were not universal and varied across the two body image measures and the subscales of the two quality of life instruments. Collectively, these results highlight the methodological challenge of selecting the most appropriate measure of body image for a given population. Many of the measures of body image, including the BSQ, were developed from the eating disorders literature. As a result, they may not be the most appropriate measures of body image for obese individuals, let alone those persons with extreme obesity20,27
The body image results of the present study also may be understood in the context of body contouring following bariatric surgery. According to the American Society of Plastic Surgery, approximately 55,000 individuals underwent body contouring surgery following massive weight loss in 2008 28. Theoretically, body image dissatisfaction has been thought to motivate cosmetic surgery 29 and studies have suggested that body image dissatisfaction predicts interest in cosmetic surgery in the future 30–31. Dissatisfaction with loose and hanging skin is also thought to play a similar motivational role in the decision to seek body contouring surgery after bariatric surgery 27. While this relationship has received relatively little empirical attention, it may help explain why larger weight losses are not directly associated with further improvements in weight and shape concerns within the first two years of bariatric surgery.
Body contouring surgery after weight loss is rarely covered by insurance. While patients often indicate they are considering plastic surgery even before they undergo their bariatric procedures, they should be reminded that these procedures will represent a significant out-of-pocket expense. Those individuals who are experiencing significant body image dissatisfaction associated with the physical changes that accompany a massive weight loss also may experience some relief from these symptoms through cognitive-behavioral psychotherapy specifically designed to address body image concerns, rather than surgical intervention.32
While men showed improvement on the SF-36 mental health summary score through postoperative Week 40 and then remained stable, women showed no further improvement on this subscale after postoperative Week 20 and actually a deterioration back to baseline by postoperative Week 92. We saw a somewhat similar pattern of results for married and non-married individuals with the emotional role subscale of the SF-36, where non-married individuals reported an initial improvement in functioning, followed by a deterioration during the postoperative period, when married individuals maintained these improvements through postoperative Week 92. Similar deteriorations in quality of life were seen in the Swedish Obese Subjects trial within the first few years of surgery 10. Our results suggest that these changes may be more likely to happen to women than men and non-married than married individuals and may underscore the emotional toll that obesity takes on some women 8,32. Nevertheless, we note that this pattern of results appeared on only selected subscales and was not uniform across the quality of life and body image measures. Furthermore, the clinical significance of these results is unclear.
While this study provides new information on the changes in quality of life and body image, it also has some limitations. Despite our best efforts, we experienced appreciable attrition over the 92 weeks of the study. Some patients were lost to follow up, while others declined further participation in the study, despite our repeated efforts through multiple modalities to retain them in the study. Attrition was not associated with any of the variables of interest in the study. Our data analytic models provide us with some degree of confidence in the validity of our findings. However, they are not a perfect substitute for greater levels of retention. Unfortunately, our experience with study retention appears to be more the rule than the exception in studies that attempt to follow patients for several years after surgery. This underscores the need for all investigators who work in the area of bariatric surgery to communicate to patients the importance of participation in research in this field, so that we can best educate other patients, providers and third-party payers on the benefits of bariatric surgery.
Future studies should continue to build on this investigation. The present study focused on one psychosocial variable under the umbrella of quality of life—body image. However, there are other areas of quality of life, such as marital and sexual functioning, that have received relatively little research attention. Given our finding on the relationship between the magnitude of weight loss and psychosocial improvements, subsequent studies should compare different procedures, which has not been done in most previous studies in the area. Finally, many of the improvements in quality of life and body image were achieved quite early in the postoperative process and well maintained through the second postoperative year. It will be interesting to see if those benefits are maintained over longer periods of time when some patients begin to regain weight.
References
- 1.Bocchieri LE, Meana M, Fisher BL. A review of psychosocial outcomes of surgery for morbid obesity. J Psychosom Res. 2002;52:155–165. doi: 10.1016/s0022-3999(01)00241-0. [DOI] [PubMed] [Google Scholar]
- 2.Herpertz S, Kielmann R, Wolf AM, Langkafel M, Senf W, Hebebrand J. Does obesity surgery improve psychosocial functioning? A systematic review. Int J Obes Relat Metab Disord. 2003;27:1300–1314. doi: 10.1038/sj.ijo.0802410. [DOI] [PubMed] [Google Scholar]
- 3.Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obes Res. 2005;13:639–648. doi: 10.1038/oby.2005.71. [DOI] [PubMed] [Google Scholar]
- 4.Sarwer DB, Wadden TA, Moore RH, et al. Preoperative eating behavior, postoperative dietary adherence and weight loss following gastric bypass surgery. Surg Obes Relat Dis. 2008;4:640–646. doi: 10.1016/j.soard.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Hout GC, van Oudheusden I, van Heck GL. Psychological profile of the morbidly obese. Obes Surg. 2004;14:479–488. doi: 10.1381/096089204323093336. [DOI] [PubMed] [Google Scholar]
- 6.Fabricatore AN, Wadden TA, Sarwer DB, Faith MS. Health-related quality of life and symptoms of depression in extremely obese persons seeking bariatric surgery. Obes Surg. 2005;15:304–309. doi: 10.1381/0960892053576578. [DOI] [PubMed] [Google Scholar]
- 7.Kolotkin RL, Crosby RD, Pendleton R, Strong M, Gress RE, Adams T. Health-related quality of life in patients seeking gastric bypass surgery vs non-treatment-seeking controls. Obes Surg. 2003;13:371–377. doi: 10.1381/096089203765887688. [DOI] [PubMed] [Google Scholar]
- 8.Kolotkin RL, Crosby RD, Gress RE, Hunt SC, Engel SG, Adams TD. Health and health-related quality of life: differences between men and women who seek gastric bypass surgery. Surg Obes Relat Dis. 2008;4:651–658. doi: 10.1016/j.soard.2008.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dymek MP, le Grange D, Neven K, Alverdy J. Quality of life and psychosocial adjustment in patients after Roux-en-Y gastric bypass: a brief report. Obes Surg. 2001;11:32–39. doi: 10.1381/096089201321454088. [DOI] [PubMed] [Google Scholar]
- 10.Karlsson J, Sjostrom L, Sullivan M. Swedish obese subjects (SOS) – an intervention study of obesity. Two-year follow-up of health-related quality of life (HRQL) and eating behavior after gastric surgery for severe obesity. Int J Obes Relat Metab Disord. 1998;22:113–126. doi: 10.1038/sj.ijo.0800553. [DOI] [PubMed] [Google Scholar]
- 11.Kolotkin RL, Crosby RD, Gress RA, Hunt SC, Adams TD. Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis. 2009;5:250–256. doi: 10.1016/j.soard.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loux TJ, Haricharan RN, Clements RH, Kolotkin RL, Bledsoe SE, Haynes B, Leath T, Harmon CM. Health-related quality of life before and after bariatric surgery in adolescents. J Ped Surg. 2008;43:1275–1279. doi: 10.1016/j.jpedsurg.2008.02.078. [DOI] [PubMed] [Google Scholar]
- 13.Malone M, Alger-Mayer S. Binge status and quality of life after gastric bypass surgery: a one-year study. Obes Res. 2004;12:473–481. doi: 10.1038/oby.2004.53. [DOI] [PubMed] [Google Scholar]
- 14.Sjostrom L, Lindroos AK, Peltonen M, et al. Swedish Obese Subjects Study Scientific Group. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–2693. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 15.Foster GD, Wadden TA, Vogt RA. Body image in obese women before, during, and after weight loss treatment. Health Psychol. 1997;16:226–229. doi: 10.1037//0278-6133.16.3.226. [DOI] [PubMed] [Google Scholar]
- 16.Sarwer DB, Wadden TA, Foster GD. Assessment of body image dissatisfaction in obese women: specificity, severity, and clinical significance. J Consult Clin Psychol. 1998;66:651–654. doi: 10.1037//0022-006x.66.4.651. [DOI] [PubMed] [Google Scholar]
- 17.Adami GF, Gandolfo P, Campostano A. Body image and body weight in obese patients. Int J Eat Disord. 1998;24:229–306. doi: 10.1002/(sici)1098-108x(199811)24:3<299::aid-eat7>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 18.Dixon JM, Dixon ME, O’Brien PE. Body image: appearance orientation and evaluation in the severely obese. Changes with weight loss. Obes Surg. 2002;12:65–71. doi: 10.1381/096089202321144612. [DOI] [PubMed] [Google Scholar]
- 19.Neven K, Dymek M, le Grange D, Maasdam H, Boogerd AC, Alverdy J. The effects of Roux-en-Y gastric bypass surgery on body image. Obes Surg. 2002;12:265–269. doi: 10.1381/096089202762552755. [DOI] [PubMed] [Google Scholar]
- 20.Sarwer DB, Thompson JK, Cash TF. Body image and obesity in adulthood. Psych Clin NA. 2005;28:69–78. doi: 10.1016/j.psc.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Wadden TA, Sarwer DB. Behavioral assessment of candidates for bariatric surgery: a patient-oriented approach. Obesity. 2006;14(Suppl 2):51S–52S. doi: 10.1038/oby.2006.283. Note: Co-publication in Surg Obes Relat Dis 2006;2:171–179. [DOI] [PubMed] [Google Scholar]
- 22.Wadden TA, Foster GD. Weight and Lifestyle Inventory (WALI) Obesity (Silver Spring) 2006;14(Suppl 2):99S–118S. doi: 10.1038/oby.2006.289. Note: Co-publication in Surg Obes Relat Dis 2006;2:180–199. [DOI] [PubMed] [Google Scholar]
- 23.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36) Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 24.Kolotkin RL, Crosby RD. Manual for the Impact of Weight on Quality of Life Measure (IWQOL and IWQOL-Lite) Durham, NC: Obesity and Quality of Life Consulting; 2009. [Google Scholar]
- 25.Cash TF, Fleming EC. The impact of body-image experiences: Development of the Body Image Quality of Life Inventory. Int J Eat Disord. 2002;31:455–460. doi: 10.1002/eat.10033. [DOI] [PubMed] [Google Scholar]
- 26.Cooper PJ, Taylor MJ, Cooper Z, Fairburn CG. The development and validation of the Body Shape Questionnaire. Int J Eat Disord. 1986;6:485–494. [Google Scholar]
- 27.Sarwer DB, Thompson JK, Mitchell JE, Rubin JP. Psychological considerations of the bariatric surgery patient undergoing body contouring surgery. Plast Reconstr Surg. 2008;121:423e–434e. doi: 10.1097/PRS.0b013e3181772aa8. [DOI] [PubMed] [Google Scholar]
- 28.American Society of Plastic Surgeons. 2009 Report of the 2008 Statistics National Clearinghouse of Plastic Surgery Statistics. Arlington Heights, IL: 2009. [Google Scholar]
- 29.Sarwer DB, Crerand CE. Body image and cosmetic medical treatments. Body Image. 2004;1:99–111. doi: 10.1016/S1740-1445(03)00003-2. [DOI] [PubMed] [Google Scholar]
- 30.Sarwer DB, Cash TF, Magee L, Williams EF, Thompson JK, Roehrig M, Tantleff-Dunn S, Kanter A, Wilfley DE, Amidon AD, Anderson DA, Romanofski M. Female college students and cosmetic surgery: An investigation of experiences, attitudes, and body image. Plastic and Reconstructive Surgery. 2005;115:931–938. doi: 10.1097/01.prs.0000153204.37065.d3. [DOI] [PubMed] [Google Scholar]
- 31.Sperry S, Thompson JK, Sarwer DB, Cash TF. Cosmetic surgery reality TV viewership: Relations with cosmetic surgery attitudes, body image, and disordered eating. Annals of Plastic Surgery. 2009;62:7–11. doi: 10.1097/SAP.0b013e31817e2cb8. [DOI] [PubMed] [Google Scholar]
- 32.Cash TF. The Body Image Workbook. 2. New Harbinger Publications; 2008. [Google Scholar]
- 33.Sarwer DB. Comment on Health and Health-Related Quality of Life: Differences between Men and Women Who Seek Gastric Bypass Surgery. Surg Obes Relat Dis. 2008;4:658–659. doi: 10.1016/j.soard.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]