Abstract
The psychopharmacology of alcohol dependence is today poised at interesting crossroads. Three major drugs Naltrexone, Disulfiram and Acamprosate have been tried and tested in various trials and have many meta-analyses each to support them. While Naltrexone may reduce craving, Acamprosate scores on cost effectiveness worldwide with Disulfiram being an alcohol deterrent drug. Studies support, refute and criticize the use of each of these drugs. Combining one or more of them is also a trend seen. The most important factor in efficacy has been the combination of psychosocial treatment with medication. Studies from the early 1970s to date have been reviewed and the findings presented in a manner useful for the busy clinician to judge the best pharmacological option in the management of alcohol dependence. The role of depot disulfiram, naltrexone, and medications like Topiramate and SSRIs under research for alcohol dependence, are also addressed.
Keywords: Alcohol Dependence, Psychopharmacology, Naltrexone, Disulfiram, Topiramate, Acamprosate, SSRIs
Introduction
Alcohol dependence is a major mental health problem in India. About five to seven per cent of the Indian population has been estimated to abuse alcohol and 10-20 million people estimated to be in need of treatment for alcohol dependence, with alcohol dependence accounting for 1.2% of the total deaths in India (Grover, Bhateja and Basu, 2007). This is a little lower than the three to five per cent estimate for major world populations (Murray and Lopez, 1997; Makela, Martikainen and Nihtila, 2005). It has also been seen that only 8-10% of total alcohol dependence patients are treated in specialty settings and less than 10% receive pharmacotherapy (Finney, Hahn and Moos, 1996). Today, with a better understanding of the basic neurobiological components of alcohol dependence, we have pharmacological agents targeted at improving drinking behavior, enhancing abstinence and preventing relapse as well as reducing the amount of alcohol people drink when they relapse (Swift, 1999; Rosenthal, 2006).
There are currently three US FDA approved medications for the relapse prevention of alcohol dependence. These are Disulfiram, Naltrexone and Acamprosate. This paper shall review the clinical experiences with these drugs, discuss the more recent trends in combination therapies and also briefly describe some new promising experimental pharmacological therapies for the treatment of alcohol dependence.
Naltrexone
Naltrexone is an opioid receptor antagonist approved by the US FDA in 1994 that reduces heavy drinking by diminishing the rewarding neurobiological effects of alcohol (Harris and Erickson, 1979; Gianoulakis, 1993; Pettinati, et al., 2006; Anton, 2008). It acts via reducing dopamine release in response to alcohol from the dopamine reward pathways in the ventral tegmental area and the nucleus accumbens (Gessa, et al., 1985; Heimer and Alheid, 1991; Benjamin, et al., 1993). It is also known to reduce the release of endogenous opioids like endorphins in response to alcohol (Herz, 1997).
Naltrexone is known to reduce craving for alcohol in both alcohol dependent patients (Monti, et al., 1999) and social drinkers (Davidson, et al., 1996; Richardson, et al., 2008). There are also a number of reviews and meta-analyses that support naltrexone as a treatment for alcohol dependence, along with 29 published randomized placebo controlled trials, some supportive and some not (Garbutt, et al., 1999; Melchior and Hoes, 1999; Kranzler, 2000; Streeton and Wheelan, 2001; Richardson, et al., 2008). Two pivotal early trials were the first to illustrate the efficacy of naltrexone in the management of alcohol dependence (Volpicelli, et al., 1992; O’Malley, et al., 1992). A recent review has reported modest favorable effects of naltrexone on heavy drinkers. In a majority of the studies reviewed, Naltrexone reduces significantly the rates of drinking in heavy drinkers by 30-60%. It reduces craving significantly though abstinence is seen usually in 25-35% cases. (Pettinati, et al., 2006). Another meta-analysis, a Cochrane collaborative, found a decrease in the rate of relapse in alcohol dependence in case of short-term studies (< 12 weeks), but the effect on increasing abstinence was small. Medium term trials (> 12 weeks) are too limited in number (eight studies) to show benefits for relapse prevention but do show increased time to the consumption of the first drink and decreased craving over time (Srisurapanont and Jarasuraisin, 2005). The dosage used in most studies is 50-100mg per day. More often than not, naltrexone was used in combination with cognitive behavioral therapy, supportive individual or group psychotherapy and relapse prevention therapy. Naltrexone alone has been shown to reduce heavy drinking rates in a smoking cessation program (King, et al., 2009) while it has also been shown to improve the cost effectiveness of cognitive behavioral therapy in alcohol dependence (Walters et al., 2009).
Naltrexone also has a favorable safety profile. It does not reduce seizure threshold nor have any fatalities been reported with naltrexone overdose. It has not been associated with pleasurable effects, does not result in tolerance and has no abuse potential (Swift, et al., 1994; Croop, Faulkner and Labriola, 1997; no recent citable studies done in the author’s knowledge). The frequency of side effects with naltrexone is low, with nausea and vomiting being the most commonly reported, followed by headache, low energy, decreased alertness, depression and anxiety. These side effects resolve in one to two days after starting naltrexone, or after a few doses, or on reducing the daily dosage (Croop, Faulkner and Labriola, 1997). Though naltrexone carries a black box warning of possible hepatotoxicity, there are no reports of hepatotoxicity with the recommended daily dosages (Yen, et al., 2006). In fact, liver enzymes which are raised often reduce with naltrexone due to decreased alcohol consumption (Berg, et al., 1996; Yen, et al., 2006).
From the clinical perspective, it is essential to note that though naltrexone has been used widely in the management of alcohol dependence there are always potential barriers to naltrexone response. Among these, the most common are medication non-adherence and heterogeneity of the alcohol dependent patient population. There are also probably different endophenotypes of alcoholism whereby some patients would respond differentially to naltrexone. We are already aware of naltrexone responders associated with response to alcohol in the laboratory (King, et al., 1997), family history of alcoholism (Jaffe, et al., 1996) and genotypes (Oslin, et al., 2003).
A long acting extended release injectable formulation of Naltrexone (encapsulated naltrexone 380mg in bio-degradable microspheres) was approved by the European FDA in 1996 for the treatment of alcohol dependence. The preparation was shown to maintain therapeutic levels for a month after injection. It also had reduced side effects and less chance of hepatic toxicity as it eliminated first pass metabolism in the liver (Garbutt, et al., 2005). Most studies with the preparation in keeping with oral naltrexone find reduction in the time to relapse in alcohol dependent patients (Johnson, et al., 2004; Kranzler, et al., 2004).
Acamprosate
Acamprosate (calcium acetylhomotaurinate) is a synthetic compound with a chemical structure similar to the amino acid neurotransmitter GABA and amino acid neuromodulator taurine. It is available as 333mg tablets with recommended dosages being two 333mg tablets thrice a day. It has been used to treat over 1.5 million patients since its introduction in 1989 and is currently available and prescribed in over 28 countries (Mason, 2001). It is hypothesized that acamprosate acts via modulation of glutamatergic hyperactivity associated with chronic alcohol induced changes (De Witte et al., 2005). Acute alcohol intake disrupts the normal balance between neuronal excitation and inhibition regulated by GABA, glutamate and other receptor systems. This results in an exaggeration of the inhibitory processes. During chronic alcohol consumption, neuroadaptation occurs via up regulation of excitatory NMDA receptors. Abrupt removal of alcohol leaves the up regulated NMDA system unopposed in a state of hyperactivity. Acamprosate may act at the regulatory sites on both ionotropic and metabotropic NMDA receptors and normalizes this hyper excitability to re-establish homeostasis (Hoffman, 2003; De Witte, 2004).
The US FDA approval of acamprosate was based on three trials that showed acamprosate’s efficacy in reducing relapse and maintaining abstinence in patients with alcohol dependence (Paille, et al., 1995; Sass, et al., 1996; Pele, et al., 1997). A number of reviews and meta-analyses have demonstrated moderate efficacy of acamprosate in the management of patients with alcohol dependence (Bouza, et al., 2004; Mason, 2005). The clinical efficacy of acamprosate was evaluated in a systematic review of published clinical trials up to 1997 with a consistent finding being 30-50% increase in non drinking days (Wilde and Wagstaff, 1997). A relatively recent meta analysis of 22 studies also reported the same effect (Mann et al., 2004). In summary, there is good evidence to support increased abstinence and decreased drinking days with acamprosate compared to placebo in the treatment of alcohol-dependent patients. The strongest effect of acamprosate is seen in recently detoxified alcohol dependents with very good data supporting its efficacy in long term studies.
In addition, all clinical trials support a favorable safety and tolerability profile of acamprosate. It has no abuse potential and the only side effect noted in all studies and on an overdose is diarrhea while hypercalcemia may be seen in chronic overdose cases only (Mason, 1996; Mann, 2004). Studies have also shown acamprosate to be a cost effective treatment (Schadlich and Brecht, 1998). However, in India, Disulfiram is cheaper than either Naltrexone or Acamprosate. Hence Disulfiram is the more cost effective treatment. Worldwide, though, Naltrexone and Acamprosate are cheaper than Disulfiram, and Disulfiram is not easily available in many nations.
Combined Naltrexone and Acamprosate Therapy
Some authors have suggested a clinical rationale for combining Naltrexone and Acamprosate therapy in the management of alcohol dependence as they act on different neurotransmitter systems (Mason, 2005; Kranzler, 2006). Clinical trials have proved that the above combination is better than acamprosate alone, though not better than naltrexone alone, especially in terms of first relapse. These were also the first studies to suggest that combined therapy is better than monotherapy in the treatment of alcohol dependence (Kiefer et al., 2003; Feeney et al., 2006). More recent researches may be underway but have not been published at this point of time in the author’s knowledge.
Disulfiram
Disulfiram, an aldehyde dehydrogenase inhibitor, has been approved by US FDA in 1951 as an aversive therapy for the management of alcohol dependence. It blocks the oxidation of ingested alcohol at the acetaldehyde stage and prevents its rapid metabolism to acetate. Thus when a disulfiram treated patient ingests even small amounts of alcohol, acetaldehyde accumulates as a result of the disulfiram-ethanol reaction and causes tachycardia, hypotension, diaphoresis, flushing, dyspnea, nausea and vomiting. These symptoms act as a deterrent to alcohol ingestion (Savas and Gullu, 1997). Disulfiram is available as 250mg tablets with the recommended dosage being 250-500mg per day. Disulfiram is often not recommended as the first line medication for newly diagnosed alcohol dependent patients but is reserved for treating patients who have previously failed one or more courses of treatment or those who are motivated to achieve complete abstinence (Fuller, et al., 1986). With the advent and emergence of Naltrexone and Acamprosate, there has been a decline in Disulfiram use with it slipping to a second line treatment in many centers for the treatment of alcohol dependence. Safety concerns may also be the reason for this as many alcoholic patients try to consume alcohol even when on Disulfiram and hence may cause themselves unnecessary harm.
Several reviews support the efficacy of supervised use of Disulfiram in the management of alcohol dependence (Banys, 1988; Brewer, 1995; Suh et al., 2006). This background alone ought to make everyone in the world of alcoholism treatment aware of disulfiram’s potential especially for the large and often demoralizing number of patients that do not respond to other treatments. There is no doubt that supervised disulfiram therapy is an integral component of any alcohol treatment program (Chick and Brewer, 1999). There are also a large number of limitations with respect to disulfiram research. In a review of studies published between 1948 and 1971 it was seen that among 42 studies only one had an adequate research design. The limitations still hold, with no randomized double blind trials being ever conducted on Disulfiram in this reviewer’s knowledge. Lack of double blinded controlled and randomized clinical trials with disulfiram is another hindrance. The reason for this is that awareness that the patient is on disulfiram is an essential for the action of disulfiram in order to enhance its efficacy and hence most studies are open ones (Lundwall and Baekeland, 1971; Hughes and Cook, 1997; Fuller and Gordis, 2004). It has been noted that disulfiram is most effective when supervised and used in alcoholism with the help of a close family member (Brewer, 2005).
Disulfiram is an old drug, long out of patent protection. It is thus cheap and marketed by manufacturers of the generic drug who do little advertising and research. There is also a ready availability of funding for naltrexone and acamprosate research which means that researchers with projects on these drugs are more likely to study acamprosate or naltrexone than disulfiram. Fears of disulfiram hepatotoxicity are often exaggerated. There is about one case in 25000 patient years (Poulsen, 1992; Brewer and Hardt, 1999; Martin and Beresford, 2007). Death from disulfiram is also very rare (Brewer, 2005). Disulfiram can be readily prescribed with Acamprosate and Naltrexone and is shown to improve the efficacy of Acamprosate (Beeson et al., 1998; Suh et al., 2006). There have been cases where disulfiram has been continued safely for over 15 years (Brewer, 1993; Garbutt, 2009).
A long acting depot preparation of Disulfiram in the form of a Disulfiram implant is also available. It was introduced in the 1950s and is still used in some parts of the world. In various studies, it shows a similar pharmacological and clinical profile like oral Disulfiram (Johnsen and Marland, 1991; 1992). No current research evidence is available on this preparation.
Comparison of the Three Drugs
There are only a few studies that provide a head on between the above three drugs. Naltrexone has been proven superior to Acamprosate in one of the earliest studies comparing the two drugs (Rubio et al., 2001). An Indian study has shown Naltrexone to be superior to Disulfiram (Naidu et al., 2000); while a retrospective chart review has shown acamprosate to be superior to naltrexone (Basu et al., 2005). No major recent studies add to this literature and future research in this area is warranted.
The author of this article has been involved in recent work on Disulfiram. In similar studies the author and others have shown disulfiram to be superior to naltrexone, acamprosate and topiramate in separate studies. They, along with others, have also shown disulfiram to be superior to naltrexone in the management of adolescents with alcohol dependence. (De Sousa and De Sousa, 2004; De Sousa and De Sousa, 2005; Petrakis et al., 2006; Pettinati et al., 2008; Laaksonen et al., 2008; De Sousa, De Sousa and Kapoor, 2008; De Sousa and De Sousa, 2008). Further studies on similar lines are already in progress.
Topiramate
Though not US FDA-approved, there are various reports of topiramate being effective in the management of alcohol dependence. It is a drug that has been used successfully in epilepsy and migraine. It is postulated to be effective in the management of alcohol dependence as it reduces dopamine release after alcohol consumption due to its ability to enhance GABA mediated inhibition through non benzodiazepine receptors (White et al., 2000; Johnson et al., 2003). There is also a possible glutamate antagonism mechanism at the alpha amino 3 hydroxy 5 methyl 4 isoxazole propionic acid receptors (Skradiski and White, 2000). Various randomized double blind controlled trials have reported the efficacy of topiramate in reducing the percentage of drinking days and in maintaining abstinence (Johnson et al., 2003; Rosenthal, 2006; Garbutt, 2006). Topiramate has been used in doses of 100-250mg per day. The drug in most studies has been used alone with conflicting results. While some studies suggest a moderate efficacy others regard it as ineffective. No specific indications, contra-indications or specific sub groups of alcohol dependent patients that may respond to Topiramate have yet been delineated.
Future Probable Pharmacological Agents
Several other classes of drugs, not yet currently approved, are under active study for use in alcohol dependence. Selective serotonin reuptake inhibitors (SSRIs) that augment brain serotenergic function have shown to reduce alcohol consumption in animal studies. Findings with alcohol dependent patients are inconsistent but these drugs are the main stay in the management of depression with alcohol dependence. Type A alcoholics (late onset, less severe dependence, less psychopathology) show a favorable response to these drugs. The two drugs that have been studied so far are Sertraline and Fluoxetine in one study each (Kranzler et al., 1996; Anton and Swift, 2003; Nunes and Levin, 2004; Dundon et al., 2004). More recent work has not been reported.
A few studies have also studied the role of 5HT-3 receptor antagonist Ondansetron with very modest results in the management of alcohol dependence (Johnson, et al., 2000; no more recent work available).
Acute alcohol consumption increases dopamine release from the nucleus accumbens while chronic alcohol consumption decreases mesostriatal dopamine activity in rodents and decreases dopamine and its metabolites in alcoholics (DiChiara and Imperato, 1985; Fulton et al., 1995). Medications that affect dopamine may thus have a potential role in alcohol dependence. Some studies have shown that the dopamine receptor antagonist, haloperidol, reduces the stimulating and euphorigenic effects of alcohol in social drinkers and reduces craving in pretreated alcoholics (Modell et al., 1993). Studies have shown mild to modest results in a similar manner with the use of antipsychotics like Clozapine, Olanzapine, Fluphenthixol and Amisulpride in separate settings (Drake et al., 2000; Wisebeck et al., 2001; Marra et al., 2002; Guardia et al., 2004).
Pharmacotherapy for alcohol dependence is always delivered in a psychosocial context that may affect the outcome of the treatment. The rigorous study of different psychotherapeutic treatments for alcohol dependence has shown several distinct approaches to be effective. Many psychosocial interventions for alcohol dependence, including Alcoholics Anonymous, can be integrated successfully with pharmacotherapy. Psychosocial interventions, ranging from brief medical management to more intensive individualized psychotherapies, have all been shown to produce positive outcomes in certain studies, depending on the specific medication and the study context. Particularly successful combinations may include the use of behavioral marital therapy plus a disulfiram contract for patients taking that medication, and the combination of naltrexone or acamprosate with cognitive-behavioral therapy or psychosocial support. Ongoing research examining the optimal combinations of medications with different psychosocial treatments for alcohol dependence may further inform the field (Weiss and Kueppenbender, 2006).
Figure 1.
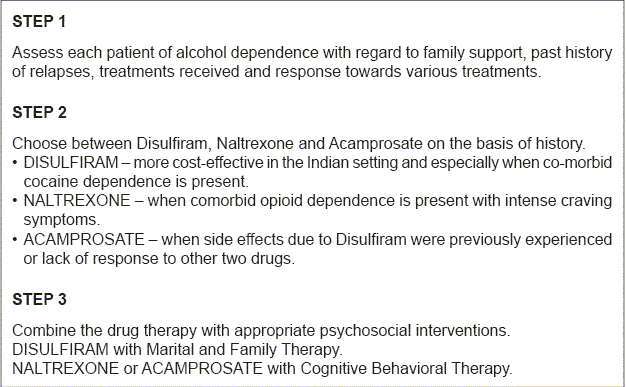
Flowchart of the paper
Concluding Remarks
Today the pharmacology scenario with respect to alcohol dependence is more promising than ever. The molecules used regularly in the management of alcohol dependence have been widely researched such that the sharp clinician can ascertain their use for specific patient populations when needed. Further studies involving comparisons of various different drugs across various settings and subsets of the alcoholic population are needed to clear any lacunae that remain.
Thumb rule for clinicians
It is important for clinicians treating alcohol dependence to note the following:
Naltrexone and Acamprosate, though effective, only reduce craving and do not deter the patient from taking alcohol. He may still drink while on these drugs with no untoward effects.
Disulfiram, though underused, is cheaper than the above two drugs but very effective as an alcohol deterrent as fear of a disulfiram ethanol reaction forces the patient to be off alcohol when on the drug.
Combination therapy of disulfiram with any of the other drugs thereby acting on different neurobiological systems may be optimal for the effective management of alcohol dependence.
The use of psycho-education about disulfiram and its actions is very essential to get the best effects out of the medication.
Take home message
The pharmacotherapy of alcohol dependence is keenly poised today. We have different drugs (Naltrexone, Disulfiram and Acamprosate) with varying mechanisms of action aimed at different populations which, when used judiciously, can bring about good results along with psychosocial interventions in the management of alcohol dependence. Newer agents like Topiramate and SSRIs are being investigated for their role in alcohol dependence.
Conflict of interest
None declared.
No funding, speaker fees or research grant received.
Declaration
This article is my original unpublished work and has not been sent for publication to any other journal.
Questions That This Paper Raises
Which is the best drug for the long-term management of alcohol dependence?
Is one drug enough or do we need multiple drug therapy in the long-term management of alcohol dependence?
Does Disulfiram have a role in the modern day pharmacotherapy of alcohol dependence?
Do newer drugs other than those approved by US FDA play a role in the management of alcohol dependence?
Do the findings from studies worldwide hold good when considering Indian patients with alcohol dependence?
About the Author

Dr. Avinash De Sousa is a consultant psychiatrist and psychotherapist with a private practice in Mumbai. He is an avid reader and has over 50 publications in national and international journals. His main areas of interest are alcohol dependence, child and adolescent psychiatry, mental retardation, autism and developmental disabilities. He is also the academic director of the Institute of Psychotherapy Training and Management, Mumbai. He actively teaches psychiatry, child psychology and psychotherapy at over 18 institutions as a visiting faculty.
Footnotes
CITATION: De Sousa A., (2010), The Pharmacotherapy of Alcohol Dependence: A State of the Art Review. In: Psychopharmacology Today: Some Issues (A.R. Singh and S.A. Singh eds.), MSM, 8, Jan - Dec 2010, p69-82.
References
- 1.Anton R.F. Naltrexone for the management of alcohol dependence. New Eng J Med. 2008;359(7):p715–721. doi: 10.1056/NEJMct0801733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anton R.F, Swift R.M. Current pharmacotherapies of alcoholism: a US perspective. Am J Addiction. 2003;12(suppl 1):pS53–S68. doi: 10.1111/j.1521-0391.2003.tb00496.x. [DOI] [PubMed] [Google Scholar]
- 3.Banys P. The clinical use of disulfiram: a review. J Psychoactive Drugs. 1988;20:p243–260. doi: 10.1080/02791072.1988.10472495. [DOI] [PubMed] [Google Scholar]
- 4.Basu D, Jhirwal O.P, Mattoo S.K. Clinical characterization of the use of acamprosate and naltrexone: data from an addiction center in India. Am J Addiction. 2005;14:p381–395. doi: 10.1080/10550490591006933. [DOI] [PubMed] [Google Scholar]
- 5.Beeson J, Aeby F, Kasas A, Lehert P, Potgieter A. Combined efficacy of disulfiram and acamprosate in the treatment of alcoholism: a controlled study. Alcohol Clin Exp Res. 1998;22:p573–579. doi: 10.1111/j.1530-0277.1998.tb04295.x. [DOI] [PubMed] [Google Scholar]
- 6.Benjamin D, Grant E.R, Pohorecky L.A. Naltrexone reverses ethanol induced dopamine release in the nucleus accumbens in awake freely moving rats. Brain Res. 1991;621:p137–140. doi: 10.1016/0006-8993(93)90309-b. [DOI] [PubMed] [Google Scholar]
- 7.Berg B.J, Pettinati H.M, Volpicelli J.R. A risk benefit analysis of naltrexone in the treatment of alcohol dependence. Drug Saf. 1996;15(4):p274–282. doi: 10.2165/00002018-199615040-00005. [DOI] [PubMed] [Google Scholar]
- 8.Bouza C, Angeles M, Munoz A, Amate J.M. Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review. Addiction. 2004;99:p811–828. doi: 10.1111/j.1360-0443.2004.00763.x. [DOI] [PubMed] [Google Scholar]
- 9.Brewer C. Long term high dose disulfiram treatment of alcohol abuse. Br J Psychiatry. 1993;163:p687–689. doi: 10.1192/bjp.163.5.687. [DOI] [PubMed] [Google Scholar]
- 10.Brewer C. Recent developments in disulfiram treatment. Alcohol Alcohol. 1995;28:p385–393. [PubMed] [Google Scholar]
- 11.Brewer C, Hardt F. Preventing disulfiram hepatitis in alcohol abusers: inappropriate guidelines and the significance of nickel allergy. Addict Biol. 1999;4:p303–308. doi: 10.1080/13556219971506. [DOI] [PubMed] [Google Scholar]
- 12.Brewer C. Supervised disulfiram is more effective in alcoholism than naltrexone or acamprosate or even psychotherapy: how it works and why it matters. Addiction. 2005;17(4):p222–233. [Google Scholar]
- 13.Chick J, Brewer C. National differences in disulfiram prescribing. Psych Bull. 1999;23:p335–339. [Google Scholar]
- 14.Croop R.S, Faulkner E.B, Labriola D.F. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. The Naltrexone Usage Study Group. Arch Gen Psychiatry. 1997;54(12):p1130–1135. doi: 10.1001/archpsyc.1997.01830240090013. [DOI] [PubMed] [Google Scholar]
- 15.Davidson D, Swift R, Fitz E. Naltrexone increases the latency to drink alcohol in social drinkers. Alcohol Clin Exp Res. 1996;20:p732–739. doi: 10.1111/j.1530-0277.1996.tb01679.x. [DOI] [PubMed] [Google Scholar]
- 16.De Witte P. Imbalance between neuroexcitatory and neuroinhibitory amino acids causes craving for ethanol. Addict Behav. 2004;29:p1325–1339. doi: 10.1016/j.addbeh.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 17.De Witte P, Littleton J, De Witte P, Parot P, Koob G. Neuroprotective and abstinence promoting effects of Acamprosate: elucidating the mechanism of action. CNS Drugs. 2005;19(6):p517–537. doi: 10.2165/00023210-200519060-00004. [DOI] [PubMed] [Google Scholar]
- 18.DeSousa A, DeSousa A. Naltrexone versus disulfiram: a one year follow up of alcohol dependence treatment. Alcohol Alcohol. 2004;39:p528–531. [Google Scholar]
- 19.DeSousa A, DeSousa A. An open randomized study comparing disulfiram and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2005;40:p545–548. doi: 10.1093/alcalc/agh187. [DOI] [PubMed] [Google Scholar]
- 20.DeSousa A, DeSousa J.A, Kapoor H. An open randomized trial comparing disulfiram and topiramate in the treatment of alcohol dependence. J Subs Abuse Treatment. 2008;34:p460–463. doi: 10.1016/j.jsat.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 21.DeSousa A. An open randomized trial comparing disulfiram and naltrexone in the management of adolescents with alcohol dependence. J Substance Use. 2008;13(6):p382–388. [Google Scholar]
- 22.Di Chiara G, Imperato A. Ethanol preferentially stimulates dopamine release in the nucleus accumbens of freely moving rats. Eur J Pharmacol. 1985;115:p131–132. doi: 10.1016/0014-2999(85)90598-9. [DOI] [PubMed] [Google Scholar]
- 23.Drake R.E, Xie H, McHugo G.J, Green A.I. The effects of Clozapine on alcohol and drug use disorders among patients with schizophrenia. Schizophr Bull. 2000;26:p441–449. doi: 10.1093/oxfordjournals.schbul.a033464. [DOI] [PubMed] [Google Scholar]
- 24.Dundon W, Dundon W, Lynch K.G, Pettinati H.M, Lipkin C. Treatment outcomes in type A and B alcohol dependence 6 months after serotenergic pharmacotherapy. Alcohol Clin Exp Res. 2004;28:p1065–1073. doi: 10.1097/01.alc.0000130974.50563.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feeney G.F, Connor J.P, Young R.M, Tucker J, McPherson A. Combined naltrexone and acamprosate with cognitive behavioral therapy is superior to medication alone for alcohol abstinence: a single Centre’s experience with pharmacotherapy. Alcohol Alcohol. 2006;41:p321–327. doi: 10.1093/alcalc/agl007. [DOI] [PubMed] [Google Scholar]
- 26.Finney J.W, Hahn A.C, Moos R.H. The effectiveness of inpatient and outpatient treatment for alcohol abuse: the need to focus on the mediators and moderators of setting effects. Addiction. 1996;91:p1773–1796. [PubMed] [Google Scholar]
- 27.Fulton M.K, Kramer G, Moeller F.G, Chae Y, Isbell P.G, Petty F. Low plasma homovanillic acid levels in recently abstinent alcoholic men. Am J Psychiatry. 1995;152:p1819–1820. doi: 10.1176/ajp.152.12.1819. [DOI] [PubMed] [Google Scholar]
- 28.Fuller R.K, Branchey L, Brightwell D.R, Derman R.M, Emrick C.D, Iber F.L, et al. Disulfiram treatment of alcoholism: a veterans administration cooperative study. JAMA. 1986;256:p1449–1455. [PubMed] [Google Scholar]
- 29.Fuller R.K, Gordis E. Does disulfiram have a role in alcoholism treatment today? Addiction. 2004;99:p21–24. doi: 10.1111/j.1360-0443.2004.00597.x. [DOI] [PubMed] [Google Scholar]
- 30.Garbutt J.C, West S.L, Carrey T.S, Lohr K.N, Crews F.T. Pharmacological treatment of alcohol dependence: a review of the evidence. JAMA. 1999;281(14):p1318–1325. doi: 10.1001/jama.281.14.1318. [DOI] [PubMed] [Google Scholar]
- 31.Garbutt J.C, Kranzler H.R, O’Malley S.S, Gastfriend D.R, Pettinati H.M, Silverman B.L. Efficacy and tolerability of long acting injectable naltrexone for alcohol dependence: a randomized controlled trial. JAMA. 2005;293:p1617–1625. doi: 10.1001/jama.293.13.1617. [DOI] [PubMed] [Google Scholar]
- 32.Garbutt J.C. Emerging pharmacological treatments for the management of alcohol dependence. J Clin Psychiatry. 2006;67(suppl 14):p35–40. [Google Scholar]
- 33.Garbutt J.C. The state of pharmacotherapy for the treatment of alcohol dependence. J Subs Abuse Treat. 2009;36(1):pS15–23. [PubMed] [Google Scholar]
- 34.Gessa G.L, Muntoni F, Collu M, Vargiu L, Meeru G. Low doses of ethanol activate dopaminergic neurons in the ventral tegmental area. Brain Res. 1985;348:p201–203. doi: 10.1016/0006-8993(85)90381-6. [DOI] [PubMed] [Google Scholar]
- 35.Gianoulakis C. Endogenous opioids and excess alcohol consumption. J Psychiatry Neurosci. 1993;18(4):p148–156. [PMC free article] [PubMed] [Google Scholar]
- 36.Grover S, Bhateja G, Basu D. Pharmacoprophylaxis of alcohol dependence: review and update Part I: Pharmacology. Indian J Psychiatry. 2007;49:p19–25. doi: 10.4103/0019-5545.31514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guardia J, Segura L, Gonzalvo B, Iglesias L, Roncero C, Cardus M, et al. A double blind placebo controlled study of olanzapine in the treatment of alcohol dependence disorder. Alcohol Clin Exp Res. 2004;28:p736–745. doi: 10.1097/01.alc.0000125352.06688.f7. [DOI] [PubMed] [Google Scholar]
- 38.Harris R.A, Erickson C.K. Alteration of ethanol effects by opiate antagonists. Curr Alcohol. 1979;5:p17–28. [PubMed] [Google Scholar]
- 39.Heimer L, Alheid G.F. Piecing together the puzzle of basal forebrain anatomy. Adv Exp Med Biol. 1991;295:p1–42. doi: 10.1007/978-1-4757-0145-6_1. [DOI] [PubMed] [Google Scholar]
- 40.Herz A. Endogenous opioid systems and alcohol addiction. Psychopharmacology. 1997;129 :p99–111. doi: 10.1007/s002130050169. [DOI] [PubMed] [Google Scholar]
- 41.Hoffman P.L. NMDA receptors in alcoholism. Int Rev Neurobiol. 2003;56:p35–82. doi: 10.1016/s0074-7742(03)56002-0. [DOI] [PubMed] [Google Scholar]
- 42.Hughes J.C, Cook C.C. The efficacy of disulfiram: a review of outcome studies. Addiction. 1997;92:p381–395. [PubMed] [Google Scholar]
- 43.Jaffe A.J, Rounsaville B, Chang G, Schottenfield R.S, Mayer R.E, O’Malley S.S. Naltrexone, relapse prevention and supportive therapy with alcoholics: an analysis of patient treatment matching. J Consult Clin Psychol. 1996;64(5):p1044–1053. doi: 10.1037//0022-006x.64.5.1044. [DOI] [PubMed] [Google Scholar]
- 44.Johnsen J, Merland J. Disulfiram implant: a double blind placebo controlled follow up on treatment outcome. Alcohol Clin Exp Res. 1991;15(3):p532–536. doi: 10.1111/j.1530-0277.1991.tb00555.x. [DOI] [PubMed] [Google Scholar]
- 45.Johnsen J, Merland J. Depot preparations of disulfiram: experimental and clinical results. Acta Psych Scand. 1992;86:p27–30. doi: 10.1111/j.1600-0447.1992.tb03311.x. [DOI] [PubMed] [Google Scholar]
- 46.Johnson B.A, Roache J.D, Javors M.A, DiClemente C.C, Cloninger R.C, Prihoda T.J, et al. Ondansetron for the reduction of drinking among biologically predisposed alcoholic patients: a randomized controlled trial. JAMA. 2000;284:p963–971. doi: 10.1001/jama.284.8.963. [DOI] [PubMed] [Google Scholar]
- 47.Johnson B.A, Ait-Daoud N, Bowden C.L, DeClemente C.C, Roache J.D, Lawson K. Oral topiramate in the treatment of alcohol dependence: a randomized controlled trial. Lancet. 2003;361:p1677–1685. doi: 10.1016/S0140-6736(03)13370-3. [DOI] [PubMed] [Google Scholar]
- 48.Johnson B.A, Ait-Daoud N, Aubin H.J, Van Den Brink W, Guzetta R, Loewy J. A pilot evaluation of the safety and tolerability of long acting injectable naltrexone in patients with alcohol dependence. Alcohol Clin Exp Res. 2004;28:p1356–1361. doi: 10.1097/01.alc.0000139823.30096.52. [DOI] [PubMed] [Google Scholar]
- 49.Kiefer F, Jahn H, Tarnaske T, Helwig H, Briken P, Holzbach R, et al. Comparing and combining naltrexone and acamprosate in the relapse prevention of alcoholism: a double blind placebo controlled trial. Arch Gen Psychiatry. 2003;60:p92–99. doi: 10.1001/archpsyc.60.1.92. [DOI] [PubMed] [Google Scholar]
- 50.King A.C, Volpicelli J.R, Frazer A, O’Brien C.P. Effect of naltrexone on subjective alcohol response in subjects with high and low risk for future alcohol dependence. Psychopharmacology. 1997;129:p15–22. doi: 10.1007/s002130050156. [DOI] [PubMed] [Google Scholar]
- 51.King A.C, Cao D, Vanier C, Wilcox T. Naltrexone decreases heavy drinking rates in smoking cessation treatment: an exploratory study. Alcohol Clin Exp Res. 2009;33(6):p1044–1050. doi: 10.1111/j.1530-0277.2009.00925.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kranzler H.R, Burleson J.A, Korner P, Babor T.F. Fluoxetine treatment seems to reduce the beneficial effects of cognitive behavioral therapy in type B alcoholics. Alcohol Clin Exp Res. 1996;20:p1534–1541. doi: 10.1111/j.1530-0277.1996.tb01696.x. [DOI] [PubMed] [Google Scholar]
- 53.Kranzler H.R. Pharmacotherapy of alcoholism: gaps in knowledge and opportunities for research. Alcohol Alcohol. 2000;35(6):p537–547. doi: 10.1093/alcalc/35.6.537. [DOI] [PubMed] [Google Scholar]
- 54.Kranzler H.R, Wesson D.R, Billot L. Drug Abuse Science Naltrexone Depot Study Group (2004), Naltrexone depot for the treatment of alcohol dependence: a multicenter randomized placebo controlled trial. Alcohol Clin Exp Res. 28:p1051–1059. doi: 10.1097/01.alc.0000130804.08397.29. [DOI] [PubMed] [Google Scholar]
- 55.Kranzler H.R. Evidence based treatments for alcohol dependence: new results and new questions. JAMA. 2006;295:p2075–2076. doi: 10.1001/jama.295.17.2075. [DOI] [PubMed] [Google Scholar]
- 56.Laaksonen E, Koski-Jannes A, Salaspuro M, Ahtinen H, Alho H. A randomized multicentre open labeled trial comparing disulfiram, naltrexone and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2008;43(1):p53–61. doi: 10.1093/alcalc/agm136. [DOI] [PubMed] [Google Scholar]
- 57.Lundwall L, Baekeland F. Disulfiram treatment of alcoholism. J Nerv Ment Dis. 1971;153(6):p381–394. doi: 10.1097/00005053-197112000-00002. [DOI] [PubMed] [Google Scholar]
- 58.Makela P, Martikainen P, Nihtila E. Temporal variations in deaths related to alcohol intoxication and drinking. Int J Epidemiol. 2005;34(4):p765–771. doi: 10.1093/ije/dyi025. [DOI] [PubMed] [Google Scholar]
- 59.Mann K. Pharmacotherapy of alcohol dependence: a review of the clinical data. CNS Drugs. 2004;18(8):p485–504. doi: 10.2165/00023210-200418080-00002. [DOI] [PubMed] [Google Scholar]
- 60.Mann K, Lehert P, Morgan M.Y. The efficacy of acamprosate in the maintenance of abstinence in alcohol dependent individuals: results of a meta-analysis. Alcohol Clin Exp Res. 2004;28:p51–63. doi: 10.1097/01.ALC.0000108656.81563.05. [DOI] [PubMed] [Google Scholar]
- 61.Marra D, Warot D, Berlin I, Hispard E, Notides C, Tilkete S, et al. Amisulpride does not prevent relapse in primary alcohol dependence: results of a pilot randomized placebo controlled trial. Alcohol Clin Exp Res. 2002;26:p1545–1552. doi: 10.1097/01.ALC.0000034666.69418.47. [DOI] [PubMed] [Google Scholar]
- 62.Martin B, Beresford T.P. Disulfiram in context, structure and safety. J Clin Psychopharmacol. 2007;27(4):p415–417. doi: 10.1097/01.jcp.0000280312.58495.35. [DOI] [PubMed] [Google Scholar]
- 63.Mason B.J. Dosing issues in the pharmacotherapy of alcoholism. Alcohol Clin Exp Res. 1996;20(Suppl 7):p10A–16A. doi: 10.1111/j.1530-0277.1996.tb01184.x. [DOI] [PubMed] [Google Scholar]
- 64.Mason B.J. Treatment of alcohol dependent out patients with Acamprosate: a clinical review. J Clin Psychiatry. 2001;62(suppl 20):p42–48. [PubMed] [Google Scholar]
- 65.Mason B.J. Acamprosate and Naltrexone treatment for alcohol dependence: an evidence based risk benefits assessment. Eur Neuropsychopharmacol. 2003;13(6):p469–475. doi: 10.1016/j.euroneuro.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 66.Mason B.J. Acamprosate in the treatment of alcohol dependence. Exp Opin Pharmacother. 2005;6(12):p2103–2115. doi: 10.1517/14656566.6.12.2103. [DOI] [PubMed] [Google Scholar]
- 67.Mason B.J. Rationale for combining acamprosate and naltrexone in the treatment of alcohol dependence. J Stud Alcohol. 2005;(Suppl):p148–156. doi: 10.15288/jsas.2005.s15.148. [DOI] [PubMed] [Google Scholar]
- 68.Melchior J.A, Hoes J.M. Relapse prevention in alcoholics: a review of acamprosate versus naltrexone. Clin Drug Invest. 1999;17:p211–216. [Google Scholar]
- 69.Modell J.G, Mountz J.M, Glaser F.B, Lee J.Y. Effect of Haloperidol on measures of craving and impaired control in alcoholic subjects. Alcohol Clin Exp Res. 1993;17(2):p234–240. doi: 10.1111/j.1530-0277.1993.tb00755.x. [DOI] [PubMed] [Google Scholar]
- 70.Monti P.M, Rosenhow D.J, Hutchison K.L, Swift R.M, Mueller T.I, Colby S.M, et al. Naltrexone’s effect on cue elicited carving among alcoholics in treatment. Alcohol Clin Exp Res. 1999;23:p1386–1394. [PubMed] [Google Scholar]
- 71.Murray C.J, Lopez A.D. Global mortality, disability and contribution of risk factors. Lancet. 1997;349:p1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 72.Naidu H, Thacore A.S, Koshy M.K. Naltrexone in alcohol dependence: a comparison with disulfiram. Ind J Psychiatry. 2000;41:p43–44. [Google Scholar]
- 73.Nunes E.V, Levin F.R. Treatment of depression in patients with alcohol and other forms of drug dependence. JAMA. 2004;291:p1887–1896. doi: 10.1001/jama.291.15.1887. [DOI] [PubMed] [Google Scholar]
- 74.Oslin D.W, Berrettini W, Kranzler H.R, Pettinati H.M, Gelernter J, Volpicelli J.R, et al. A functional polymorphism of the mu opioid receptor gene is associated with naltrexone response in alcohol dependent patients. Neuropsychopharmacology. 2003;28:p1546–1552. doi: 10.1038/sj.npp.1300219. [DOI] [PubMed] [Google Scholar]
- 75.O’Malley S.S, Jaffe A.J, Chang G, Schottenfield R.S, Mayer R.E. Naltrexone and coping skills therapy for alcohol dependence: a controlled study. Arch Gen Psychiatry. 1992;49:p881–887. doi: 10.1001/archpsyc.1992.01820110045007. [DOI] [PubMed] [Google Scholar]
- 76.Paille F.M, Guelfi J.D, Perkins A.C, Royer R.J, Steru L, Parot P. Double blind randomized multicentre trial of acamprosate in maintaining abstinence from alcohol. Alcohol Alcohol. 1995;30:p239–247. [PubMed] [Google Scholar]
- 77.Pelc I, Verbanck P, Le Bon O, Gavrilovic M, Lion K, Lehert P. Efficacy and safety of acamprosate in the treatment of detoxified alcohol dependent patients: a 90 day placebo controlled dose finding study. Br J Psychiatry. 1997;171:p73–77. doi: 10.1192/bjp.171.1.73. [DOI] [PubMed] [Google Scholar]
- 78.Petrakis I.L, Poling J, Levinson C, Nich C, Caroll K, Ralevski E, et al. Naltrexone and disulfiram in patients with alcohol dependence and comorbid post traumatic stress disorder. Biol Psychiatry. 2006;60(7):p777–783. doi: 10.1016/j.biopsych.2006.03.074. [DOI] [PubMed] [Google Scholar]
- 79.Pettinati H.M, O’Brien C.P, Rabinowitz A.R, Wortman S.M, Oslin D.W, Kampman K.M, et al. The status of Naltrexone in the treatment of alcohol dependence: specific effects on heavy drinking. J Clin Psychopharmacol. 2006;26:p610–625. doi: 10.1097/01.jcp.0000245566.52401.20. [DOI] [PubMed] [Google Scholar]
- 80.Pettinati H.M, Kampman K.M, Lynch K.G, Xie H, Dackis C, Rabinowitz A.R, et al. A double blind placebo controlled trial that combines naltrexone and disulfiram in the treatment of cocaine and alcohol dependent patients. Addict Behav. 2008;33(5):p651–667. doi: 10.1016/j.addbeh.2007.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Poulsen E.H. Disulfiram therapy – adverse drug reactions and interactions. Acta Psych Scand. 1992;86:p59–66. doi: 10.1111/j.1600-0447.1992.tb03317.x. [DOI] [PubMed] [Google Scholar]
- 82.Richardson K, Baillie A, Reid S, Morley K, Teeson M, Saanibale C, et al. Do acamprosate or naltrexone have an effect on daily drinking by reducing craving for alcohol? Addiction. 2008;103(6):p953–959. doi: 10.1111/j.1360-0443.2008.02215.x. [DOI] [PubMed] [Google Scholar]
- 83.Rosenthal R.N. Current and future drug therapies for alcohol dependence. J Clin Psychopharmacol. 2006;26(Supp 1):pS20–S29. [Google Scholar]
- 84.Rubio G, Jimenez-Arriero M.A, Ponce G, Palamo T. Naltrexone versus acamprosate: one year follow up of alcohol dependence treatment. Alcohol Alcohol. 2001;36:p419–425. doi: 10.1093/alcalc/36.5.419. [DOI] [PubMed] [Google Scholar]
- 85.Sass H, Soyka M, Mann K, Zeiglgansberger W. Relapse prevention by acamprosate. Results from a placebo controlled trial on alcohol dependence. Arch Gen Psychiatry. 1996;53:p673–680. doi: 10.1001/archpsyc.1996.01830080023006. [DOI] [PubMed] [Google Scholar]
- 86.Savas M.C, Gullu J.H. Disulfiram ethanol reaction – the significance of supervision. Annals Pharmacother. 1997;31:p374–375. doi: 10.1177/106002809703100325. [DOI] [PubMed] [Google Scholar]
- 87.Schadlich P.K, Brecht J.G. The cost effectiveness of acamprosate in the treatment of alcoholism in Germany. Economic evaluation of the Prevention of Relapse with Acamprosate in the Management of Alcoholism (PRAMA) study. Pharmacoeconomics. 1998;13(6):p719–730. doi: 10.2165/00019053-199813060-00008. [DOI] [PubMed] [Google Scholar]
- 88.Skradski S, White H.S. Topiramate blocks kainite evoked cobalt influx into cultured neurons. Epilepsia. 2000;41(Suppl 1):pS45–S47. doi: 10.1111/j.1528-1157.2000.tb02171.x. [DOI] [PubMed] [Google Scholar]
- 89.Srisurapanont M, Jarusuraisin N. Naltrexone for the treatment of alcoholism: a meta analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2005;8:p267–280. doi: 10.1017/S1461145704004997. [DOI] [PubMed] [Google Scholar]
- 90.Streeton C, Wheelan G. Naltrexone, a relapse prevention maintenance treatment of alcohol dependence: a meta analysis of randomized controlled trials. Alcohol Alcohol. 2001;36(6):p544–552. doi: 10.1093/alcalc/36.6.544. [DOI] [PubMed] [Google Scholar]
- 91.Suh J.J, Pettinati H.M, Kampman K.M, O’Brien C.P. The status of Disulfiram: a half of a century later. J Clin Psychopharmacol. 2006;26:p290–302. doi: 10.1097/01.jcp.0000222512.25649.08. [DOI] [PubMed] [Google Scholar]
- 92.Swift R.M, Whelihan W, Kuznetsov O, Buongiorno G, Hsuing H. Naltrexone induced alterations in human ethanol intoxication. Am J Psychiatry. 1994;151(10):p1463–1467. doi: 10.1176/ajp.151.10.1463. [DOI] [PubMed] [Google Scholar]
- 93.Swift R.M. Drug therapy for alcohol dependence. New Eng J Med. 1999;340:p1482–1490. doi: 10.1056/NEJM199905133401907. [DOI] [PubMed] [Google Scholar]
- 94.Volpicelli J.R, Alterman A.I, Hayashida M, O’Brien C.P. Naltrexone in the treatment of alcohol dependence. Arch Gen Psychiatry. 1992;49:p876–880. doi: 10.1001/archpsyc.1992.01820110040006. [DOI] [PubMed] [Google Scholar]
- 95.Walters D, Connors J.P, Feeney G.F, Young R.M. The cost effectiveness of Naltrexone added to cognitive behavioral therapy in the treatment of alcohol dependence. J Addict Dis. 2009;28(2):p137–144. doi: 10.1080/10550880902772456. [DOI] [PubMed] [Google Scholar]
- 96.Weiss R.D, Kueppenbender K.D. Combining psychosocial treatments with pharmacotherapy for the management of alcohol dependence. J Clin Psychopharmacol. 2006;(Suppl 1):pS37–S42. doi: 10.1097/01.jcp.0000248604.58305.b3. [DOI] [PubMed] [Google Scholar]
- 97.White H.S, Brown S.D, Woodhead J.H, Woodhead J.H, Skeen G.A, Wolf H.H. Topiramate modulates GABA evoked currents in murine cortical neurons by non benzodiazepine mechanisms. Epilepsia. 2000;41(Suppl 1):pS17–S20. [PubMed] [Google Scholar]
- 98.Wilde M.I, Wagstaff A.J. Acamprosate. A review of its pharmacology and its clinical potential in the management of alcohol dependence after detoxification. Drugs. 1997;53:p1038–1053. doi: 10.2165/00003495-199753060-00008. [DOI] [PubMed] [Google Scholar]
- 99.Wilkins J.N. Traditional pharmacotherapy for alcohol dependence. J Clin Psychiatry. 2006;67(suppl 14):p17–22. [Google Scholar]
- 100.Wisebeck G.A, Weijers H.G, Lesch O.M, Glaser T, Toennes P.J, Boening J. Fluphenthixol decanoate and relapse prevention in alcoholics: results from a placebo controlled study. Alcohol Alcohol. 2001;36:p329–334. doi: 10.1093/alcalc/36.4.329. [DOI] [PubMed] [Google Scholar]
- 101.Yen M.H, Ko H.C, Tang F.I, Lu R.B, Hong J.S. Study of hepatotoxicity of Naltrexone in the treatment of alcoholism. Alcohol. 2006;38(2):p117–120. doi: 10.1016/j.alcohol.2006.05.003. [DOI] [PubMed] [Google Scholar]