Abstract
Objective
The identification and treatment of critical illness is often initiated by emergency medical services (EMS) providers. We hypothesized that emergency department (ED) patients with severe sepsis who received EMS care had more rapid recognition and treatment compared with non-EMS patients.
Methods
Prospective observational study of ED patients with severe sepsis treated with early goal-directed therapy (EGDT). We included adults with suspected infection, evidence of systemic inflammation, and either hypotension after a fluid bolus or elevated lactate. Prehospital and ED clinical variables and outcomes data were collected. The primary outcome was time to initiation of antibiotics in the ED.
Results
There were 311 patients with 160 (51.4%) transported by EMS. EMS transported patients had more organ failure (sequential organ failure assessment score 7.0 vs. 6.1, p =0.02), shorter time to first antibiotics (111 vs. 146 minutes, p=0.001) and, shorter time from triage to EGDT initiation (119 vs. 160 minutes, p=0.005), compared to non-EMS transported patients. Among EMS patients, if the EMS provider indicated a written impression of sepsis, there was a shorter time to antibiotics (70 vs. 122 minutes, p=0.003) and a shorter time to EGDT initiation (69 vs. 131 minutes, p=0.001), compared to those without an impression of sepsis.
Conclusions
In this prospective cohort, EMS provided initial care for half of severe sepsis patients requiring EGDT. Patients presented by EMS had more organ failure and a shorter time to both antibiotic and EGDT initiation in the ED.
Introduction
Background
Severe sepsis imparts a significant burden on the United States (US) healthcare system, affecting approximately 750,000 persons annually, with an estimated mortality rate of 30% and annual costs of $16 billion.1 More than 500,000 cases of severe sepsis are initially managed in US emergency departments (ED) annually, with an average emergency department length of stay of 5 hours.2 The cornerstones of the ED management of severe sepsis include timely diagnosis, early administration of appropriate antibiotics, and early aggressive quantitative resuscitation.3–7
During the last several decades, emergency medical services (EMS) systems have developed an important role in the initial management of patients with life threatening injury and illness.8–10 EMS personnel are required to accurately recognize acute life threatening conditions and provide potential life saving interventions, such as initial resuscitation and airway management, in addition to expeditious transport to the most appropriate medical care facility.
The primary hypothesis of this study was that ED patients treated for severe sepsis and who received EMS care prior to hospital arrival had more timely initiation of definitive sepsis treatment, defined as time required to administer anitbiotics and initiate quantitative resuscitation, compared with non-EMS transported patients. A secondary objective was to determine if, among EMS transported patients, recognition of sepsis by EMS personnel resulted in differential time to definitive sepsis treatment, as compared to patients in whom sepsis was not recognized.
Methods
Study Design
This was a prospective observational study of patients treated in the ED with early goal directed therapy (EGDT) for severe sepsis.7 The institution specific EGDT protocol has been previously described in depth.11 The study took place from November 2005 to July 2008 and it was reviewed and approved by the institutional review board and privacy board of Carolinas Healthcare System prior to patient enrollment.
Setting
All patients were enrolled in an urban 800 bed teaching hospital with >100,000 patient visits per year and an associated emergency medicine residency program. The ED is staffed by emergency medicine resident physicians supervised by board certified emergency medicine attending physicians. The prehospital care system is comprised of a single advanced life support EMS agency, which serves a population of approximately 867,000 individuals with an average yearly call volume of 90,000 resulting in approximately 69,000 yearly patient transports.
Selection of Participants
Eligible subjects were prospectively identified by board-certified emergency physicians in the ED, and inclusion criteria were: 1) age > 17 years; 2) suspected or confirmed infection; 3) two or more systemic inflammatory response syndrome (SIRS) criteria12: heart rate > 90 beats per minute, respiratory rate > 20 breaths per minute, temperature >38 or < 36° C, white blood cell count > 12,000 or < 4000 cells/mm3 or > 10% bands; 4) systolic blood pressure < 90 mm Hg or mean arterial pressure < 65 mm Hg after a 20 milliliter per kilogram isotonic fluid bolus OR anticipated need for intensive care unit (ICU) care and a serum lactate concentration ≥ 4.0 millimoles per liter. Exclusion criteria were: 1) need for immediate surgery with an anticipated departure to the operating room in < 6 hours; 2) absolute contraindication for an internal jugular or subclavian central venous catheter; 3) transfer from another hospital.
Methods of Measurement
Clinical variables and outcomes data were prospectively abstracted on standardized forms from the patient’s hospital record and electronic EMS patient care report form. The primary outcome variable for this analysis was time to initiation of definitive severe sepsis treatment, defined as administration of an antibiotic. This was a continuous time variable encompassing the interval from patient triage into the ED to first antibiotic administration. Triage time was the time stamp recorded by the triage nurse during initial evaluation for ambulatory patients or the time a nurse recorded that a patient was placed in a room, for EMS patients. Anitibiotic administration time was the time a nurse recorded in their notes that the first antibiotic was administered. Recent literature has emphasized the association between initiation of antibiotics within 1 hour of severe sepsis recognition and hospital survival4,13, therefore time to antibiotic treatment was also analyzed as a dichotomous variable with patients categorized as either receiving antibiotic therapy in ≤ 1 hour or > 1 hour of ED triage.
The main secondary outcome variable was time to recognition of severe sepsis, defined as time to initiation of EGDT. This was also a continuous time variable encompassing the interval from patient triage to initiation of the hospital “Code Sepsis” protocol, an institutional specific EGDT protocol that has previously been described.11 The Code Sepsis time was the time documented by an automated hospital paging system that is triggered by the emergency physician at the time he or she places a central venous catheter for hemodynamic monitoring. In addition, we collected in-hospital mortality.
The main independent variable of interest was the provision of EMS care prior to arriving at the ED. This was a dichotomous variable with patients classified as either receiving or not receiving EMS care prior to ED admission. To allow for a subgroup analysis, patients transported by EMS were further classified based on the documented primary impression of illness by EMS personnel. Thus EMS transported patients were classified as either a primary impression of sepsis, which required explicit use of the word ‘sepsis’ and indication that this was the paramedics primary clinical concern in either the narrative or impression sections of the chart, or any other primary impression.
Other independent variables collected included the demographic variables age, gender, race, as well as the patient’s initial sequential organ failure assessment (SOFA) score measured in the ED.14 SOFA score is a quantitative measure of both the number and severity of failed organs and its utility as a predictive instrument in ED patients with severe sepsis has been previously documented.15 Other clinical variables collected include minimum systolic blood pressure, minimum oxygen saturation, maximum heart rate, respiratory rate, temperature, and serum lactate. Inter-observer reliability of abstracted data, specifically the primary impression of sepsis, was assessed by a blinded, independent data abstractor on 10% of the EMS charts.
Primary Data Analysis
Study population characteristics were analyzed using descriptive statistics, including frequencies and 95% confidence intervals (CI), means, and standard deviations (SD) and were tested using unpaired t-tests or Mann-Whitney test depending on normality for continuous data and chi-square tests for categorical data. Inter-observer agreement of abstracted data elements were tested using Cohen’s kappa statistic. To determine if patient characteristics differed based on the provision of EMS care prior to hospital arrival, we assessed the univariate association between time to antibiotics and receiving EMS care using the Mann-Whitney test as well as 95% CI for the difference in means. Comparable analyses were conducted on the secondary outcome variable.
To further assess the associations between the main outcome and independent variables, linear regression was performed to adjust for the potential confounding of the demographic variables and SOFA score. An investigator driven forward stepwise model building approach was undertaken whereby the naive model consisted of only the primary outcome and main independent variable. Other independent variables were added to the model one at a time to assess for potential confounding of the main effect. Model fit was assessed by inspecting residual plots.
The association between EMS care and antibiotic treatment as a dichotomous variable was analyzed using a test of independent proportions and 95% CIs for the difference in proportions. In order to adjust for the potential confounding variables previously mentioned, logistic regression was performed using a forward stepwise method similar to that performed in the linear regression. Model fit was assessed using the Hosmer-Lemeshow goodness of fit test. The association between EMS care and inhospital mortality was examined using a test of independent proportions and 95% CIs for the difference in proportions.
A subgroup analysis was preformed among patients presenting with EMS care. The analysis was conducted to determine if the distribution of time to antibiotic treatment among these patients differed based on whether EMS providers indicated a primary impression of sepsis. Patient characteristics were also analyzed to determine if differences existed based on EMS primary impression. Finally, a linear regression model was constructed to assist in interpreting the measure of effect in the presence of potential confounding variables.
We calculated that in order to find a 30 minute decrease in the primary outcome in the EMS care group compared to the non-EMS care group, assuming equal distribution of the subjects, an alpha of 0.05 and a beta of 0.20 would require a minimum sample of 143 patients per group or 286 patients total. All analyses were performed using Stata v10.1 (College Station, TX) and for all tests, p<0.05 was considered significant.
Results
There were 333 patients diagnosed with severe sepsis initially available for analyses with 311 (94%) having complete data. Twenty two patients were excluded from the analysis because data regarding the primary outcome variable or independent variables were missing. The Kappa statistic for inter-observer agreement of the abstracted data was 0.82 indicating good agreement.
Table 1 includes the demographics and clinical characteristics of the patients included in the analysis. Briefly, there were 148 (47.6%) male patients, 167 (53.7%) were Caucasian, the average age was 58.9 (SD = 17.5), and the average initial SOFA score was 6.6 (SD = 3.4). Of the 311 patients included, 160 (51.5%) received EMS care prior to arriving at the ED. Patients receiving EMS care were slightly older (61.3, 95% CI 58.7 to 63.8) and had slightly higher initial SOFA scores (7.0, 95% CI 6.5 to 7.6) than those not receiving EMS care, mean age 56.3 (95% CI 53.4 to 59.2) and mean initial SOFA 6.1 (95% CI 5.6 to 6.7). There was no variability in the gender or race of patients receiving EMS care. No patients in the group that did not receive EMS care were placed in a waiting room after initial triage.
Table 1.
Clinical characteristics and demographics of the study population
| Variable Name | Entire Study Population (n=311) | Transported By EMS (n=160) | Not transported by EMS (n=151) |
|---|---|---|---|
| Gender | |||
| Male | 161 (48.5%) | 83 (49.7%) | 78 (47.3%) |
| Female | 171 (51.5%) | 84 (50.3%) | 87 (52.7%) |
| Race | |||
| White | 176 (53.7%) | 89 (54.3%) | 87 (53.0%) |
| Non-white | 152 (46.3%) | 75 (45.7%) | 77 (47.0%) |
| Age* | 58.9 (17.4) | 61.2 (58.7–63.7) | 56.5 (53.7–59.3) |
| ED SOFA Score* | 6.8 (3.5) | 7.2 (6.6–7.7) | 6.4 (5.8–6.9) |
| ED Minimum SBP (mm Hg) | 73.3 (17.6) | 71.5 (68.8–74.2) | 75.1 (72.2–78.1) |
| ED Minimum SaO2 (%) | 91.1 (11.7) | 91.3 (89.8–92.7) | 90.9 (88.5–93.2) |
| ED Maximum HR (beats/min) | 120.3 (24.9) | 120.0 (116.1–124.0) | 120.7 (116.7–124.7) |
| ED Maximum RR* (breaths/min) | 29.7 (11.0) | 31.1 (29.1–33.0) | 28.2 (26.6–29.9) |
| Maximum Temperature (°F) | 99.7 (9.4) | 99.2 (97.6–100.8) | 100.1 (98.7–101.5) |
| Highest Lactate (mmol/L) | 4.4 (3.7) | 4.8 (4.2–5.4) | 4.0 (3.4–4.6) |
All continuous data are presented as means with standard deviations and categorical data presented as proportions with 95% confidence intervals.
Indicates the statistical finding of p<0.05 between the EMS and non EMS transported groups.
Abbreviations: EMS – emergency medical services; ED – emergency department; SOFA – sequential organ failure assessment; SBP – systolic blood pressure; mm Hg – millimeters of mercury; SaO2 – oxygen saturation; HR – heart rate; RR – respiratory rate; °F – degrees Fahrenheit; mmol/L – millimoles per liter
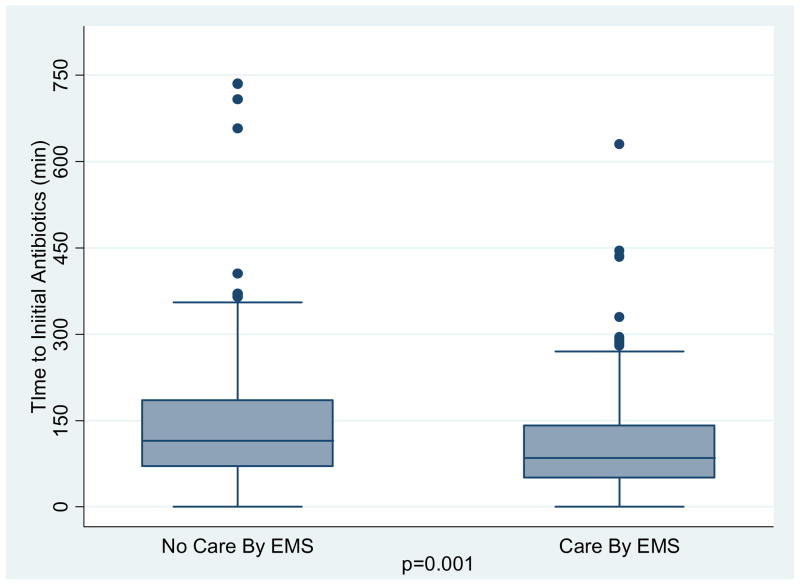
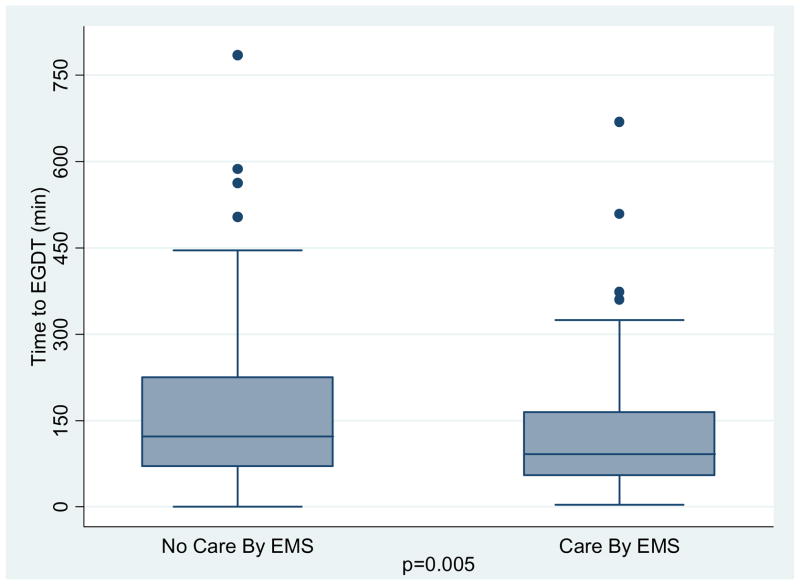
Figure 1 displays the distribution of time to first antibiotic treatment categorized according to the provision of EMS care prior to ED arrival. Patients transported by EMS had a shorter time from ED triage to initial antibiotic administration in the ED (111 minutes vs. 146 minutes, difference of 35 minutes, 95% CI 11 to 59, p=0.001) as compared to those not transported by EMS. Figure 2 displays the distribution of time to initiation of EGDT categorized according to provision of EMS care prior to arrival. Patients transported by EMS had a shorter time from ED triage to initiation of EGDT (119 minutes vs. 160 minutes, difference of 41 minutes, 95% CI 15 to 67, p=0.005) as compared to those not transported by EMS.
Figure 1.
Distribution of time to initial antibiotic administration in the ED according to provision of EMS care. Distribution of data and median values are presented. EMS – emergency medical services.
Figure 2.
Distribution of time to early goal directed therapy initiation in the ED according to provision of EMS care. Distribution of data a median values are presented. EGDT – early goal directed therapy; EMS – emergency medical services.
When adjusting for the potential confounding variables of age and initial SOFA score using linear regression, EMS care was not significantly associated with decreased time to antibiotic treatment (22 minutes, 95% CI −1 to 45, p=0.055). However, EMS care remained significantly associated with a decrease in EGDT initiation (Table 2). Individuals receiving EMS care prior to ED arrival had a decrease in the time to initiation of EGDT of 29 minutes (95% CI −4 to −55, p=0.021) compared to those not receiving EMS care when controlling for age and initial SOFA score. Residual plots indicated that the assumption of homoscedasticity did not appear to have been violated in these models.
Table 2.
Multivariable Linear Regression Model Assessing Factors Associated with Initiation of early goal directed therapy (EGDT).
| Variable Name | Coefficient | SE | 95% CI | Wald | p Value |
|---|---|---|---|---|---|
| EMS Care | −0.29 | 0.21 | −0.91, −0.07 | −2.32 | 0.021 |
| Age | −0.01 | 0.01 | −0.04, −0.01 | −3.93 | 0.001 |
| ED Initial SOFA | −0.08 | 0.03 | −0.19, −0.07 | −4.19 | 0.001 |
Coefficients shown in minutes.
Abbreviations: EMS – emergency medical services; SE – standard error; CI – confidence interval; ED – emergency department; SOFA – sequential organ failure assesment score.
When analyzed as a dichotomous variable, patients who received EMS care had an increased frequency of early antibiotic treatment (≤ 1 hour) than those without EMS care (35%, 95% CI 28% to 42% vs. 20%, 95% CI 13% to 26%; p=.003). Logistic regression indicated that individuals who received EMS care had a significantly increased odds (Odds Ratio (OR) = 2.2, 95% CI 1.3 to 3.6) of receive antibiotic treatment in ≤ 1 hour compared to those who did not receive EMS care. This association remained significant when adjusting for the potential confounding effects of age and initial SOFA score (OR = 1.94; 95% CI = 1.14 to 3.29) with this model demonstrating good fit using the Hosmer-Lemeshow goodness of fit test (p=0.64). The in-hospital mortality for those patients receiving EMS care was 25% (95% CI 18% to 32) compared to those not receiving EMS care (17%, 95% CI 11% to 23%; proportion difference 8%, 95% CI −1% to 18%).
In subgroup analysis, there were 160 patients that received EMS care prior to ED arrival with paramedics documenting a primary impression of sepsis in 33 (20.6%). When compared to patients without EMS recognition of sepsis, individuals with EMS recognized sepsis had a shorter time to antibiotic treatment (70 minutes vs. 122 minutes, difference of 52 minutes, 95% CI 17 to 86, p<0.001) and shorter initiation of EGDT (69 minutes vs. 131 minutes, difference of 62 minutes, 95% CI 23 to 100, p=0.001). When utilizing multivariable linear regression models and controlling for age and initial SOFA score, individuals with EMS recognized sepsis had a decrease in the time to initiation of antibiotics (49 minutes 95% CI −17 to −82; p=0.003) and time to EGDT (59 minutes 95% CI −23 to −95; p=0.002) compared to those with sepsis unrecognized by EMS
Discussion
In this study, we documented the impact of EMS care on the ED management of patients with severe sepsis. Specifically, we found that patients who received EMS care prior to ED arrival had a 35 minute decrease in the time to antibiotic administration and 41 minute decrease in time to initiation of EGDT when compared to patients who did not receive EMS care. Patients who received EMS care had a 15% increased frequency of early antibiotic treatment (≤ 1 hour) than non-EMS patients. Furthermore, among patients in whom sepsis was the primary impression, there was a significant decrease in time to antibiotics (52 minutes) and time to EGDT initiation (62 minutes), when compared to patients in whom EMS providers did not recognize sepsis. These results suggest that provision of EMS care impacts both the diagnostic and treatment process of severe sepsis patients in the ED.
The importance of these findings is that several relatively simple and inexpensive changes to the EMS care process could affect the care of sepsis patients in the hospital setting. We found that patients who had sepsis recognized by EMS providers had a markedly more rapid time course in sepsis care processes in the ED, as compared to those that did not have sepsis recognized. This suggests that interventions targeted at increasing EMS personnel’s ability to recognize sepsis may impact their continuing hospital care. Additional research could be designed to test if incorporation of non-invasive diagnostic modalities in the prehospital setting, such as the measurement of temperature or point-of-care lactate, could aid EMS personnel in more timely and accurate diagnosis of sepsis.
Although there is very little literature on the role of EMS in the care of early sepsis, two previous reports have investigated this topic. Wang et al found that EMS provides initially care for 34% of patients treated for an infection in the ED and 60% of patients with severe sepsis.16 We report similar findings, with EMS providing care for approximately 50% of patients with severe sepsis. In a second study, Seymour et al reported that less than half of EMS transported patients with severe sepsis received intravenous fluid prior to ED arrival.17 However the authors found no association between prehospital fluid resuscitation and achievement of EGDT goals. Our report builds on these previous studies by evaluating time to important ED care processes according to the provision of EMS services. Our results suggest that if a patient is recognized as having sepsis early by EMS personnel, an important trajectory is started that results in decreased time to two interventions that are associated with improved survival, aggressive resuscitation and early antibiotic administration.4, 6, 7
This study has several limitations that warrant comment. First, this is a single center study and as such our results may not be generalizable to populationsat other institutions. Second, our hospital is serviced by a single EMS provider and thus our results may not be applicable to situations in which a hospital is serviced by more than one EMS provider. Third, all patients were identified by their inclusion in our institutional EGDT protocol. It is possible that patients with severe sepsis were treated in our ED for severe sepsis during the study time frame but not resuscitated with EGDT and thus not included in this report. Fourth, the outcomes we studied in this manuscript are processes of medical care rather than patient oriented outcomes. The exact impact of our findings on patient outcomes is unknown. Fifth, we did not examine specific care processes provided by EMS personnel (e.g. fluids, vasopressors) but rather the overall impact of the EMS encounter, which includes both medical care and transport. It is possible that our findings are a result of more expedient time to physician contact in the ED; however, our subgroup analysis of sepsis recognition by EMS providers presents quantitative data to alleviate this potential concern. Finally, our findings are only associations between EMS care and ED process of care and causality cannot be established.
In conclusion, EMS provided initial care for half of severe sepsis patients requiring EGDT. Patients presenting by EMS had more organ failure and a shorter time to both antibiotic and EGDT initiation, the latter of which remained significant after adjusting for confounders. If sepsis is recognized by EMS personnel, the reduction in time to antibiotic and EGDT initiation is more substantial.
Acknowledgments
Dr Jones is supported by grant K23GM076652-01A1, from the National Institute of General Medical Sciences/National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Angus D, Linde-Zwirble W, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001 July;29(7):1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Wang HE, Shapiro NI, Angus DC, et al. National estimates of severe sepsis in United States emergency departments. Crit Care Med. 2007;35:1928–36. doi: 10.1097/01.CCM.0000277043.85378.C1. [DOI] [PubMed] [Google Scholar]
- 3.Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 4.Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006 June;34:1589–96. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 5.Jones AE, Brown MD, Trzeciak S, et al. The Effect of a Quantitative Resuscitation Strategy on Mortality in Patients with Sepsis: A Meta-Analysis. Crit Care Med. 2008;36:2734–9. doi: 10.1097/CCM.0b013e318186f839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones AE, Shapiro NI, Trzeciak S, et al. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303:739–46. doi: 10.1001/jama.2010.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 8.Blackwell T, Kellam JF, Thomason M. Trauma care systems in the United States. Injury. 2003;34:735–9. doi: 10.1016/s0020-1383(03)00152-9. [DOI] [PubMed] [Google Scholar]
- 9.Jollis JG, Roettig ML, Aluko AO, et al. Implementation of a statewide system for coronary reperfusion for ST-segment elevation myocardial infarction. JAMA. 2007;298:2371–80. doi: 10.1001/jama.298.20.joc70124. [DOI] [PubMed] [Google Scholar]
- 10.Acker JE, III, Pancioli AM, Crocco TJ, et al. Implementation strategies for emergency medical services within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association Expert Panel on Emergency Medical Services Systems and the Stroke Council. Stroke. 2007;38:3097–115. doi: 10.1161/STROKEAHA.107.186094. [DOI] [PubMed] [Google Scholar]
- 11.Jones AE, Focht A, Horton JM, et al. Prospective external validation of the clinical effectiveness of an emergency department-based early goal directed therapy protocol for severe sepsis and septic shock. Chest. 2007;132:425–32. doi: 10.1378/chest.07-0234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101:1644–55. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 13.Gaieski DF, Pines JM, Band RA, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38:1045–1053. doi: 10.1097/CCM.0b013e3181cc4824. [DOI] [PubMed] [Google Scholar]
- 14.Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–10. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 15.Jones AE, Trzeciak S, Kline JA. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37:1649–54. doi: 10.1097/CCM.0b013e31819def97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang HE, Weaver MD, Shapiro NI, et al. Opportunities for Emergency Medical Services care of sepsis. Resuscitation. 2010 February;81:193–7. doi: 10.1016/j.resuscitation.2009.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seymour CW, Cooke CR, Mikkelsen ME, et al. Out-of-hospital fluid in severe sepsis: effect on early resuscitation in the emergency department. Prehosp Emerg Care. 2010;14:145–52. doi: 10.3109/10903120903524997. [DOI] [PMC free article] [PubMed] [Google Scholar]