Abstract
Under the Abbreviated New Drug Application pathway, a proposed generic salmon calcitonin nasal spray is required to demonstrate pharmaceutical equivalence and bioequivalence to the brand-name counterpart or the reference listed drug. This review discusses two important aspects of pharmaceutical equivalence for this synthetic peptide nasal spray product. The first aspect is drug substance sameness, in which a proposed generic salmon calcitonin product is required to demonstrate that it contains the same active ingredient as that in the brand-name counterpart. The second aspect is comparability in product- and process-related factors that may influence immunogenicity (i.e., peptide-related impurities, aggregates, formulation, and leachates from the container/closure system). The comparability of these factors helps to ensure the product safety, particularly with respect to immunogenicity. This review also highlights the key features of in vitro and/or in vivo studies for establishing bioequivalence for a solution nasal spray containing a systemically acting salmon calcitonin.
Key words: bioequivalence, generic, immunogenicity, nasal spray, pharmaceutical equivalence, salmon calcitonin
INTRODUCTION
Calcitonin is a peptide hormone produced by the parafollicular cells of the thyroid in mammals and by the ultimobranchial gland of birds and fish (1). This peptide has an inhibiting effect on the activity of osteoclasts and reduces the resorption of bone salts into the blood. Calcitonin has been used for the treatment of osteoporosis, the management of Paget’s disease, and the initial treatment of hypercalcemia (2,3). Two calcitonin peptide drugs have been approved in the USA. They are salmon calcitonin and human calcitonin. Salmon calcitonin has a 50-fold greater potency than human calcitonin and has much less propensity for aggregation than human calcitonin (4). Therefore, salmon calcitonin is the favored therapeutic and is presently the only marketed form of this peptide drug in the USA. It is available as an injectable product and a nasal spray (5).
Whether produced by synthetic methods or by recombinant DNA technology, salmon calcitonin is a 32 amino acid residue peptide of known primary structure (amino acid sequence) and does not exhibit complex higher-order structures in aqueous solutions. The molecular structure of this peptide drug can be characterized and verified by a variety of analytical technologies. Thus, it is possible for a drug manufacturer to produce a salmon calcitonin drug product containing an active ingredient that is the same as the active ingredient in a brand-name counterpart. For generic versions of a synthetic salmon calcitonin drug product, although the active ingredient may be identical, product- and process-related factors, including peptide-related impurities, aggregates, formulation variables such as excipients, and leachates from the container/closure system, may differ and affect product safety, particularly in the area of immunogenicity. Therefore, the development of a generic synthetic salmon calcitonin drug product warrants, among other scientific considerations, deliberations of the effect of these product- and process-related factors on drug product safety and efficacy.
This review discusses a scientific evaluation of generic versions of a synthetic salmon calcitonin nasal spray drug product. We provide background information on the Food and Drug Administration (FDA) requirements for generic drug approvals, followed by a discussion of the scientific issues unique to a generic synthetic salmon calcitonin nasal spray drug product. In particular, we emphasize the scientific data that are critical for drug substance (active pharmaceutical ingredient) sameness, comparability of product- and process-related factors known to influence immunogenicity, and bioequivalence for this peptide drug product in the context of an Abbreviated New Drug Application (ANDA).
OVERVIEW OF THE REGULATORY REQUIREMENTS FOR THE GENERIC DRUG APPROVAL
A generic drug product is one that is therapeutically equivalent to an innovator or the first version of the drug product approved by the FDA, and designated as the reference listed drug (RLD). An ANDA, which includes supporting data for review and approval of a generic drug product, is submitted to the Office of Generic Drugs. For approval, an ANDA is required to contain data to show that the drug product is both pharmaceutically equivalent as well as bioequivalent to the RLD.
Pharmaceutical equivalence requires that the generic drug product contains the same active ingredient(s) as the RLD, that it be identical in strength, dosage form, and route of administration, and that it meets compendial or other applicable standards of strength, quality, purity, and identity (6). In this context, an ANDA sponsor is required to provide chemistry, manufacturing, and controls documentation for the generic drug product, consisting of information on the drug substance, including characterization, method of manufacture, and controls; and information on the drug product, including composition, method of manufacture, controls, packaging, and stability. Pharmaceutical equivalence, however, may permit some differences in characteristics of the generic and innovator drug products, such as excipients and in certain circumstances, labeling.
Bioequivalence refers to the absence of a statistically significant difference in the rate and extent to which the active ingredient in a pharmaceutically equivalent drug product becomes available at the site of action, when administered to subjects at the same molar dose under similar conditions (6). For drug products that contain a systemically acting drug formulated in an immediate- or modified-release oral dosage form, an ANDA sponsor is generally required to provide in vivo pharmacokinetic data to demonstrate bioequivalence between the generic drug product and the RLD. The two drug products are considered bioequivalent if the 90% confidence intervals (CIs) for the geometric mean test/reference ratios of area under the curve (AUC) and peak plasma concentration (Cmax) both fall within the limits of 80–125%. Under certain circumstances, in vivo pharmacokinetic data may not be needed for establishing bioequivalence (7).
Once an ANDA sponsor provides sufficient data to demonstrate that a generic drug product is pharmaceutically equivalent and bioequivalent to the RLD, FDA deems these two drug products to be therapeutic equivalents and assigns the generic product a therapeutic equivalence code (e.g., AB) in the Approved Drug Products with Therapeutic Equivalence Evaluations (the Orange Book). Therapeutically equivalent drug products are expected to have the same clinical efficacy and safety profiles when administered to patients under conditions specified in the labeling, and may be substituted for each other without any adjustment in dose or other additional monitoring.
SYNTHETIC SALMON CALCITONIN NASAL SPRAY
Pharmaceutical Equivalence
This review focuses on two critical aspects of pharmaceutical equivalence for a synthetic salmon calcitonin nasal spray. The first important aspect is demonstration of drug substance sameness, because the overall efficacy and safety of a proposed generic drug product is largely based upon the premise that it contains the same active pharmaceutical ingredient as the RLD that has been shown to be safe and effective. Demonstration of the identical active pharmaceutical ingredient structure is definitely more challenging for peptide drugs such as salmon calcitonin than for typical small molecules. The second important aspect is control of product- and process-related factors, including peptide-related impurities, aggregates, formulation factors including excipients, and leachates from the container/closure system. Such control is critical for ensuring that the proposed generic salmon calcitonin nasal spray is of comparable purity and quality to the RLD, because these factors may influence the safety and specifically, the immunogenicity of a peptide or protein drug product (8). These two important aspects are discussed below.
Drug Substance Sameness
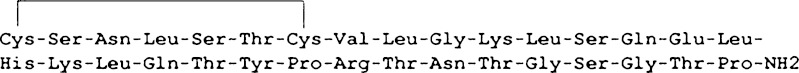
Salmon calcitonin is a simple peptide consisting of 32 amino acid residues. It has a molecular weight of 3,431.9 Da. The primary structure of this peptide is shown in Fig. 1. This peptide contains a disulfide bond between cysteine residues at positions 1 and 7, and ends with an amidated proline at the carboxyl terminus.
Fig. 1.
Primary structure (amino acid sequence) of salmon calcitonin
Nuclear magnetic resonance (NMR) and circular dichroism analyses indicate that salmon calcitonin lacks any significant higher-order structures in an aqueous solution and exhibits substantial conformational flexibility (9,10). However, salmon calcitonin shows structural ordering in the presence of sodium dodecyl sulfate (SDS) and dimyristoylphosphatidylglycerol, as well as in a water/trifluroethanol mixture (11,12). In these solvents, α-helices form and have been postulated to resemble the conformation of salmon calcitonin bound to its membrane-bound receptor (11).
The degree of the structural ordering may have significant implications for the biological activity of salmon calcitonin. For instance, a study by Arvinte et al. suggested that the greater in vivo potency of salmon calcitonin relative to human calcitonin might be attributed to the fact that salmon calcitonin adopted an α-helical structure more readily than human calcitonin (11). In addition, in an SDS environment, different conformations were observed among calcitonin species that differed in their amino acid sequence, and these differences appeared to correlate well with their hypocalcemic potency (13). The above studies of salmon calcitonin suggest that the structural ordering of this peptide observed in structure-promoting solvents is determined mainly by the peptide’s primary structure, thermodynamic factors (e.g., temperature and concentration), and interactions with other components (e.g., solvents and excipients).
For the reasons stated above, the primary structure and the disulfide bond between cysteine residues at positions 1 and 7 are the critical determinants of drug substance sameness for salmon calcitonin. The primary structure and the disulfide bond between the two cysteine residues can be characterized using orthogonal methods, including (but not limited to) amino acid analysis, mass spectroscopy (MS), amino acid sequencing (e.g., Edman degradation), peptide mapping and diagonal methods (14,15). Drug substance sameness can be further evaluated by an in vitro potency bioassay, such as the United States Pharmacopeia (USP) bioidentity test (16). Such an in vitro potency assay is useful for assessing conformational changes of salmon calcitonin upon its binding to a receptor, and comparing the ability of salmon calcitonin to bind to a receptor in the presence of different excipients.
Product-Related Factors Pertaining to Immunogenicity
Drug Substance
A primary concern regarding the therapeutic use of salmon calcitonin is its potential to induce unwanted immune responses. In contrast to human calcitonin where the generation of antibodies is rare (17), the formation of antibodies against salmon calcitonin is common, occurring in a very high percentage of patients (40–70%) (18). As further indicated in the labeling of Miacalcin Nasal Spray (19), there have been a few reports of serious allergic-type reactions in patients receiving Miacalcin (calcitonin-salmon) nasal spray and injection, including anaphylaxis and anaphylactic shock.
Although there is only 50% sequence homology between salmon and human calcitonin, not all patients treated with salmon calcitonin generate a detectable antibody response. This observation may reflect the lack of biological factors providing “danger signals” to the immune system in the drug product or to the sensitivity of the assays used to detect such antibodies. Importantly, neutralizing antibodies that mediate resistance to therapy were observed only in a subset of antibody positive patients (18). Thus, the therapeutic effect was not lost in most patients in spite of the development of antibodies. Studies with salmon calcitonin peptide fragments and chimeric calcitonin species suggest that the antigenic epitope is located in the sequence of Gly10-Lys-Leu-Ser-Gln-Glu15 (20), an epitope not apparently shared by human calcitonin which differs at four of the six residues in this stretch. The foreign specificity of the antibody response to salmon calcitonin is further supported by the findings that antibodies to salmon calcitonin showed no cross-reactivity with human calcitonin (20), and that patients with neutralizing antibodies to salmon calcitonin still responded to the human calcitonin therapy (21,22). This information indicates that the immunogenic response to salmon calcitonin is intrinsic to the amino acid sequence of this peptide which determines a foreign epitope.
Therefore, establishing sameness for the salmon calcitonin drug substance addresses the principal determinant of immunogenicity. However, there are other product- and process-related factors, such as peptide-related impurities, aggregates, excipients, and leachates from the container/closure system that can potentially affect the immunogenicity of a salmon calcitonin nasal spray product (23,24). Moreover, multiple aspects of the immune response may be impacted by these factors, including the kinetics of antibody generation, the development of a neutralizing antibody response, and the durability of the immune response. Thus, control of these product- and process-related factors is critical for ensuring the comparability of immunogenicity for salmon calcitonin drug products, and is discussed below.
Aggregates/Peptide-Related Impurities
The effect of aggregates on the immunogenicity of a drug product has been known for a long time, particularly with respect to intravenous immunoglobulin, human growth hormone, and interferon-α2a (IFN-α2a) (25). Aggregates may elicit an immune response associated with clinical effects, including the generation of neutralizing antibodies as well as hypersensitivity responses. Not all aggregates are equal in terms of their ability to elicit immune responses. Generally, it appears that small aggregates (e.g., dimers and trimers) are inefficient in inducing immune responses, whereas large aggregates (>100 kDa) appear to be more immunogenic. In particular, high molecular weight (MW) peptide aggregates, which are presented in a highly arrayed structure in the native conformation, pose a significant risk in terms of generation of immune responses that may neutralize the activity of the therapeutic peptide product, as well as cross-reactively neutralize an endogenous peptide counterpart. The effect of such large MW aggregates on immunogenicity is illustrated in the case of IFN-α2a. In this case, clinical studies revealed diminished immunogenicity of IFN-α2a drug products by improving the drug substance purification process and formulation (26,27) to eliminate oxidized species associated with high MW aggregates. This observation is also consistent with the finding of preclinical studies that suggested a strong role for aggregated species in immunogenicity.
Aggregates that display epitopes unique to the aggregated species may not lead to product neutralization or cross-reactivity on endogenous monomeric peptides, but may cause hypersensitivity responses. Peptide aggregates may be generated during the manufacture of a drug substance and drug product, as well as during storage (28–31). Salmon calcitonin has been shown to be susceptible to dimerization and further aggregation (32). The formation of aggregates during storage of peptides and proteins is strongly influenced by the formulation, which is generally designed to preserve the active conformation(s) of peptides, thereby minimizing their propensity to unfold, aggregate and degrade.
Salmon calcitonin has a much lower tendency for aggregation relative to human calcitonin, which aggregates very rapidly. However, for the above reasons, the development of an equivalent salmon calcitonin drug product requires a comparative analysis of aggregation profiles between the proposed generic product and the RLD. Such a comparative analysis performed under long-term storage and accelerated/stress conditions (e.g., elevated temperatures) ensures that the proposed generic product and the RLD do not exhibit significantly different aggregation profiles, especially when the proposed generic formulation uses a different excipient from the RLD. This means that the sizes of peptide aggregates in the proposed generic product are comparable to those in the RLD, and that their corresponding levels are lower or the same as the levels observed in the RLD. In addition, it is important to evaluate aggregate formation by using orthogonal techniques, including (but not limited to) size exclusion chromatography, analytical ultracentrifugation (AUC), NMR, and field flow fractionation (33–36), to cover all relevant aspects of aggregate size. Furthermore, evaluation of sub-visible particulates, using USP <788> and/or other methods to evaluate sub-visible particulates in the size range of 2–10 μm, can be performed to ensure comparability of particles that may affect immunogenicity.
Like aggregates, peptide modifications (peptide-related impurities), such as oxidation, deamidation, hydrolysis, truncation, or epimerization/racemization, have the potential to adversely impact the immunogenicity, as well as the activity of the drug product. Peptides appear to be more susceptible to deamidation than larger proteins whose conformations appear to protect sites from potential deamidation. Indeed, a peptide sequence of a monoclonal antibody (mAb) Fc element was much more susceptible to deamidative changes than the parent protein (37). Moreover, peptide deamidation has been shown to markedly increase aggregation for some peptides (38). One of the major degradation pathways of salmon calcitonin involves deamidation of the Gln14 and Gln20 residues (32). However, this degradation pathway has not been shown to be associated with enhanced aggregation. Peptide products may also contain d-enantiomers that can potentially enhance or diminish immunogenicity, depending on the number and types of substitutions (39). Like aggregates, these peptide modifications may arise during the manufacture of a drug substance and drug product, and/or during storage.
Thus, due to the potential adverse impact of peptide-related impurities on the immunogenicity of salmon calcitonin, it is critical to conduct a comparative evaluation of the peptide-related impurity profiles of the proposed generic product and the RLD under different conditions. Such a comparison can be conducted under long-term storage and accelerated/stress conditions by using sensitive analytical methods, such as high-performance liquid chromatography that can distinguish a subtle amino acid modification in the salmon calcitonin sequence (e.g., l-leucine vs. d-leucine). If the impurity profile of the proposed generic product is markedly different from the RLD, appropriate adjustments need to be made, for example, to the manufacturing process (e.g., purification) of drug substance and/or formulation in order to achieve the comparability of the proposed generic product and the RLD with respect to peptide-related impurities throughout the shelf life. This means that if peptide-related impurities are present in the RLD, the same impurities can also be present in the proposed generic product and at levels the same as or lower than those in the RLD.
Formulation
An appropriate formulation design of a peptide product is highly important with respect to stabilization against physical and chemical degradation. If the formulation does not adequately confer stability to peptides, the molecules are susceptible to physical degradation such as aggregation, as well as to chemical degradation such as deamidation and oxidation, particularly when the product is not optimally stored or handled. Excipients used in a formulation may also enhance the immunogenic potential of the product by interacting with a peptide through direct binding and modification of peptide conformation (40). These excipient–peptide interactions may thus affect the immunogenicity of the drug product. Finally, excipients themselves may be immunogenic, though this is rare (41–43).
If the formulation of the proposed generic product differs in any component from that of the RLD, it is essential to assess the effects of the difference in formulation on the stabilization of peptides against physical and chemical degradation. Such assessments can be done by performing comparative real time and/or forced degradation stability studies using the analytical methods described above. It is also essential to evaluate peptide–excipient interactions. One approach would be to use techniques, such as surface plasma resonance, NMR, differential scanning calorimetry, immunoassays (e.g., enzyme-linked immunosorbent assay) and bioassays (e.g., USP bioidentity test), to ensure that any difference in excipients between the proposed generic product and the RLD does not affect the conformation and activity of salmon calcitonin and does not lead to any significant difference in the excipient–peptide interactions (44–48).
Even if the formulation of the proposed generic product uses the same excipients as those used in the RLD, there can still be supplier-to-supplier differences in the excipient quality that can potentially affect the product performance. Therefore, it is important to evaluate the quality of excipients (e.g., purity) and select the supplier(s) that can consistently provide excipients that meet the quality standards for intended use.
Leachates
The concern over leachates from a container/closure system with respect to the immunogenicity of salmon calcitonin is mainly based upon the effects of materials leached from prefilled syringes into therapeutic protein products, such as erythropoietin (Eprex) (49). In the reformulated erythropoietin product, the non-ionic detergent polysorbate 80 facilitated leaching of substances from the uncoated rubber, which appeared to enhance the immune response to Eprex. It has been suggested that some of these compounds acted as immune adjuvants, while others might cause aggregation of the product and thereby elicited antibody responses to Eprex (epoetin α) (23,50). The resulting antibodies cross-reacted with endogenous proteins, and caused a surge in pure red cell aplasia (PRCA) (51). The increased number of PRCA cases corresponded precisely with the Eprex formulation change (49), in which human serum albumin used in the original formulation was replaced with glycine and polysorbate 80.
The use of a suitable container/closure system and formulation can minimize the amount of leachates from the container/closure system throughout the shelf life, and therefore mitigates the immunogenicity concerns due to leachates. It is important to analyze the qualitative as well as quantitative nature of the proposed generic and RLD products’ leachable profile(s) over the shelf life and under accelerated/stress conditions by using analytical methods, such as gas chromatograph/MS and liquid chromatograph/MS (52,53). Such an analysis is performed to ensure the absence of leachates to a sensitive detection threshold or the comparability of leachable profiles between the proposed generic product and the RLD throughout the product shelf life.
Bioequivalence
Bioequivalence testing is a critical tool for evaluating the effects of design (e.g., formulation and/or device) in a pharmaceutically equivalent or generic drug product on drug delivery. It is used to ensure that the active ingredient in a pharmaceutically equivalent product becomes available at the site of action at the same rate and extent as the RLD, when administered to subjects at the same molar dose under similar conditions.
Nasal delivery of a systemically acting peptide drug is dependent on the drug substance, formulation, and device characteristics (54,55). Thus, development of a bioequivalent salmon calcitonin nasal spray solution can rely on qualitative (Q1) and quantitative (Q2) sameness of formulation and comparability of nasal spray device (e.g., valve, pump, and actuator designs). Q1 means that the proposed generic product uses the same inactive ingredient(s) as the RLD. Q2 means that concentrations of the inactive ingredient(s) used in the proposed generic product are within ±5% of those used in the RLD. By taking into account these two design principles in drug product development, the equivalent performance of the proposed generic nasal spray product and the RLD with respect to drug delivery can therefore be evaluated by in vitro tests, including single actuation content through container life, droplet size distribution by laser diffraction, droplet size distribution by cascade impactor, spray pattern, plume geometry, priming, and repriming (55).
The concentration of an excipient or the use of a particular preservative may alter the nasal absorption of salmon calcitonin. Thus, if the proposed generic formulation contains an excipient different from that in the RLD formulation or uses the same excipient as the RLD but at a different concentration, in vitro tests by themselves will not be sufficient to evaluate the excipient effect on bioequivalence. Therefore, it is important to perform an additional in vivo bioequivalence study to evaluate whether the proposed generic product and the RLD behave the same with respect to nasal drug delivery of salmon calcitonin to the systemic circulation.
Such an in vivo bioequivalence study is generally based upon a two-way crossover study design. A replicate study design may also be acceptable. Healthy subjects are preferred for the bioequivalence study as they are generally less variable than patients, and therefore may be more sensitive in detecting effects of excipients and other formulation parameters on bioequivalence to the RLD. Pharmacokinetic parameters, such as the AUC and Cmax, are determined from the salmon calcitonin plasma concentration-time profiles of the proposed generic drug product and compared with those of the RLD. The two drug products are considered bioequivalent if the 90% CIs for the geometric mean test/reference ratios of AUC and Cmax both fall within the limits of 80–125%.
CONCLUSIONS
This review presents a scientific evaluation of generic versions of a synthetic salmon calcitonin nasal spray drug product. In the context of an ANDA, a proposed generic salmon calcitonin nasal spray is required to be pharmaceutically equivalent to the RLD. Two key aspects of pharmaceutical equivalence are discussed: the demonstration of drug substance (active pharmaceutical ingredient) sameness; and comparability in product- and process-related factors influencing immunogenicity (i.e., peptide-related impurities, aggregates, formulation, and leachates from the container/closure system). These two aspects are particularly important for ensuring the comparability of immunogenicity between the proposed generic drug product and the RLD. The proposed generic drug product is also required to be bioequivalent to the RLD. Once bioequivalence is established, the pharmaceutical equivalent is expected to have the same clinical effect and safety profile as the RLD when administered to patients under the condition specified in the labeling. These two drug products may be substituted for each other without any dose adjustment and other additional warning.
Footnotes
The opinions expressed in this review by the authors do not necessarily reflect the views or policies of the Food and Drug Administration (FDA).
REFERENCES
- 1.Sexton PM, Findlay DM, Martin TJ. Calcitonin. Curr Med Chem. 1999;6:1067–1093. [PubMed] [Google Scholar]
- 2.Sato M, Grese TA, Dodge JA, Byrant HU, Turner CH. Emerging therapies for the prevention or treatment of postmenopausal osteoporosis. J Med Chem. 1999;42:1–24. doi: 10.1021/jm980344o. [DOI] [PubMed] [Google Scholar]
- 3.Friedman PA. Agents affecting mineral ion homeostasis and bone turnover. In: Brunton LL, Lazo JS, Parker KL, editors. Goodman and gilman’s the pharmacological basis of therapeutics. 11. New York: McGraw-Hill; 2005. pp. 1647–1678. [Google Scholar]
- 4.Arvinte T, Cudd A, Drake AF. The structure and mechanism of formation of human calcitonin fibrils. J Biol Chem. 1993;268:6415–6422. [PubMed] [Google Scholar]
- 5.Orange book: approved drug products with therapeutic equivalence evaluations. Available at: http://www.accessdata.fda.gov/scripts/cder/ob/default.cfm (2009). Accessed 4 January 2010
- 6.Orange book: approved drug products with therapeutic equivalence evaluations. 30th ed. 2010. pp. iii–v [PubMed]
- 7.FDA’s draft guidance for industry. Waiver of in vivo bioavailability and bioequivalence studies for immediate-release solid oral dosage forms based on a biopharmaceutics classification system. US Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER), Rockville, MD; 2000
- 8.Schellekens H. Bioequivalence and the immunogenicity of biopharmaceuticals. Nat Rev Drug Discov. 2002;1:456–462. doi: 10.1038/nrd818. [DOI] [PubMed] [Google Scholar]
- 9.Motta A, Morelli MA, Goud N, Temussi PA. Sequential 1 H NMR assignment and secondary structure determination of salmon calcitonin in solution. Biochem. 1989;28:7996–8002. doi: 10.1021/bi00446a005. [DOI] [PubMed] [Google Scholar]
- 10.Epand RM, Epand RF, Orlowski RC, Seyler JK, Colescott RL. Conformational flexibility and biological activity of salmon calcitonin. Biochem. 1986;25:1964–1968. doi: 10.1021/bi00356a019. [DOI] [PubMed] [Google Scholar]
- 11.Epand RM, Epand RF, Orlowski RC, Schlueter RJ, Boni LT, Hui SW. Amphipathic helix and its relationship to the interaction of calcitonin with phospholipids. Biochem. 1983;22:5074–5084. doi: 10.1021/bi00291a005. [DOI] [PubMed] [Google Scholar]
- 12.Arvinte T, Drake AF. Comparative study of human and salmon calcitonin secondary structure in solutions with low dielectric constants. J Bio Chem. 1993;268:6408–6414. [PubMed] [Google Scholar]
- 13.Siligardi G, Samori B, Melandri S, Visconti M, Drake AF. Correlations between biological activities and conformational properties for human, salmon, eel, porcine calcitonins and elcatonin elucidated by CD spectroscopy. Eur J Biochem. 1994;221:1117–1125. doi: 10.1111/j.1432-1033.1994.tb18832.x. [DOI] [PubMed] [Google Scholar]
- 14.Brown JR, Hartley BS. Location of disulphide bridges by diagonal paper electrophoresis. The disulphide bridges of bovine chymotrypsinogen A. Biochem J. 1966;101:214–228. doi: 10.1042/bj1010214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Creighton TE. Proteins: structure and molecular properties. 2. New York: W. H. Freeman and Company; 1997. [Google Scholar]
- 16.U.S. Pharmacopeia 32/National Formulary 27, Calcitonin Salmon. 1 December 2009 to 1 May 2010. Available at: http://www.uspnf.com. Accessed February 11, 2010
- 17.Grauer A, Reinel HH, Lunghall S, Lindh E, Ziegler R. Formation of neutralizing antibodies after treatment with human calcitonin. Am J Med. 1993;95:439–442. doi: 10.1016/0002-9343(93)90315-G. [DOI] [PubMed] [Google Scholar]
- 18.Grauer A, Ziegler R, Raue F. Clinical significance of antibody against calcitonin. Exp Clin Endocrinol Diabetes. 1995;103:345–351. doi: 10.1055/s-0029-1211376. [DOI] [PubMed] [Google Scholar]
- 19.NDA 017808 Labeling, Miacalcin (calcitonin-salmon) Nasal Spray, Rev. October 2009. Available at: http://www.accessdata.fda.gov/scripts/cder/drugsatfda/. Accessed September 30, 2010
- 20.Kozono T, Hirata M, Endo K, Satoh K, Takanashi H, Miyauchi T, et al. A Chimeric analog of human and salmon calcitonin eliminates antigenicity and reduces gastrointestinal disturbances. Endocrinol. 1992;131:2885–2890. doi: 10.1210/en.131.6.2885. [DOI] [PubMed] [Google Scholar]
- 21.Singer FR. Clinical efficacy of salmon calcitonin in Paget’s disease of bone. Calcif Tissue Int. 1991;49:S7–S8. doi: 10.1007/BF02561369. [DOI] [PubMed] [Google Scholar]
- 22.Rojanasathit S, Rosenberg E, Haddad JG. Paget’s bone disease: response to human calcitonin in patients resistant to salmon calcitonin. Lancet. 1974;2:1412–1415. doi: 10.1016/S0140-6736(74)90072-5. [DOI] [PubMed] [Google Scholar]
- 23.Schellekens H. Factors influencing the immunogenicity of therapeutic proteins. Nephrol Dial Transplant. 2005;20:vi3–vi9. doi: 10.1093/ndt/gfh1092. [DOI] [PubMed] [Google Scholar]
- 24.De Groot AS, Scott DW. Immunogenicity of protein therapeutics. Trends Immunol. 2007;11:482–490. doi: 10.1016/j.it.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 25.Rosenberg AS. Effects of protein aggregates: an immunologic perspective. AAPS J. 2006;8:E501–E507. doi: 10.1208/aapsj080359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryff JC. Clinical investigation of the immunogenicity of interferon-alpha 2a. J Interferon Cytokine Res. 1997;17:S29–S33. [PubMed] [Google Scholar]
- 27.Hochuli E. Interferon immunogenicity: technical evaluation of interferon-alpha 2a. J Interferon Cytokine Res. 1997;17:S15–S21. [PubMed] [Google Scholar]
- 28.Sarciaux JM, Mansour S, Hageman MJ, Nail SL. Effects of buffer composition and processing conditions on aggregation of bovine IgG during freeze-drying. J Pharm Sci. 1999;88:1354–1361. doi: 10.1021/js980383n. [DOI] [PubMed] [Google Scholar]
- 29.Hansson UB. Aggregation of human immunoglobulin G upon freezing. Acta Chem Scand. 1968;22:483–489. doi: 10.3891/acta.chem.scand.22-0483. [DOI] [PubMed] [Google Scholar]
- 30.Eckhardt BM, Oeswein JQ, Bewley TA. Effect of freezing on aggregation of human growth hormone. Pharm Res. 1991;8:1360–1364. doi: 10.1023/A:1015888704365. [DOI] [PubMed] [Google Scholar]
- 31.Wang W. Protein aggregation and its inhibition in biopharmaceutics. Int J Pharm. 2005;289:1–30. doi: 10.1016/j.ijpharm.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 32.Windisch V, Deluccia F, Duhau L, Herman F, Mencel JJ, Tang SY, et al. Degradation pathways of salmon calcitonin in aqueous solution. J Pharm Sci. 1997;86:359–364. doi: 10.1021/js9602305. [DOI] [PubMed] [Google Scholar]
- 33.Bocian W, Sitkowski J, Tarnowska A, Bednarek E, Kawecki R, Koźmiński W, et al. Direct insight into insulin aggregation by 2D NMR complemented by PFGSE NMR. Proteins. 2008;71:1057–1065. doi: 10.1002/prot.21969. [DOI] [PubMed] [Google Scholar]
- 34.Kamberi M, Chung P, DeVas R, Li L, Li Z, Ma X, et al. Analysis of non-covalent aggregation of synthetic hPTH (1-34) by size-exclusion chromatography and the importance of suppression of non-specific interactions for a precise quantitation. J Chromatogr B Technol Biomed Life Sci. 2004;810:151–155. doi: 10.1016/j.jchromb.2004.07.026. [DOI] [PubMed] [Google Scholar]
- 35.Lebowitz J, Lewis MS, Schuck P. Modem analytical ultracentrifugation in protein science: tutorial review. Protein Sci. 2002;11:2067–2079. doi: 10.1110/ps.0207702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levin S. Field flow fractionation in biomedical analysis. Biomed Chromatogr. 1991;5:133–137. doi: 10.1002/bmc.1130050308. [DOI] [PubMed] [Google Scholar]
- 37.Sinha S, Zhang L, Duan S, Williams TD, Vlasak J, Ionescu R, et al. Effect of protein structure on deamidation rate in the Fc fragment of an IgG1 monoclonal antibody. Protein Sci. 2009;18:1573–1584. doi: 10.1002/pro.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nilsson MR, Driscoll M, Raleigh DP. Low levels of asparagine deamidation can have a dramatic effect on aggregation of amyloidogenic peptides: Implications for the study of amyloid formation. Protein Sci. 2002;11:342–349. doi: 10.1110/ps.48702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Regenmortel MH, Muller S. D-peptides as immunogens and diagnostic reagents. Curr Opin Biotechnol. 1998;9:377–382. doi: 10.1016/S0958-1669(98)80011-6. [DOI] [PubMed] [Google Scholar]
- 40.Lam XM, Patapoff T, Nguyen T. The effect of benzyl alcohol on recombinant human interferon-gamma. Pharm Res. 1997;14:725–729. doi: 10.1023/A:1012190120061. [DOI] [PubMed] [Google Scholar]
- 41.Kim SH, Ahn Y. Anaphylaxis caused by benzalkonium in a nebulizer solution. J Korean Med Sci. 2004;19:289–290. doi: 10.3346/jkms.2004.19.2.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hofmann H, Goerz G, Plewig G. Anaphylactic shock from chlorobutanol-preserved oxytocin. Contact Dermat. 1986;15:241. doi: 10.1111/j.1600-0536.1986.tb01344.x. [DOI] [PubMed] [Google Scholar]
- 43.Boyvat A, Akyol A, Gürgey E. Contact sensitivity to preservatives in Turkey. Contact Dermat. 2005;52:329–332. doi: 10.1111/j.0105-1873.2005.00607.x. [DOI] [PubMed] [Google Scholar]
- 44.Pattnaik P. Surface plasmon resonance: applications in understanding receptor-ligand interaction. Appl Biochem Biotechnol. 2005;126:79–92. doi: 10.1385/ABAB:126:2:079. [DOI] [PubMed] [Google Scholar]
- 45.Bruylants G, Wouters J, Michaux C. Differential scanning calorimetry in life science: thermodynamics, stability, molecular recognition and application in drug design. Curr Med Chem. 2005;12:2011–2020. doi: 10.2174/0929867054546564. [DOI] [PubMed] [Google Scholar]
- 46.Hudson FM, Andersen NH. Exenatide: NMR/CD evaluation of the medium dependence of conformation and aggregation State. Biopolymers. 2004;76:298–308. doi: 10.1002/bip.20126. [DOI] [PubMed] [Google Scholar]
- 47.Chen WL, Liu WT, Yang MC, Hwang MT, Tsao JH, Mao SJ. A novel conformation-dependent monoclonal antibody specific to the native structure of beta-lactoglobulin and its application. J Dairy Sci. 2006;89:912–921. doi: 10.3168/jds.S0022-0302(06)72156-7. [DOI] [PubMed] [Google Scholar]
- 48.Costantino HR, Culley H, Chen L, Morris D, Houston M, Roth S, et al. Development of calcitonin salmon nasal spray: similarity of peptide formulated in chlorobutanol compared to benzalkonium chloride as preservative. J Pharm Sci. 2009;98:3691–3706. doi: 10.1002/jps.21690. [DOI] [PubMed] [Google Scholar]
- 49.Sharma B, Bader F, Templeman T, Lisi P, Ryan M, Heavner GA. Technical investigations into the cause of the increased incidence of antibody-mediated pure red cell aplasia associated with Eprex®. Eur J Hosp Pharm. 2004;5:86–91. [Google Scholar]
- 50.Hermeling S, Schellekens H, Crommelin DJ, Jiskoot W. Micelle-associated protein in epoetin formulations: a risk factor for immunogenicity? Pharm Res. 2003;20:1903–1907. doi: 10.1023/B:PHAM.0000008034.61317.02. [DOI] [PubMed] [Google Scholar]
- 51.Boven K, Stryker S, Knight J, Thomas A, van Regenmortel M, Kemeny DM, et al. The increased incidence of pure red cell aplasia with an Eprex formulation in uncoated rubber stopper syringes. Kidney Int. 2005;67:2346–2353. doi: 10.1111/j.1523-1755.2005.00340.x. [DOI] [PubMed] [Google Scholar]
- 52.Ball D, Blanchard J, Jacobson-Kram D, McClellan RO, McGovern T, Norwood DL, et al. Development of safety qualification thresholds and their use in orally inhaled and nasal drug product evaluation. Toxicol Sci. 2007;97:226–236. doi: 10.1093/toxsci/kfm058. [DOI] [PubMed] [Google Scholar]
- 53.Norwood DL, Paskiet D, Ruberto M, Feinberg T, Schroeder A, Poochikian G, et al. Best practices for extractables and leachables in orally inhaled and nasal drug products: an overview of the PQRI recommendations. Pharm Res. 2008;25:727–739. doi: 10.1007/s11095-007-9521-z. [DOI] [PubMed] [Google Scholar]
- 54.Edman P, Björk E. Routes of delivery: case studies: nasal delivery of peptide drugs. Adv Drug Delivery Rev. 1992;8:165–177. doi: 10.1016/0169-409X(92)90001-7. [DOI] [Google Scholar]
- 55.FDA’s draft guidance for industry. Bioavailability and bioequivalence studies for nasal aerosols and nasal sprays for local action. US Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER), Rockville, MD; 2003