Abstract
Revision total hip arthroplasty in the setting of a large proximal femoral deficiency or a peri-prosthetic fracture remains a challenging problem. We describe the development, surgical technique and the use of cementless revision stems with distal inter-locking screws to provide immediate stability of the femoral implant. Results were assessed in a large multicentre French study conducted with the french hip and knee surgery society (SFHG). We retrospectively reviewed 725 revisions using interlocking stems from 14 French orthopaedic departments. Seven different stems were used in this series. In-patient records were retrieved, and in addition to demographic data the indication for revision, the preoperative and postoperative PMA and Harris hip scores were documented. The bone deficiency was classified on the basis of the French National Orthopaedic Meeting (SOFCOT) classification. Intraoperative complications and problems if any were retrieved from operative notes. Clinical status and radiographs at the final follow-up were evaluated, paying special attention to the metaphyseal filling index. Average follow-up was 4.5 years. As for the clinical results, the mean Harris hip score at last follow-up was 81. Therefore, it increased by an average of 31 points. Bone reconstruction was assessed on the cortico-medullary index in the metaphyseal area and at mid-shaft increasing from 36 to 45 and 54 to 63, respectively. Radiologically, 637 implants were stable, and 40 demonstrated subsidence. Forty-eight implants have been revised. We found a significant relation between the metaphyseal filling index, the stability of the stem and the quality of bone reconstruction. Results were analysed with respect to three groups of stems: group 1 was a straight, partially HA-coated implant; group 2 was a curved, fully HA-coated implant; and group 3 was a curved, partially-coated implant. Group 1 showed a significantly higher rate of failure when compared with the others types of implants. Group 2 had better functional results than group 3, which in turn reported better results than group 1. With regard to implant fixation, group 2 had significantly better results. Both groups 2 and 3 induced less thigh pain than group 1. The distal interlocking stem has shown promising results for femoral revisions. The advantages are initial axial and rotational stability and consistent bony in-growth owing to hydroxyapatite coating. Distal locked stems are mainly indicated to treat complex femoral revision with severe bone loss and peri-prosthetic fractures.
Introduction
Distally locked stems were developed in France in 1988 to address complex femoral revision secondary to osteolysis or peri-prosthetic femoral bone fractures. These implants, initially without surface treatment, were straight titanium stems, and were conceived as a holding method allowing femoral reconstitution. Furthermore, investigators were able to observe, in the great majority of cases, a spontaneous rebuilding of the bone stock. The result being the same with or without bone grafting. In theory their insertion should have been followed by further revision with shorter primary implants. In fact, this operation was rarely performed in view of the excellent reconstructions and favourable clinical results in elderly patients [1]. Subsequent implants have evolved towards the concept of one-stage use, with partial or full coating, straight or curved stem, extension of locking and modularity, able to bring about a reconstructive osteogenesis process without bone grafting. This paper assesses the current status of this concept, and reveals clinical and radiological results of a large multi-centre study to highlight the strengths and weaknesses of this technique.
Materials and methods
Implants
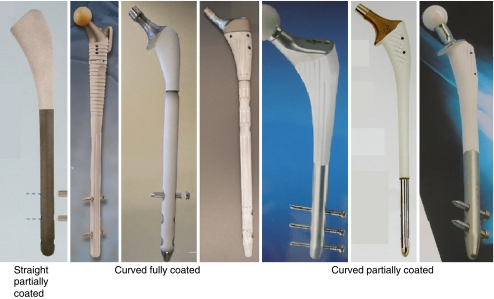
All femoral implants are made of TiAlV (ISO 5832/3). A range of stems with or without collar are available in France, in different lengths (190–300 mm) and different diameters (10–16 mm). Some are always straight, but more recent devices are curved following a radius of 1500 mm, corresponding to the average curvature of a standard femur. Most of the stems are coated with 80 μ hydroxyapatite, HA coating on the first or on the two proximal thirds. Few stems are fully coated (Fig. 1). The implant concept is based on primary distal fixation by interlocking, even in cases of extensive bone loss, as a prelude to secondary fixation by osteointegration. This distal mechanism of fixation permits an exact restoration of the length of the lower limb, and provides initial axial and rotational stability.
Fig. 1.
Different types of distal locked stems
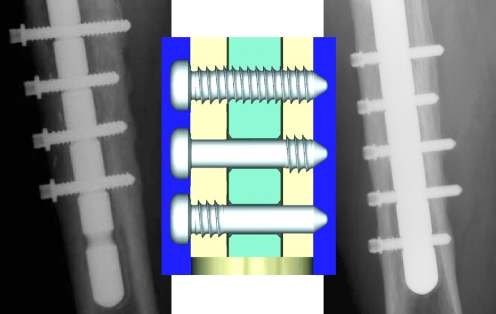
During the first period, 5-mm diameter titanium pegs with distal threads were used [1]. There were no breakages, but the lack of a collar caused subsiding defects. Fully titanium threaded screws, 5.5 mm in diameter with a collar, were later used but offered a little contact with the stem hole and had a low resistance to screw breakage with secondary stem subsidence. Practical and mechanical resistance studies led to the adoption of laterally threaded titanium screws (Fig. 2). Partially threaded screw offer better fit with the stem hole and a better resistance to breakage. Moreover, the lack of threading eliminates the risks of corrosion.
Fig. 2.
Screw evolution
Operative technique
Pre-operative planning should be performed to determine the appropriate stem and femoral deformities, with AP and sagittal X-rays. The use of the locking stem allows a trans-femoral approach, which necessitates adequate contact of the proximal femur with the stem coating. The femoral flap facilitates cement and implant removal, especially in cases of stem breakage, and allows stem extraction without hip dislocation in cases of severe stiffness or intra-pelvic migration [2].
In addition, the femoral flap permits a more thorough IM cleaning in cases of infection and creates a very good acetabular exposure for cup revision. In some cases of fractures, separation of the fracture fragments can be used to extract the stem and insert the locking stem.
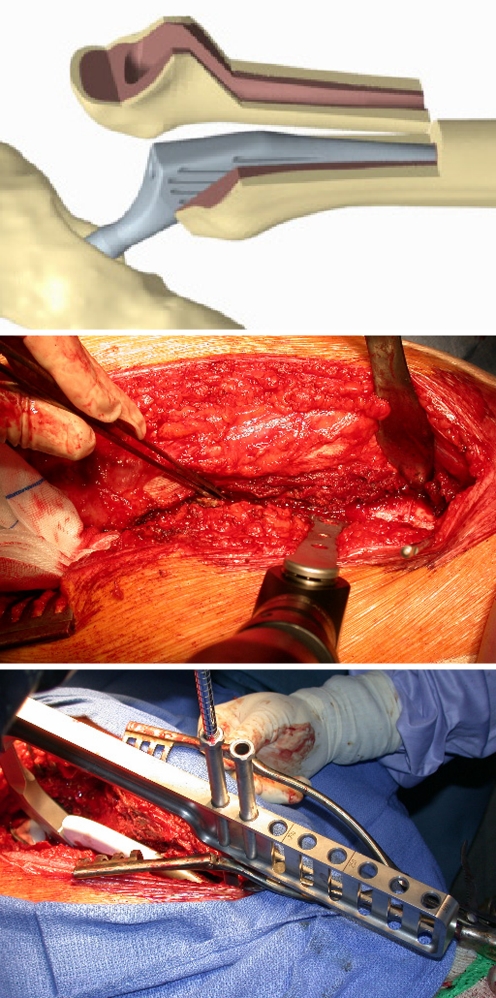
Transfemoral approach
Femorotomy should be planned on pre-operative X-rays to determine the length of the femoral flap. The distal part of the flap should be located at a distance of one femoral diameter from the first locking hole to prevent stem breakage. If the previous stem can be removed it will facilitate osteotomy. Elevation of vastus lateralis must be limited to avoid devascularising the femoral flap, with control of the perforating vessels to reduce bleeding. A retractor is inserted anterior to the femur at the distal limit of the planned flap to retract the vastus lateralis; at this point the lower limit is marked with a drill. To avoid a distal fracture insertion of a metallic wire just below the femoral flap is recommended. Femorotomy is undertaken in a sagital plane from the neck along the femoral axis, parallel to the distal drill. Longitudinal and distal cuts are performed with an oscillating saw (Fig. 3). A large Lambotte osteotome is introduced in the osteotomy and the femoral flap is carefully lifted and pushed forward. Removal of fibrous tissues or cement can be completed easily. If the initial stem cannot be extracted, the vastus lateralis can be detached from the sub-trochanteric crest to expose the antero-lateral face of the femur. Using an oscillating saw, a parallel cut is performed anteriorly. In these cases, the flap must extend beyond the stem tip.
Fig. 3.
Transfemoral approach and targeting
Prosthesis insertion
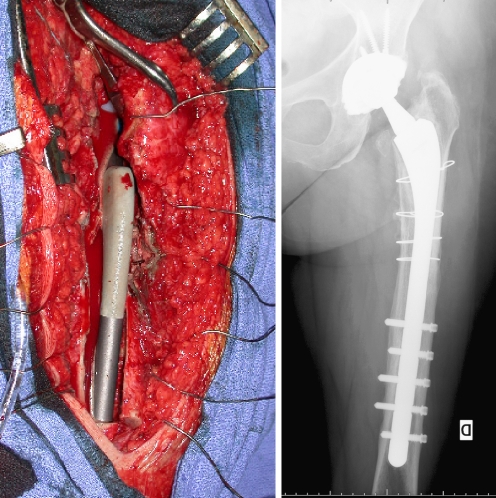
The intra-medullary canal is reamed progressively, millimeter by millimeter up to the diameter planned, to obtain, if possible, press-fit in the residual femur. The last reamer used should be rigid in cortical contact to determine the stem diameter. The prosthesis holder and targeting instrumentation are fixed to the stem and introduced into the canal without strong hammering. When adequate position in terms of length and anteversion is achieved, a clamp should temporarily fix the stem to the medial cortex. Before drilling a trial reduction should be performed to verify limb length. It is recommended to start locking from the most distal hole leaving the drill in situ to align the targeting device without any risk of distorsion. Targeting is carried out through aiming tubes. Usually, there are two drills: one short, 3.2 mm, to only penetrate the first cortex, avoiding the risk of skidding off the femur surface; and the other 5.5 mm, to penetrate the second cortex. All the screws are fitted in using the same technique. After removal of the prosthetic holder, the prosthetic head is impacted and reduced into the cup. After prosthetic holder removal, three to five steel wires, 2 mm in diameter depending of the length of the flap, are passed around the femur and around the flap. The femoral flap is reduced with a clamp and metallic wires are tightened on the lateral cortex of the femur (Fig. 4). Depending on the shape of the back of the stem, the greater trochanter may impinge against the stem and hinder an exact reduction; in this case, the thickness of the greater trochanter can be reduced as required with rongeurs. When the medial part of the femur remains too distant from the stem, an osteotomy of the medial cortex must be performed, at a different level of the lateral flap, to adjust the femoral canal to the stem diameter. Full weight-bearing is allowed post-operatively with crutches.
Fig. 4.
Femoral flap fixation
Experimental study
The experimental locking stem model built with finite elements was tested by two of the authors (PM, DVD) under eccentric loading of 300 daN. This model insures a security area with a minimal distance of two diameters. Standard tests demonstrated, first, slight stem sliding over the screw, and second, medial cortex contact and then distal locking. Undersizing the stem's diameter increases medial stresses on the stem, and if the first screw is missing, stresses are maximal at the level of the first hole, with a high risk of stem breakage.
Composite bone was used for the mechanical study with three different design studies: one with carefully closed lateral flap, one with segmental bone loss and one with total metaphyseal bone loss. In compression loading, severity of bone loss increases partial screw loading, and decreases rigidity of the proximal prosthetic femur. Distribution of partial screw loading is not predictable on different tests, with maximal loading observed on the first, second or third screw. Random position of the screw into the hole explains these results; thus, we advocate the use of a minimum of three screws. In rotation loading, a closed femoral flap improves stem stability, and decreases micro-mobility. To summarise, positioning the proximal cortex as close as possible to the proximal stem is important to decrease mechanical stresses applied to the stem and screws. The first screws must be inserted in all cases.
Population
In 2008, we retrospectively recorded data from 725 revisions with interlocking stem from 14 French orthopaedic departments and the results were presented during the French National Orthopaedic Meeting (SOFCOT). The average follow-up was 4.5 years (range, 1–15 years). A total of 260 patients had more than five years follow-up and 55 had more than eight years follow-up. Mean age at surgery was 68 years old. Four hundred and fifteen patients underwent revision surgery for the first time while 310 patients underwent iterative revision. Indications were 482 aseptic loosening, 150 periprosthetic fractures, and 93 septic loosening. Failed stems were cemented in 508 cases and cementless in 217 cases. Bone damage, with grading using the SOFCOT classification [3], demonstrated severe bone loss: 11% stage 4, 28% stage 3 and 40% stage 2. The majority of periprosthetic fractures (70%) were Vancouver B2 or B3 with loose implant [4].
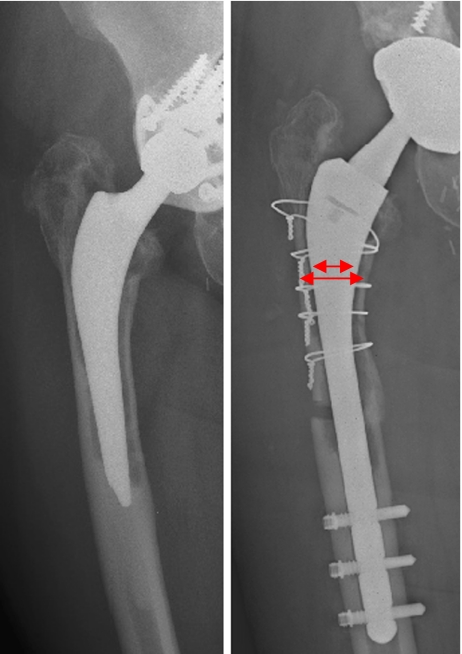
Seven different distal locked stems (Fig. 1) were used in this series: 205 straight stems with partial HAP coating (Ultime™) with modular neck, 405 curved stems with partial HAP coating (Aura™, DLS™, Linea™) and 115 curved stems with total HAP coating (Reef™, Rennaissance™, Extreme™). These last implants had metaphyseal/diaphyseal modularity. Stems had an average length of 240 cm (range, 150–360) and were locked with an average of three screws (range, 1–8). A trans-femoral approach was used in 529 revisions. Patients had a clinical and radiological evaluation at the latest follow-up. Clinical results were assessed using the Harris hip score, and radiological results were based upon stem migration and cortico-medullary index at metaphyseal and diaphyseal area. Morever, quality of the stem filling was studied with the ratio (Fig. 5) between stem diameter and femoral canal diameter 2 cm below the lesser trochanter, and was called the metaphyseal filling index (MFI). Failures were defined as stem/removal–replacement, stem revision, implant fracture, stem migration over 5 mm or extended osteolysis.
Fig. 5.
Metaphyseal filling index (MFI) stem diameter/canal diameter
Results
Regarding the clinical results, the mean Harris hip score at last follow-up was 81. The score therefore increased by an average of 31 points. However, no correlation could be established between the amount of femoral defect and the amount of clinical improvement. With regard to patient subjective evaluation, most were very satisfied or satisfied and only 3.6 % were not satisfied. Among these 26 patients, 21 experienced failure of their revision surgery.
With regard to thigh pain at the last follow-up, most patients reported no pain, 16.5 % experienced thigh pain under stress and 4.5 % had incapacitating pain. Among these 31 patients, 27 sustained a failure of their interlocked stem. The results of septic loosening were basically the same as that for aseptic loosening, but with low rate of sepsis recurrence (7%). In cases of peri-prosthetic fractures, fracture union was obtained in 95% of cases, but thigh pain was present in 20% of patients. Advantages of the locking stem in peri-prosthetic fracture are the high rate of fracture healing, with immediate weight bearing, and without subsidence of the stem.
Bone reconstruction was assessed on cortico-medullary index in the metaphyseal area and at mid-shaft increasing from 36 to 45 and 54 to 63, respectively. Radiologically, 637 implants were stable, and 40 demonstrated subsidence. Forty eight have been revised.
The overall rate of intra-operative fractures in this series was 14%, mainly including metaphyseal and flap fractures, easily fixed with wires or cables. There was significant difference between the approaches, with twice the risk of distal fracture or cortical perforation without a femoral flap. There was no difference between straight and curved stems. The overall rate of screw breakage was 4%. The use of lateral threaded screws reduced this risk significantly. There was a strong correlation between diameter less than 5 mm and the risk of breakage. Screw breakage was significantly associated with age under 70 years and use of a straight collarless stem with reduced coating (p < 0.05). A low metaphyseal filling index increases the risk of locking failure (p < 0.0001). The rate of stem breakage was low at 1.4%; a high correlation with the type of stem can be detected, with eight failures affecting the first generation of straight non coated stem. In all cases breakage occurred at the first hole level. Other statistical tests demonstrated no correlation between the risk of material failure and patient weight, severity of bone loss, immediate weight bearing or the use of a femoral flap. Distal screws were removed in 63 cases for complication such as thigh pain or migration, but also as a routine for some surgeons. In these cases, screws were removed earlier. No correlation was detected with the type of approach. After screw removal, 21 stems demonstrated subsidence with a migration over 10 mm, and 13 needed recurrent revision surgery. Twenty-seven locked stems had to be exchanged for a standard stems because of thigh pain, and 21 were revised using other revision stems. Thigh pain or screw breakage were associated with a high risk of unstable stem. The survival rate was 96% at ten years using the revision of femoral component for loosening as the end point, and 93% using revision of the femoral component for any reason as the end point.
It is interesting to analyse the relation between the metaphyseal filling index and the stability of the stem and the quality of bone reconstruction. In cases of filling index under 75%, there were ten times more broken screws and stem subsidence (p < 0.001). The improvement of metaphyseal bone quality was significantly higher when the filling index was superior to 75% (p < 0.001). On the other hand there was no correlation with the diaphyseal filling index. A logistic regression model was developed and applied to all explanatory variables; it appears that whatever the type of failure, a high post-operative metaphyseal filling index is a predictive factor of success. Finally, a thorough analysis of the transfemoral approach significantly reveals the favourable influence of osteoclasis combined with femoral flap on the metaphyseal index compared to an isolated femoral flap. Better results are achieved when performing osteoclasis which provides a close contact between living bone and HA coating.
Results were analysed with respect to three groups of stem; group 1 used a straight, partially HA-coated implant (Ultime™); group 2 used a curved, fully HA-coated implant (Reef™, Renaissance™, Extreme™); and group 3 used a curved, partially-coated implant ( DLS™, Aura™,Linea™). When considering implant status at last follow-up, group 1 reported a significantly higher rate of failure when compared with the others types of implants (p < 0.0001). Group 2 reported better functional results than group 3 (p < 0.007), which in turn reported better results than group 1 (p < 0.0001). Concerning implant fixation, group 2 reported significantly better results (p < 0.0001). Both groups 2 and 3 experienced less thigh pain than group 1 (p < 0.0001).
Discussion
In cases of femoral loosening, results of cemented revisions of femoral components were unpredictable, and the intermediate results were discouraging [5, 6]. These poor results with cemented revisions have led investigators to explore cementless options [7–9]. However, in the revision setting, the proximal femur is often deficient and provides a poor biological and mechanical environment for proximal porous ingrowth; in cases of pronounced bone defect and deficient isthmus, distal fixation of an extensively porous-coated implant is unable to provide primary stability [10]. Although the overall femoral mechanical loosening rate was 10%, a number of other complications, including intra-operative fractures (28%) and thigh pain (25%) were noted [11]. Recent assessment of the Wagner stem pointed out a significant rate of claudication and dislocation due to the design and frequent limb discrepancy [12]. In addition, the distal fixation of an extensively porous-coated implant comes at the expense of proximal stress-shielding. In such cases, Courpied et al. [13] recommend the use of bulk cortical allograft with cemented stem for femoral reconstruction in order to restore bone capital and initial stem stability. Results demonstrated only four cases of failure in 44 reconstructions, but authors recommend the use of an additional trochanteric claw plate to improve final hip stability [14].
Another possible option for achieving initial stability of the femoral component is to fix it with distal interlocking screws. These screws can provide axial and rotational stability; in addition, if such a stem requires a further revision, it will be removed more easily and cause less bone loss compared with the extensively porous-coated stems. Mahomed et al. [15] reported that distal interlocking increased the torsional stability by 320% and the axial stability by 230%. However, they concluded that interlocking screws have only an additional effect and can never be used alone to stabilise the stem. This statement is supported by our data and by the study of Storeanos et al. [16] demonstrating the role of femoral canal filling. Initially, the cumulative survival of a non coated straight stem (Kent™) at five, ten and 15 years was 93%, 89% and 77%, respectively. In patients aged more than 70 years, the cumulative survival at 15 years was 92%, compared with 68% in those aged less than 70 years [17].
Kim et al. [18] reported early good results of 68 consecutive revisions using a cementless distal interlocking femoral stem. Harris score improved to 88 points; no osteolysis and no radiological loosening were noted. No repeat revision was needed during the follow-up period of 40 months. In a series of 43 total hip revisions using a distal interlocking fully HA-coated curved stem, Philippot et al. [19] noted only one long-term failure at 58 months follow-up. More recently, Fink et al. [20] designed a prospective study of 15 revisions with a defective isthmus, using a cementless distal curved component with additional distal interlocking screws. During a short follow-up period of 35 months, there was one stem loosening related to screw breakage in a case of a stem that was too thin. Bony ingrowth fixation occurred in 12 cases, and stable fibrous fixation in two cases. Harris hip score rose to 75. These results demonstrated efficiency of this concept. The locking mechanism increases primary stability required for the bone ingrowth, even in cases of severe bone loss, especially if bone loss spreads to the femoral isthmus. Prevention of subsidence and rotation of the stem inside the femur is evident.
Management of peri-prosthetic fractures can be difficult. Among these, type B fractures represent approximately 80% of all cases [21]. Type B2 where the stem is loose are harder to manage. But the most difficult cases are type B3 where the stem is loose with an extremely poor bone stock proximally [22]. From a clinical point of view, there are two main issues: first, that the fracture heals and second, that the prosthesis does not fail. Locking plates or cable do not prevent the stem subsidence and crack opening [23]. The easiest and most common treatment method for this is revision of the stem with an extensively coated device that allows the creation of an intramedullary rod-type effect from the stem [24]. The essential feature of this technique is to bypass the fracture site through a press fit of the distal part of the stem into the intact femur. If this is not achievable, it may not be appropriate to use this technique. In addition, distal press-fit fixation increases the proximal stress shielding and the risk of fracture non union. In such cases distal locked stems may be preferred to achieve a strong initial fixation allowing weight bearing and secondary bone ongrowth at the site of the fracture [25]. Nevertheless, Learmonth [26] reported breakage of the screws in five of 22 peri-prosthetic fractures treated with interlocking stem, because the stem was too thin.
The trans-femoral approach should be performed to simplify stem removal, complete femoral cleaning and to reduce the rate of intra-operative complications. The trans-femoral approach also has biological advantages, it stimulates bone reconstruction and allows adaptation to the stem to obtain an extensive contact between the stem and the living bone. More recently, some authors have described this approach as “extended trochanteric osteotomy” [27, 28]. In our series bone reconstruction was assessed on improvement of cortico-medullary index at the metaphyseal area and demonstrated constant augmentation; no correlation could be established with severity of SOFCOT grading. In a series of 17 patients using long HA-coated interlocking stems, Malhotra et al. [29] noted bone ingrowth in 83% of cases and no stem required revision at a minimum 27 months follow-up. Volkmann et al. [30] observed restoration and reorganisation of proximal bone stock about the 109 first Bicontact™ prosthesis used for high grade femoral defects with an average 5.5 years.
To summarise, use of the distal locking stem achieves an easy and strong initial fixation even in cases of severe bone loss. Likewise, the stems enhance bone growth and reconstruction, without addition of bone grafting. Subsequent secondary bone ongrowth is encouraged by transfemoral approach and medial osteoclasis, and a full coated stem. Distal locked stems are mainly indicated to treat complex femoral revision (grade SOFCOT 3 or 4) and peri-prosthetic fractures.
References
- 1.Vives P, Plaquet JL, Leclair A, Blejwas D, Filloux JF. Tige de reprise verrouillée pour descellement des prothèses totales de hanche. Conception. Résultats préliminaires. Acta Orthop Belg. 1992;59:28–35. [PubMed] [Google Scholar]
- 2.Picault C. Transfemoral approach and distally locked stem. France: Sauramps Editor; 1999. Technique of trans-femoral approach for removal of a failed implant of total hip prosthesis and its replacement with a cementless distally locked stem; pp. 41–51. [Google Scholar]
- 3.Vives P, Lestang M, Paclot P, Cazeneuve JF. Le descellement aseptique: definitions, classifications. Rev Chir Orthop. 1989;75:29–31. [Google Scholar]
- 4.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 5.Eisler T, Svensson O, Iyer V, et al. Revision total hip arthroplasty using third generation cementing technique. J Arthroplasty. 2000;15:974–981. doi: 10.1054/arth.2000.9825. [DOI] [PubMed] [Google Scholar]
- 6.Schmale GA, Lachiewicz PF, Kelly SS. Early failure of revision total hip arthroplasty with cemented precoated femoral components: comparison with uncemented components at 2 to 8 years. J Arthroplasty. 2000;15:718–729. doi: 10.1054/arth.2000.6623. [DOI] [PubMed] [Google Scholar]
- 7.Weeden SH, Paprosky WG. Minimal 11 years follow-up of extensively porous coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17:134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]
- 8.Moreland JR, Moreno MA. Cementless femoral revision arthroplasty of the hip: minimum 5 years follow-up. Clin Orthop. 2001;393:194–201. doi: 10.1097/00003086-200112000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Gosens T, Langelaan EJ. Clinical and radiological outcome of hydroxyapatite-coated femoral stem in revision hip arthroplasty. Int Orthop. 2005;4:219–223. doi: 10.1007/s00264-005-0659-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cameron HU. The long term success of modular proximal fixation stems in revision total hip arthroplasty. J Arthroplasty. 2002;17:138–141. doi: 10.1054/arth.2002.32462. [DOI] [PubMed] [Google Scholar]
- 11.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10 year-results of extensively porous coated stems in revision hip arthroplasty. Clin Orthop. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 12.Boisgard S, Moreau PE, Tixier H, Levai JP. Reconstruction osseuse, inégalité de longueur des membres, taux de luxation de 52 prothèses de Wagner, en révision d’arthroplasties totales de hanche au recul moyen de 44 moi. Rev Chir Orthop. 2001;87:147–154. [PubMed] [Google Scholar]
- 13.Courpied JP, Postel M.Allogreffes massives pour reconstruction de la diaphyse fémorale Rev Chir Orthop 198975suppl 153–54.2660202 [Google Scholar]
- 14.Vastel L, Lemoine CT, Kerboull M, Courpied JP. Structural allograft and cemented long-stem prosthesis for complex revision hip arthroplasty: use of a trochanteric claw plate improves final hip function. Int Orthop. 2007;6:851–857. doi: 10.1007/s00264-006-0275-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahomed N, Schatzker J, Hearn T. Biomechanical analysis of a distally interlocked press-fit femoral total hip prosthesis. J Arthroplasty. 1993;8:129–132. doi: 10.1016/S0883-5403(06)80051-3. [DOI] [PubMed] [Google Scholar]
- 16.Storeanos N, Sweschke J, Raukear GJ, et al. Revision total hip arthroplasty with a custom cementless stem with distal cross-locking screws. Early results in femora with large proximal segmental deficiencies. J Bone Joint Surg Am. 2006;88:1709–1084. doi: 10.2106/JBJS.E.00141. [DOI] [PubMed] [Google Scholar]
- 17.Sexton SA, Stossel CA, Haddad FS. The Kent hip prosthesis: an evaluation of 145 prostheses after a mean of 5.1 years. J Bone Joint Surg Br. 2006;88:310–314. doi: 10.1302/0301-620X.88B3.17087. [DOI] [PubMed] [Google Scholar]
- 18.Kim YM, Kim HJ, Song WS, Yoo JJ. Experiences with the Bicontact revision stems with distal interlocking. J Arthroplasty. 2004;19:27–34. doi: 10.1016/j.arth.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 19.Philippot R, Delangle F, Verdot FX, Farizon F, Fessy MH. Femoral deficiency reconstruction using a hydroxyapatite-coated locked modular stem. A series of 43 total hip revisions. Orthop Traum Surg Res. 2009;95:119–126. doi: 10.1016/j.otsr.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Fink B, Grossmann A, Fuerst M. Distal interlocking screws with a modular revision stem for revision total hip arthroplasty in severe bone defect. J Arthroplasty. 2010;25:759–765. doi: 10.1016/j.arth.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Corten K, Vanrykel F, Bellemans J, et al. An algorithm for the surgical treatment of periprosthetic fractures around a well-fixed femoral component. J Bone Joint Surg Am. 2009;91:1424–1430. doi: 10.2106/JBJS.H.01335. [DOI] [PubMed] [Google Scholar]
- 22.Lindahl H, Malchau H, Oden A, Garellick G. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br. 2006;88B:26–30. doi: 10.1302/0301-620X.88B1.17029. [DOI] [PubMed] [Google Scholar]
- 23.Tsiridis E, Haddad FS, Gie GA. Dall-Miles plates for periprosthetic femoral fractures. A critical review of 16 cases. Injury. 2004;34:107–110. doi: 10.1016/S0020-1383(02)00161-4. [DOI] [PubMed] [Google Scholar]
- 24.Rosenberg A. Managing periprosthetic femoral stem fractures. J Arthroplasty. 2006;21:101–104. doi: 10.1016/j.arth.2006.02.167. [DOI] [PubMed] [Google Scholar]
- 25.Migaud H, Gabrion A, Mertl P. Distally locked stem for complex femoral revision. Oper Tech Orthop. 2004;14:130–136. doi: 10.1053/j.oto.2004.03.002. [DOI] [Google Scholar]
- 26.Learmonth ID. The management of periprosthetic fractures around the femoral stem. J Bone Joint Surg Br. 2004;86:13–19. [PubMed] [Google Scholar]
- 27.Chen WM, McAuley JP, Engh CA, Jr, et al. Extended slide trochanteric osteotomy for revision total hip arthroplasty. J Bone Joint Surg Am. 2000;82:1215–1219. doi: 10.2106/00004623-200009000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Miner TM, Momberger NG, Chong D, et al. The extended trochanteric osteotomy in revision hip arthroplasty: a critical review of 166 cases at mean 3 year 9 months follow-up. J Arthroplasty. 2001;16:188–194. doi: 10.1054/arth.2001.29385. [DOI] [PubMed] [Google Scholar]
- 29.Malhotra R, Dua A, Kiran EK, Bhan S. Femoral revision using long hydroxyapatite-coated interlocking stem. Arch Orthop Trauma Surg. 2008;128:355–362. doi: 10.1007/s00402-007-0334-7. [DOI] [PubMed] [Google Scholar]
- 30.Volkmann R, Bretschneider C, Eingartner C, Weller S. Revision arthroplasty-femoral aspect: the concept to solve high grade defects. Int Orthop. 2003;27(suppl 1):S24–S28. [PubMed] [Google Scholar]