Abstract
Advances in surgical technique and implant technology have improved the ten-year survival after primary total hip arthroplasty (THA). Despite this, the number of revision procedures has been increasing in recent years, a trend which is predicted to continue into the future. Revision THA is a technically demanding procedure often complicated by a loss of host bone stock which may be compounded by the need to remove primary implants. Both cemented and uncemented implant designs are commonly used in the United Kingdom for primary and revision THA and much controversy still exists as to the ideal method of stem fixation. In this article we discuss revision of the femur using cemented components during revision THA. We focus on three clinical scenarios including femoral cement-in-cement revision where the primary femoral cement-bone interface remains well fixed, femoral cement-in-cement revision for peri-prosthetic femoral fractures, and femoral impaction grafting. We discuss the clinical indications, surgical techniques and clinical outcomes for each of these procedures.
Introduction
Primary THA may require revision surgery for a number of reasons including aseptic osteolysis/loosening, sepsis, instability, peri-prosthetic fracture, pseudo-tumour and pain [1]. Revision THA presents a number of technical difficulties to the arthroplasty surgeon, often due to loss of host bone stock and the need to remove the primary implant. Both cemented and uncemented implants are commonly used for primary THA in the United Kingdom, although currently cemented components remain more popular [1]. Removal of well-fixed cement risks further loss of host bone stock, cortical perforation and fracture. It is also a time-consuming technique which is technically demanding. In this manuscript we will discuss revision of the femur using cemented components with respect to three different clinical scenarios:
Femoral cement-in-cement revision where the primary femoral cement-bone interface remains well fixed
Femoral cement-in-cement revision for peri-prosthetic femoral fractures
Cemented femoral components and femoral impaction grafting
Femoral cement-in-cement revision where the primary femoral cement-bone interface is well fixed
The removal of well fixed polymethylmethacrylate (PMMA) bone cement is a technically challenging and time consuming process which risks fracture/perforation of the femur during revision total hip arthroplasty (THA). The logic of this practice was first questioned by Greenwald et al. who advocated the retention of a well-fixed cement mantle and re-cementation of a new component into the existing mantle [2]. When the existing mantle was prepared by drying and rasping, shear strength was 94% that of a single cement block. The shear strength was found to be maximal when the cement was added early, which was attributed to the increased availability of free monomer, promoting polymerisation with the existing cement mantle. It was suggested that rasping the surface of the existing cement mantle helped to clean the surface and possibly expose residual activator/monomer in addition to providing a surface for improved mechanical interlock. Although this practice has been questioned in the orthopaedic literature, further biomechanical and clinical studies have supported the use of this technique in appropriate circumstances [3–6]. Lieberman et al. reported a series of 19 patients with no femoral stem loosening at a mean follow-up of five years [4]. Rosenstein et al. measured the interference shear strength of cement in samples from human femora and found that in all cases the shear strength of the cement–cement interface was greater than that of the cement–bone interface [5]. Indeed, the cement–bone interfaces were 30% weaker when fresh cement was placed against a revised bare bone surface. Such findings support the retention of well-fixed cement rather than its removal and re-cementation.
Since 1989 it has been routine practice in Exeter to perform cement-in-cement femoral revision for cases in which the femoral cement mantle is well fixed both clinically and radiologically. Indications for this technique include removal of the femoral stem to improve access when revising the acetabular component, exchanging a monoblock stem with a damaged head or a modular stem with a damaged/incompatible taper, altering the version of the femoral component in cases of recurrent instability, altering leg length for discrepancy, replacing the component for fracture of the stem, altering femoral offset, or for loosening at the prosthesis–cement interface.
Operative technique [7, 8]
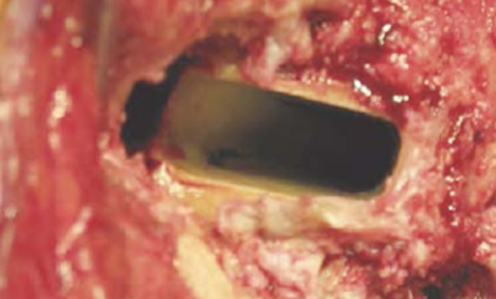
The proximal cement above the shoulder of the prosthesis must be removed using a burr or osteotome before extracting the stem with a punch (Fig. 1). A collarless, polished, tapered stem is relatively straightforward to remove and lends itself to this technique. Collared, curved and matt surfaced stems can also usually be extracted from within the cement mantle by removing more of the lateral proximal cement.
Fig. 1.
The stem is removed with a punch after any cement over the shoulder has been removed. Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
The femoral neck is then re-cut 2–3 mm below the existing cut if necessary to allow the cement–bone interface to be carefully inspected (Fig. 2). Any small loose fragments of cement above the level of the lesser trochanter should be removed. The cement-in-cement technique should be abandoned for another more appropriate method of revision if there is soft tissue at the cement–bone interface which extends distally, if the cement mantle is loose below the lesser trochanter, or if there is loss of host bone.
Fig. 2.
The cement mantle and cement–bone interface are carefully assessed. Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
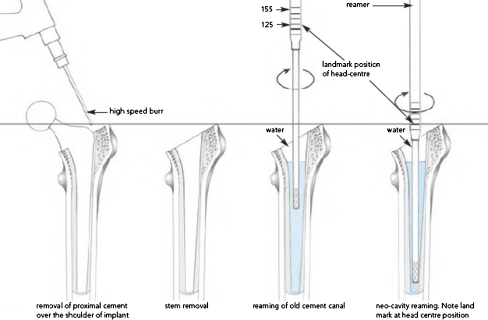
A trial stem of appropriate length, offset and version is then chosen to fit inside the existing cement mantle. In cases in which the stem version has to be altered, considerable cement may have to be burred away proximally to allow the stem to rotate within the mantle. In some cases, the distal cement mantle must also be expanded by a few millimetres with a cylindrical reamer to allow rotation of the stem (Fig. 3).
Fig. 3.
Preparation of the femur for stem removal and reaming of the existing cement mantle to facilitate new stem insertion. Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
Once an adequate trial reduction has been achieved and the position of the stem marked, the mantle is prepared by washing and drying. Fresh PMMA cement (Simplex) is then introduced in a retrograde manner into the old canal, using a cement gun with a narrow (revision) nozzle (Fig. 4).
Fig. 4.
New cement is inserted into the old cement mantle. Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
It is then pressurised and the new stem inserted in the normal manner. In most cases we use an Exeter stem with the same offset as the stem that has been removed but with a slimmer body (Fig. 5).
Fig. 5.
The new stem is inserted. Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
When inserting the new stem, it is essential to ensure that it is properly supported proximally to at least the lowest of the three marker rings on the stem.
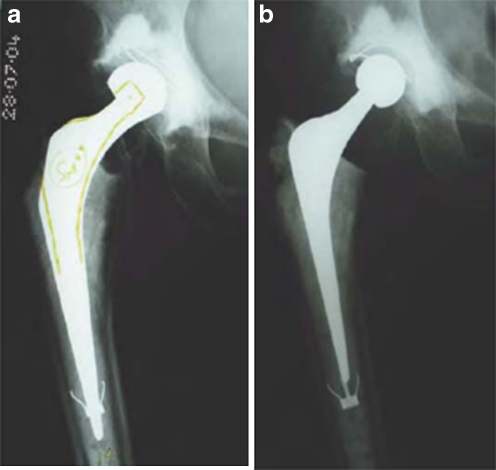
The 125-mm long 44-mm offset cement-in-cement revision stem was introduced in 2006. It is 25 mm shorter than a standard Exeter stem but, unlike the other smaller stems in the Exeter range, retains an offset of 44 mm. It is also slimmer both distally and front to back than a standard stem. It will, therefore, fit inside the cement mantle of any of the 44- or 50-mm offset stems in the range, and into that of the 37.5-mm stems with minor burring of the proximal cement mantle. Its short length also means that it will fit into the mantle of almost all commonly used cemented stems without the need to extend the cavity in the mantle distally (Fig. 6).
Fig. 6.
Before (a) and after (b) cement-in-cement acetabular and femoral revision for instability. The monoblock femoral component was revised to facilitate exposure, because of head size incompatibility and to allow for increase in offset. Note that the femoral neck was re-cut to allow careful inspection of the cement mantle. The 125-mm short 44-mm offset cement-in-cement revision stem has been used in this case, avoiding the need to remove the old metal centraliser from the original cement mantle. Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
Clinical results
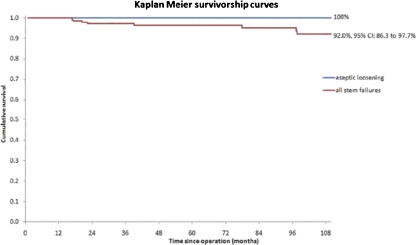
Duncan et al. reviewed the outcome after femoral cement-in-cement revision in Exeter [6]. One hundred thirty-six cement-in-cement femoral revisions in 134 patients performed between 1989 and 1999 with complete clinical and radiological follow-up at a minimum of five years (range five to 15 years, mean eight years) were reviewed. The indication for surgery for the total cohort was acetabular component failure/loosening in 75%, recurrent dislocation/subluxation in 15%, sepsis in 6%, access for removal of ectopic bone in 2%, and peri-prosthetic fracture in 2%. The cement-in-cement revision was the first revision in 102/136 cases (75%), the second in 24/136 (17.6%), the third in 4/136 (2.9%), the fourth in 1/136 (0.7%) and a second-stage procedure for infection in 5/136 (3.7%). The mean follow-up was eight years (range five to 15 years). At the most recent review, no stem has had to be revised for aseptic loosening and no stem was radiologically loose. The Kaplan Meier survival for this group was therefore 100% (95% CI 91.4–100). The survival rate for revision for all causes (aseptic loosening, fracture of the stem, peri-prosthetic fracture, infection and dislocation) was 92.0% (95% CI 86.3–97.7; Fig. 7).
Fig. 7.
Kaplan Meier cumulative survival curves for aseptic loosening and stem revision for any reason (aseptic loosening, fracture, infection and dislocation). Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
Marcos et al. reported clinical and radiological outcomes using the cement-in-cement femoral revision technique [9]. Between 1999 and 2005, 37 aseptic revision procedures were performed in 35 patients with an average age of 68 years. The reasons for revision included femoral stem fracture, cup failure, acetabular protrusion after hemi-arthroplasty and recurrent dislocation. At a mean follow-up of 46 months, none of the patients required further femoral revision. The average post-operative Merle D’Aubigne score was 16.6 points (p < 0.05). No evidence of radiological stem failure was observed and no femoral component was considered to be at risk for loosening.
The encouraging outcome of these cases has prompted a widening of the indications for cement-in-cement revision of the femur in Exeter.
Cement-in-cement revision for femoral peri-prosthetic fracture
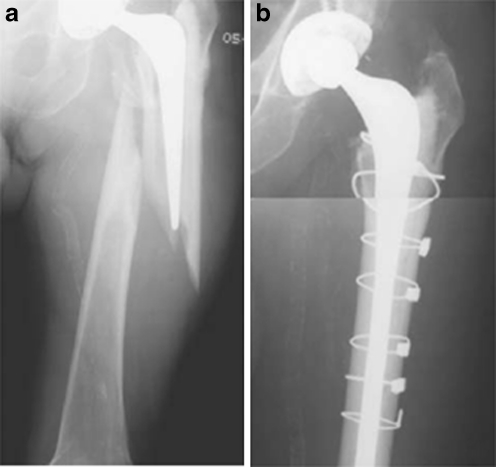
Revision surgery for peri-prosthetic femoral fractures in the presence of an unstable cemented femoral stem traditionally requires removing both the stem and all existing cement. However, in situations where the femoral cement remains well-fixed to the bone fragments, even though the femur is fractured and the stem is now “loose” (Vancouver B2), in selected cases we have retained the cement–bone interface and existing cement and performed a cement-in-cement revision after reducing and stabilising the fracture (Fig. 8).
Fig. 8.
Before (a) and after (b) cement-in-cement revision of a Vancouver B2 peri-prosthetic femoral fracture to a long-stem prosthesis. Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
This technique is particularly applicable to non-comminuted fractures that can be reduced anatomically after removal of the now loose stem [10]. Concern has been expressed that cemented revision in such cases will promote fracture non-union due to interposition of cement between the fracture fragments [11]. The traditional technique, therefore, is to remove the femoral cement to allow insertion of a distally fixed uncemented stem. However, removal of well-fixed cement from the fracture fragments risks further loss of bone stock and comminution of the proximal femur. It is much less destructive and time-consuming to retain the well-fixed cement, only burring away sufficient to allow insertion of a new long cemented stem following fracture reduction, observing the well proven principles of the cement-in-cement femoral revision technique.
Briant-Evans et al. reported the outcomes of 23 Vancouver type B2 peri-prosthetic femoral fractures (between 1995 and 2005) treated by reducing the fracture and cementing a revision stem into the pre-existing cement mantle, with or without supplementary fixation [10]. Three of 23 (13%) patients died in the first six months for reasons not related to surgery, one of 23 (4%) was too frail to attend follow-up and was, therefore, excluded from the study and one of 23 (4%) underwent revision surgery for a non-union. The remaining 18 (78%) cases all healed with radiographic union after a mean of 4.4 months (range 2–11 months). There was no evidence of lysis/loosening or subsidence of the revision stems within the old cement mantle in any of these cases at most recent follow-up after a mean of three years (range 0.3–9.3 years). These results compare favourably with those of other more established techniques and support the use of the cement-in-cement revision in anatomically reducible peri-prosthetic fractures with a well-preserved pre-existing cement mantle. Although a theoretical concern of the use of cemented stem fixation in this small series of selected cases did not adversely affect fracture union, indeed the union rate was comparable or better than other published series using techniques without the use of cement. Due to the time saved by avoiding cement removal, the reduction in bleeding from the exposed bone bed due to the retention of the cement mantle and by avoiding the risk of further damage to what is often weak osteoporotic bone, this technique is particularly useful for the elderly patient and those not fit for prolonged surgical procedures.
Femoral impaction grafting
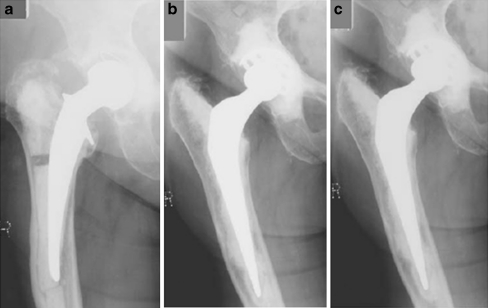
Femoral impaction grafting with a cemented femoral prosthesis was first performed in Exeter in 1987 (Fig. 9). This technique of bone restoration during revision THA has proven to be highly successful [12–17]. In 1993, Gie et al. reported the initial experience of 56 revision procedures with follow-up of 18–49 months [12]. Encouraging results were reported and it was evident that the technique allowed for restoration of femoral bone stock as the impacted femoral allograft was subsequently incorporated and remodelled by the host skeleton.
Fig. 9.
First case of impaction grafting: pre-op (a), post-op (b) and at five years (c). Reproduced with permission and copyright© of the Exeter Hip Unit, Princess Elizabeth Orthopaedic Hospital
This initial success stimulated the development of specialised instruments and implants such as femoral meshes, the long stems (introduced in 1992) and the 205-mm fully tapered stem (introduced in 1998). Such advances permitted application of the technique to more difficult cases.
Clinical results
Halliday et al. published the results of femoral impaction grafting performed at Exeter with a minimum follow-up of five years [15]. This series of 226 revision hip operations in 207 patients included all cases performed during the initial experience described with impaction grafting, for whom dedicated instruments were not available, in addition to the results of cases performed using the first generation of instruments (none received long-stemmed prostheses as they were not available at that time).
Five of 226 (2.2%) patients underwent reoperations for deep infection. A further 12 of 226 (5%) femoral re-operations were performed for fracture (ten of 12) and aseptic loosening (two of 12). A further four of 226 (2%) patients were deemed to have failed clinically or radiologically but were unfit for/did not wish further surgery. The overall rate of aseptic loosening including reoperation for fracture or mechanical loosening including those designated as failures which did not undergo further surgery was therefore 7% (16/221). Survivorship at ten to 11 years with revision of the femur for any reason as the endpoint was 90.5%. Survivorship with revision for aseptic loosening as the endpoint was 99.1%. Radiological review demonstrated cortical healing in 87% of the femoral zones that had previously shown loss of cortical bone, illustrating the value of femoral impaction grafting in its ability to restore bone stock. However, the authors highlighted the incidence of post-operative fractures and recommended use of long-stemmed prostheses for more challenging cases with distal femoral bone loss.
There are now a number of reports in the literature that have reproduced the results of the Exeter group. Schreurs et al. published their results of 33 cases of femoral impaction grafting with a cemented polished tapered stem at a mean of 10.4 years. Radiographic analysis demonstrated that none of the cement mantles had migrated within the femur. None of the femoral components had required revision. Three post-operative femoral fractures occurred all at the tip of the femoral prosthesis through a segmental bone defect that had been present at the time of the revision operation. All three fractures were treated successfully with plate fixation and further femoral revision was not required.
Wraighte et al. also reported similar results in a series of 75 patients reviewed at a mean of 10.5 years [13]. Radiological review showed good evidence of femoral bone stock reconstitution and survivorship for any femoral re-operation was 92%.
Finally, long-term follow up data from the Swedish registry for femoral impaction grafting with the Exeter stem has been reported by Ornstein et al. [16]. This series included 1,305 procedures performed in 1,188 patients with follow-up between five and 18 years. Among this large number of cases only 70 further revisions were performed. Thirty-three re-operations were performed for infection or fracture, 13 for subsidence and 11 for aseptic loosening. Late failure in this series was rare with 65/70 re-operations preformed within 48 months of the initial revision procedure. The survivorship at 15 years (for all causes of failure) was 94%.
Discussion
Nearly five decades of technological and surgical innovation has resulted in improved implant survival in patients undergoing primary THA [18]. Despite this, the number of revision procedures has been increasing in recent years, a phenomenon which is predicted to continue into the future [19]. Revision THA frequently presents a substantial technical challenge for the arthroplasty surgeon due to loss of host bone stock and the need to remove the primary implant. Removal of well-fixed femoral cement risks bone loss, cortical perforation and fracture, also it is time-consuming and technically demanding. To remove sufficient cement to allow the insertion of an uncemented component often requires an extended trochanteric osteotomy or cortical window, which in turn demands long-stemmed, distally fixed components. This extends the ‘zone of injury’ from the implant further down the femoral canal and increases the difficulty of any subsequent revision procedures in the future. All of these problems can be avoided by using the cement-in-cement technique, making it a quick, versatile and attractive option. A collarless, polished, tapered stem lends itself to cement-in-cement revision and effectively makes the stem modular at the stem–cement interface. This enables the surgeon to alter stem offset, version and the depth of insertion, which allow the stem to be adjusted for maximum stability and appropriate leg length at the time of acetabular revision. Concern has been expressed in the past about the durability of this technique [3]; however, our findings agree with those of others, all of whom have recorded good results with durable fixation and a low failure rate in the short/medium term [4, 20]. In the light of these favourable results the original indications for this procedure have now been expanded to include the treatment of Vancouver B2 peri-prosthetic fractures in cases where the cement bone interface is well fixed and the fracture reducible with encouraging short- to mid-term results.
One issue of concern when using the technique of cement-in-cement revision of the femur, particularly if done simply to facilitate acetabular revision, is that coarse analysis of joint registry data will show prejudice against stems removed for cement-in-cement revision. The National Joint Registry of England and Wales no longer includes data sets that recognise both femoral and acetabular cement-in-cement revision [1]. This is also a weakness of other national joint registries. It is therefore essential that this technique be correctly registered when comparative data are being analysed if accurate conclusions regarding primary implant survival are to be drawn.
Impaction grafting of the femur has been demonstrated to be an effective means of restoring bone stock during femoral revision [12–17]. It also allows fixation in wide, patulous or “drain pipe” femora which may be difficult or impossible with other techniques. Although more time consuming and more technically challenging than the alternative surgical option of using a distally fixed, uncemented stem, it has the inherent advantage of restoring host bone stock which is of particular importance in younger patients who may require further revision surgery in the future. Each revision THA presents its own unique challenges and the arthroplasty surgeon must be equipped with a range of skills, including familiarity with the techniques described above, if they are to deal effectively with these demanding cases.
References
- 1.National Joint Registryfor England and Wales. Available at: http://www.njrcentre.org.uk/NjrCentre/LinkClick.aspx?fileticket=EuUKuR4jPyc%3d&tabid=86&mid=523. Accessed 16 November 2010
- 2.Greenwald AS, Narten NC, Wilde AH. Points in the technique of recementing in the revision of an implant arthroplasty. J Bone Joint Surg Br. 1978;60(1):107–110. doi: 10.1302/0301-620X.60B1.627570. [DOI] [PubMed] [Google Scholar]
- 3.Li PL, Ingle PJ, Dowell JK. Cement-within-cement revision hip arthroplasty: should it be done? J Bone Joint Surg Br. 1996;78(5):809–811. [PubMed] [Google Scholar]
- 4.Lieberman JR, Moeckel BH, Evans BG, Salvati EA, Ranawat CS. Cement-within-cement revision hip arthroplasty. J Bone Joint Surg Br. 1993;75(6):869–871. doi: 10.1302/0301-620X.75B6.8245073. [DOI] [PubMed] [Google Scholar]
- 5.Rosenstein A, MacDonald W, Iliadis A, McLardy-Smith P. Revision of cemented fixation and cementbone interface strength. Proc Inst Mech Eng H. 1992;206(1):47–49. doi: 10.1243/PIME_PROC_1992_206_261_02. [DOI] [PubMed] [Google Scholar]
- 6.Duncan WW, Hubble MJW, Howell JR, Whitehouse SL, Timperley AJ, Gie GA. Revision of the femoral stem using a cement-in-cement technique: a five- to 15-year review. J Bone Joint Surg Br. 2009;91(5):577–582. doi: 10.1302/0301-620X.91B5.21621. [DOI] [PubMed] [Google Scholar]
- 7.Ling RSM, Lee AJC, Gie GA, Timperley AJ, Hubble MJW, Howell JR, Whitehouse SL. The Exeter hip—40 years of innovation in total hip arthroplasty. Exeter Hip Publishing, Exeter, pp 283-294
- 8.Cement-in-cement short revision stem. Operative technique. Stryker Europe 2004. Literature EXEBR02E01. www.stryker.com
- 9.Marcos L, Buttaro M, Comba F, Piccaluga F. Femoral cement within cement technique in carefully selected aseptic revision arthroplasties. Int Orthop. 2009;33(3):633–637. doi: 10.1007/s00264-008-0516-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briant-Evans TW, Veeramootoo D, Tsiridis E, Hubble MJW. Cement-in-cement stem revision for Vancouver type B peri-prosthetic femoral fractures after total hip arthroplasty. 3 year follow up of 23 cases. Acta Orthop. 2009;80(5):548–552. doi: 10.3109/17453670903316827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 12.Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg Br. 1993;75:14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- 13.Schreurs BW, Arts JJ, Verdonschot N, Buma P, Slooff TJ, Gardeniers JW. Femoral component revision with use of impaction bone-grafting and a cemented polished stem. J Bone Joint Surg Am. 2005;87(11):2499–2507. doi: 10.2106/JBJS.D.02547. [DOI] [PubMed] [Google Scholar]
- 14.Wraighte PJ, Howard PW. Femoral impaction bone allografting with an Exeter cemented collarless, polished, tapered stem in revision hip replacement: a mean follow-up of 10.5 years. J Bone Joint Surg Br. 2008;90(8):1000–1004. doi: 10.1302/0301-620X.90B8.20390. [DOI] [PubMed] [Google Scholar]
- 15.Halliday BR, English HW, Timperley AJ, Gie GA, Ling RS. Femoral impaction grafting with cement in revision total hip replacement. Evolution of the technique and results. J Bone Joint Surg Br. 2003;85(6):809–817. [PubMed] [Google Scholar]
- 16.Ornstein E, Linder L, Ranstam J, Lewold S, Eisler T, Torper M. Femoral impaction bone grafting with the Exeter stem - the Swedish experience: survivorship analysis of 1,305 revisions performed between 1989 and 2002. J Bone Joint Surg Br. 2009;91(4):441–446. doi: 10.1302/0301-620X.91B4.21319. [DOI] [PubMed] [Google Scholar]
- 17.English H, Timperley AJ, Dunlop D, Gie G. Impaction grafting of the femur in two-stage revision for infected total hip replacement. J Bone Joint Surg Br. 2002;84(5):700–705. doi: 10.1302/0301-620X.84B5.12504. [DOI] [PubMed] [Google Scholar]
- 18.Swedish Hip Arthroplasty Register Annual Report 2008. Available online at: http://www.jru.orthop.gu.se/ Accessed 4 October 2010
- 19.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(7):1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 20.Mandziak DG, Howie DW, Neale SD, McGee MA. Cement-within-cement stem exchange using the collarless polished double-taper stem. J Arthroplasty. 2007;22(7):1000–1006. doi: 10.1016/j.arth.2007.06.001. [DOI] [PubMed] [Google Scholar]