Abstract
Acetabular osteolysis associated with socket loosening is one of the main long-term complications of total hip arthroplasty. In case of major bone loss, where <50% host bone coverage can be obtained with a porous-coated cementless cup, it is generally agreed that a metal ring or cage in association with a cemented component and allograft bone should be used. In order to promote allograft bone consolidation and incorporation, we have associated demineralised bone matrix (DBM, Grafton® A Flex) to the construct ion. Here we describe the technical details of major acetabular reconstruction using the Kerboull acetabular reinforcement device with allograft bone and DBM. This device has a hook that must be placed under the teardrop of the acetabulum and a plate for iliac fixation. The main advantages of this device are help in restoring the normal centre of hip rotation, guiding the reconstruction and partially unloading the graft. The Kerboull acetabular reinforcement device has provided a 92% survival rate free of loosening at 13-year follow-up in a consecutive series of 60 type III and IV deficiencies. Our preliminary results using DBM indicate faster allograft consolidation and remodelling.
Introduction
Revision acetabular reconstructions represent a great challenge to orthopaedic surgeons, particularly in patients with severe segmental and combined pelvic deficiencies. In general, a porous-coated, noncemented cup with at least 50% host bone coverage or standard cemented implants in case of cavitary defects is required [1–4]. Deficiencies are filled with allograft, either structural or particulate. However, deficiencies requiring >50% coverage of the socket by allograft should be supported by a metal ring or cage with a cemented cup [4]. This protects the graft from mechanical overload during its revascularisation phase. The majority of these deficiencies fall into types III and IV defects as defined by the American Academy of Orthopaedic Surgeons (AAOS) classification system [5]. The most commonly used metal rings are the Muller acetabular ring and Burch-Schneider antiprotrusio cage [6]. Another design is the ring hook cages first introduced by Kerboull [7] and later adapted to the Muller ring by Koch et al. [8]. The techniques to insert these devices are variable in terms of optimal position and allograft use. More specifically, little emphasis has been placed on restoring normal hip anatomy, with the majority of the surgical technique focusing on placing the cage on intact host bone [9]. In addition, some recent publications have described device or screw fixation failures, indicating incomplete incorporation of the allograft to the host bone and micromotion [10–15]. Demineralised bone matrix (DBM), first described by Urist et al. [16], is obtained after mineral content extraction of bone through acid treatment. However, a wide range of types and modes of preparation of bone and carriers associated to the DBM for delivery are commercially available. Among the available formulations, enhanced osteoinduction associated with the use of a glycerol-based carrier, combined with the improved osteoconductive characteristics of fibre-based DBM [17–22], has the strongest clinical support (Grafton® DBM, Osteotech Inc., Eatontown, NJ, USA). This paper provides a detailed description of the surgical technique for acetabular reconstruction using allograft bone and DBM with the Kerboull acetabular device that is based on restoration of a normal hip centre and acetabular bone stock. Preliminary results are also provided.
Surgical technique
All revisions are performed through a lateral approach with a trochanteric osteotomy in order to obtain an optimal view of the acetabular cavity. During the revision, multiple samples are taken for frozen section and culture to assess the aseptic character of the failure. A wide exposure of the acetabular cavity is necessary to completely remove the loosened socket and the cement fragments, if present. After excision of the fibrous membrane adherent to the socket and the granulation tissue filling the defects, the acetabular cavity is washed with pulsatile lavage. Reaming of this cavity is not performed because of the fragility of the acetabular walls related to the loss of bone stock. The severity of bone loss is then assessed, and in case of major bone deficiency, the final decision to reconstruct using allograft, Grafton A Flex® and the Kerboull acetabular device is made. These allografts consist of femoral heads retrieved during total hip arthroplasties performed for primary osteoarthritis. They are conditioned in a sterile environment and stored at −80°C. None of these bone grafts is irradiated. Preparation of the grafts is performed with the use of an oscillating saw to remove the remaining cartilage and soft tissues. The grafts are finally cut into fragments of variable size and shape according to the type of defect being dealt with. The DBM used is a form specifically designed for acetabular grafting. In summary, cortical long-bone shafts were frozen at −70°C after treatment for lipid, blood and cellular matrix removal. Bone was then milled into elongated fibres that were decalcified in 0.6 N hydrochloric acid (HCl), rinsed in sterile water and soaked in ethanol. Fibres were combined with the carrier and wet-laid into a nonwoven flexible sheet, which can be created in preformed shapes. In the application described here, a flexible disc 6 cm in diameter with a split (Grafton DBM A-Flex®) was used, which allows the disc to be manually formed into a slightly conical or hemispherical shape to conform to any size of acetabular cavity.
The Kerboull acetabular device
The Kerboull acetabular reinforcement device consists of a four-branched hemispherical cross made of 316-L stainless steel, which aims to guide and reinforce the bony reconstruction of the acetabular cavity. Its shape results from the orthogonal crossing of two hemispherical plates. The vertical plate ends distally with a hook that must be inserted under the teardrop component and proximally with a plate perforated by four holes for iliac screw fixation above the acetabulum. The horizontal plate is asymmetrical, with an anterior branch shorter than the posterior, determining 10° of anteversion of the opening plane of the device. A left and a right series of the device are available in six sizes in which sockets 37–53 mm of outside diameter can be cemented. The size of the acetabular device to be implanted is guided by the opposite normal hip. In case of bilateral hip replacement, patient morphology and cavity size in its lower half must be used as a guide. The aim of the reconstruction guided by the acetabular device is to restore an acetabular cavity of normal size, in an anatomically correct position, and with mechanical properties near enough to a normal acetabulum. The following steps for acetabular reconstruction have been standardised.
Trial of the acetabular device
After removing the fibrous tissue surrounding the inferior margin of the acetabulum, the hook of the acetabular device is placed under it, in its posterior portion, near the ischium. Then, the acetabular device is tilted 40–45°. This procedure should not tend to eject the hook from the inferior margin of the acetabulum. If it does, three hypotheses are to be explored: (a) The size of the acetabular device is too large; a smaller size has to be tried. (b) The inferior margin of the acetabulum is damaged; it has to be reconstructed by an allograft fragment shaped to fit the defect. (c) The inferior branch comes into contact with an acetabular bone fragment, which has to be progressively removed until the hook remains in place under the inferior margin of the acetabulum.
At this stage, the vertical branch of the device should be located in a strictly frontal plane. In case of bone loss from the acetabular roof, the plate stands distant from bone. The acetabular device should not be abducted more than 45° in order to bring the plate in contact with bone, as it would tend to eject the inferior hook. Neither should the device be opened nor the plate bent in order to adapt them to the bone loss. On the contrary, the acetabular device is used as a guide to evaluate the size and location of the acetabular defects as well as the size and shape of the allograft fragments needed to achieve the reconstruction. At this stage, we recommend performing an anteroposterior (AP) radiograph of the hip to check the correct position of the plate and hook. Once this assessment is performed, the trial acetabular device is removed.
Placement of the Grafton A Flex
Before starting the reconstruction with allograft bone, after complete cleaning of the acetabular cavity and removal of fibrous tissues, the Grafton DBM A Flex is placed in direct contact with the host bone (Fig. 1). As it is available only in one size, any material hanging out of the acetabular cavity, such as in cases of a small acetabulum, may be trimmed away and either used as a bone graft at another stage of the surgery or discarded. Whereas in the case of a large cavity, the material should be placed at a location where maximum surface area of the material will lie in direct contact with the allograft fragments that will be placed at the next stages.
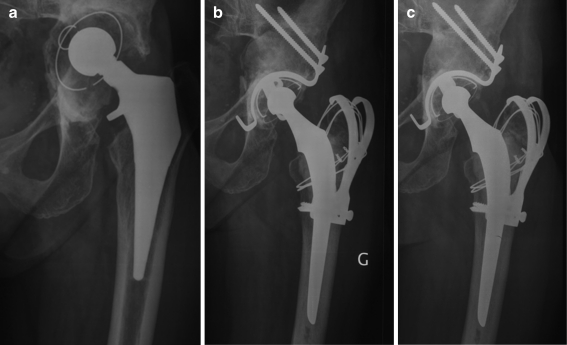
Fig. 1.
Grafton® demineralised bone matrix (DBM) A Flex™ is placed in direct contact with host bone. No fibrous tissue should be interposed between Grafton® DBM A Flex™ and host bone. During placement of the Kerboull device, the inferior hook should be positioned below the inferior margin of the acetabulum and the iliac plate at 40–45° of abduction
Reconstruction of the roof (superior rim and dome)
Bone-loss reconstruction usually starts with acetabular roof restoration unless there is massive destruction of the medial wall. This superior bone defect is reconstructed, when possible, by a single allograft fragment meticulously shaped from a femoral-head allograft in order to resist compression stresses in the load-bearing area. The superior portion of the graft, made of cancellous bone, is shaped to a convex form to fit the bony outlines of the damaged roof. Its inferior cancellous side is made concave to fit the convexity of the acetabular device. The plate of the device is placed against the lateral side of the allograft made of sclerotic subchondral bone. Its surface is not reduced before testing the trial device to avoid obtaining a graft of insufficient thickness. Several trials are sometimes necessary to achieve perfect adaptation of the graft to the host bone and to the acetabular device. This graft fragment is eventually directly fixed to the host bone with a 5-mm screw if it cannot be press-fitted in the remaining host bone. In case of minor destruction of the roof, a graft is shaped to increase the depth of the cavity and offer the plate a stable support in the right position. In case of minimal acetabular defect, simply by enlarging the cavity without altering its rims, the acetabular device can be directly fixed to the iliac host bone.
Reconstruction of the medial wall
In case of isolated bone loss of the acetabular floor, a thick equatorial slice cut from a femoral head is generally sufficient to fill the defect. The graft is shaped to the size of the defect, and its outside pelvic side is made concave to fit the convexity of the acetabular device. The femoral-head slice has to be ten to 15-mm thick to remain five to seven mm thick after its preparation. If the inferior margin of the acetabulum is damaged, it must be reconstructed in order to fix the hook of the acetabular device. In this case, bone loss usually extends to the medial wall and has a triangular shape. The restoration of the inferior margin is performed with a graft fragment of identical size and shape to the bone defect and of sufficient thickness to be fixed into the hook of the acetabular device. If bone loss concerns only the inferior margin of the acetabulum, a graft fragment of rectangular beam shape is used. If the extension of the bone defect from the acetabular inferior margin affects a wide portion of the acetabular floor, a single femoral-head allograft slice is used to perform the reconstruction to improve its stability. This single-fragment reconstruction of the medial wall is preferred to using multiple fragments, in which stability remains poor even if supported by the acetabular device. Finally, if several fragments are to be used, they can be fixed with a wire to the inferior branch of the device.
Fixation of the acetabular device
Once reconstruction of the superior and medial walls is achieved, the acetabular device is placed back in position. Its correct position is checked and its stability tested. The plate then is fixed to the iliac host bone with 5-mm screws. The fixation starts with the inferior hole of the plate. The screw direction is oblique, towards the sacroiliac joint. Before screwing it completely, another screw is inserted to 3/4 of its length into the anterior hole to stabilise the acetabular device. Then, both screws are screwed tight. These screws generally penetrate the grafted roof. Complete tightening of the inferior screw brings the acetabular device into tension, which is demonstrated by the locking of the hook under the inferior margin of the acetabulum (Fig. 2). If this procedure tends to remove the hook from the inferior margin of the acetabulum, the thickness of the superior graft is insufficient. A slice of allograft must then to be placed under the plate of the device, and the tightening of the screws must be performed until the acetabular device loses its elasticity.
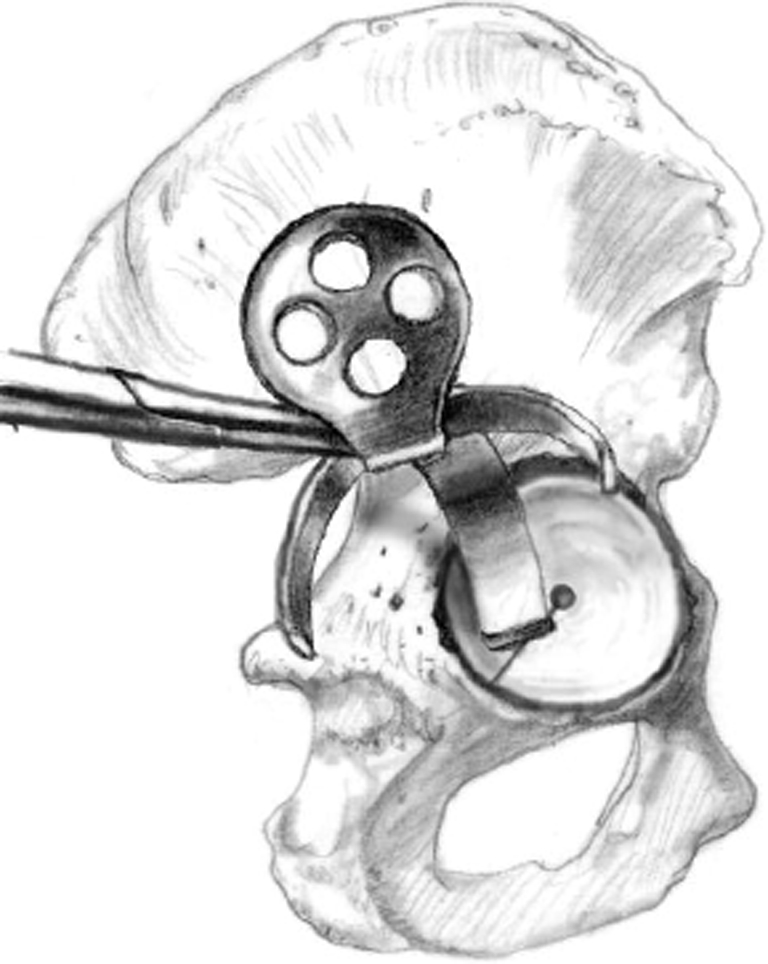
Fig. 2.
The device is fixed with two to three bicortical 5-mm outer-diameter screws directed towards the sacroiliac joint without reaching it, and 10° posteriorly
Reconstruction of the anterior and posterior walls
Reconstruction of the anterior and posterior walls is performed using allograft fragments shaped into form and impacted between the residual walls and the horizontal branches of the acetabular device. These fragments can be directly fixed to the acetabular device by wires or screws if their stability is judged insufficient. A posterior bone defect, located at the superior portion of the posterior wall, is frequently present; it must be reconstructed by an adequate allograft fragment directly fixed to the iliac host bone. Finally, the reconstruction is completed by morsellised cancellous bone packed into the cavitary defects of the pubis and ischium and into the gaps between the different allograft fragments in order to avoid any cement leak.
Cementing the acetabular component
The reconstructed and reinforced acetabular cavity is then washed with pulsatile lavage. Stability of the allograft fragments is checked, correct adaptation and orientation of the trial socket is confirmed and the acetabular component is ultimately cemented (Fig. 3).
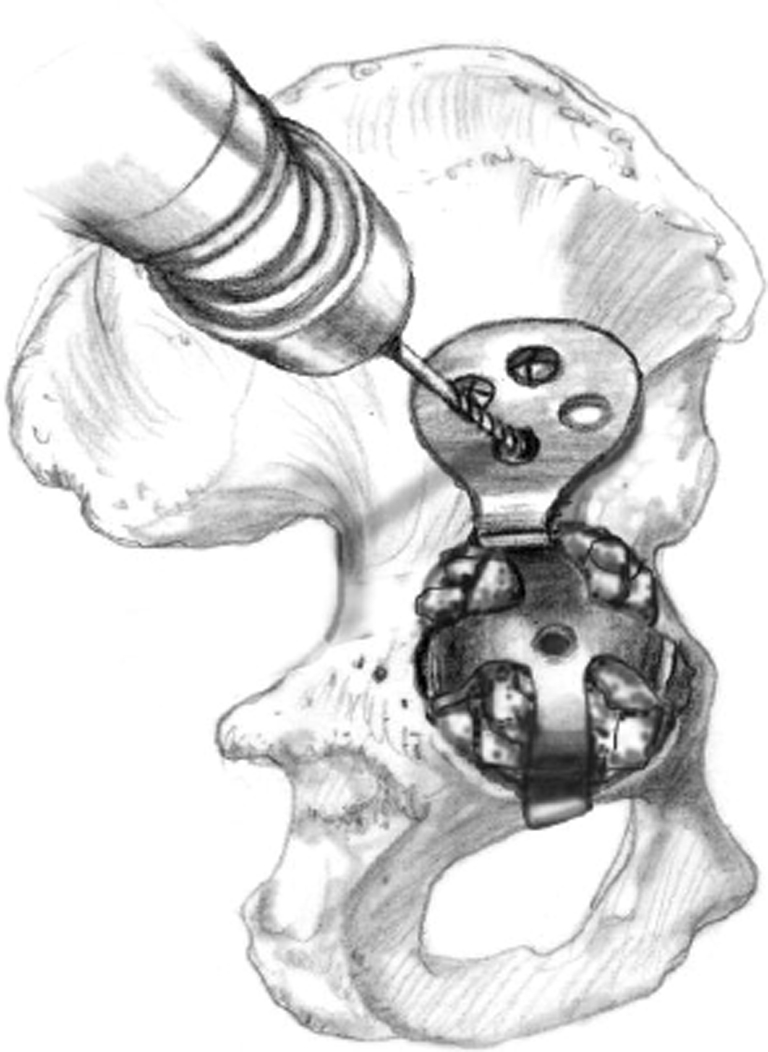
Fig. 3.
After complete reconstruction of the deficient acetabulum that has become completely contained, an all-polyethylene socket is cemented in the usual postion
Postoperative treatment
Postoperative treatment includes anticoagulation therapy, systemic antibiotics and indomethacin to prevent heterotopic ossification. Passive motion exercises of the revised joint are started immediately. Patients are free to ambulate with two crutches after three days. Full weight bearing is usually allowed after the sixth postoperative week.
Discussion
There is clinical and biomechanical evidence that joint reaction forces increase with superior and lateral placement of the hip centre [23–25]. In their classic article, Johnston et al. [24] demonstrated that inferior and medial placement of the hip centre resulted in a maximum reduction of joint reaction force and moment generating muscle requirements. Delp et al. [23] showed, with a 3D computer model, that increasing the hip centre by 2 cm in the superior and lateral direction decreases abductor moment arms by 28%. However, increasing the hip centre in the superior direction alone, along with prosthetic neck-length compensation, had little effect on moment arms. Joint reaction forces similarly increase with superior and lateral hip-centre placement >25 mm, as shown in an experimental model by Doehring et al. [26]. These authors demonstrated that with a 25-mm displacement of the hip centre, the joint reaction force increase 29% (approximately 7.5–8.0 times body weight) and up to 37% with a placement of 37 mm. This is compared with a joint reaction force of 1.5–2.0 times body weight at the normal hip centre. There was no increase in joint reaction force with superior hip placement alone. Vertical placement of the acetabulum has been shown to produce higher polyethylene wear rates [27, 28]. These factors may influence the rate of mechanical failure in metallic reinforcement devices.
Udomkiat et al. [29] reported clinical and radiographic short-term results of three different metallic reconstruction devices (Burch-Sneider, Ganz, and Mueller) for mostly type II and III defects. The overall mechanical failure rate, at average 4.6 years, was 17%. The Burch-Sneider cage had less favourable biomechanical characteristics than the other devices: abduction angles of 70.7 ± 12.6 and elevated hip centres of 16.6 ± 12.5 mm. Hip-centre lateralisation was not documented, which could show an even more unfavourable biomechanical environment. The Ganz ring, with an inferior hook, had abduction angles of 61.9 ± 10.5 and elevated hip centres of 12.6 ± 15.2 mm. No statistical analysis was documented on these parameters; however, there was no difference in the mechanical failure rate between the three devices. The authors’ conclusions were that structural allograft, in contrast to particulate allograft, should be used in the superior portion of the acetabulum to prevent early failure. However, there was no consideration of the unfavourable biomechanical environment around the graft itself most likely contributing to early failure. In general, the surgical technique, particularly with the Burch-Schneider cage, focused on stabilising the implant on host bone. This would lead, particularly with large deficiencies, to superior and lateral hip-centre placement, which would explain a higher mechanical failure rate.
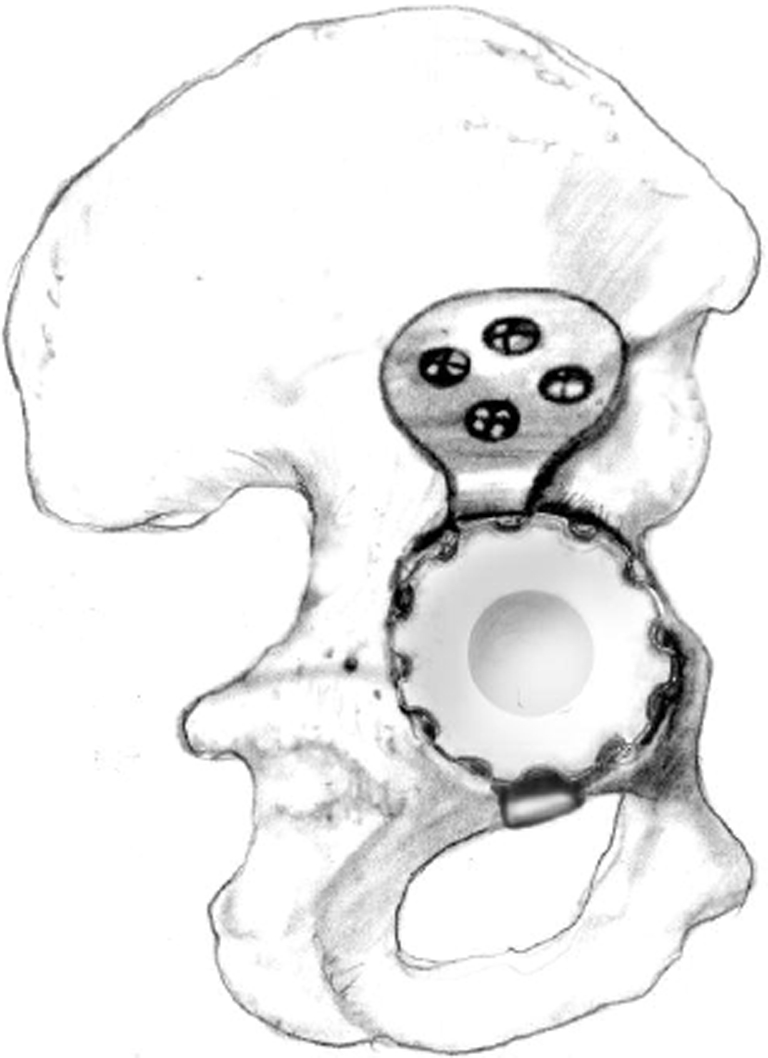
In contrast, Kerboull et al. [30] reported ten year follow-up data on types III and IV deficiencies, with 92.1 ± 5% survivorship. The biomechanical parameters were more favourable with a device abduction angle of 38.7 ± 7.6°. This device and the surgical technique focus on normal hip-centre orientation using an inferior crimping hook. The modified technique proposed in our paper is based upon a specifically designed form of DBM for acetabular reconstruction. At this stage, we have performed nine cases of type III deficiencies using this technique. No complication related to the use of DBM occurred up to one year of follow-up, and the specific form was easy to handle and place in this acetabular cavity. We regularly observed graft incorporation by three months as indicated by the disappearance of the radiolucent line at the graft–host interface. Remodelling activity was seen as early as six month follow-up, compared with one to two years in the absence of DBM. Based upon these preliminary results, it appears that fibre-based DBM could enhance allograft bone incorporation and remodelling in major acetabular reconstruction (Fig. 4). If these observations are borne out in the longer term, they could prove important to long-term stability of the reconstruction. Continued follow-up of these patients is ongoing.
Fig. 4.
a Preoperative anteroposterior (AP) radiograph of the hip of a 65-year-old woman with a combined structural and cavitary defect involving the acetabular roof and anterior and posterior walls 12 years following primary hybrid total hip arthroplasty. b By 3 months, the demarcation line between allograft and host bone had disappeared. c By 1-year follow-up, allograft remodelling could clearly be seen
References
- 1.Comba F, Buttaro M, Pusso R, Piccaluga F. Acetabular revision surgery with impacted bone allografts and cemented cups in patients younger than 55 years. Int Orthop. 2009;33:611–616. doi: 10.1007/s00264-007-0503-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun C, Lian YY, Jin YH, Zhao CB, Pan SQ, Liu XF. Clinical and radiographic assessment of cementless acetabular revision with morsellised allografts. Int Orthop. 2009;33:1525–1530. doi: 10.1007/s00264-009-0722-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vargas B, Caton J. Acetabular revision with freeze-dried irradiated and chemically treated allograft: a minimum 5-year follow-up of 17 cases. Int Orthop. 2009;33:35–39. doi: 10.1007/s00264-007-0444-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 5.D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;243:126–137. [PubMed] [Google Scholar]
- 6.Cabanela ME. Reconstruction rings and bone graft in total hip revision surgery. Orthop Clin North Am. 1998;29:255–262. doi: 10.1016/S0030-5898(05)70324-2. [DOI] [PubMed] [Google Scholar]
- 7.Kerboull M. Revision surgery for aseptic loosening of total hip replacement. In: Postel M, Kerboull M, Evrard J, Courpied JP, editors. Acetabular reconstruction. Berlin: Springer Verlag; 1985. pp. 85–90. [Google Scholar]
- 8.Koch P, Tannast M, Fujita H, Siebenrock K, Ganz R. Minimum ten year results of total hip arthroplasty with the acetabular reinforcement ring in avascular osteonecrosis. Int Orthop. 2008;32:173–179. doi: 10.1007/s00264-006-0303-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berry DJ, Muller ME. Revision arthroplasty using an anti-protrusio cage for massive acetabular bone deficiency. J Bone Joint Surg Br. 1992;74:711–715. doi: 10.1302/0301-620X.74B5.1527119. [DOI] [PubMed] [Google Scholar]
- 10.Baba T, Shitoto K. Revision of total hip arthroplasty using the Kerboull and KT plates. Int Orthop. 2010;34:341–347. doi: 10.1007/s00264-009-0789-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawai T, Tanaka C, Ikenaga M, Kanoe H, Okudaira S. Total hip arthroplasty using Kerboull-type acetabular reinforcement device for rapidly destructive coxarthrosis. J Arthroplasty. 2010;25:432–436. doi: 10.1016/j.arth.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Kawanabe K, Akiyama H, Onishi E, Nakamura T. Revision total hip replacement using the Kerboull acetabular reinforcement device with morsellised or bulk graft: results at a mean follow-up of 8.7 years. J Bone Joint Surg Br. 2007;89:26–31. doi: 10.1302/0301-620X.89B1.18037. [DOI] [PubMed] [Google Scholar]
- 13.Okano K, Miyata N, Enomoto H, Osaki M, Shindo H. Revision with impacted bone allografts and the Kerboull cross plate for massive bone defect of the acetabulum. J Arthroplasty. 2010;25:594–599. doi: 10.1016/j.arth.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 14.Tanaka C, Shikata J, Ikenaga M, Takahashi M. Acetabular reconstruction using a Kerboull-type acetabular reinforcement device and hydroxyapatite granules: a 3- to 8-year follow-up study. J Arthroplasty. 2003;18:719–725. doi: 10.1016/S0883-5403(03)00149-9. [DOI] [PubMed] [Google Scholar]
- 15.Lunn J, Kearns SS, Quinlan W, Murray P, Byrne O. J Impaction allografting and the Kerboull acetabular reinforcement device. 35 hips followed for 3-7 years. Acta Orthopedica. 2005;76:298–302. [PubMed] [Google Scholar]
- 16.Urist M, Silverman BF, Buring K, Dubuc FL, Rosenberg JM. The bone induction principle. Clin Orthop Relat Res. 1967;53:243–283. doi: 10.1097/00003086-196707000-00026. [DOI] [PubMed] [Google Scholar]
- 17.Cammisa FP, Lowery G, Garfin SR, Geisler FH, Klara PM, McGuire RA, Sassard WR, Stubbs H, Block JE. Two-year fusion rate equivalency between Grafton DBM gel and autograft in posterolateral spine fusion: a prospective controlled trial employing a side-by-side comparison in the same patient. Spine. 2004;29:660–666. doi: 10.1097/01.BRS.0000116588.17129.B9. [DOI] [PubMed] [Google Scholar]
- 18.Khan SN, Fraser JF, Sandhu HS, Cammisa FP, Girardi FP, Lane JM. Use of osteopromotive growth factors, demineralized bone matrix, and ceramics to enhance spinal fusion. J Am Acad Orthop Surg. 2005;13:129–137. doi: 10.5435/00124635-200503000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Louis-Ugbo J, Murakami H, Kim HS, Minamide A, Boden SD. Evidence of osteoinduction by Grafton demineralized bone matrix in nonhuman primate spinal fusion. Spine. 2004;29:360–366. doi: 10.1097/01.BRS.0000090823.12652.F9. [DOI] [PubMed] [Google Scholar]
- 20.Martin GJ, Boden SD, Titus L, Scarborough NL. New formulations of demineralized bone matrix as a more effective graft alternative in experimental posterolateral lumbar spine arthrodesis. Spine. 1999;24:637–645. doi: 10.1097/00007632-199904010-00005. [DOI] [PubMed] [Google Scholar]
- 21.Peterson B, Whang PG, Iglesias R, Wang JC, Lieberman JR. Osteoinductivity of commercially available demineralized bone matrix. Preparations in a spine fusion model. J Bone Joint Surg Am. 2004;86:2243–2250. doi: 10.2106/00004623-200410000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Hierholzer C, Sama D, Toro JB, Peterson M, Helfet DL. Plate fixation of ununited humeral shaft fractures: effect of type of bone graft on healing. J Bone Joint Surg Am. 2006;88:1442–1447. doi: 10.2106/JBJS.E.00332. [DOI] [PubMed] [Google Scholar]
- 23.Delp SL, Wixson RL, Komattu AV, Kocmond JH. How superior placement of the joint center in hip arthroplasty affects the abductor muscles. Clin Orthop Relat Res. 1996;328:137–146. doi: 10.1097/00003086-199607000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Johnston RC, Brand RA, Crowninshield RD. Reconstruction of the hip. A mathematical approach to determine optimum geometric relationships. J Bone Joint Surg Am. 1979;61:639–652. [PubMed] [Google Scholar]
- 25.Yoder SA, Brand RA, Pedersen DR, O’Gorman TW. Total hip acetabular component position affects component loosening rates. Clin Orthop Relat Res. 1988;228:79–87. [PubMed] [Google Scholar]
- 26.Doehring TC, Rubash HE, Shelley FJ, Schwendeman LJ, Donaldson TK, Navalgund YA. Effect of superior and superolateral relocations of the hip center on hip joint forces. An experimental and analytical analysis. J Arthroplasty. 1996;11:693–703. doi: 10.1016/S0883-5403(96)80008-8. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530–534. doi: 10.1016/S0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 28.Schmalzried TP, Guttmann D, Grecula M, Amstutz HC. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76:677–688. doi: 10.2106/00004623-199405000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Udomkiat P, Dorr LD, Won YY, Longjohn D, Wan Z. Technical factors for success with metal ring acetabular reconstruction. J Arthroplasty. 2001;16:961–969. doi: 10.1054/arth.2001.27669. [DOI] [PubMed] [Google Scholar]
- 30.Kerboull M, Hamadouche M, Kerboul L. The Kerboull acetabular reinforcement device in major acetabular reconstructions. Clin Orthop Relat Res. 2000;378:155–168. doi: 10.1097/00003086-200009000-00025. [DOI] [PubMed] [Google Scholar]