Abstract
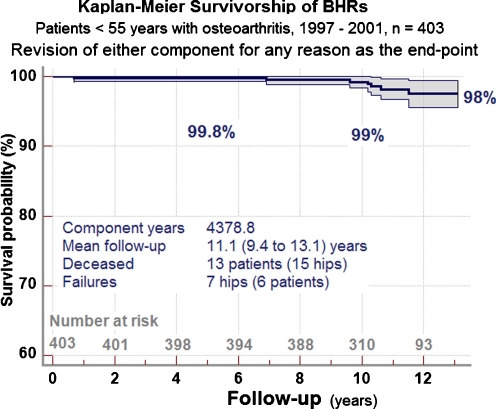
The best indication for hip resurfacing is a young active patient with severe hip arthritis, good hip morphology and reasonable bone quality. With revision of either component for any reason as the endpoint, there were 68 revisions in our series of 3,095 consecutive Birmingham Hip Resurfacings (BHR) (1997–2009), including all diagnoses in all ages. This equates to a revision rate of 2.2% and survivorships of 99, 97 and 96% at five, ten and 13 years, respectively. In patients under 55 years with osteoarthritis, the survivorship is 99 and 98% at ten and 13 years. These results provide medium-term evidence that BHR when performed well in properly selected patients offers excellent outcomes and implant survivorship. Small changes to implant materials and design can affect joint function and survivorship significantly as seen from the withdrawal of certain resurfacing devices recently from clinical use. The clinical history of one device cannot be extrapolated to other devices.
Introduction
The resurgence of hip resurfacing in the early 1990s [1] was a response to the poor performance of conventional hip arthroplasty in young patients. Resurfacing was by no means a novel concept then. Several iterations had been used during the 1950s through the 1980s with high early failure rates, leaving total hip arthroplasty (THA) as the only arthroplasty option for both old and young patients. Young patients with higher activity levels experienced early failures with THA [2], even though their longer life expectancy required that they last longer. Exploration of other conservative solutions which could potentially delay the need for an eventual THA continued. When it appeared that metal-on-metal (MoM) resurfacings might be the way forward, their primary goal was to buy time until an age at which conventional arthroplasty would be suitable for the patient. Therefore, if resurfacing offered around ten years of good function without, in the process, jeopardising the possibility of later conversion to a THA, it would be a viable conservative option. Other benefits such as reducing dislocations or preventing stress shielding would be added bonuses. The development [3] of modern resurfacing was directed towards meeting this specific need in young active patients.
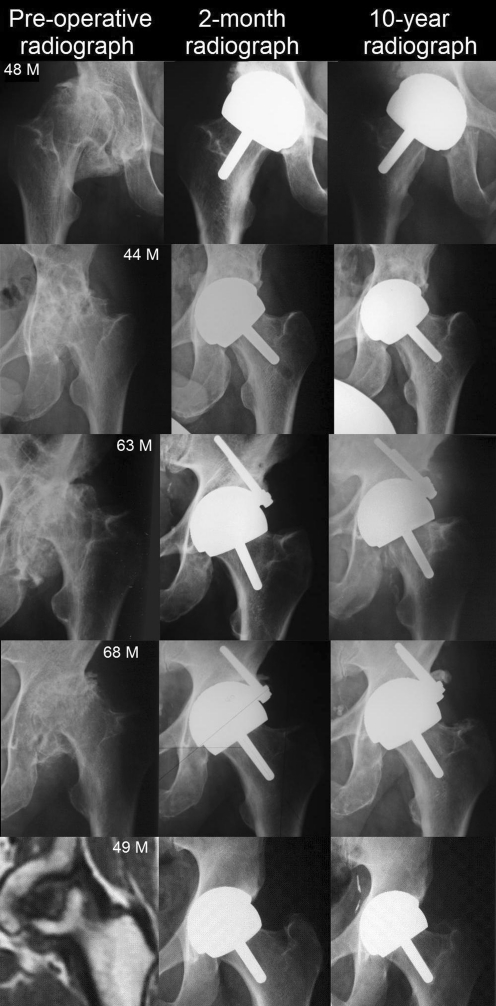
In the early years in the absence of clinical results it was difficult to discern how far the indications could be extended. Not encountering a femoral neck fracture in our first 700 cases led us to believe that the resurfacing stem buttressed and protected the neck [1]. We then started including patients with progressively poorer bone quality (Fig. 1). Although these and many other individual patients performed well for over ten years, our current evidence suggests that performing a hip resurfacing in such unfavourable circumstances increases the risk of failure. With hindsight and because of current availability of alternative conservative devices [4] we would not now perform a resurfacing in some of those patients.
Fig. 1.
These and several other young patients in our series who had extensive pre-operative cystic destruction of the femoral head often from long-term anti-inflammatory intake, or had severe avascular necrosis of the femoral head, have continued to have good hip function and unremarkable radiology 10–13 years after their resurfacing. There are others with such bone loss, who suffered femoral failures, as described in this paper. Based on our evidence we no longer perform or advise a resurfacing in the presence of this degree of femoral head damage
Indications
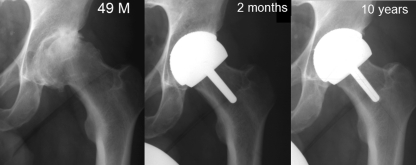
The most common indication for hip resurfacing in a Western series is end-stage hip osteoarthritis in a young active patient. Provided the surgeon is trained to perform the procedure and the bone quality and anatomy around the affected hip are reasonable, resurfacing offers an ideal solution for such a patient (Fig. 2).
Fig. 2.
The quality of life of this very active 49-year-old farmer was severely affected by primary osteoarthritis of his hip. Regular anatomy and reasonably good bone quality make him an ideal candidate for hip resurfacing. His high activity level and increased femoral offset makes resurfacing a more attractive option than a total hip replacement in his case
A resurfacing rather than a replacement is particularly suitable for patients with a particularly large femoral offset (Fig. 2) or a wide femoral canal, or those with femoral shaft deformity or osteopetrosis, in whom it is difficult to fit a stem, and in young patients who need better revision options. In older inactive patients a THA would be preferable especially in the presence of suboptimal bone quality, although chronological age is not the only consideration. Patient activities, co-morbidities and bone quality should also be taken into account. Our results demonstrate that medium-term results are as good in older patients as in young patients, provided resurfacing is used judiciously.
Patients with active infection, severe limb vascular deficiency, inadequate motor power and the skeletally immature are unsuitable for any arthroplasty procedure. Patients with Crowe grade IV dysplasia and malignant tumours in and around the hip are best treated with a THA. Patients with femoral head avascular necrosis (AVN), severe cystic change or poor quality bone in the femoral head and neck are at high risk of failure with a resurfacing and therefore contra-indicated, as are severe leg length discrepancy, severe post-Perthes’ or post-slipped capital femoral epiphysis (SCFE) arthritis, if the anatomical abnormality cannot be restored satisfactorily. Since resurfacings employ MoM bearings, patients in renal failure or with proven hypersensitivity to metal are also unsuitable. A woman in childbearing age planning to have a baby is advised to either have the baby before the procedure or wait at least two years thereafter.
Results
In addition to our own follow-up, our patients are regularly monitored by two independent Outcomes Centres which allow us to capture all problems and failures as they occur. Our results from a consecutive cohort of 3,095 BHRs (Birmingham Hip Resurfacing, Smith & Nephew Orthopaedics, Warwick, UK) performed by a single surgeon (DJWM) between 1997 and 2009 are taken into consideration in this report. Mean age of patients at operation is 53 years (range 13–86 years) and mean follow-up eight years (range 0.7–13 years) giving a total of 24,929 component years; 57 patients (71 hips) died through unrelated causes 5.6 years (mean) after the operation.
Survivorship
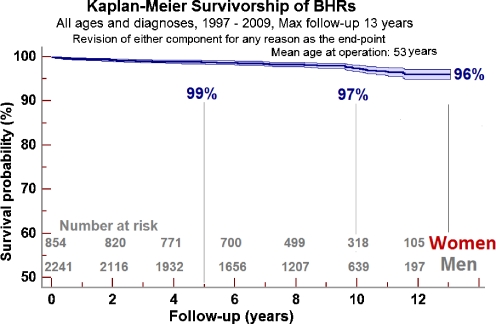
Sixty eight revisions were performed between 0 and 11.6 years after the operation (mean 4.8 years) giving us an overall failure rate of 2.2% (Table 1) and a Kaplan-Meier survivorship of 96% at 13 years (Fig. 3) with revision of either component for any reason as the endpoint.
Table 1.
Revisions performed 0–11.6 years after the operation (n = 68)
| Reason for failure | Number | Percentage |
|---|---|---|
| Femoral neck fracture | 12 | 0.4% |
| Femoral head collapse | 25 | 0.8% |
| Infection | 14 | 0.5% |
| Dislocation | 2 | 0.06% |
| Cup loosening | 2 | 0.06% |
| ARMeD | 10 | 0.3% |
| Osteolysis | 1 | 0.03% |
| Persistent groin pain | 2 | 0.06% |
ARMeD adverse reaction to metal debris
Fig. 3.
3,095 consecutive BHRs performed between 1997 and 2009, revision of either component for any reason as the endpoint
The most common failure mode is from femoral head collapse and there is no significant difference (p = 0.7) between men (0.8%) and women (0.9%). The risk factors were either pre-existent AVN or cystic change. The incidence of femoral neck fractures also does not differ (p = 0.7) in men (0.4%) and women (0.5%). All the adverse reactions to metal debris (ARMeD) occurred in women and the incidence of infection is slightly higher in women (0.9%) compared to men (0.3%).
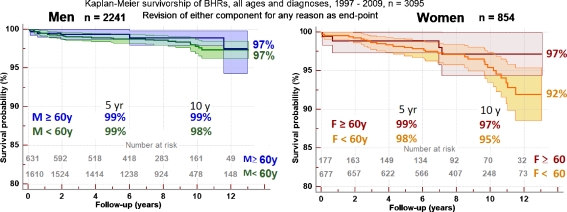
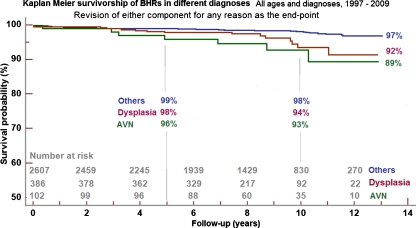
The survivorship at five, ten and 13 years in men is 99, 98 and 97% and in women 98, 96 and 93%, respectively. Men and women 60 years and above and men under 60 have a 13-year survivorship of 97% (Fig. 4), while in women under 60 it is 92%. The lower survivorship in young women may be related to the fact that in young women developmental hip dysplasia (DDH) is a common primary pathology and DDH is associated with a relatively inferior survivorship (Fig. 5). In women under 60 years, 32% had a primary diagnosis of DDH compared to 15% in women 60 years or older and 6% in men. AVN was the primary pathology in 4.3 and 3.4% of men and women under 60 years and 1.6 and 0% in men and women at the age of 60 or above, respectively.
Fig. 4.
Gender differences in implant survivorship
Fig. 5.
Implant survivorship of BHRs in different diagnoses
Since young active patients are the raison d’être for hip resurfacing, we regularly monitor a cohort of patients younger than 55 years with osteoarthritis treated with 403 BHRs. In an earlier publication we showed that their early results are superior to those of conventional THA [5]. None of these patients have been advised to alter their occupational activities and a majority of them continue to participate in regular sporting activities. Twelve patients died due to unrelated causes and seven hips have been revised over the past 13 years in this group giving a 13-year survivorship of 98% (Fig. 6).
Fig. 6.
Kaplan-Meier survivorship of BHRs in patients under the age of 55 years with symptomatic osteoarthritis
Clinico-radiological results
All 124 BHRs performed in 1997 were reviewed with clinico-radiological and multi-slice computed tomography (CT) scan assessments (with metal artefact reduction software) at a post-ten-year follow-up. DeLee and Charnley [6] acetabular zones and Amstutz [7] femoral stem zones were used for radiological assessment. Over the 13 years, there were 12 unrelated deaths and seven revisions (one femoral neck fracture, four femoral head collapse and two infections). Median Oxford hip score is 13 and 90th percentile 20. The best possible Oxford score is 12 and the worst possible 60. Mean hip flexion in the cohort is 125° (median 130°) and the ranges of other movements are shown in Table 2.
Table 2.
Ranges of movements (°)
| Range of motion in the resurfaced hip | Fixed flexion | Flexion | Abduction | Adduction | External rotation | Internal rotation |
|---|---|---|---|---|---|---|
| Average | 1.6 | 125.3 | 36.5 | 25.8 | 36.7 | 27.4 |
| Standard deviation | 2.9 | 14.8 | 6.2 | 6.9 | 7.6 | 9.7 |
| Minimum | 0 | 85 | 20 | 10 | 10 | 0 |
| Quartile 1 | 0 | 120 | 35 | 20 | 30 | 20 |
| Median | 0 | 130 | 40 | 25 | 40 | 30 |
| Quartile 3 | 3 | 140 | 40 | 30 | 40 | 35 |
| 90th percentile | 5 | 140 | 41.5 | 35 | 45 | 40 |
Eleven patients had Brooker [8] grade 1 heterotopic ossification, seven had grade 2 and one had grade 3. There was one hip each with a femoral fixation score of 1 and 2, four with score 3 and none had scores above 3. Two hips had an acetabular fixation score of 1, one hip each had a score of 2, 4, 5 and 6 and none above 6, i.e. no hip had complete lucencies in all zones or component migration. In summary, none of the components show radiographic evidence of instability. Multi-slice CT scanning did not show the presence of the so-called asymptomatic pseudotumours.
Discussion
Several clinical series [9–12] and registry data [13–15] continue to report good early and medium-term results with BHRs. Other series [16] and registry data [15, 17] have identified poor-performing resurfacings of different other designs. The rarity of dislocations is a distinct advantage over conventional hip arthroplasty. The extremely low incidence of component loosening in our series shows that fixation problems have largely been solved in the BHR in contrast to the loosening reported [18] with the Durom resurfacing device (Zimmer, Swindon, UK).
In addition to failures due to reasons such as infection, resurfacings fail through one of two modes, mechanical failures such as femoral neck fractures and bearing-related failures such as failures due to osteolysis [19], soft tissue reactions and periarticular necrosis [20]. These can occur due to one of three risk factors: patient-related, surgeon-related and implant-related.
As opposed to a hip replacement, the femoral head and neck are retained in a hip resurfacing with the result that resurfacing is not only bone-conserving at the outset, it also offers bone density preservation [21] in the long term through more natural load bearing. While this is beneficial to patients, it comes with two costs. Retention of the proximal femur limits operative access to the socket [22] and increases component placement error. Furthermore, this potential weak spot increases the risk of femoral neck fracture in the early months and of femoral head collapse over a longer period.
The incidence of femoral neck fractures in our series (0.4%) is not dissimilar to the 1–1.5% incidence in large multi-centre BHR series (89 surgeons from the Australian series [23] and 141 surgeons from the UK [24]). This demonstrates that BHR implantation is a reproducible intervention. For many surgeons in the large series, these cases included their learning curve experiences as well. Reports show that resurfacing conversions to THA for fracture had hip function similar to primary hip arthroplasties [25]. Periprosthetic fractures occur following THA as well, with an incidence of 1.1% after primary THAs and 4.0% after revisions [26]. In comparison to the management of most periprosthetic fractures around THAs, femoral neck fracture following hip resurfacing is relatively easier to deal with.
The most common reason for femoral failure in our series is collapse of the femoral head which, on average, occurs at a later post-operative stage than a fracture and the risk factors for this include pre-existent cystic change in the femoral head and femoral head AVN. Our incidence compares well with other reports [24]. Figure 4 shows that the survivorship in patients with AVN is significantly lower than that in other diagnoses (p < 0.001) and we now recognise that it is unwise to resurface femoral heads riddled with cysts or damaged by AVN as shown in Fig. 1. In such situations we now use a BMHR (Birmingham Mid-Head Resection, Smith & Nephew Orthopaedics, Warwick, UK) which does not rely on the integrity of the proximal half of the femoral head. It employs the BHR cup and bearing and has shown promising results [4] in such patients.
Patient factors constitute only one set of weak links in the chain of events that leads to resurfacing failure. A second risk factor for failure is surgical technique-related. One centre which reported a higher incidence of femoral neck fractures attributed it to the very devascularising nature of their posterior approach [27]. Subsequently they found that when correct surgical principles [28] were applied, the approach was no longer detrimental to femoral vascularity. The same centre also reported an increasing incidence of pseudotumours following resurfacing. The range of cup inclinations in their series extended up to 80°, and retrieval analysis [29] of their pseudotumour explants showed edge loading in all failures, implying component positioning error. Using the BHR, surgeons should aim for cup inclination of 40° and a combined anteversion angle (sum of cup and femoral neck anteversion) of no more than 45° in order to prevent edge loading.
Development of periprosthetic pseudotumours or ARMeD, which is one of the bearing-related failure mechanisms, is a matter for concern. We have seen ten such reactions in the 3,095 BHRs (0.3%). All our cases were in women and following revision to a non-MoM-bearing THA they are functioning well. Analysis of our cases suggests that although component positions in terms of cup inclination and anteversion were within the acceptable range, excess femoral anteversion from minor hip dysplasia was overlooked, leading to excess combined anteversion, edge loading and high wear. In young women hip dysplasia is the predominant reason for development of premature arthritis. Therefore, we carefully assess femoral anteversion before and during the operation. If pre-operative assessment suggests severe femoral malrotation we advise a multi-slice CT scan. If the anteversion is in excess of 45° we advise that either the resurfacing should be combined with a subtrochanteric derotation osteotomy or the patient should undergo a THA. Due consideration should be given by the patient and the surgeon to the longer rehabilitation period and the higher risks associated with a combined resurfacing and osteotomy. With lesser degrees of malrotation, we assess intra-operatively and position the cup with correspondingly reduced anteversion, so that combined cup and neck anteversion does not exceed 45°. Surgeon error in component positioning is a major risk factor for excess wear. Several techniques and mechanical guides are currently available to aid surgeons to achieve optimal cup orientation and precise femoral component positioning. Experimental and clinical studies [30, 31] have shown that computer navigation has the potential to make implant positioning more reliable. It is hoped that, as these modern techniques evolve and become more user-friendly, reduced surgeon error in implant positioning should decrease the incidence of wear-related failures.
The many nuances [32] of implant design and materials constitute the third risk factor for resurfacing failures. Our past experience [19] has shown that changes to materials processing can be detrimental to implant survivorship. More recently the consistently poor performance of the ASR device (Johnson & Johnson DePuy Ltd., Leeds, UK) was shown to be due to unfavourable design features such as the low angle of articulation and reduced diametral clearance [16]. Other influential factors include component thickness, surface roughness, out of roundness, locking mechanism for introducers, fixation surfaces [18] and their features. Two resurfacing devices, the Durom and the ASR which were introduced as advances of a generation, on the basis of laboratory predictions of success, have been withdrawn after high failure rates and possible long-term effects on the well-being of patients. Laboratory optimisation of design alone is an insufficient predictor of clinical success. All the variables that the device will be subject to in vivo are not fully understood and may not be realistically reproducible in the laboratory. Small changes can lead to unforeseen clinical problems. New implants should not be introduced into the wide world until clinical performance is proven in the designer centres over sufficient length of time.
Conclusion
In conclusion, evidence is progressively accruing to the effect that Birmingham Hip Resurfacing when performed well in properly selected patients continues to demonstrate excellent outcomes in the medium term. The first remit of hip resurfacing, which is to provide at least ten symptom-free years of joint function, has been met in a majority of patients. Small changes in the materials or design characteristics can affect joint function and survivorship significantly and it is wrong to assume that the clinical history of one device can be extrapolated to other devices.
Acknowledgments
Conflicts of interest The institution of the authors (DJWM, JD, HZ and CP) receives funding from Smith and Nephew Orthopaedics UK, and DJWM is a paid consultant to Smith and Nephew Orthopaedics UK.
References
- 1.McMinn D, Treacy R, Lin K, Pynsent P. Metal on metal surface replacement of the hip. Experience of the McMinn prosthesis. Clin Orthop Relat Res. 1996;329(Suppl):S89–S98. doi: 10.1097/00003086-199608001-00009. [DOI] [PubMed] [Google Scholar]
- 2.Joshi AB, Porter ML, Trail IA, Hunt LP, Murphy JC, Hardinge K. Long-term results of Charnley low-friction arthroplasty in young patients. J Bone Joint Surg Br. 1993;75(4):616–623. doi: 10.1302/0301-620X.75B4.8331119. [DOI] [PubMed] [Google Scholar]
- 3.McMinn DJW. Development of metal/metal hip resurfacing. Hip Int. 2003;13:S41–S53. doi: 10.1177/112070000301302s09. [DOI] [PubMed] [Google Scholar]
- 4.Daniel J, Pradhan C, Ziaee H, McMinn DJ. A clinicoradiologic study of the Birmingham Mid-Head Resection device. Orthopedics. 2008;31(12 Suppl 2):124–128. [PubMed] [Google Scholar]
- 5.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 6.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 7.Beaulé PE, Dorey FJ, LeDuff MJ, Gruen T, Amstutz HC. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93. doi: 10.1097/00003086-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Brooker AF, Bowerman JW, Robinson RA, et al. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 9.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 10.Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years. An independent prospective review of the first 230 hips. J Bone Joint Surg Br. 2007;89(11):1431–1438. doi: 10.1302/0301-620X.89B11.19336. [DOI] [PubMed] [Google Scholar]
- 11.Reito A, Puolakka T, Pajamäki J (2010) Birmingham hip resurfacing: five to eight year results. Int Orthop 2010 Jun 19. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 12.Ollivere B, Duckett S, August A, Porteous M. The Birmingham Hip Resurfacing: 5-year clinical and radiographic results from a District General Hospital. Int Orthop. 2010;34:631–634. doi: 10.1007/s00264-009-0821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aulakh TS, Kuiper JH, Dixey J, Richardson JB (2010) Hip resurfacing for rheumatoid arthritis: independent assessment of 11-year results from an international register. Int Orthop 2010 May 25. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 14.Khan M, Kuiper JH, Edwards D, Robinson E, Richardson JB. Birmingham hip arthroplasty: five to eight years of prospective multicenter results. J Arthroplasty. 2009;24(7):1044–1050. doi: 10.1016/j.arth.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 15.Annual report 2009 of the National Joint Replacement Registry of the Australian Orthopaedic Association (2010) http://www.dmac.adelaide.edu.au/aoanjrr/documents/aoanjrrreport_2010.pdf. Accessed 8 2010
- 16.Jameson SS, Langton DJ, Nargol AV. Articular surface replacement of the hip: a prospective single-surgeon series. J Bone Joint Surg Br. 2010;92(1):28–37. doi: 10.1302/0301-620X.92B1.22769. [DOI] [PubMed] [Google Scholar]
- 17.7th Annual report 2010 of the National Joint Registry for England and Wales (2010) http://www-new.njrcentre.org.uk/NjrCentre/LinkClick.aspx?fileticket=QkPI7kk6B2E%3d&tabid=86&mid=523. Accessed 8 2010
- 18.Long WT, Dastane M, Harris MJ, Wan Z, Dorr LD. Failure of the Durom Metasul acetabular component. Clin Orthop Relat Res. 2010;468(2):400–405. doi: 10.1007/s11999-009-1071-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daniel J, Ziaee H, Kamali A, Pradhan C, Band T, McMinn DJ. Ten-year results of a double-heat-treated metal-on-metal hip resurfacing. J Bone Joint Surg Br. 2010;92(1):20–27. doi: 10.1302/0301-620X.92B1.21530. [DOI] [PubMed] [Google Scholar]
- 20.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010;92(1):38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 21.Kishida Y, Sugano N, Nishii T, Miki H, Yamaguchi K, Yoshikawa H. Preservation of the bone mineral density of the femur after surface replacement of the hip. J Bone Joint Surg Br. 2004;86(2):185–189. doi: 10.1302/0301-620X.86B2.14338. [DOI] [PubMed] [Google Scholar]
- 22.Myers GJ, Morgan D, McBryde CW, O’Dwyer K. Does surgical approach influence component positioning with Birmingham Hip Resurfacing? Int Orthop. 2009;33:59–63. doi: 10.1007/s00264-007-0469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Joint Surg Br. 2005;87(4):463–464. doi: 10.1302/0301-620X.87B4.15498. [DOI] [PubMed] [Google Scholar]
- 24.Carrothers AD, Gilbert RE, Jaiswal A, Richardson JB. Birmingham hip resurfacing: the prevalence of failure. J Bone Joint Surg Br. 2010;92(10):1344–1350. doi: 10.1302/0301-620X.92B10.23504. [DOI] [PubMed] [Google Scholar]
- 25.Ball ST, Duff MJ, Amstutz HC. Early results of conversion of a failed femoral component in hip resurfacing arthroplasty. J Bone Joint Surg Am. 2007;89(4):735–741. doi: 10.2106/JBJS.F.00708. [DOI] [PubMed] [Google Scholar]
- 26.Springer BD, Berry DJ, Lewallen DG. Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision. J Bone Joint Surg Am. 2003;85:2156–2162. doi: 10.2106/00004623-200311000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Little CP, Ruiz AL, Harding IJ, McLardy-Smith P, Gundle R, Murray DW, Athanasou NA. Osteonecrosis in retrieved femoral heads after failed resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:320–323. doi: 10.2106/JBJS.D.02927. [DOI] [PubMed] [Google Scholar]
- 28.Simpson DJ, Ranson I, Mellon S, De Smet KA, Murray DW, Gill HS (2009) Operative technique to reduce intra-femoral pressure during hip resurfacing. http://www.ors.org/web/Transactions/55/2011.PDF
- 29.Kwon YM, Glyn-Jones S, Simpson DJ, Kamali A, McLardy-Smith P, Gill HS, Murray DW. Analysis of wear of retrieved metal-on-metal hip resurfacing implants revised due to pseudotumours. J Bone Joint Surg Br. 2010;92:356–361. doi: 10.1302/0301-620X.92B3.23281. [DOI] [PubMed] [Google Scholar]
- 30.Pitto RP, Malak S, Anderson IA. Accuracy of a computer-assisted navigation system in resurfacing hip arthroplasty. Int Orthop. 2009;33:391–395. doi: 10.1007/s00264-008-0644-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krüger S, Zambelli PY, Leyvraz PF, Jolles BM. Computer-assisted placement technique in hip resurfacing arthroplasty: improvement in accuracy? Int Orthop. 2009;33:27–33. doi: 10.1007/s00264-007-0440-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heisel C, Kleinhans JA, Menge M, Kretzer JP. Ten different hip resurfacing systems: biomechanical analysis of design and material properties. Int Orthop. 2009;33:939–943. doi: 10.1007/s00264-008-0607-y. [DOI] [PMC free article] [PubMed] [Google Scholar]