Abstract
Long-term results of a retrospective series of primary arthroplasty with the original cementless dual mobility socket (A) and the midterm results with the second generation (B) are reported. In series A (follow-up 16.5 years) 437 total hip arthroplasties (THA) were included and in series B (follow-up five years) 231 hips. The 15-year survival rate was 84.4 ± 4.5% (revision for any reason as endpoint); 30 hips (6.8%) were revised for aseptic loosening. Five THA were revised for dislocation: two early and three after ten years or more. With the second generation socket neither dislocation nor revision for mechanical reasons were observed. The survival rate was 99.6 ± 0.4% (revision for any reason). The prevalence of revision for dislocation was very low in our series. This concept does not avoid wear and aseptic loosening, especially in young active patients, but the long-term stability has been confirmed. Dual mobility can be recommended for patients over 70 years of age and for younger patients with high risk of dislocation.
Introduction
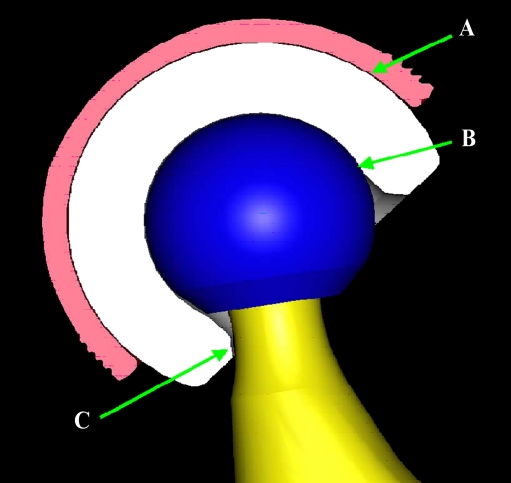
The dual mobility cup, developed by Professor Gilles Bousquet and the engineer André Rambert at the end of the 1970s, was innovative in the field of total hip replacement. Its goal was to decrease the dislocation rate by associating two articular surfaces: one with a larger diameter situated between a metallic cup and a polyethylene insert, and the other one with a smaller diameter situated between the femoral head and the retentive polyethylene insert (Fig. 1). Good midterm results have been reported [3, 21]. We report the results of a long series including 437 hips with a minimum follow-up of 15 years, as well as another series of 231 hips using the second generation insert with a minimum follow-up of five years.
Fig. 1.
The dual mobility concept (A: The larger joint; B: The smaller joint; C: The third joint)
Materials and methods
Materials
The first group of patients (group A) included hips operated on between 1984 and 1990 using the original Bousquet dual mobility cup. The second group (group B) included hips operated on between September 2000 and December 2002 with the second generation cups (Novae E®, SERF Company, Saint-Étienne, France) (Fig. 2).
Fig. 2.
Evolution between the original Bousquet dual mobilitycup (left) and the second generation cup (right)
The surgical approaches were anterolateral according to Hardinge for group A and according to Thomine for group B. In group A, the cup used was covered on its convexity by a layer of alumina ceramic. The primary stability of the metallic shell was obtained by a press-fit after adequate reaming and was enhanced by a tripod fixation system. The polyethylene insert that was mobile in the metallic shell (larger joint) always received a 22.2-mm metallic head (smaller joint). This “smaller joint” was retentive. In group B, the metallic shell was covered with a dual layer (hydroxyapatite and alumina ceramic) to facilitate bony ingrowth [9]. The shape of the metallic shell was modified to become hemispherical (anterior and posterior metallic flanges were suppressed). In order to provide a better press-fit, the polar region was also modified to become flatter. Finally, the polyethylene insert was also modified by added retentivity with chamfer to decrease contact stress between the prosthesis neck segment and polyethylene implant (which was called the “third joint”). The femoral component used was a Charnley-Kerboull (MK 3®) in group A and a Dedicace® in group B (Stryker, Pusignan, France), cemented in both groups. The diameter of the femoral head was 22.2 mm.
The characteristics of the two groups of patients are reported in Table 1. The two groups had some differences other than the modifications of the metallic cup and insert: the mean age was significantly higher in group B. In fact, in the second group, whilst awaiting more precise information concerning the polyethylene wear, we limited the use of this kind of prosthesis for patients aged more than 70 years or for younger patients with a very high risk of dislocation.
Table 1.
Demographic data of both groups
| Group A | Group B | |
|---|---|---|
| Number of THA (patients) | 437 (389) | 231 (221) |
| Mean age (range) | 61 (25–87) | 74 (38–92) |
| Males (%) | 54 | 45 |
| Charnley classification (%) | ||
| A | 69.0 | 38.5 |
| B | 16.5 | 49.8 |
| C | 14.5 | 11.7 |
| Mean BMI | 26 | 27 |
| Osteoarthritis (%) | 74 | 80 |
| Mean diameter of metal back (range) | 53 (41–63) | 53 (47–63) |
THA total hip arthroplasty, BMI body mass index
Methods
Both groups represent continuous, exhaustive and retrospective studies. A clinical and radiological survey was proposed to all patients after the surgical procedure. All patients were contacted for evaluation at the longest follow-up possible.
All prostheses having more than 15 years of follow-up in group A and more than five years of follow-up in group B were analysed clinically following the Postel and Merle d’Aubigné (PMA) classifications for function and the Charnley classification to assess the general status. The radiological analysis was performed by an independent observer (CL for group A and LA for group B), using an anteroposterior (AP) pelvic view and AP and lateral hip views before, immediately after surgery and at last follow-up. Radiological images were analysed for radiolucent lines, granulomas and signs of loosening of the acetabular and femoral components. The X-ray findings were compared to the previous films to evaluate evolution of abnormal signs. The term “loosening” was used to describe any kind of non-fixation of the components, cemented or not. The Sedel classification [20] was used to evaluate the clinical and radiological status. The cases of failure were thoroughly analysed.
We report the results using the number of hips, not the number of patients. The statistical analysis was performed using the software StatView 4.5. The comparison of the quantitative variables was performed by correlation tests using the chi-square. The qualitative variables were analysed by using tests of variance and Bonferroni-Dunn. The significance threshold was chosen for a p value of less than or equal to 0.05.
Results
The complications and results of the two groups are detailed in Tables 2 and 3.
Table 2.
Results and complications of both groups
| Group A | Group B | |
|---|---|---|
| Number of THA (patients) | 437 (389) | 231 (221) |
| Assessment at maximum follow-up | 164 | 123 |
| Deceased | 137 (31.5%) | 45 (20%) |
| Lost (%) | 92 (21%) | 28 (12%) |
| Mean follow-up (years) | 16.5 | 5.2 |
| Revisions for any causes | 44 | 1 |
| Revisions for mechanical reasons | 37 (8.5%) | 0 |
| Early luxations | 2 | 0 |
| Delayed luxations | 3 | 0 |
| Notch on femoral neck | 6 (3.7%) | 0 |
| Femoral granulomas at 5 years | 28 (6.4%) | 2 (1.6%) |
| Survival rate at 5 years (any reason) | 95.6 ± 2.3% | 99.6 ± 0.4% |
| Survival rate at 10 years | 90% | NA |
| Survival rate at 15 years | 84.40% | NA |
THA total hip arthroplasty, NA not available
Table 3.
Radiological and clinical results according to Sedel’s classification
| Resultsa | Group Ab | Group Bc |
|---|---|---|
| A | 69% | 96.7% |
| B | 11% | 2.5% |
| C | 17.7% | 0 |
| D | 2.4% | 0.8% |
aA good clinical results and no radiological problems, B good clinical results and important radiological changes, C good radiological results and poor clinical results, D poor radiological and clinical results
b16.5 years follow-up
c5.2 years follow-up
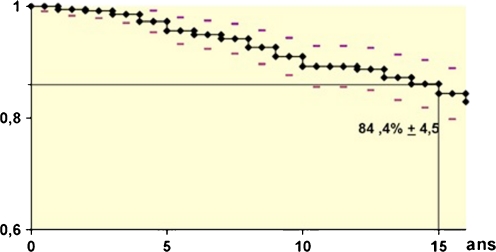
Survivorship
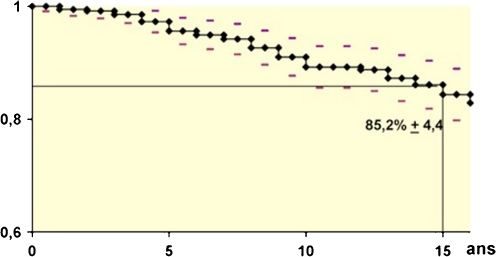
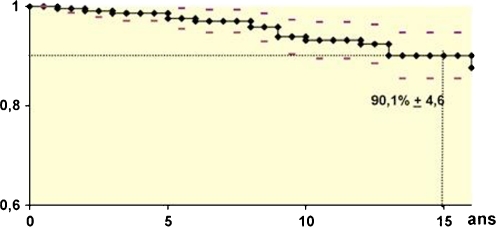
The study showed that the survivorship of the prosthesis was known for 345 hips (79%) represented by 164 prostheses with a mean follow-up of 16.5 years; 137 died with the prosthesis in place and there were 44 cases of failure. Ninety-two hips were lost to follow-up (21%). The 437 hips are taken into account in the composition of the survival curves, while patients who died and were lost widened the confidence interval from the time they were lost to follow-up. Using actuarial analysis of survival, after having defined the failure as a removal of the cup, for any reason, the overall survival rate was 84.4 ± 4.5% at 15 years of follow-up (Fig. 3). If we excluded cases of failure due to septic reasons, keeping only the 37 mechanical failures, the survival rate was 85.2 ± 4.4% at 15 years of follow-up (Fig. 4). The survival curves taking into account primary osteoarthritis (mean age at the time of surgery 64 ± 9 years) and aseptic loosening of the acetabular or femoral component as endpoint showed a survival rate of 90.1 ± 4.6% at the 15-year follow-up (Fig. 5).
Fig. 3.
Survivorship curve according to Kaplan-Meier. Endpoint: revision of the socket for any reason (group A)
Fig. 4.
Survivorship curve according to Kaplan-Meier. Endpoint: revision of the socket for aseptic reasons (infections excluded) (group A)
Fig. 5.
Survivorship curve according to Kaplan-Meier. Primitive osteoarthritis. Endpoint: revision of the socket for mechanical reasons (group A)
The failures
A total of 44 revisions were made in group A, seven for infection and 37 for mechanical causes. Among all 437 interventions, five dislocations were identified (1.1% of group A). The two “early” dislocations at four and six years were due to technical errors: an excessive anteversion of the cup and femoral stem, confirmed by a computed tomography (CT) scan in one case, and in the second case the cause was bad handling of the soft tissues after a total hip arthroplasty performed on a hip with sequelae of congenital hip dislocation. The other three cases were late intraprosthetic dislocations that occurred eight, 11 and 16 years after surgery in three women aged 39, 70 and 72 years at operation.
A total of 30 hips were revised for loosening: 15 femoral on average 13 years after surgery and 15 acetabular, including five for some form of non-integration, and ten presenting later, on average nine years after implantation. Finally, two prostheses were revised for unexplained pain.
After a mean follow-up of 5.2 years, group B showed no cases of dislocation and no revision surgery was done for aseptic loosening. Only one revision was performed for an infected case.
Patients with a follow-up of more than 15 years
A total of 164 hips (141 patients) were reviewed at a mean of 16.5 years. This population was not different from the original whole series of patients. Due to the higher average age after more than 15 years of follow-up (74 years), there were more Charnley class C (30%). Functionally, 79% were rated as excellent or very good (PMA = 18 or 17), 15% good (PMA = 16 or 15) and 6% bad (PMA ≤ 14).
The Sedel classification [19] summarises the radiological and clinical results (Table 3). In group A, 68.9% of patients were classified as A. There were 96.7% in group B at five years of follow-up.
Discussion
Dislocations
The goal is reached: in our important series of patients, only five dislocations were noted: two early in the larger joint due to technical errors and three late intraprosthetic dislocations (in the small joint). The intraprosthetic dislocation is specific for the dual mobility prosthesis [1, 10, 16]. The dislocation happens in the small joint between the head and the polyethylene insert due to deterioration of the quality of the retentive rim of the insert. The head lies on the metallic shell after verticalisation of the polyethylene insert. The total rate of 1.15% with 16.5 years of follow-up is lower than in the series of single-motion prostheses reported in the literature [7, 11, 13, 17–19, 25–27] that is estimated to be between 2% and 16%. Berry et al. [6] in their study done at the Mayo Clinic on 19,680 hips reported an incidence of dislocation of 1.8% at one year, 7% at five years and an increase of 1% per additional period of five years. At the follow-up of our group A, the dislocation rate should be 9% according to Berry’s findings, instead of the 1.15% rate that we observed. In our group B, with five years of follow-up, we had observed no dislocation. These results are consistent with other published series concerning double mobility designs [15, 22, 23].
Wear
Despite the decrease of the dislocation rate, an increase of wear could be a predictable complication due to a double surface of friction. Standard radiological methods do not measure the wear of polyethylene with precision. Lautridou et al. [14] attempted to measure the distance between the projection of the axis of the neck and the centre of the metal cup. With this rough method, wear was measured in 44 hips having a follow-up of more than 15 years and the wear was at least 3 mm for 13 of the hips. Indirect signs (granulomas) and examination of explants are to be considered as possible ways of wear assessment until measurements by radiostereometric analysis, which we are developing, become known [24]. Adam et al. [2] showed that the observation of 40 explanted inserts did not provide evidence of any significant wear of the convexity of the insert. Femoral granulomas in group A were due to standard wear that is also seen with fixed inserts [4, 12] and may also be caused by debris released by the third joint. With an equal observation time the wear was four times less common in group B using the second generation cup. However, we must bear this outcome in mind. In fact in the series, the appearance of granulomas was significantly correlated with younger age (p = 0.01) and heavy occupational activity (p = 0.008).
The third joint
The larger joint begins to function when the smaller joint has finished its range of liberty. The prosthetic neck engages the polyethylene insert, pushing on its rim. The friction between the metal neck and the rim of the insert is a genuine third joint. It occurs in extreme movements that are infrequent in normal walking. Contact occurs in flexion adduction internal rotation, external rotation and extension, which may constitute dislocating movements in a single mobility model.
Consequences:
Wear of the rim of the polyethylene insert causing debris
Deterioration of the retaining ring promoting intraprosthetic dislocation
Causes:
A neck too thick, giving an inadequate ratio of neck to “mouth” (entrance into the circle of polyethylene insert)
A non-chamfered polyethylene rim providing earlier contact creating wear
Different centres for the metal back and the insert resulting in an automatic realignment effect, which makes contact between the neck and the rim of the insert always at the same place
The second generation (Novae E®) corrected these defects based on the observation of the explants. We can therefore expect that the good results of our series at five years will continue.
The notch
A notch on the metal neck was observed in almost 4% of our historical series, despite the use of slim necks. It was due to rubbing of the neck on the metal back. It could also be the cause of metallosis. The modification of the metal back in the second generation has made it disappear.
Aseptic loosening
With regard to the revision cases for aseptic loosening in group A: the age at the time of implantation was significantly lower than the mean of the population (p = 0.0007) and the activity level significantly correlated with the loosening (p = 0.02). In contrast, the average diameter of the cup, the sex, the aetiology, the status of the contralateral hip, the cement used for the femoral stem, preserving the hip centre of rotation, and the inclination of the cup horizontally did not significantly influence the incidence of aseptic loosening. One loosening of the cup was due to an inadequate indication (post-radiation osteonecrosis).
Conclusions
Our historical series is continuous, exhaustive and consistent. It allows us to study the longevity of this initial cup of Bousquet and provide answers to questions about the dual mobility in primary total hip arthroplasty.
Our dislocation rate is low (1.15% at a mean of 16.2 years). This is a significant improvement over all series of the single mobility total hip prosthesis and it confirms the results of other series concerning dual mobility. Our rate of intraprosthetic dislocation is low due to the optimal diameter of the neck of the femoral component which is smooth, polished and without surface irregularities. The rate of dislocation is even lower with the second generation by improving the “third joint” and due to a rigorous technique, including good cup orientation. The very low dislocation rate does not justify poor positioning of the components.
It is now possible to conclude with certainty that the double mobility significantly reduces the risk of dislocation.
Even though the cup is of the first generation, the survival rate at 15 years was 85.4%, if we include the mechanical failures. This rate is comparable to many series of simple mobility but slightly below the reference couple (85% at 20 years with the Charnley prosthesis) [5, 8, 28, 29]. In our group A, the rate of femoral and acetabular aseptic loosening was 5.7%. This rate was significantly higher when the implantation was performed in a young active patient. Moreover, radiographic abnormalities, resulting from wear, deserve special attention because they are quite frequent and slowly evolving. Polyethylene wear compromises the longevity of total hip arthroplasty because of granulomatous osteolysis. It also exists with this type of implant as it does with other implants, cemented or not. Research done on the explants [2] did not show excessive wear in relation to the concept of dual mobility or the original tripod fixation.
Changes made to the design of the cup, the addition of hydroxyapatite on the convexity of the metal cup, should improve results in our series. The five-year results of the second generation model are encouraging (no dislocation, survival of 99.6 ± 0.4%, all causes of revisions included).
The principles of dual mobility have proven their effectiveness in decreasing dislocation rates. However, due to wear causing aseptic loosening, after the first decade, and especially among young active patients at the time of implantation, we reserve our current indication for patients older than 70 years of age and younger patients at high risk of dislocation.
We have implemented a prospective, randomised study comparing the wear of the double mobility designs to those with fixed insert, using radiostereometric analysis. The accuracy and reproducibility of this method are sufficiently large [24] to hope for rapid results.
Acknowledgement
A special thanks is given to Charbel Moussallem for his editorial help.
References
- 1.Adam P, Philippot R, Dargai F, Coumert S, Farizon F, Fessy MH. Double mobilité et luxation intra prothétique. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(6 Suppl):185. [Google Scholar]
- 2.Adam P, Farizon F, Fessy MH. Analyse de surface après explantation de 40 cupules rétentives à double mobilité. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:627–636. doi: 10.1016/s0035-1040(05)84466-6. [DOI] [PubMed] [Google Scholar]
- 3.Aubriot JH, Lesimple P, Leclercq S. Etude du cotyle non scellé de Bousquet dans cent prothèses totales de hanche hybrides. Recul moyen de 5 ans. Acta Orthop Belg. 1993;59(Suppl 1):267–271. [PubMed] [Google Scholar]
- 4.Avedikian J, Soyer J, Dumez JF, Muller A, Pries P, Clarac JP. L’implant cotyloïdien dans l’arthroplastie totale de Charnley. Revue de 309 dossiers avec un recul minimum de 15 ans. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(2):116–124. [PubMed] [Google Scholar]
- 5.Haute Autorité de Santé (2007) Evaluation des prothèses de hanche. www.hassante.fr/portail/upload/docs/application/pdf/rapport_evaluation_des_protheses_de_hanche.pdf
- 6.Berry DJ, Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86-A(1):9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan JJ, Heithoff BE, Goetz DD, Sullivan PM, Pedersen DR, Johnston RC. Prevention of dislocation after hip arthroplasty: lessons from long-term followup. Clin Orthop Relat Res. 2001;393:157–162. doi: 10.1097/00003086-200112000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Callaghan JJ, Templeton JE, Liu SS, Petersen DR, Goetz DD, Sullivan PM, et al. Results of Charnley total hip arthroplasty at a minimum of thirty years. A concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86-A(4):690–695. doi: 10.2106/00004623-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Epinette JA, Manley MT, D’Antonio JA, Edidin AA, Capello WN. A 10-year minimum follow-up of hydroxyapatite-coated threaded cups: clinical, radiographic and survivorship analyses with comparison to the literature. J Arthroplasty. 2003;18(2):140–148. doi: 10.1054/arth.2003.50039. [DOI] [PubMed] [Google Scholar]
- 10.Guyen O, Pibarot V, Vaz G, Chevillote C, Carret JP, Bejui-Hugues J. Unconstrained tripolar implant for primary total hip arthroplasty in patient at risk for dislocation. J Arthroplasty. 2007;22(6):849–858. doi: 10.1016/j.arth.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Huten D (1996) Luxations et subluxations des prothèses totales de hanche. In: Conférences d’enseignement de la SOFCOT. Paris: Expansion scientifique française, 1996. p. 19–46 (Cahiers d’enseignement de la SOFCOT; 55)
- 12.Keener JD, Callaghan JJ, Goetz DD, Pederson D, Sullivan P, Johnston RC. Long-term function after Charnley total hip arthroplasty. Clin Orthop Relat Res. 2003;417:148–156. doi: 10.1097/01.blo.0000096807.78689.19. [DOI] [PubMed] [Google Scholar]
- 13.Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. 2006;447:19–23. doi: 10.1097/01.blo.0000218752.22613.78. [DOI] [PubMed] [Google Scholar]
- 14.Lautridou C, Lebel B, Burdin G, Vielpeau C. La cupule rétentive, à double mobilité, non scellée de Bousquet dans l’arthroplastie totale de hanche. A propos de 437 hanches. Survie à 16.5 ans de recul moyen. Analyse des échecs. Rev Chir Orthop Reparatrice Appar Mot. 2008;94(8):731–739. doi: 10.1016/j.rco.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Leclercq S, Benoit JY, Rosa JP, Euvrard P, Leteurtre C, Girardin P. Results of the Evora dual mobility socket: five years follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:37–42. doi: 10.1016/j.rco.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Lecuire F, Benareau I, Rubini J, Basso M. Luxation intra-prothétique dans la cupule à double mobilité de Bousquet. Rev Chir Orthop Reparatrice Appar Mot. 2004;90(3):249–255. doi: 10.1016/s0035-1040(04)70101-4. [DOI] [PubMed] [Google Scholar]
- 17.Levy BA, Berry DJ, Pagnano MW. Long-term survivorship of cemented all-polyethylene acetabular components in patients > 75 years of age. J Arthroplasty. 2000;15(4):461–467. doi: 10.1054/arth.2000.4340. [DOI] [PubMed] [Google Scholar]
- 18.Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84-A(Suppl 2):2–20. doi: 10.2106/00004623-200200002-00002. [DOI] [PubMed] [Google Scholar]
- 19.Masaoka T, Yamamoto K, Shishido T, Katori Y, Mizoue T, Shirasu H, Nunodaint D. Study of hip joint dislocation after total hip arthroplasty. Int Orthop. 2006;30(1):26–30. doi: 10.1007/s00264-005-0032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nizard R, Ferrari A, Banallec L, Hamadouche M. Méthode d’étude des prothèses totales de hanche chez les patients de moins de 50 ans. Rev Chir Orthop Reparatrice Appar Mot. 1998;84:78–80. [Google Scholar]
- 21.Philippot R, Adam P, Farizon F, Fessy MH, Bousquet G. Survie à dix ans d’une cupule double mobilité non cimentée. Rev Chir Orthop Reparatrice Appar Mot. 2006;92(4):326–331. doi: 10.1016/s0035-1040(06)75762-2. [DOI] [PubMed] [Google Scholar]
- 22.Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33(4):927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Philippot R, Farizon F, Camilleri JP, et al. Survival of dual mobility socket with a mean 17 years follow-up. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:43–48. doi: 10.1016/j.rco.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 24.Pineau V, Lebel B, Gouzy S, Dutheil JJ, Vielpeau C. Dual mobility hip arthroplasty wear measurement: experimental accuracy assessment using radiostereometric analysis (RSA) Orthop Traumatol Surg Res. 2010;96(6):609–615. doi: 10.1016/j.otsr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 25.Turner RS. Postoperative total hip prosthetic femoral head dislocations. Incidence, etiologic factors, and management. Clin Orthop Relat Res. 1994;301:196–204. [PubMed] [Google Scholar]
- 26.Knoch M, Berry DJ, Harmsen WS, Morrey BF. Late dislocation after total hip arthroplasty. J Bone Joint Surg Am. 2002;84-A(11):1949–1953. doi: 10.2106/00004623-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64(9):1295–1306. [PubMed] [Google Scholar]
- 28.Wroblewski BM. 15-21-year results of the Charnley low-friction arthroplasty. Clin Orthop Relat Res. 1986;211:30–35. [PubMed] [Google Scholar]
- 29.Wroblewski BM, Fleming PA, Siney PD. Charnley low-frictional torque arthroplasty of the hip. 20-to-30 year results. J Bone Joint Surg Br. 1999;81(3):427–430. doi: 10.1302/0301-620X.81B3.9521. [DOI] [PubMed] [Google Scholar]