Abstract
Objectives:
Previous studies that have assessed the risk of developing epilepsy have failed to account for the competing risk of death, significant in the elderly where epilepsy incidence is highest. We report the lifetime risk for epilepsy, accounting for the competing risk of mortality.
Methods:
Lifetime risk and cumulative incidence of epilepsy were examined among Rochester, MN, residents between 1960 and 1979. Age-, gender-, and calendar year–specific deaths were obtained for Rochester, MN. Lifetime risk was calculated as the conditional probability of developing epilepsy by a specific age for a person reaching that age who had not yet developed epilepsy. Lifetime risk and cumulative incidence were compared for age and time period.
Results:
We identified 412 individuals with incident epilepsy diagnosed between January 1, 1960, and December 31, 1979. Lifetime risk was 1.6% to age 50 and 3.0% to age 80; cumulative incidence was 1.7% to age 50 and 3.4% to age 80. Similar differences were seen across epilepsy etiologies. Lifetime risk through 87 years of age increased over time from 3.5% in 1960–1969 to 4.2% in 1970–1979.
Conclusions:
One in 26 people will develop epilepsy during their lifetime. Lifetime risk provides an estimate of an individual's risk for epilepsy over his or her remaining lifetime, translates into the number of people who are expected to develop epilepsy, and assists health care planners as they estimate service needs for epilepsy.
Epilepsy is the fourth most common neurologic disorder with an average annual incidence of about 55 per 100,000 population in the United States1 and in Europe. The incidence curve is j-shaped with high incidence rates in infants under 1 year of age (100/100,000), falling by age 20, and remaining low (20/100,000) until age 60, when it begins a dramatic climb, reaching 175/100,000 by age 80.
The long-term risk for developing epilepsy is measured as the lifetime risk (LR), which is the probability that a person will develop epilepsy over his or her remaining lifetime.2 Because it considers the impact of the competing risk of dying, the LR is important for diseases like epilepsy, where the incidence increases dramatically in older ages. Useful to clinicians, it describes the risk of developing epilepsy in individuals from their current age through their remaining lifetime. LR is also useful for public health planning purposes because it forecasts the burden of epilepsy in the community.
LR has been measured for other diseases with high incidence in the elderly, including stroke and Alzheimer disease,3 but LR for epilepsy has not been assessed. This is relevant because the incidence of epilepsy increases dramatically beginning at age 60 years and the elderly are the fastest growing segment of the general population in developed countries. We present estimates of the LR for epilepsy in a population-based study from Rochester, MN, during the period 1960 through 1979.
METHODS
Previous studies in Rochester, MN, have assessed the incidence of seizure disorders from 1935 to 1984.1 Our case group is restricted to the subjects who developed epilepsy between 1960 and 1979. Epilepsy was defined as 2 or more unprovoked seizures and unprovoked seizures as a seizure without an identified proximate precipitant. Incident epilepsy was ascertained through the records-linkage system of the Rochester Epidemiologic Project, which links all medical records from medical facilities in Southeastern Minnesota and includes inpatient, outpatient, emergency room, doctor's private office, and home visits. We reviewed the medical records of all residents with a diagnosis of seizure, convulsion, epilepsy, or conditions known to be related to seizures.
Factors measured.
The age at epilepsy diagnosis was used in calculating cumulative incidence and LR. Separate analysis considered epilepsy diagnosis at age ≥60 years, using 5-year age groups. Epilepsy etiology was categorized as progressive symptomatic, remote symptomatic, or idiopathic/cryptogenic.4 Deaths in the general population of Rochester, MN, were obtained by age, gender, and calendar year5–8 to calculate LR.
The study was approved by the IRB at Columbia University. Data were collected by chart abstraction and consent was not obtained from subjects.
Statistical analysis.
We defined Rj as the total population at risk at any given age j.
Cumulative incidence.
We let ej equal the total number of cases in the study period at each age j. hj estimates the hazard, which is the probability that a person of age j will develop epilepsy in the next instant of time.9 We calculated hj by dividing ej/Rj. The survival probability (Sj) at each age j was calculated, using the following:
where j = 1, …, 97.
For example, to determine the cumulative hazard until age 5, hj was summated from the age of 0 until 5 with the negative result of the summation exponentiated (note: Sj = 1 when j = 0). Next, the hazard (hj) was multiplied by the survival probability at age j − 1 (fj = hj[Sj−1]), representing the age-specific incidence at age j. Finally, cumulative incidence was calculated as the summation of the age-specific incidences from age 0 to age j (Fj = Σfj).
The cumulative incidence of epilepsy does not reflect the competing risk of death prominent in the elderly where epilepsy incidence is most increased. Instead, deaths are considered to be equivalent to withdrawals with the same assumed but unassessed future risk of epilepsy as subjects who are censored alive.
Remaining lifetime risk.
Unlike cumulative incidence, the LR adjusts for the competing risk of death by considering deaths and incident epilepsy as events. That is, people who die are considered to have zero risk for developing epilepsy. To calculate LR, the variable hj* represented the adjusted hazard, computed as the deaths plus cases (ej*) divided by Rj (hj* = ej*/Rj). The adjusted hazard was used to calculate the adjusted survival probability, Uj* (Uj* = exp[−1* Σ(hj*)]). The variable fj* was calculated by multiplying the original hazard (hj) by Uj*−1, the age-specific incidence adjusted for the competing risk of death (fj* = hj[Uj*−1]). This permitted calculation of LR, a summation of the age-specific incidences from age 0 to age j adjusted for the competing risk of death (Fj* = Σfj*).
RESULTS
Incident epilepsy was diagnosed in 412 individuals between January 1, 1960, and December 31, 1979; 60.2% had partial seizures. Median age was 25.9 years with 26.9% ≥60 years at diagnosis and 49.3% were female. The number of cases increased between 1960 and 1969 and 1970–1979, representing a trajectory of growth and aging of the population. There were 465,698 person-years of exposure in 1960–1969 and 556,316 in 1970–1979 with a total of 3,885 deaths, 1,737 in 1960–1969, and 2,148 in 1970–1979. In 1970, life expectancy was 69.4 years for men and 76.8 years for women in Minnesota.10
Cumulative incidence and lifetime risk for epilepsy.
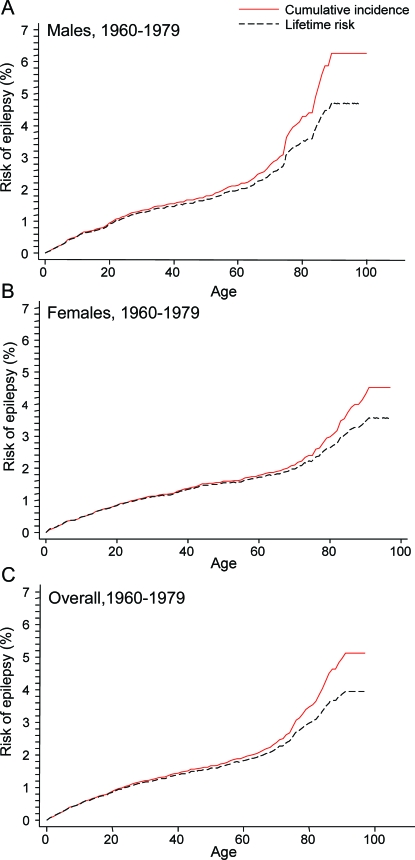
The cumulative incidence was 0.9% to age 20, 1.7% to age 50, and 3.4% to age 80 (figure 1A). The LR was 0.9% to age 20, 1.6% to age 50, and 3.0% to age 80. The curves begin to noticeably diverge at age 70 years when mortality begins to increase, demonstrating that cumulative incidence overestimates LR when the competing risk of mortality becomes large. Relative to LR, cumulative incidence was 6.6% higher at age 70–74 and 17.8% higher at age 80–84. These trends were observed for men and for women (figure 1, B and C) and by epilepsy etiology, with the greatest difference observed for progressive symptomatic epilepsy where incidence increases most dramatically in the elderly (table e-1 and figures e-1, e-2, and e-3 on the Neurology® Web site at www.neurology.org).
Figure 1. Cumulative incidence and lifetime risk for epilepsy overall and in males and females.
(A) Cumulative incidence and lifetime risk of epilepsy in males, 1960–1979. (B) Cumulative incidence and lifetime risk of epilepsy in females, 1960–1979. (C) Cumulative incidence and lifetime risk of epilepsy, 1960–1979.
Remaining lifetime risk by age.
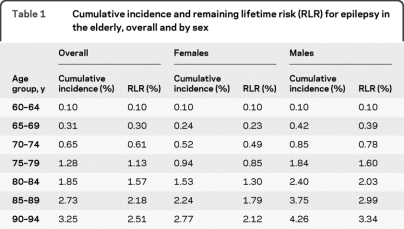
Remaining LR sets the risk at 0 for the beginning age or age group, whereas LR considers the risk from age 0 onward. To highlight the impact of increasing mortality on differences between cumulative incidence and remaining LR for epilepsy, we examined these measures in the elderly overall and by gender by 5-year age groups (table 1). With increasing mortality from age 70–74 years onward, remaining LR becomes lower than cumulative incidence.
Table 1.
Cumulative incidence and remaining lifetime risk (RLR) for epilepsy in the elderly, overall and by sex
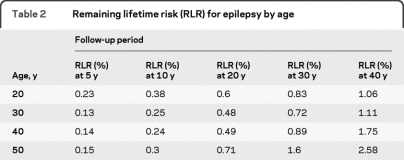
We also examined the remaining LR over a 40-year period, beginning at different ages (table 2). For a 20-year-old without epilepsy, the LR for epilepsy is 0.23% over the next 5 years, 0.6% over the next 10 years, and 1.06% over the next 40 years or until age 60 years. In contrast, for a 50-year-old without epilepsy, the LR for epilepsy is 0.15% over the next 5 years, 0.71% over the next 20 years, and 2.58% over the next 40 years or until age 90 years.
Table 2.
Remaining lifetime risk (RLR) for epilepsy by age
Time trends in the lifetime risk.
The LR of epilepsy was 3.5% through 97 years of age during 1960–1969 vs 4.2% during 1970–1979.
Number developing epilepsy.
Applying age- and gender-specific LR estimates to the July 2007 US population (301,139,947) 11,744,457 individuals (3.9%) will ultimately develop epilepsy in their lifetime.
DISCUSSION
Based upon the LR calculations in this population-based study, 1 in 26 people will develop epilepsy during their lifetime. Men have a higher risk of developing epilepsy (1 of every 21 males) than women (1 of every 28 females). This approach is more accurate than cumulative incidence, and it is better comprehended by most people who are accustomed to similar statistics provided for cancer.
Cumulative incidence has been used in etiologic studies of epilepsy and for public health purposes to determine health care needs of a population. It is useful in children, because mortality is low, and in etiologic studies. However, cumulative incidence may overestimate the risk for developing diseases with high incidence in the elderly where significant mortality represents a competing risk. This is because the cumulative incidence assumes that individuals who die before they can be observed to have the disease are assumed to have developed the disease at the same rate as those who survive.11 In contrast, LR adjusts for the competing risk of death by setting the risk for disease after death at 0, and it provides a better measure of the risk for developing epilepsy given survival to a specific age, particularly in the elderly where the risk of death due to other causes is high.12
LR can be used for individual risk prediction with the usual caveats because it is a measure based upon population estimates3 and not upon factors related to any one individual (e.g., familial life expectancy, risk factors). Even with this limitation, LR is informative about the number who will develop epilepsy, 1 in 26 people in the population, which may be easier to communicate than the percentage of people who will develop epilepsy by a given age.
The LR for epilepsy from Rochester, MN, is likely similar to that for other developed countries with comparable sociodemographics for the specific birth cohorts. However, our findings may not be applicable to other populations with markedly different death rates due to a low life expectancy, such as developing countries. Additionally, our findings will not be applicable to other populations that may have a greater incidence of epilepsy. These limitations of the LR are small, however, since the distribution of different etiologic groups may also differ in different age groups with very different expectations of life in these settings. The LR for specific epilepsy etiologies may be greater in populations where treatments of stroke, for example, have markedly improved survival thereby increasing the time period in which such individuals are at increased risk for developing epilepsy.
Our data are drawn from 1960 to 1979. This does not compromise the validity of the comparison between cumulative incidence and LR. However, with the increase in life expectancy, the LR of epilepsy should be greater than what we report, particularly for males. Between 1970 and 2005 in the United States, life expectancy has risen from 67.1 years to 75.2 years for males and from 74.7 years to 80.4 years for females.13
Using the methodology described in this article, LR has been assessed for other neurologic disorders, including stroke,3 dementia,3 and Parkinson disease.14 In the elderly, the LR for epilepsy is 0.31% for a 65- to 69-year-old and 1.6% to age 80 for a 50-year-old. In Framingham, MA, the LR is 14.3% for first stroke to age 85 for a 55-year- old and 4.0% for dementia to age 80 for a 65-year-old.
Our data suggest that almost 12 million individuals in the United States will develop epilepsy in their lifetime. The impact of this calculation is greatest in the elderly who have the highest incidence, an important concern given the aging population. Information obtained from the LR has several important uses. LR provides physicians with an estimate of an individual's risk for developing epilepsy over his or her remaining lifetime, a risk estimate that readily translates into numbers of people who are expected to develop epilepsy, and it provides useful information for health care planners estimating services needed for epilepsy.
Supplementary Material
Editorial, page 10
Supplemental data at www.neurology.org
- LR
- lifetime risk
DISCLOSURE
Dr. Hesdorffer has served on a scientific advisory board for Pfizer Inc.; has received funding for travel from UCB; serves as an Editor of Epilepsia, Editor of Epilepsy Research, and as a Contributing Editor of Epilepsy Currents; and has received research support from the CDC (DP002209 [PI]), the AUCD (RT01 [Co-I (PI of Columbia subcontract)]), the NIH (NINDS NS31146 [Co-I (PI of Columbia subcontract)]), NINDS NS043209 [Co-I (PI of Columbia subcontract)]), and NICHD HD042823 [Co-I]), and the Maternal and Child Health Bureau (MC00007 [Co-I]). Dr. Logroscino serves as an Associate Editor for Neuroepidemiology; has received speaker honoraria from Lundbeck Inc. and Novartis; serves on the Special Committee of the Italian Ministry of Health for Neuromuscular diseases; and receives research support from the University of Bari. E.K.T. Benn and N. Katri report no disclosures. Dr. Cascino serves as an Associate Editor for Neurology® and receives research support from NeuroPace, Inc., and the NIH (R01 NS53998-03 [PI]). Dr. Hauser has served on a scientific advisory board for Lundbeck, Inc. and Ovation Pharmaceuticals, Inc.; has served as a consultant for Pfizer Inc. and Intranasal; serves on the editorial boards of Acta Neurologica Scandinavia, Neuroepidemiology, and Epilepsy Research; and has received research support from the CDC [AAMC MM-1002-07/07 (PI)] and from the NIH/NINDS [5 T32 NS07153 (PI), R01 NS020656 (Co-I), R01 NS036319 (Co-I), and R01 NS043472 (Co-I)] and the Hotchkiss Neurological Institute.
REFERENCES
- 1. Hauser WA, Annegers JF, Kurland LT. Incidence of epilepsy, unprovoked seizures in Rochester, Minnesota: 1935–1984. Epilepsia 1993;34:453–468 [DOI] [PubMed] [Google Scholar]
- 2. Gaynor JJ, Feuer EJ, Tan CC, et al. On the use of cause-specific failure and conditional failure probabilities: examples from clinical oncology data. J Am Stat Assoc 1993;88:400–409 [Google Scholar]
- 3. Seshadri S, Wolf PA. Lifetime risk of stroke and dementia: current concepts, and estimates from the Framingham Study. Lancet Neurol 2007;6:1106–1114 [DOI] [PubMed] [Google Scholar]
- 4. Commission on Classification and Terminology of the International League Against Epilepsy Guidelines for epidemiological studies on epilepsy. Epilepsia 1993;34:592–596 [DOI] [PubMed] [Google Scholar]
- 5. US Department of Health, Education, and Welfare Public Health Service 950 Minnesota State Life Tables 1949–1951, vital statistics. Special Reports 1956;41(suppl 22). [Google Scholar]
- 6. 1960 Minnesota State Life Tables 1959–1961. Public Health Service Publication No. 1252. 1960;2(24). [Google Scholar]
- 7. 1970 U.S. Decennial Lifetables 1969–1971. DHEW Publication No. HRA 75-1151. 1970;2(24). [Google Scholar]
- 8. 1980 U.S. Decennial Lifetables 1979–1981. DHEW Publication No. PHS 86-1151-24. 1980;2(24). [Google Scholar]
- 9. Klein JP, Moeschberger ML. Survival Analysis: Techniques for Censored and Truncated Data, 2nd ed. New York: Springer Science + Business Media, LLC; 2003 [Google Scholar]
- 10. Vital Statistics of Women (2004): Minnesota and the United States. Legislative Status Report on the Economic Status of Women. Available at: http://www.commissions.leg.state.mn.us/oesw/fs/vitalstats.pdf Accessed October 29, 2008 [Google Scholar]
- 11. Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet 1999;353:89–92 [DOI] [PubMed] [Google Scholar]
- 12. Schouten LJ, Straatman H, Kiemeney LALM, Verbeek ALM. Cancer incidence: life table risk versus cumulative risk. J Epidemiol Community Health 1994;48:596–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kung HC, Hoyert DL, Xu JQ, Murphy SL. Deaths: Final data for 2005. National Vital Statistics Reports; vol 56 no 10. Hyattsville, MD: National Center for Health Statistics; 2008 [PubMed] [Google Scholar]
- 14. Driver JA, Logroscino G, Gaziano JM, Kurth T. Incidence and remaining lifetime risk of Parkinson disease in advanced age. Neurology 2009;72:432–438 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.