Abstract
Research indicates that major depressive disorder (MDD) is associated with alterations in autonomic control, particularly cardiac control as measured by heart rate variability (HRV). In this preliminary study, we investigated the neural correlates of autonomic control by measuring both HRV and associated brain activity during the performance of mildly stressful tasks. Medically healthy female subjects with MDD (N=10) and healthy controls (N=7) underwent H2 15O-PET and ECG recording while performing a handgrip motor task and an n-back task. Indices of HRV were calculated and correlated with regional cerebral blood flow (rCBF). Differences in the rCBF and HRV correlations between depressed and healthy subjects were evident in both the medial and lateral orbital cortices. In addition, these areas appeared to be involved in different facets of autonomic control with regard to sympathetic or parasympathetic dominance of cardiac control. These results are consistent with the known roles of networks within the orbital cortex in both autonomic control and the pathophysiology of MDD.
Keywords: Autonomic, PET, MRI, depression, brain
1. Introduction
Homeostasis in the body is controlled by the autonomic nervous system, which can be divided into the sympathetic and parasympathetic systems. The physiological alterations occurring with major depressive disorder (MDD) extend beyond the brain, partly by altering the influence of these autonomic networks on a wide array of physiologic systems. Depressed subjects have been shown to exhibit gastric dysmotility, possibly as a result of increased sympathetic modulation (Ruhland et al., 2008). Depressive symptoms have been associated with increased sympathetic vascular resistance in response to stress (Matthews et al., 2005). Finally, alterations in the autonomic nervous system modulating corticotrophin releasing hormone and central noradrenergic systems are commonly found in MDD (Gold and Chrousos, 2002).
The most commonly studied aspect of the concurrence of MDD and autonomic dysfunction involves cardiac autonomic control of heart rate variability (HRV). Although controversy exists within the literature, most studies indicate that subjects with MDD show reduced parasympathetic/vagal control of cardiac activity as compared to healthy controls (Udupa et al., 2007), and vagal control appears to be negatively correlated with depression severity (Agelink et al., 2001; Agelink et al., 2002). In addition, depressed subjects show greater values of the autonomic index LF/HF, which may indicate a preponderance of sympathetic to parasympathetic control, as compared to healthy control subjects (Udupa et al., 2007). Depressed subjects also show reduced baroreflex sensitivity (Davydov et al., 2007). A recent study in male twins showed that depressive symptoms were associated with reduced HRV. In this study, when HRV was compared within twin pair between the twin with higher depressive symptoms and his brother, dizygotic, but not monozygotic, twins exhibited significant differences in the full HRV spectrum, indicating a genetic influence on the association (Vaccarino et al., 2008).
Multiple brain regions participate in the modulation of autonomic responses, and there is considerable overlap between regions regulating autonomic function and regions modulating emotional behavior. In particular, the anatomical connections between the cingulate gyrus, medial orbitofrontal cortex (MOFC), anterior insula, and amygdala, and their projections to basal forebrain structures and brainstem nuclei, form an extended “visceromotor” network which plays a major role in modulating the autonomic, endocrine, and behavioral aspects of emotional and motivated behavior (Ongur and Price, 2000; Ongur et al., 2003). Physiological activity in both the subgenual ACC (Drevets et al., 1997; Drevets et al., 2002; Neumeister et al., 2006) and the amygdala (Drevets, 1999) is elevated in subjects with MDD in the depressed phase relative to the remitted phase of MDD, to an extent that correlates positively with depression severity. Activity in the anterior insula also increases during depressive episodes in MDD (Drevets et al., 1992). Electrophysiological studies in humans and experimental animals, along with functional neuroimaging studies in humans also have implicated these visceromotor areas in central autonomic regulation (Price, 1999; Ter Horst et al., 1996; Westerhaus and Loewy, 2001).
Previous studies assessed the neural correlates of HRV during a variety of mood states in healthy subjects. For example, Lane, et al. (Lane et al., 2009) reported that the putative vagally mediated component of HRV correlated with changes in regional cerebral blood flow (rCBF) during emotion induction (happiness, sadness, and disgust) as compared to neutral stimuli in the medial prefrontal cortex (Medial PFC, BA 10) and left insula. Another study found a correlation between total vagal HRV and the difference in BOLD response in the left insula during unpredictable aversive electrical shocks delivered in a synchronous manner with respect to the ECG R-wave, versus shocks delivered at a delay following an R-wave (Gray et al., 2009). That study also found that the change in vagally mediated HRV correlated with the change in BOLD response during delayed versus synchronous shocks in the amygdala and periaqueductal grey (PAG). In addition, there is substantial evidence from the literature supporting central mediation of cardiac control during task performance. For example, Napadow et al. showed that parasympathetic HR modulation correlated with BOLD response during a handgrip task in a variety of areas, most notably the posterior insula and amygdala (Napadow et al., 2008). Additionally, Critchley, et al. found that changes in hemodynamic activity in the ACC, OFC, and insula were associated with HRV during both a predominately motor task (handgrip) and a predominantly cognitive task (n-back) (Critchley et al., 2003).
The current study extends these studies in healthy subjects to depressed individuals. We applied neuroimaging of rCBF to determine how neurophysiological activity differentially correlates with autonomic tone in brain regions implicated in the regulation of both autonomic and emotional function in healthy versus depressed individuals. As the first investigation to correlate neuroimaging findings and indices of autonomic tone in subjects with MDD, this preliminary study investigates differences in neural correlates of autonomic cardiac control to elucidate the neurobiological underpinnings of autonomic dysfunction in mood disorders.
2. Methods
2.1 Subjects
In order to eliminate potentially confounding our results by gender differences, this preliminary study included female subjects only. This population may be particularly relevant to studies of depression, since MDD occurs twice as often in women as in men (Kessler et al., 1993), and following an adverse cardiac event, this gender gap widens even further (Gottlieb et al., 2004; Wiklund et al., 1993). Our sample included seventeen right-handed (two subjects exhibited mixed handedness), medically healthy females. Ten met DSM-IV criteria for MDD as established by both the Structured Clinical Interview for DSM-IV and an unstructured diagnostic interview with a psychiatrist, and seven had no personal or family history (in first degree relatives) of mood disorders. Given the small sample size, we consider this to be a preliminary study. All subjects had been free of psychotropic medication for at least three weeks (eight weeks for fluoxetine). This study was approved by the NIMH Institutional Review Board, and all subjects provided informed consent.
Prior to this study, subjects underwent medical and psychiatric evaluation, physical examination, laboratory testing (complete blood count, electrolytes, liver and thyroid function tests), ECG, and neuromorphological MRI. Exclusion criteria included having cardiovascular disease, history of cardiac arrhythmias, anemia, electrolyte disturbances, ECG abnormalities, exposure to medications (except nicotine) likely to affect CBF or cardiovascular function in the two weeks prior to scanning, meeting DSM-IV criteria for drug or alcohol abuse within 1 year, or lifetime history of alcohol or drug dependence. Pregnant or lactating women, women with irregular menstrual cycles, and post- or peri-menopausal women also were excluded. Of the healthy subjects, four were studied in the follicular phase of the menstrual cycle, two in the luteal phase, and one while actively menstruating (menstrual phase was assessed using a home ovulation test). Of the depressed subjects, six were studied in the follicular phase, two in the luteal phase, and two while actively menstruating. One healthy subject was a past smoker, and two healthy and two depressed subjects were current smokers. Depression severity was rated using the Beck Depression Inventory (BDI) (Beck et al., 1961) and the Montgomery-Asberg Depression rating scale (Montgomery and Asberg, 1979).
2.2 Study Design and Tasks
Neurophysiological measures were obtained using the PET-rCBF technique, and electrophysiological measures were obtained simultaneously using ECG. While undergoing PET and ECG, subjects either rested with eyes fixed on a cross-hair, or performed working memory or motor tasks of varying difficulty level.
In the baseline fixation task, subjects were asked to fix their eyes on a cross-hair presented on a video monitor for 150 seconds; this block occurred twice. In the motor task, subjects were asked to squeeze a handgrip dynamometer (Interface, Inc. Scottsdale, AZ) with their dominant hand to match an intensity target set at three strength levels (10, 30, and 50% of each subjects' maximal effort, thus the task was calibrated according to each individual's strength). Subjects were instructed to squeeze the dynamometer for 9 seconds, then relax for 6 seconds (15 seconds total), This sequence was repeated 10 times within each strength level block so that each handgrip block was a total of 150 seconds in length. The cognitive task consisted of a working memory n-back task at three levels of difficulty (1-back, 2-back, and 3-back), using pseudo-random sequences of consonant letters. Each letter was presented for 500ms, followed by a 2.5s inter-stimulus interval during which a fixation cross-hair was displayed. Subjects were asked to respond to target stimuli, consisting of a letter identical to the letter presented one, two, or three trials before, for the 1-back, 2-back, and 3-back, respectively. Each difficulty level block consisted of 50 trials (150 seconds total). Subjects were instructed to respond to target stimuli with their right hand using a button box. Of the 50 stimuli presented in each block, 33% were target stimuli. In both motor and cognitive tasks, blocks of each difficulty level were presented twice, and block order was counterbalanced across subjects.
2.3 Behavioral Assessments
During the handgrip task, performance was calculated by measuring the area under the grip intensity vs. time curve. The parameter “handgrip accuracy” was calculated as deviation of the ratio of actual grip strength and target grip strength from one. During the n-back task, the composite performance measure “n-back accuracy” was calculated as the sum of the correct responses minus the total number of incorrect responses, divided by the total number of trials.
2.4 Autonomic measurements
The ECG data were collected at 500 Hz during scanning using a 1902 amplifier and Power1401 data acquisition interface (Cambridge Electronic Devices, Cambridge, UK). Spike2 software (Science Products GmbH, Hofheim, Germany) was used to detect R-spikes, and a time series of inter-beat intervals was extracted from R-spikes acquired during the last 120 seconds of each behavioral block. Previous research using 120 second recording epochs has shown that both LF power and HF power can be accurately assessed with epocs of this length compared to longer recording epocs (De Rivencourt, 2008). HRV indices were computed according to published guidelines using an autoregressive algorithm (Colombo et al., 1989). Briefly, the high frequency component (HF), which is mediated almost entirely by parasympathetic activity transmitted via the vagus nerve (Akselrod et al., 1985; Pomeranz et al., 1985) was calculated from the ECG power spectrum from 0.15 to 0.5 Hz. The peak frequency within this band, fHF, is proportional to average respiratory frequency and was calculated so that respiratory effects could be controlled for (Thayer et al., 2002; Yildiz and Ider, 2006). The low frequency component (LF), which partially reflects sympathetic tone (Malliani and Pagani, 1991; Malliani et al., 1994), but is dominated by parasympathetic tone (Thayer et al., In Press) and respiration (Yildiz and Ider, 2006), was calculated from the ECG power spectrum from 0.01 to 0.15 Hz. From these data, we calculated natural logs of total low and high frequency power (lnHF and lnLF) and the ratio LF/HF, which putatively reflects the relative balance of sympathetic and parasympathetic tone (Malliani et al., 1990). Finally, the time domain parameter RMSSD, a measure of parasympathetic tone, was calculated as the root mean squared difference of successive R-R intervals as a measure of beat-to-beat variability (Bigger et al., 1993; 1996).
2.5 PET Image Acquisition
Subject preparation for PET scanning included intravenous cannulation and head stabilization using a thermoplastic mask. Emission images were acquired using a GE Advance (35 contiguous slices with 4.25mm plane separation, 3D resolution=6 to 7mm FWHM, 3D acquisition mode) following 10 mCi of H2 15O administration during each of the 14 behavioral blocks. Slow infusions of H2 15O were initiated 30 seconds before scanning (at the beginning of each behavioral block) and continued for 120 seconds. Acquisition of the PET data was limited to the final 120 seconds to allow for inflow of the tracer. HRV indices were calculated for this same 120 second interval. Transmission scans (about 8 min) were acquired using rotating rods of 68Ge/68Ga for attenuation correction.
2.6 Statistical Analysis
Autonomic variables were analyzed in SAS (SAS Institute, Cary NC), using a repeated measures mixed model with difficulty level and diagnosis as factors, and age as a covariate. Because the parameter fHF is proportional to respiratory rate, it was used as a covariate in all analyses. A variance-component covariance structure was used, and diagnosis was incorporated into the covariance matrix when modeling autonomic variables in which variances differed significantly across groups. To assess the relationship between performance and autonomic activity, the mixed model was repeated with the accuracy measure entered as a covariate. A post-hoc 2×2 ANOVA where autonomic variables were averaged across task difficulty level was performed to assess the significance of any differences in autonomic variables due to diagnosis and task factors.
Image analysis was performed using SPM2 (Wellcome Department of Imaging Neuroscience, University College London, London, UK) within Matlab 6 or 7 (Mathworks, Natick, MA, USA). PET images were realigned, and then co-registered to structural T1 MRI scans. The MRI scans were acquired at 3 Tesla using MP-RAGE or IR-fSPGR pulse sequences (0.86mm in-plane resolution; 1.2 mm slice thickness). The accuracy of co-registration to the PET images was indistinguishable between these two MRI scan types. The MRI scans were spatially normalized to a template brain, and the resulting transformation then was applied to the co-registered PET images. In order to compute correlations between rCBF and autonomic indices, a multi-group conditions-and-covariates model was constructed for each index. Each model included six conditions (one each for the fixation, handgrip, and N-back tasks in each diagnostic group). Age and fHF (peak high frequency, proportional to respiratory rate) were included as nuisance variables. Covariates for task difficulty level and autonomic variable were allowed to interact by condition, so that the correlation between rCBF and autonomic variable was estimable for each diagnostic group separately. Subject grand means were scaled to 50 within group, and global normalization was performed using an AnCova by subject (within group).
Contrasts for positive and negative correlations between rCBF and each autonomic index during the performance of each task were calculated for the healthy and depressed subjects separately. Additional contrasts were performed to show areas where the correlation between rCBF and the autonomic index differed significantly between groups. Regression coefficients, which are the extracted beta weights from the SPM2 general linear model, are reported to indicate the magnitude of the dependence of rCBF on the autonomic index.
To reduce the likelihood of Type-I error, the search area included in the primary analysis was limited to regions of interest (ROI) defined a priori on the basis of previous literature that reported brain structures where neurophysiological and autonomic activity were correlated. The ROI selected were the left and right anterior cingulate cortex, anterior insula, amygdala, and OFC. The anterior insula ROI encompassed the agranular insula and the sulcal portion of LOFC (BA 47s, see (Ongur et al., 2003)). For each ROI, a binary mask was drawn on the MRI template used for spatial normalization. Small volume corrections (Worsley et al., 1996) were applied to adjust the results of the SPM analyses for the effects of multiple testing, and results were reported for pcorrected < 0.00625 (calculated as 0.05 divided by 8, the number of a priori regions).
To reduce the likelihood of Type-II error, areas located outside the predefined ROI were explored in whole brain analyses conducted post hoc. For each contrast, t-images were displayed with a threshold of puncorrected <0.05. Gaussian random field theory was used to identify clusters which remained significant at pcorrected<0.05 after applying the cluster test to correct for multiple comparisons (Poline et al., 1997). Within each significant cluster, the voxel with the highest voxel t-value is reported. Voxels were also reported for which the voxel-corrected p-value was significant at pcorrected<0.05. A conjunction analysis of the handgrip and n-back contrasts was performed to confirm the significance across both tasks.
Finally, to ensure that any differences noted between groups in the correlation between rCBF and autonomic activity were not due to absolute differences in rCBF between healthy and depressed subjects, we averaged across task difficulty and used a two-sample t-test in SPM to assess group differences. Subject grand means were scaled to 50 within group, and global normalization was performed using proportional scaling.
3. Results
3.1 Behavioral and autonomic results
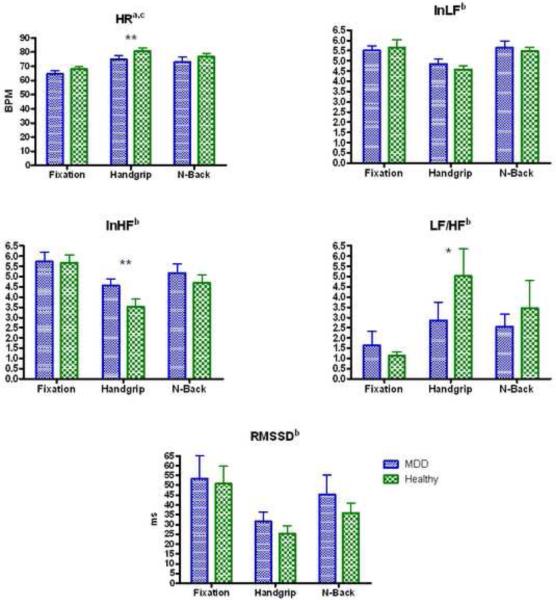
Demographic data and clinical ratings of depression severity for subjects appear in Table 1; there was no significant difference between MDD and control subjects on age, body-mass-index (BMI), blood pressure, or distance traversed in the walk-run task (only five subjects from each group completed the walk-run task). Performance accuracy did not differ between groups on either the motor task or the N-back task. There was no difference between groups in baseline autonomic function, as assessed during the resting fixation condition (p>0.05), although there was a dependence of LF/HF on age (F1,13=6.65, p=0.0229). Likewise, in the n-back condition there was no difference in autonomic function between groups, although HR, lnHF, and lnLF were significantly dependent on age (p=0.0215, p=0.0488, and p=0.0438, respectively). During the handgrip condition, healthy controls exhibited higher HR (F1,14=5.10, p=0.0405) and a trend toward greater LF/HF (F1,14=3.84, p=0.0703) as compared to MDD subjects, while MDD subjects showed greater lnHF than controls (F1,14=9.56, p=0.008).
Table 1.
Demographic information for subject groups. The groups did not differ significantly on any parameter.
| Age | BMI | BP-Systolic | BP-Diastolic | Walk-Run Distance (m) | BDI | MADRS | |
|---|---|---|---|---|---|---|---|
| MDD (N=10) | 33±9.9 | 22.6±3.8 | 112±12.5 | 69±7.7 | 1602 ± 277.1 (N=5) | 26±13.9 (N=9) | 25±9.3 (N=10) |
| HC (N=7) | 31±9.3 | 23.7±6.8 | 104±11.6 | 66±7.8 | 1369 ± 233.0 (N=5) | 1±2.2 (N=7) | 0±0 (N=7) |
When accuracy was included as a covariate in the analysis of the n-back task data, lnLF was significantly dependent (F1,30=6.13, p=0.0191) and lnHF showed a nonsignificant trend toward dependence (F1,30=3.98, p=0.0552) on performance. For the handgrip task, however, the autonomic variables and performance accuracy were not correlated. The post-hoc ANOVA showed all autonomic variables were significantly dependent on task (Figure 1). For all autonomic variables, there was no significant diagnosis × task interaction, so the interaction terms were not included in the model.
Figure 1.
Autonomic variables (mean + SEM) for each task by group.
aMain effect of task significant by ANOVA at p<0.001
bmain effect of task significant by ANOVA a p<0.05
cMain effect of group trended towards significance at 0.05<p<0.1
** Main effect of group significant at p<0.05 in the mixed model for a given task
* Main effect of group trended towards significance at 0.05<p<0.1
3.2 Imaging Results
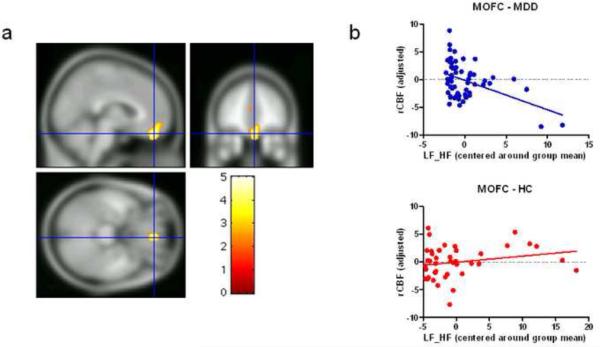
Data for the ROI defined a priori appear in Table 2. In the handgrip task, control subjects showed a negative correlation between rCBF and HR in the anterior insula, while MDD subjects exhibited positive correlations between CBF and lnHF in the LOFC (BA47). In both fixation and n-back conditions, the controls showed positive correlations between rCBF and RMSSD in the right amygdala. When the depressed subjects and controls were compared directly, the controls showed a positive correlation between rCBF and LF/HF while depressed subjects showed an inverse correlation in the right orbital cortex ROI, in an area of the MOFC (Talairach coordinate 6, 45, −22, Z=4.29).
Table 2.
Areas within the regions of interest defined a priori where the correlations between autonomic indices and rCBF remained significant after applying small volume corrections for multiple comparisons in the depressed or control samples.
| Autonomic Index | Diagnoisis | Task | ROI for SVC | Region | Direction of Correlation | Voxel Z | Talairach Coordinatec |
|---|---|---|---|---|---|---|---|
| Heart Rate | Control | Handgrip | LAI | Anteior Insula | − | 4.29a | −34 18 3 |
| InHF | MDD | Handgrip | ROC | Orbitofrontal Cortex, BA 47b | + | 4.41a | 34 40 −12 |
| RMSSD | Control | Fixation | RA | Amygdala | + | 3.68a | 22 −5 −13 |
| NBack | RA | Amygdala | + | 3.68a | 16 −7 − 15 |
Indicates that the voxel is significant in SVC at p≤0.001 (family-wise error)
The BA47 region corresponded to the rostral portion of BA47 which (Hansen et al. 2003; Ongur et al. 2003).
Stereotaxic coordinates correspond to the spatial array of Talairach and Tournoux (1988) in which values Kindicate the distance in mm from the origin (anterior commissure), with positive x indicating right, positive y indicating anterior, and positive z indicating dorsal to a plane containing both the anterior and posterior commissures.
Abbreviations: LAI=left anterior insula, RAI=right anterior insula, RA=right amygdala
The whole brain analysis showed additional regions where rCBF and the autonomic indices were significantly correlated. Since the primary focus of this manuscript is to describe differences between healthy subjects and subjects with MDD, we discuss only between-group differences, within-group results are available in the supplementary materials (supplementary tables 1 and 2). The whole brain analysis also revealed clusters of significant effects within the anterior insula that were not encompassed within the predefined ROI for this region, and thus were not included in table 2.
The regions where the dependence of rCBF on an autonomic index differed significantly between groups appear Table 3. Notably, the differences between groups were primarily evident during task performance; the only difference between groups during fixation involved the relationship between RMSSD and rCBF in the fusiform gyrus, where control subjects showed a positive correlation, and depressed subjects showed essentially no correlation. During the handgrip task, where we showed a significant difference between groups in mean HR, and a nonsignificant trend towards a difference between groups in mean LF/HF, we also found concomitant differences in rCBF between groups, in the precentral gyrus (HR) and MOFC (LF/HF). Although we found a significant difference in mean lnHF between groups during the handgrip tasks, we found no corresponding rCBF effects. Although lnLF did not differ between groups during the handgrip task, the relationship between lnLF and rCBF during the handgrip task differed significantly between groups in the cerebellum.
Table 3.
Regions identified in the whole brain analysis where control and depressed subjects significantly differed in their associations between rCBF and cardiac autonomic indices. The region name and sterotaxic coordinates of each cluster maxima are given, as well as other voxels remaining significant after applying voxel-wise corrections for multiple testing within and outside significant clusters. Regression coefficients from the general linear model are given, with the larger regression coefficient shown in boldface.
| Autonomic Index | Regresson Coefficient Healthy | Regression Coefficient MDD | Task | Region | Voxel Z | Talairach coordinated |
|---|---|---|---|---|---|---|
| HR | 0.3167 | −0.1229 | NBack | Lateral Superior Frontal Gy | 5.00a,b | −18 28 56 |
| 0.3293 | −0.1296 | Superior Parietal C | 5.28b | −30 −66 46 | ||
| −0.1493 | 0.0772 | Dorsomedial Superior Frontal Gy | 4.58c | −12 −17 43 | ||
| −0.3485 | 0.1067 | Parieto-Occipital C | 5.20b | 20 −72 44 | ||
| −0.3004 | 0.1112 | Handgrip | Precentral Gy | 4.85b,c | 48 2 40 | |
| InHF | −1.5069 | 1.032 | NBack | Lingual Gy | 3.72c | 8 −56 1 |
| InLF | −1.8206 | 0.4887 | Handgrip | Cerebellum, Declive | 4.18a | −44 −66 −17 |
| 2.4199 | −0.6527 | NBack | Brainstem, Pons | 4.23a | −16 −34 −33 | |
| LF/HF | 0.2254 | −0.6262 | Handgrip | Medial Orbitofrontal C (BA 10r) | 4.85b,c | 4 44 −22 |
| 0.1787 | −0.8616 | Nback | Temporal Polar Cortex | 4.69a | 46 −21 −28 | |
| RMSSD | 0.1351 | −0.0450 | Fix | Fusiform Gy | 4.76b | −46 −47 −8 |
| 0.1256 | −0.0003 | Nback | Ventrolateral PFC | 3.94a | 46 27 6 | |
| −0.1157 | 0.0050 | Medial Cerebellum | 3.23a | −6 −67 −22 |
significant at p≤0.05 after applying corrections for multiple comparisons using the cluster test
significant at p≤0.05 (family-wise error) after voxel-wise correction for multiple comparisons
significant at p≤0.001 after applying corrections for multiple comparisons using the cluster test
Stereotaxic coordinates and Abbreviations interpreted as in Table 2
During the n-back task, although we found no significant behavioral differences between groups, the relationship between HR and rCBF differed significantly between the MDD and control groups in the lateral superior frontal gyrus, superior parietal cortex, dmSFG, and parietooccipital cortex; between lnHF and rCBF in the lingual gyrus; between LF/HF and rCBF in the temporal polar cortex; and between RMSSD and rCBF in the ventrolateral PFC and medial cerebellum.
In the MOFC, during the handgrip task the controls showed a positive relationship between LF/HF and rCBF, while the depressed subjects showed a negative correlation (Figure 2). The differential relationships between rCBF and the autonomic parameters that accounted for group differences in other regions are indicated in table 3.
Figure 2.
a) Illustration of the cluster within medial orbitofrontal cortex (MOFC) in which the correlation between rCBF and LF/HF differed significantly between subjects with MDD and healthy controls. The t-value image was thresholded at the voxel p-value of p<0.01 uncorrected, with a cluster extent 300 voxels b) The rCBF, adjusted for regressors of no interest, plotted versus the mean centered LF/HF for the voxel within the MOFC cluster shown in a) with the peak t-value (x=4, y=44, z=−22).
The globally normalized rCBF differed between groups in the dorsolateral PFC during all conditions tested, and in the fusiform gyrus in the handgrip task (Table 4).
Table 4.
Regions where normalized rCBF differed significantly between depressed and control groups during each behavioral condition.
| Task | Contrast | Region | Voxel Z | Talairach coordinate |
|---|---|---|---|---|
| Fixation | HC > MDD | Dorsolateral PFC | 4.40b | 32 27 37 |
| Dorsolateral PFC | 4.05a | −22 42 24 | ||
| Handgrip | HC > MDD | Dorsolateral PFC | 3.83a | 32 29 35 |
| Fusiform Gy | 3.72a | 32 −70 −10 | ||
| N-Back | HC > MDD | Dorsolateral PFC | 4.26a | −22 38 22 |
| Dorsolateral PFC | 3.99b | 22 36 26 |
significant at p≤0.05 after applying corrections for multiple comparisons using the cluster test
significant at p≤0.001 after applying corrections for multiple comparisons using the cluster test
Stereotaxic coordinates and Abbreviations interpreted as in Table 2
4. Discussion
We demonstrated significant differences between healthy and depressed subjects in the electrophysiological indices and the neurophysiological correlates of HRV. Although these results must be considered preliminary due to the small sample sizes, they support the application of our experimental paradigm as a strategy for elucidating the neural bases of autonomic dysregulation in MDD. While performing motor and cognitive tasks designed to differentially modulate autonomic function, subjects from both groups exhibited an overall decrease in HRV, suggesting withdrawal of parasympathetic control of the cardiac cycle, and an increase in the ratio of sympathetic-to-parasympathetic control of the HR. In depressed subjects, however, while we found no significant difference in baseline autonomic function relative to controls, HR was lower and lnHF higher than in controls during the motor task, possibly reflecting an attenuated parasympathetic withdrawal response to stress in MDD. In addition to the cardiovascular results, our neuroimaging analyses revealed significant differences between depressed and healthy subjects in the correlations between rCBF and autonomic indices in multiple regions associated with emotional and autonomic function. Of particular interest, correlations between rCBF and HRV differed between groups in the FPC/MOFC, and dorsomedial superior frontal gyrus (dmSFG).
As reviewed earlier, findings in the literature indicate reduced vagal control of HRV in depressed subjects assessed under resting conditions. We did not find differences in these autonomic parameters in the resting, fixation point task, which may be related to our small sample size. In contrast, during the handgrip task the lnHF was greater in depressed females than in controls. We interpret this as an attenuated parasympathetic withdrawal response under the mild stress associated with this task in MDD. In a recent study of healthy volunteers, using a number generation task, Shinba et al. (Shinba et al., 2008) found that subjects with higher anxiety and depressive symptom rating scale scores exhibited attenuation of the change in HRV in response to a stressful task, consistent with our results. Furthermore, others have shown in a resting state that females with MDD exhibit increased HRV, in contrast to males with MDD, who showed reduced HRV (Chambers and Allen, 2007; Thayer et al., 1998).
The neuroimaging data revealed areas where the relationships between autonomic indices and rCBF differed between depressed and healthy subjects. Given the relevance of the visceromotor network to both depression and autonomic control, the results in the MOFC particularly merit comment. We found a significant difference between healthy and depressed subjects in the correlation between LF/HF and rCBF in the MOFC and FPC (BA 10p) during the handgrip task. Area 10p is part of the medial prefrontal network which projects to numerous subcortical autonomic control areas, including the medial hypothalamic nuclei, the dorsolateral column of the PAG, and the dorsal part of the central nucleus of the amygdala (reviewed in (Drevets et al., 2008)), as well as the ventral tegmental area and medial dorsal thalamus (Drevets, 2007). In addition, the MOFC is hypothesized to support a representation of autonomic state during motivational tasks (reviewed in (Nagai et al., 2004)). Our results suggest that differences in the function of this network between healthy and depressed subjects may underlie the neurophysiological basis for alterations in autonomic activity in subjects with MDD.
The ventromedial FPC/MOFC area where rCBF showed differential correlations with LF/HF in depressed versus healthy subjects corresponds to areas where we previously showed metabolic increases in depression that were correlated positively with depression severity (Hasler et al., 2008). Histopathologic abnormalities also have been found in depressed subjects in the FPC, including reductions in myelin basic protein (Honer et al., 1999), and reductions in glial cells as compared to healthy controls (reviewed in (Drevets, 2007)). Impaired ventromedial FPC/MOFC function may alter the balance of sympathetic and parasympathetic autonomic regulation during stress consistent with our observation that ventromedial FPC/MOFC function increases along with sympathetic activation during the hand-grip task in healthy controls but not in depressed subjects.
Also of particular interest was the finding in the dmSFG, where the relationship between rCBF and HR differed between depressives and controls. Neurophysiological activity has been found to increase in the dmSFG during modified n-back tasks, and subjects with lesions of the superior frontal sulcal cortex exhibit deficits in performance on working memory tasks derived from the n-back paradigm (du Boisgueheneuc et al., 2006). This area has also been reported to show sustained hemodynamic activity during the delay between stimulus presentation and the recall performance associated with working memory tasks (Petit et al., 1998).
While the results from this study suggest that central neural control underlies differences in autonomic responses found between depressed and healthy subjects, the pathological mechanisms giving rise to this interaction in MDD are unknown. It has been hypothesized that alterations in HRV in depressed subjects are mediated by dysfunction arising in the central serotonergic system (Hildreth et al., 2008). The extant data indicate that 5HT1A function and binding are reduced in multiple regions in depressed humans (reviewed in (Drevets et al., 2008; Nugent et al., 2008)), and 5-HT1A receptor function has been linked to autonomic function in studies of experimental animals. (Dando et al., 1998; Skinner et al., 2002).
Several issues regarding this study's methodology merit comment. There are limitations to using correlational data to identify mechanisms. When both rCBF in a certain area and an autonomic index increase during task performance, this may not necessarily indicate that the identified region contributes to autonomic control. Such an association may instead indicate that rCBF in the region and the autonomic index both increase in response to increasing difficulty, mediated by separate mechanisms. In addition, group differences in activity in these regions may be due to a task by diagnosis interaction in hemodynamic activity. Studies examining the correlation between n-back task difficulty and brain activation have identified differences in healthy vs. depressed samples in our primary ROIs, namely the subgenual ACC and MOFC (Rose et al., 2006). It remains unclear if these between-group differences reflect differing cognitive processes between groups, or differences in autonomic response. Furthermore, some of the areas identified in our post-hoc whole brain analysis overlap with areas previously reported to show differences between healthy and depressed subjects during n-back task performance without consideration of autonomic data (Fitzgerald et al., 2008; Harvey et al., 2005; Matsuo et al., 2007; Walsh et al., 2007). Thus, the conclusions from this study must be interpreted in light of the literature identifying regions known to participate in autonomic regulation.
Another limitation of this study is that females were not studied in the same phase of their menstrual cycle, given that HRV may be modulated by gonadal steroids (Sato and Miyake, 2004). While this limitation may have contributed to Type II error, it would not account for differences between groups, since the proportions of each group studied within a particular menstrual phase were similar. In addition, the relatively small size of the samples may have reduced our sensitivity to detect differences between groups, and increased our Type II error. Therefore, our findings must be considered preliminary. Finally, given the prominent gender differences in neural control of HRV, the results of our study cannot be generalized to males.
Although HRV has been studied extensively in MDD, this study was unique in its exploration of neural correlates of autonomic function through PET imaging. Although no baseline differences in neural control were evident, performance of a motor and cognitive task revealed prominent differences in neural correlates of autonomic control between subjects with MDD and healthy controls. This study revealed differences in neural correlates of autonomic control, particularly in the MOFC and dmSFG which may deepen our understanding of autonomic dysfunction in mood disorders. Future studies along the same lines may provide crucial advances toward elucidating the pathophysiology of MDD.
Supplementary Material
Abbreviations/Glossary
- MDD
Major Depressive Disorder
- HRV
Heart Rate Variability
- PFC
Prefrontal Cortex
- OFC
Orbitofrontal Cortex
- MOFC
Medial OFC
- LOFC
Lateral OFC
- FPC
Frontal Polar Cortex
- dmSFG
Dorsomedial Superior Frontal Gyrus
- HR
Heart rate
- lnHF
Natural log of high frequency power of the heart rate spectrum, an indicator of parasympathetic activation
- lnLF
Natural log of low frequency power of the heart rate spectrum, partially dependent on sympathetic tone, but strongly dependent on parasympathetic activity as well
- LF/HF
Ratio of low to high frequency power, generally used as an index of the balance of sympathetic to parasympathetic tone
- RMSSD
Root mean square of successive differences of R-R intervals
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agelink MW, Majewski T, Wurthmann C, Postert T, Linka T, Rotterdam S, Klieser E. Autonomic neurocardiac function in patients with major depression and effects of antidepressive treatment with nefazodone. Journal of Affective Disorders. 2001;62(3):187–198. doi: 10.1016/s0165-0327(99)00202-5. [DOI] [PubMed] [Google Scholar]
- Agelink MW, Boz C, Ullrich H, Andrich J. Relationship between major depression and heart rate variability. Clinical consequences and implications for antidepressive treatment. Psychiatry Research. 2002;113(1–2):139–149. doi: 10.1016/s0165-1781(02)00225-1. [DOI] [PubMed] [Google Scholar]
- Akselrod S, Gordon D, Madwed JB, Snidman NC, Shannon DC, Cohen RJ. Hemodynamic regulation: investigation by spectral analysis. American Journal of Physiology. 1985;249(4 Pt 2):H867–875. doi: 10.1152/ajpheart.1985.249.4.H867. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bigger JT, Fleiss JL, Rolnitzky LM, Steinman RC. The ability of several short-term measures of RR variability to predict mortality after myocardial infarction. Circulation. 1993;88(3):927–934. doi: 10.1161/01.cir.88.3.927. [DOI] [PubMed] [Google Scholar]
- Chambers AS, Allen JJ. Sex differences in cardiac vagal control in a depressed sample: implications for differential cardiovascular mortality. Biol Psychology. 2007;75(1):32–36. doi: 10.1016/j.biopsycho.2006.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo R, Mazzuero G, Soffiantino F, Ardizzoia M, Minuco G. A Comprehensive PC Solution to Heart Rate Variability Analysis. Mental Stress. 1989:475–478. [Google Scholar]
- Critchley HD, Mathias CJ, Josephs O, O'Doherty J, Zanini S, Dewar BK, Cipolotti L, Shallice T, Dolan RJ. Human cingulate cortex and autonomic control: converging neuroimaging and clinical evidence. Brain. 2003;126(Pt 10):2139–2152. doi: 10.1093/brain/awg216. [DOI] [PubMed] [Google Scholar]
- Dando SB, Skinner MR, Jordan D, Ramage AG. Modulation of the vagal bradycardia evoked by the stimulation of upper airway receptors by central 5-HT1 receptors in anaesthetized rabbits. British Journal of Pharmacology. 1998;125(2):409–417. doi: 10.1038/sj.bjp.0702085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davydov DM, Shapiro D, Cook IA, Goldstein I. Baroreflex mechanisms in major depression. Progress in Neuropsychopharmacology and Biological Psychiatry. 2007;31(1):164–177. doi: 10.1016/j.pnpbp.2006.08.015. [DOI] [PubMed] [Google Scholar]
- De Rivencourt M. Cardiovascular and eye activity measures as indices for momentary changes in mental effort during simulated flight. Ergonomics. 2008;51(9):1295–1319. doi: 10.1080/00140130802120267. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Videen TO, Price JL, Preskorn SH, Carmichael ST, Raichle ME. A functional anatomical study of unipolar depression. Journal of Neuroscience. 1992;12(9):3628–3641. doi: 10.1523/JNEUROSCI.12-09-03628.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drevets WC, Price JL, Simpson JR, Jr., Todd RD, Reich T, Vannier M, Raichle ME. Subgenual prefrontal cortex abnormalities in mood disorders. Nature. 1997;386(6627):824–827. doi: 10.1038/386824a0. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Prefrontal cortical-amygdalar metabolism in major depression. Annals of the New York Academy of Science. 1999;877:614–637. doi: 10.1111/j.1749-6632.1999.tb09292.x. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Bogers W, Raichle ME. Functional anatomical correlates of antidepressant drug treatment assessed using PET measures of regional glucose metabolism. European Neuropsychopharmacology. 2002;12(6):527–544. doi: 10.1016/s0924-977x(02)00102-5. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Orbitofrontal cortex function and structure in depression. Annals of the New York Academy of Science. 2007;1121:499–527. doi: 10.1196/annals.1401.029. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Price JL, Furey ML. Brain structural and functional abnormalities in mood disorders: implications for neurocircuitry models of depression. Brain Structure and Function. 2008;213(1–2):93–118. doi: 10.1007/s00429-008-0189-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- du Boisgueheneuc F, Levy R, Volle E, Seassau M, Duffau H, Kinkingnehun S, Samson Y, Zhang S, Dubois B. Functions of the left superior frontal gyrus in humans: a lesion study. Brain. 2006;129(Pt 12):3315–3328. doi: 10.1093/brain/awl244. [DOI] [PubMed] [Google Scholar]
- Electrophysiology T.F.o.t.E.S.o.C.a.t.N.A.S.o.P.a. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93(5):1043–1065. [PubMed] [Google Scholar]
- Fitzgerald PB, Srithiran A, Benitez J, Daskalakis ZZ, Oxley TJ, Kulkarni J, Egan GF. An fMRI study of prefrontal brain activation during multiple tasks in patients with major depressive disorder. Human Brain Mapping. 2008;29(4):490–501. doi: 10.1002/hbm.20414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs low CRH/NE states. Molecular Psychiatry. 2002;7(3):254–275. doi: 10.1038/sj.mp.4001032. [DOI] [PubMed] [Google Scholar]
- Gottlieb SS, Khatta M, Friedmann E, Einbinder L, Katzen S, Baker B, Marshall J, Minshall S, Robinson S, Fisher ML, Potenza M, Sigler B, Baldwin C, Thomas SA. The influence of age, gender, and race on the prevalence of depression in heart failure patients. Journal of the American College of Cardiology. 2004;43(9):1542–1549. doi: 10.1016/j.jacc.2003.10.064. [DOI] [PubMed] [Google Scholar]
- Gray MA, Rylander K, Harrison NA, Wallin BG, Critchley HD. Following one's heart: cardiac rhythms gate central initiation of sympathetic reflexes. J Neurosci. 2009;29(6):1817–1825. doi: 10.1523/JNEUROSCI.3363-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey PO, Fossati P, Pochon JB, Levy R, Lebastard G, Lehericy S, Allilaire JF, Dubois B. Cognitive control and brain resources in major depression: an fMRI study using the n-back task. Neuroimage. 2005;26(3):860–869. doi: 10.1016/j.neuroimage.2005.02.048. [DOI] [PubMed] [Google Scholar]
- Hasler G, Fromm S, Carlson PJ, Luckenbaugh DA, Waldeck T, Geraci M, Roiser JP, Neumeister A, Meyers N, Charney DS, Drevets WC. Neural response to catecholamine depletion in unmedicated subjects with major depressive disorder in remission and healthy subjects. Archives of General Psychiatry. 2008;65(5):521–531. doi: 10.1001/archpsyc.65.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildreth CM, Padley JR, Pilowsky PM, Goodchild AK. Impaired serotonergic regulation of heart rate may underlie reduced baroreflex sensitivity in an animal model of depression. American Journal of Physiology: Heart and Circulatory Physiology. 2008;294(1):H474–480. doi: 10.1152/ajpheart.01009.2007. [DOI] [PubMed] [Google Scholar]
- Honer WG, Falkai P, Chen C, Arango V, Mann JJ, Dwork AJ. Synaptic and plasticity-associated proteins in anterior frontal cortex in severe mental illness. Neuroscience. 1999;91(4):1247–1255. doi: 10.1016/s0306-4522(98)00679-4. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey. I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorders. 1993;29(2–3):85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Lane RD, McRae K, Reiman EM, Chen K, Ahern GL, Thayer JF. Neural correlates of heart rate variability during emotion. Neuroimage. 2009;44(1):213–222. doi: 10.1016/j.neuroimage.2008.07.056. [DOI] [PubMed] [Google Scholar]
- Malliani A, Lombardi F, Pagani M, Cerutti S. Clinical exploration of the autonomic nervous system by means of electrocardiography. Annals of the New York Academy of Science. 1990;601:234–246. doi: 10.1111/j.1749-6632.1990.tb37304.x. [DOI] [PubMed] [Google Scholar]
- Malliani A, Pagani M. Spectral analysis of cardiovascular variabilities in the assessment of sympathetic cardiac regulation in heart failure. Pharmacology Research. 1991;24(Suppl 1):43–53. doi: 10.1016/1043-6618(91)90120-m. [DOI] [PubMed] [Google Scholar]
- Malliani A, Pagani M, Lombardi F. Physiology and clinical implications of variability of cardiovascular parameters with focus on heart rate and blood pressure. American Journal of Cardiology. 1994;73(10):3C–9C. doi: 10.1016/0002-9149(94)90617-3. [DOI] [PubMed] [Google Scholar]
- Matsuo K, Glahn DC, Peluso MA, Hatch JP, Monkul ES, Najt P, Sanches M, Zamarripa F, Li J, Lancaster JL, Fox PT, Gao JH, Soares JC. Prefrontal hyperactivation during working memory task in untreated individuals with major depressive disorder. Molecular Psychiatry. 2007;12(2):158–166. doi: 10.1038/sj.mp.4001894. [DOI] [PubMed] [Google Scholar]
- Matthews SC, Nelesen RA, Dimsdale JE. Depressive symptoms are associated with increased systemic vascular resistance to stress. Psychosomatic Medicine. 2005;67(4):509–513. doi: 10.1097/01.psy.0000160467.78373.d8. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Nagai Y, Critchley HD, Featherstone E, Trimble MR, Dolan RJ. Activity in ventromedial prefrontal cortex covaries with sympathetic skin conductance level: a physiological account of a “default mode” of brain function. Neuroimage. 2004;22(1):243–251. doi: 10.1016/j.neuroimage.2004.01.019. [DOI] [PubMed] [Google Scholar]
- Napadow V, Dhond R, Conti G, Makris N, Brown EN, Barbieri R. Brain correlates of autonomic modulation: combining heart rate variability with fMRI. Neuroimage. 2008;42(1):169–177. doi: 10.1016/j.neuroimage.2008.04.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumeister A, Hu XZ, Luckenbaugh DA, Schwarz M, Nugent AC, Bonne O, Herscovitch P, Goldman D, Drevets WC, Charney DS. Differential effects of 5-HTTLPR genotypes on the behavioral and neural responses to tryptophan depletion in patients with major depression and controls. Archives of General Psychiatry. 2006;63(9):978–986. doi: 10.1001/archpsyc.63.9.978. [DOI] [PubMed] [Google Scholar]
- Nugent AC, Neumeister A, Goldman D, Herscovitch P, Charney DS, Drevets WC. Serotonin transporter genotype and depressive phenotype determination by discriminant analysis of glucose metabolism under acute tryptophan depletion. Neuroimage. 2008;43(4):764–774. doi: 10.1016/j.neuroimage.2008.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ongur D, Price JL. The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cerebral Cortex. 2000;10(3):206–219. doi: 10.1093/cercor/10.3.206. [DOI] [PubMed] [Google Scholar]
- Ongur D, Ferry AT, Price JL. Architectonic subdivision of the human orbital and medial prefrontal cortex. Journal of Comparative Neurology. 2003;460(3):425–449. doi: 10.1002/cne.10609. [DOI] [PubMed] [Google Scholar]
- Petit L, Courtney SM, Ungerleider LG, Haxby JV. Sustained activity in the medial wall during working memory delays. Journal of Neuroscience. 1998;18(22):9429–9437. doi: 10.1523/JNEUROSCI.18-22-09429.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poline JB, Worsley KJ, Evans AC, Friston KJ. Combining spatial extent and peak intensity to test for activations in functional imaging. Neuroimage. 1997;5(2):83–96. doi: 10.1006/nimg.1996.0248. [DOI] [PubMed] [Google Scholar]
- Pomeranz B, Macaulay RJ, Caudill MA, Kutz I, Adam D, Gordon D, Kilborn KM, Barger AC, Shannon DC, Cohen RJ, et al. Assessment of autonomic function in humans by heart rate spectral analysis. American Journal of Physiology. 1985;248(1 Pt 2):H151–153. doi: 10.1152/ajpheart.1985.248.1.H151. [DOI] [PubMed] [Google Scholar]
- Price JL. Prefrontal cortical networks related to visceral function and mood. Annals of the New York Academy of Science. 1999;877:383–396. doi: 10.1111/j.1749-6632.1999.tb09278.x. [DOI] [PubMed] [Google Scholar]
- Rose EJ, Simonotto E, Ebmeier KP. Limbic over-activity in depression during preserved performance on the n-back task. Neuroimage. 2006;29(1):203–215. doi: 10.1016/j.neuroimage.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Ruhland C, Koschke M, Greiner W, Peupelmann J, Pietsch U, Hocke M, Yeragani VK, Bar KJ. Gastric dysmotility in patients with major depression. Journal of Affective Disorders. 2008;110(1–2):185–190. doi: 10.1016/j.jad.2007.12.236. [DOI] [PubMed] [Google Scholar]
- Sato N, Miyake S. Cardiovascular reactivity to mental stress: relationship with menstrual cycle and gender. Journal of Physiological Anthropology and Applied Human Science. 2004;23(6):215–223. doi: 10.2114/jpa.23.215. [DOI] [PubMed] [Google Scholar]
- Shinba T, Kariya N, Matsui Y, Ozawa N, Matsuda Y, Yamamoto K. Decrease in heart rate variability response to task is related to anxiety and depressiveness in normal subjects. Psychiatry and Clinical Neurosciences. 2008;62(5):603–609. doi: 10.1111/j.1440-1819.2008.01855.x. [DOI] [PubMed] [Google Scholar]
- Skinner MR, Ramage AG, Jordan D. Modulation of reflexly evoked vagal bradycardias by central 5-HT1A receptors in anaesthetized rabbits. British Journal of Pharmacology. 2002;137(6):861–873. doi: 10.1038/sj.bjp.0704941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ter Horst GJ, Hautvast RW, De Jongste MJ, Korf J. Neuroanatomy of cardiac activity-regulating circuitry: a transneuronal retrograde viral labelling study in the rat. European Journal of Neuroscience. 1996;8(10):2029–2041. doi: 10.1111/j.1460-9568.1996.tb00723.x. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Smith M, Rossy LA, Sollers JJ, Friedman BH. Heart period variability and depressive symptoms: gender differences. Biological Psychiatry. 1998;44(4):304–306. doi: 10.1016/s0006-3223(98)00008-0. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Sollers JJ, 3rd, Ruiz-Padial E, Vila J. Estimating respiratory frequency from autoregressive spectral analysis of heart period. IEEE Engineering in Medicine and Biology Magazine. 2002;21(4):41–45. doi: 10.1109/memb.2002.1032638. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Hansen AL, Johnsen BH. Non-invasive assessment of autonomic influences on the heart: Impedance cardiography and heart rate variablility. In: Luecken LJ, Gallo LC, editors. Handbook of Physiological Research Methods in Health Psychology. Sage Publications; Newbury Park, CA: In Press. [Google Scholar]
- Udupa K, Sathyaprabha TN, Thirthalli J, Kishore KR, Raju TR, Gangadhar BN. Modulation of cardiac autonomic functions in patients with major depression treated with repetitive transcranial magnetic stimulation. Journal of Affective Disorders. 2007;104(1–3):231–236. doi: 10.1016/j.jad.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Vaccarino V, Lampert R, Bremner JD, Lee F, Su S, Maisano C, Murrah NV, Jones L, Jawed F, Afzal N, Ashraf A, Goldberg J. Depressive symptoms and heart rate variability: evidence for a shared genetic substrate in a study of twins. Psychosomatic Medicine. 2008;70(6):628–636. doi: 10.1097/PSY.0b013e31817bcc9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh ND, Williams SC, Brammer MJ, Bullmore ET, Kim J, Suckling J, Mitterschiffthaler MT, Cleare AJ, Pich EM, Mehta MA, Fu CH. A longitudinal functional magnetic resonance imaging study of verbal working memory in depression after antidepressant therapy. Biological Psychiatry. 2007;62(11):1236–1243. doi: 10.1016/j.biopsych.2006.12.022. [DOI] [PubMed] [Google Scholar]
- Westerhaus MJ, Loewy AD. Central representation of the sympathetic nervous system in the cerebral cortex. Brain Research. 2001;903(1–2):117–127. doi: 10.1016/s0006-8993(01)02453-2. [DOI] [PubMed] [Google Scholar]
- Wiklund I, Herlitz J, Johansson S, Bengtson A, Karlson BW, Persson NG. Subjective symptoms and well-being differ in women and men after myocardial infarction. European Heart Journal. 1993;14(10):1315–1319. doi: 10.1093/eurheartj/14.10.1315. [DOI] [PubMed] [Google Scholar]
- Worsley KJ, Marrett S, Neelin P, Vandal AC, Friston KJ, Evans AC. A Unified Statistical Approach for Determining Significant Signals in Cerebral Activation. Human Brain Mapping. 1996;4(1):58–73. doi: 10.1002/(SICI)1097-0193(1996)4:1<58::AID-HBM4>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Yildiz M, Ider YZ. Model based and experimental investigation of respiratory effect on the HRV power spectrum. Physiological Measurement. 2006;27(10):973–988. doi: 10.1088/0967-3334/27/10/004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.