Abstract
Hypertension has been identified as a risk factor for aortic valve calcium (AVC) but the magnitude of the risk relation with hypertension severity or whether age affects the strength of this risk association has not been studied. The relationship of hypertension severity, as defined by JNC-7 hypertension stages or blood pressure (BP), to CT-assessed AVC prevalence and severity was examined in 4,274 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) without treated hypertension. Analyses were stratified by age < or ≥ 65 years, were adjusted for common cardiovascular risk factors, and excluded those on antihypertensive medications. In age-stratified, adjusted analyses, Stage I/II hypertension was associated with prevalent AVC in those <65 but not in those ≥65 years of age [OR (95% CI): 2.31 (1.35, 3.94) vs. 1.33 (0.96, 1.85), P-interaction = 0.041]. Similarly, systolic BP and pulse pressure (PP) were more strongly associated with prevalent AVC in those <65 than those ≥65 years of age [OR (95% CI): 1.21 (1.08, 1.35) vs. 1.07 (1.01, 1.14) per 10 mmHg increase in systolic BP, Pinteraction = 0.006] and [OR (95% CI): 1.41 (1.21, 1.64) vs. 1.14 (1.05, 1.23) per 10 mmHg increase in PP]. No associations were found between either hypertension stage or BP and AVC severity. In conclusion, stage I/II hypertension, as well as higher systolic pressure and pulse pressure were associated with prevalent AVC. These risk associations were strongest in participants younger than age 65 years.
Keywords: Blood Pressure, Aortic Valve, Calcification
Introduction
Previous studies evaluating the association of hypertension with aortic valve disease have used various definitions of hypertension, and mostly have dichotomized hypertension as present or absent in adjusted risk models, rather than examining blood pressure (BP) as a continuous risk variable.1 Also, none have examined the association of aortic valve calcium (AVC) with various stages of hypertension as defined by Joint National Committee (JNC-7) guidelines.2 Furthermore, most studies evaluating this relation have used echocardiography to assess AVC. Recently, computed tomography (CT) has been established as a highly reproducible method for quantifying AVC.3,4 The severity of AVC has been shown to be an independent predictor of worse clinical outcomes.5,6 We hypothesized that BP components and hypertension stages are independent predictors of the presence and severity of AVC, as assessed using baseline CT scans from patients enrolled in the Multi-Ethnic Study of Atherosclerosis. Additionally we investigated if age modified these associations, similar to previously observed attenuation of risk for AVC with dyslipidemia in advancing age.7
Methods
MESA is a prospective cohort study designed to investigate the prevalence and progression of subclinical cardiovascular disease in a population-based sample. Details of the study design have been published elsewhere.8 There were 6,814 participants in MESA ages 45–84 from four ethnic groups, White, African American, Hispanic, and Chinese. Recruitment took place from July 2000 to August 2002 at six US field centers (Baltimore City and Baltimore County, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; New York, New York; and St. Paul, Minnesota). All participants were free of known cardiovascular disease at the time of enrollment. The institutional review boards at all participating institutions approved the study, and all participants provided informed consent.
Baseline information, including demographic variables, socioeconomic status, medical history, and medications were collected using questionnaires. During the initial examination, height and weight, as well as waist and hip circumferences were measured. A resting BP was measured three times in the seated position using a Dinamap model Pro 100 automated oscilometric sphygmomanometer. The last 2 measurements were averaged and used for these analyses.
Chest CT was performed on all participants twice during the initial examination. Images were generated with either cardiac-gated electron beam CT scanner (Imatron C-150; GE Medical Systems, Milwaukee, Wisconsin) or electrocardiogram-triggered four-detector row CT scanners. Details of scanning methodology and quality control,9 as well as reproducibility3 and the effect of scanner type,10 in MESA have been reported previously. AVC was defined as any calcified lesion within the aortic valve leaflets, excluding lesions involving the aortic and mitral annulus, sinuses, and wall of the ascending aorta.3,4,11 AVC quantification of lesions was determined using the method of Agaston et al.12 A total AVC score was calculated for each participant from the summation of all individual lesions. Absence of AVC was assigned a score of zero. All studies were evaluated retrospectively at the MESA CT reading center (Harbor-UCLA Research and Education Institute) by a single blinded reader (JT).
Comparisons between BP categories, based on JNC-7 criteria with demographic measures and cardiovascular risk factors are expressed using means and proportions. AVC scores first were categorized as present (AVC> 0) or absent (AVC=0). We used a 2-stage regression approach for analysis. Because the prevalence of calcification is less than 10% we use odd ratios (OR) from a logistic regression model to estimate relative risks (RR). Using this method we examined the prevalence of AVC > 0 (i.e. the proportion with scores > 0) in unadjusted and adjusted models with both BP stage categories, based on JNC-7 criteria, and continuous measures of systolic, diastolic, and pulse pressure. Among those with detectable calcium (ie in participants with strictly AVC > 0) we used the AVC score as a continuous variable in a multivariable linear regression to assess associations of AVC severity with BP. Given the skewed nature of the AVC distribution, natural log transformation of AVC was modeled. Models for logistic and linear regressions were adjusted for age, gender, race, body-mass index (BMI), smoking, diabetes, low-density lipoprotein (LDL) concentration, high-density lipoprotein (HDL) concentration, and use of lipid lowering medications.
Age interactions were tested in the adjusted regression analyses and considered significant at p < 0.05. Age was stratified as older or younger than 65 years to compare to previous elderly cohort analysis.13 Because there were a small number of younger participants with advanced hypertension, Stages I and II were combined for these analyses. If interactions were significant we presented the stratified results.
We excluded participants with treated hypertension (n=2,533), as done in previous blood pressure studies in MESA,14 because the effect of blood pressure medication on AVC and the amount of misclassification as a result of treatment on blood pressure is unknown. A sensitivity analysis including treated hypertension patients in the analysis was conducted but did not change inferences. All statistical analysis were performed with SPSS 16.0.1 software for Windows (SPSS Inc, Chicago, Illinois) and S-Plus (release 8.0, Insightful Inc, Seattle, WA)
Results
There were 4,275 participants without treated hypertension in this analysis, 2,783 were <65 years old. Differences were present in AVC risk factors between those with and without hypertension (Table 1). Hypertensive participants were more often older, diabetic, had a higher BMI, and more likely to be African-American. Overall, 407 participants had AVC, for a prevalence of 9.5% in this cohort. This AVC prevalence is lower than in previous reports from the MESA cohort,7,15 due to the exclusion of participants with treated hypertension who had a prevalence of AVC of 20%.
Table 1.
Participant Characteristics by Joint National Committee (JNC)-7 Stage of Hypertension.*
| Variable | Normal (n=2206) |
Pre-HTN (n=1304) |
Stage I (n=566) |
Stage II (n=199) |
|---|---|---|---|---|
| AVC Prevalence | 139 (6%) | 144 (11%) | 93 (17%) | 31 (16%) |
| AVC Score† | 45 [17,144] | 54 [18,115] | 73 [15,209] | 69 [17,246] |
| Age (years) | 57 (9) | 62 (10) | 65 (10) | 68 (9) |
| Female | 1215 (55%) | 600 (46%) | 279 (49%) | 118 (59%) |
| White | 960 (44%) | 515 (40%) | 215 (38%) | 63 (32%) |
| Chinese | 325 (15%) | 153 (12%) | 71 (13%) | 23 (12%) |
| Black | 402 (18%) | 320 (25%) | 148 (26%) | 70 (35%) |
| Hispanic | 519 (24%) | 316 (24%) | 131 (23%) | 43 (22%) |
| Ever Smoked | 1079 (49%) | 662 (51%) | 297 (53%) | 98 (50%) |
| Body Mass Index (kg/m2) | 26.8 (5.0) | 28.4 (5.1) | 28.0 (5.3) | 29.2 (6.0) |
| Waist Circumference (cm) | 93 (14) | 99 (13) | 98 (14) | 101 (15) |
| Diabetes mellitus | 140 (6%) | 124 (10%) | 69 (12%) | 26 (13%) |
| Glucose (mg/dL) | 98 (26) | 104 (33) | 104 (28) | 106 (27) |
| Low-density lipoprotein (mg/dL) | 119 (32) | 121 (31) | 121 (30) | 123 (32) |
| High-density lipoprotein (mg/dL) | 52 (15) | 51 (15) | 52 (15) | 52 (15) |
| Triglycerides† (mg/dL) | 103 [72, 148] | 115 [77, 165] | 119 [82, 168] | 116 [85, 165] |
| Lipid Lowering Meds | 206 (9%) | 141 (11%) | 70 (12%) | 18 (9%) |
Data are presented as mean(SD) for continuous variables, number(%) for categorical variables
JNC-7 categories: Normal (SBP < 120mmHg and DBP < 80mmHg), Pre-HTN (SBP 120–139 mmHg or DBP 80–89mmHg), Stage I (SBP 140–159mmHg or DBP 90–99mmHg), Stage II (SBP ≥160 mmHg or DBP ≥ 100mmHg)
Median [IQR]
Abbreviations: AVC, aortic valve calcium; DBP, diastolic blood pressure; HTN, hypertension; SBP, systolic blood pressure.
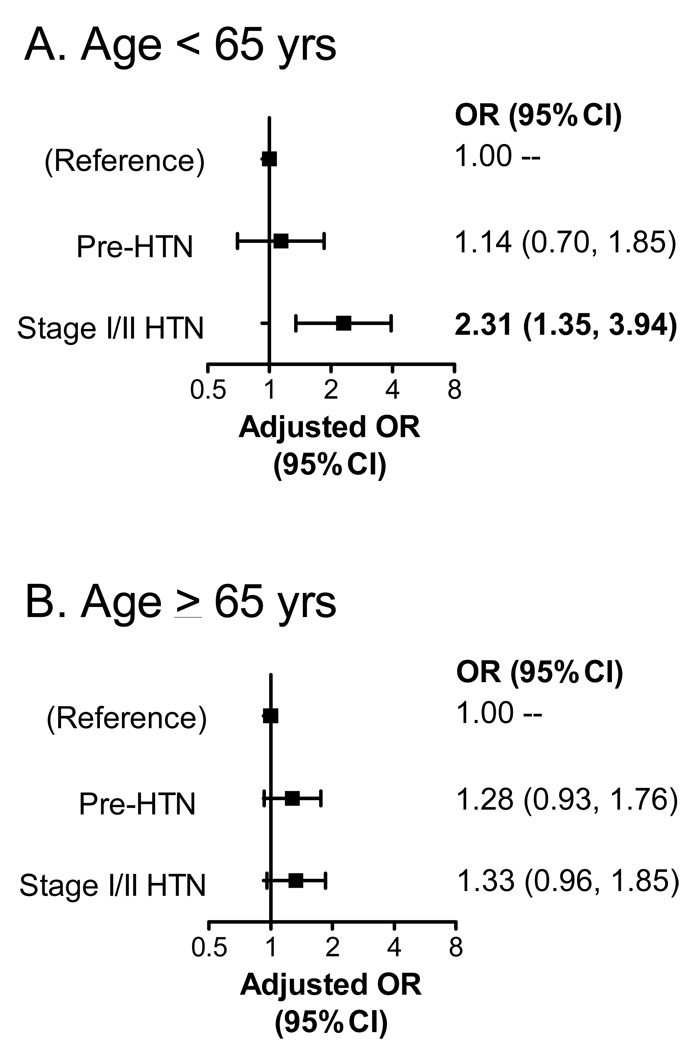
The adjusted OR for stage I or II hypertension was 1.27 (95% CI: 0.96–1.69). In multivariable analyses, there was a significant interaction between age and hypertension stage (P-interaction = 0.041). Stages I or II hypertension were more strongly associated with prevalent AVC in participants < age 65 years (Fig. 1A), than in those ≥ age 65 years (Fig. 1B). JNC-7-defined prehypertension was not significantly associated with an increased OR for prevalent AVC in either age stratum.
Figure 1. Association of JNC-7 Hypertension Stages with Prevalent AVC.
Shown are the adjusted odds ratios (ORs) and 95% confidence intervals for AVC by hypertension stage in those age < 65 years (Fig. 1A) and ≥ 65 years (Fig. 1B), adjusted for gender, race, BMI, smoking, DM, LDL, HDL, and lipid lowering meds.
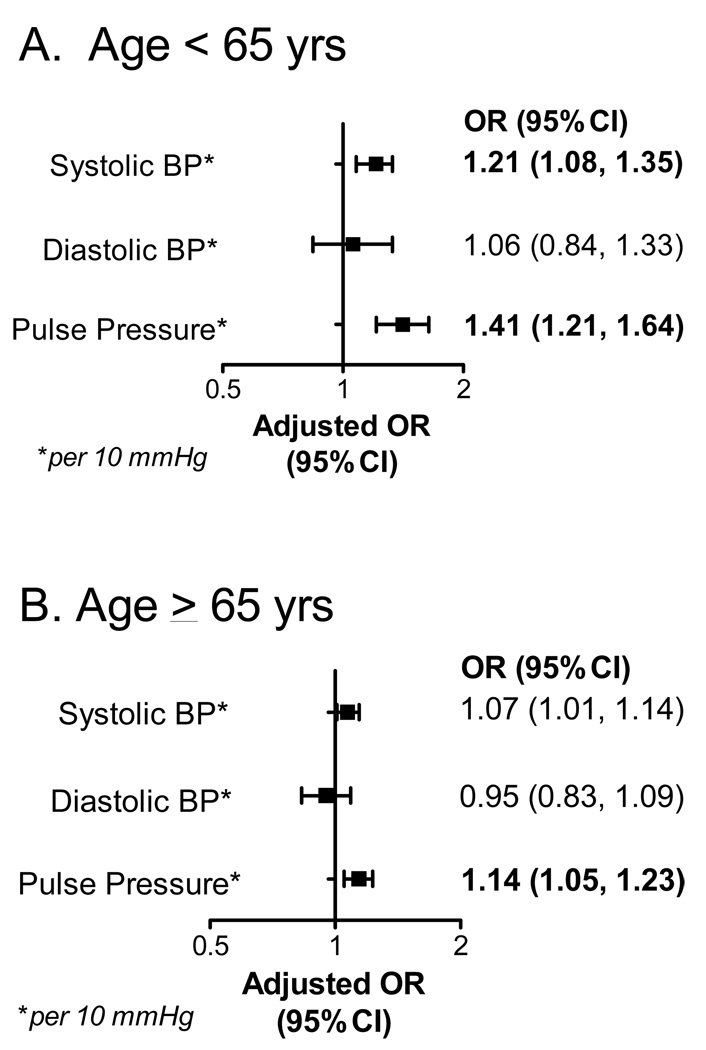
We found similar significant age interactions with continuous measures of blood pressure (P-interaction = 0.006). Though the adjusted ORs for prevalent AVC in systolic blood pressure (per 10 mmHg increase) were increased significantly both for participants age < 65 years (Fig. 2A) and for participants ≥ 65 yrs (Fig. 2B), the association was significantly greater in those <age 65. There was no association of prevalent AVC with diastolic blood pressure (Figs. 2A and B). Of the blood pressure variables, pulse pressure had the strongest association with prevalent AVC (Figs. 2A and B).
Figure 2. Association of Blood Pressure with Prevalent AVC.
Shown are the odds ratios (ORs) and 95% confidence intervals for AVC, , per 10 mmHg increment, in those age < 65 years (Fig. 2A) and ≥ 65 years (Fig. 2B), adjusted for gender, race, BMI, smoking, DM, LDL, HDL, and lipid lowering meds.
There were no statistically significant associations or age interactions of either JNC-7-defined hypertension stages (Table 2) or blood pressure (Table 3) with AVC severity.
Table 2.
Association of Aortic Valve Calcium Severity and Joint National Committee-7 Stage in Participants without Treated Hypertension.
| AVC>0 (N) | Unadjusted Exp(β)† (95% CI) |
Adjusted* Exp(β)† (95% CI) |
|
|---|---|---|---|
| Normal | 133 | 1.00 (ref) | 1.00 (ref) |
| Pre-HTN | 144 | 1.07 (0.75, 1.52) | 0.91 (0.65, 1.29) |
| Stage I & II | 125 | 1.33 (0.92, 1.92) | 1.18 (0.82, 1.70) |
adjusted for gender, race, body mass index, smoking, diabetes mellitus, low-density lipoprotein, high-density lipoprotein, and lipid lowering meds
Exp(β) = relative difference in geometric mean AVC score per higher HTN level.
Abbreviations: AVC, aortic valve calcium; HTN, hypertension.
Table 3.
Association of Aortic Valve Calcium Severity and Continuous Systolic and Diastolic Blood Pressure in Participants without Treated Hypertension.
| Unadjusted Exp(β)† (95% CI) |
Adjusted* Exp(β)† (95% CI) |
|
|---|---|---|
| Systolic BP‡ | 1.07 (1.00, 1.15) | 1.06 (0.99, 1.14) |
| Diastolic BP‡ | 1.07 (0.91, 1.25) | 1.05 (0.89, 1.23) |
|
Pulse pressure‡ (Systolic BP-Diastolic BP) |
1.09 (1.00, 1.19) | 1.09 (0.98, 1.20) |
Adjusted for gender, race, body mass index, smoking, diabetes mellitus, low-density lipoprotein, high-density lipoprotein, and lipid lowering meds
Exp(β) = relative difference in geometric mean AVC score per higher 10mmHg of blood pressure level.
per 10 mmHg increase
Abbreviations: BP, blood pressure.
Discussion
This study confirms that hypertension is associated with AVC as measured by CT, and demonstrates that hypertension severity, defined by either JNC-7 hypertension stage or continuous BP, is associated with increased risk for prevalent AVC. This study also demonstrates an important age interaction, specifically that the association of hypertension with prevalent AVC is greatest in those age <65 years. We did not find any associations with hypertension and severity of AVC.
The finding of an association between hypertension and AVC is consistent with the results of previous studies.13,16–21 Most previous analyses have used only the presence of hypertension in evaluating the associations with AVC as measured by echocardiography. In the reports by Lindroos and Boon, the ORs for AVC in the presence of hypertension, were 1.74 and 2.38 respectively. However, both studies used a more severe definition of hypertension, with a systolic blood pressure >160 mmHg or diastolic >90 mmHg16 or 95 mmHg20. Also in contrast to the present study, in which hypertension was defined by JNC-7 stages, other previous population study cohorts including, the Cardiovascular Health Study (CHS) and the Stroke Prevention: Assessment of Risk in a Community (SPARC) study, defined hypertension by either self report or antihypertensive medication use. In CHS, the reported OR was 1.23 (95% CI: 1.1 – 1.4) and in SPARC the OR was 1.93 (95% CI: 1.12 – 3.32). In addition, none of these prior studies was able to demonstrate an association of BP as a continuous variable with aortic sclerosis. These previous studies did not exclude those with treated hypertension, which may have biased the results of their BP-based analyses.
Other prior studies using CT have assessed potential risk-associations of hypertension with AVC.18,21 However, these studies were comprised of high-risk populations referred for coronary artery calcificium screening. Pohle et al,21 reported a non-significant association of AVC with known or treated hypertension, with an OR of 1.3 (95%: CI 0.8 – 1.9). In a study by Wong et al,18 actual systolic and diastolic BP measurements were studied, though it is unclear whether those with treated hypertension were excluded from their analyses. Their results were similar to those of the present study, with a borderline association of systolic BP with AVC [OR (95% CI) 1.11 (0.997 – 1.23)] and an inverse relationship of diastolic BP with AVC [OR (95% CI) 0.76 (0.62 – 0.92)]. The positive association of systolic BP with AVC, in combination with a negative association of diastolic BP with AVC likely is due to increased arterial stiffness.22,23 Thus, the use of a combination of systolic BP with diastolic BP, i.e., pulse pressure, in adjusted models may result in better classification of hypertension-associated risk for AVC.24
This study extends the results of previous studies by demonstrating that the association of hypertension with AVC is strongest in those less than age 65 years. While hypertension remains an important cardiovascular risk factor in the elderly,25 the effect of hypertension is attenuated in older populations.26 Similarly, the impact of lipoprotein-associated risk on AVC has been shown to be attenuated with age.7 If these findings are confirmed in future prospective studies, then targeting traditional risk factors, specifically dyslipidemia and hypertension, may be most effective in those less than age 65 years.
Though CT assessment of AVC has been validated as a reproducible method for quantifying calcification severity,27 this study found no association of hypertension with AVC severity. Recent studies have found that risk-factors associated with prevalent AVC may not be similarly associated with AVC severity,7,15 raising the possibility that factors governing AVC initiation may differ from those governing AVC progression.
This study has several limitations. First, as it is a secondary analysis and cross-sectional in design, causal inference is not possible. Second, because MESA was a cohort of healthy individuals without known cardiovascular disease, the overall prevalence of AVC was low, limiting power to detect associations in smaller subgroups, such as those with more advanced hypertension. This also may have limited the ability to detect associations for AVC severity with higher BP. We are also unable to measure the healthy cohort effect on age interactions in MESA. Similarly, observed interactions may in part be a result of excluding treated hypertension individuals, who are likely to be older. Finally, given the observational nature of the data, residual confounding may be present.
Acknowledgments
Funding: This research was supported by contracts N01-HC-95159 through N01-HC-95169 from the National Heart, Lung, and Blood Institute. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rabkin S. The association of hypertension and aortic valve sclerosis. Blood Press. 2005;14:264–272. doi: 10.1080/08037050500233320. [DOI] [PubMed] [Google Scholar]
- 2.Chobanian A, Bakris G, Black H, Cushman W, Green L, Izzo JJ, Jones D, Materson B, Oparil S, Wright JJ, Roccella E. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.Budoff M, Mao S, Takasu J, Shavelle D, Zhao X, O'Brien K. Reproducibility of electron-beam CT measures of aortic valve calcification. Acad Radiol. 2002;9:1122–1127. doi: 10.1016/s1076-6332(03)80513-5. [DOI] [PubMed] [Google Scholar]
- 4.Budoff M, Takasu J, Katz R, Mao S, Shavelle D, O'Brien K, Blumenthal R, Carr J, Kronmal R. Reproducibility of CT measurements of aortic valve calcification, mitral annulus calcification, and aortic wall calcification in the multi-ethnic study of atherosclerosis. Acad Radiol. 2006;13:166–172. doi: 10.1016/j.acra.2005.09.090. [DOI] [PubMed] [Google Scholar]
- 5.Rosenhek R, Binder T, Porenta G, Lang I, Christ G, Schemper M, Maurer G, Baumgartner H. Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med. 2000;343:611–617. doi: 10.1056/NEJM200008313430903. [DOI] [PubMed] [Google Scholar]
- 6.Feuchtner G, Müller S, Grander W, Alber H, Bartel T, Friedrich G, Reinthaler M, Pachinger O, zur Nedden D, Dichtl W. Aortic valve calcification as quantified with multislice computed tomography predicts short-term clinical outcome in patients with asymptomatic aortic stenosis. J Heart Valve Dis. 2006;15:494–498. [PubMed] [Google Scholar]
- 7.Owens D, Katz R, Johnson E, Shavelle D, Probstfield J, Takasu J, Crouse J, Carr J, Kronmal R, Budoff M, O'Brien K. Interaction of age with lipoproteins as predictors of aortic valve calcification in the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168:1200–1207. doi: 10.1001/archinte.168.11.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bild D, Bluemke D, Burke G, Detrano R, Diez Roux A, Folsom A, Greenland P, Jacob DJ, Kronmal R, Liu K, Nelson J, O'Leary D, Saad M, Shea S, Szklo M, Tracy R. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 9.Carr J, Nelson J, Wong N, McNitt-Gray M, Arad Y, Jacobs DJ, Sidney S, Bild D, Williams O, Detrano R. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 10.Budoff M, Katz R, Wong N, Nasir K, Mao S, Takasu J, Kronmal R, Detrano R, Shavelle D, Blumenthal R, O'brien K, Carr J. Effect of scanner type on the reproducibility of extracoronary measures of calcification: the multi-ethnic study of atherosclerosis. Acad Radiol. 2007;14:1043–1049. doi: 10.1016/j.acra.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 11.Shavelle D, Budoff M, Buljubasic N, Wu A, Takasu J, Rosales J, Otto C, Zhao X, O'Brien K. Usefulness of aortic valve calcium scores by electron beam computed tomography as a marker for aortic stenosis. Am J Cardiol. 2003;92:349–353. doi: 10.1016/s0002-9149(03)00646-5. [DOI] [PubMed] [Google Scholar]
- 12.Agatston A, Janowitz W, Hildner F, Zusmer N, Viamonte MJ, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 13.Stewart B, Siscovick D, Lind B, Gardin J, Gottdiener J, Smith V, Kitzman D, Otto C. Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J Am Coll Cardiol. 1997;29:630–634. doi: 10.1016/s0735-1097(96)00563-3. [DOI] [PubMed] [Google Scholar]
- 14.Psaty B, Arnold A, Olson J, Saad M, Shea S, Post W, Burke G. Association between levels of blood pressure and measures of subclinical disease multi-ethnic study of atherosclerosis. Am J Hypertens. 2006;19:1110–1117. doi: 10.1016/j.amjhyper.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 15.Katz R, Wong N, Kronmal R, Takasu J, Shavelle D, Probstfield J, Bertoni A, Budoff M, O'Brien K. Features of the metabolic syndrome and diabetes mellitus as predictors of aortic valve calcification in the Multi-Ethnic Study of Atherosclerosis. Circulation. 2006;113:2113–2119. doi: 10.1161/CIRCULATIONAHA.105.598086. [DOI] [PubMed] [Google Scholar]
- 16.Boon A, Cheriex E, Lodder J, Kessels F. Cardiac valve calcification: characteristics of patients with calcification of the mitral annulus or aortic valve. Heart. 1997;78:472–474. doi: 10.1136/hrt.78.5.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agmon Y, Khandheria B, Meissner I, Sicks J, O'Fallon W, Wiebers D, Whisnant J, Seward J, Tajik A. Aortic valve sclerosis and aortic atherosclerosis: different manifestations of the same disease? Insights from a population-based study. J Am Coll Cardiol. 2001;38:827–834. doi: 10.1016/s0735-1097(01)01422-x. [DOI] [PubMed] [Google Scholar]
- 18.Wong N, Sciammarella M, Arad Y, Miranda-Peats R, Polk D, Hachamovich R, Friedman J, Hayes S, Daniell A, Berman D. Relation of thoracic aortic and aortic valve calcium to coronary artery calcium and risk assessment. Am J Cardiol. 2003;92:951–955. doi: 10.1016/s0002-9149(03)00976-7. [DOI] [PubMed] [Google Scholar]
- 19.Gotoh T, Kuroda T, Yamasawa M, Nishinaga M, Mitsuhashi T, Seino Y, Nagoh N, Kayaba K, Yamada S, Matsuo H. Correlation between lipoprotein(a) and aortic valve sclerosis assessed by echocardiography (the JMS Cardiac Echo and Cohort Study) Am J Cardiol. 1995;76:928–932. doi: 10.1016/s0002-9149(99)80263-x. [DOI] [PubMed] [Google Scholar]
- 20.Lindroos M, Kupari M, Valvanne J, Strandberg T, Heikkilä J, Tilvis R. Factors associated with calcific aortic valve degeneration in the elderly. Eur Heart J. 1994;15:865–870. doi: 10.1093/oxfordjournals.eurheartj.a060602. [DOI] [PubMed] [Google Scholar]
- 21.Pohle K, Otte M, Mäffert R, Ropers D, Schmid M, Daniel W, Achenbach S. Association of cardiovascular risk factors to aortic valve calcification as quantified by electron beam computed tomography. Mayo Clin Proc. 2004;79:1242–1246. doi: 10.4065/79.10.1242. [DOI] [PubMed] [Google Scholar]
- 22.Franklin S, Larson M, Khan S, Wong N, Leip E, Kannel W, Levy D. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 23.Dart A, Kingwell B. Pulse pressure--a review of mechanisms and clinical relevance. J Am Coll Cardiol. 2001;37:975–984. doi: 10.1016/s0735-1097(01)01108-1. [DOI] [PubMed] [Google Scholar]
- 24.Franklin S, Lopez V, Wong N, Mitchell G, Larson M, Vasan R, Levy D. Single versus combined blood pressure components and risk for cardiovascular disease: the Framingham Heart Study. Circulation. 2009;119:243–250. doi: 10.1161/CIRCULATIONAHA.108.797936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beckett N, Peters R, Fletcher A, Staessen J, Liu L, Dumitrascu D, Stoyanovsky V, Antikainen R, Nikitin Y, Anderson C, Belhani A, Forette F, Rajkumar C, Thijs L, Banya W, Bulpitt C. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 26.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 27.Messika-Zeitoun D, Aubry M, Detaint D, Bielak L, Peyser P, Sheedy P, Turner S, Breen J, Scott C, Tajik A, Enriquez-Sarano M. Evaluation and clinical implications of aortic valve calcification measured by electron-beam computed tomography. Circulation. 2004;110:356–362. doi: 10.1161/01.CIR.0000135469.82545.D0. [DOI] [PubMed] [Google Scholar]