Abstract
Background:
Remote coverage of ICUs is increasing, but staff acceptance of this new technology is incompletely characterized. We conducted a systematic review to summarize existing research on acceptance of tele-ICU coverage among ICU staff.
Methods:
We searched for published articles pertaining to critical care telemedicine systems (aka, tele-ICU) between January 1950 and March 2010 using PubMed, Cumulative Index to Nursing and Allied Health Literature, Global Health, Web of Science, and the Cochrane Library and abstracts and presentations delivered at national conferences. Studies were included if they provided original qualitative or quantitative data on staff perceptions of tele-ICU coverage. Studies were imported into content analysis software and coded by tele-ICU configuration, methodology, participants, and findings (eg, positive and negative staff evaluations).
Results:
Review of 3,086 citations yielded 23 eligible studies. Findings were grouped into four categories of staff evaluation: overall acceptance level of tele-ICU coverage (measured in 70% of studies), impact on patient care (measured in 96%), impact on staff (measured in 100%), and organizational impact (measured in 48%). Overall acceptance was high, despite initial ambivalence. Favorable impact on patient care was perceived by > 82% of participants. Staff impact referenced enhanced collaboration, autonomy, and training, although scrutiny, malfunctions, and contradictory advice were cited as potential barriers. Staff perceived the organizational impact to vary. An important limitation of available studies was a lack of rigorous methodology and validated survey instruments in many studies.
Conclusions:
Initial reports suggest high levels of staff acceptance of tele-ICU coverage, but more rigorous methodologic study is required.
Although intensivist care is associated with lower ICU and hospital mortality and with reduced length of stay,1 only one-third of critically ill patients receive intensivist care, and the shortfall is projected to worsen.2 As a result, hospitals increasingly rely on tele-ICU coverage.3 For the purposes of this article, we define tele-ICU coverage as the application of telemedicine4 to in-hospital critical care units, thereby encompassing an array of technologies of varying complexity5,6 that allow physical ICUs to access critical care experts in real time.
At the present time, it is estimated that 10% of US hospitals use some form of tele-ICU coverage, and expansion seems likely.7 Despite rapid adoption, reported effectiveness of tele-ICU coverage has varied across studies,8‐11 and studies often have neglected to address tele-ICU impact on staff. Staff impact is important as evidenced by a report of one hospital system that dropped tele-ICU coverage after 2 years.12 Not only do monitoring and intervention by specialists likely influence the interpersonal dynamics of the ICU staff but also that same staff is responsible for implementing and operating the new system. The objective of the present study was to systematically evaluate the published and unpublished literature addressing acceptance of tele-ICU coverage by ICU staff with a focus on benefits and challenges seen by frontline providers adopting this new technology.
Materials and Methods
Literature Search
Our literature review was conducted in accordance with guidelines for the conduct of systematic reviews.13‐15 Reliance on deidentified published data precluded the need for institutional review board approval. With the assistance of a medical research librarian, we searched for studies evaluating staff acceptance of critical care telemedicine systems published between January 1, 1950, and March 31, 2010, using PubMed, Cumulative Index to Nursing and Allied Health Literature, Global Health, Web of Science, and Cochrane Library. Because terminology for tele-ICU has not been standardized, our search used several terms to describe tele-ICU systems (eg, eICU, remote ICU, virtual ICU) alone and in combination with relevant medical subject heading terms (eg, critical care AND telemedicine). We supplemented this search with a keyword search and review of abstracts presented at relevant major scientific conferences between 2006 and 2009.
Inclusion Criteria
Studies were considered eligible for inclusion if they met each of the following criteria: (1) addressed real-time telemedicine within an ICU, (2) presented original quantitative or qualitative data on the impact of tele-ICU coverage, and (3) assessed staff acceptance of tele-ICU coverage. We defined staff acceptance as any objective or subjective evaluation, recognizing that our broad inclusion criteria would result in studies that included both more- and less-rigorous assessments. Staff included in these studies might include physicians, nurses, and administrators working in either the ICU or the monitoring center. Two authors (P. C. and L. B. Y.) independently reviewed each study, and discrepancies were resolved through discussion.
Data Abstraction and Analysis
Staff acceptance was a primary focus in some studies but of ancillary interest in others. Formal meta-analysis was not possible given the variation in methodology used in individual studies. We therefore relied on a standard content analytic method16,17 that integrated both quantitative and qualitative findings within categories describing tele-ICU impact.18,19
After importing the studies into NVivo 8 content analysis software (QSR International, Pty, Ltd; Doncaster, Victoria, Australia),20 one of the investigators with formal training in content analysis (L. B. Y.) abstracted data on the tele-ICU configuration investigated, including type of technology involved (bedside monitors for each patient, a single mobile camera, or a remote-controlled robot), coverage level (scheduled telerounds, on-call consultation, or ongoing monitoring and consultation), and tele-ICU structure. Structure was coded as hub and spoke (single monitoring center covering multiple ICUs), parent-child (one hospital extending existing intensivist coverage remotely to another), or collaborative/network (mobile intensivists offering services from home, hospital, or any other location). Also coded were study method (quantitative survey, qualitative survey, interview, or case study), participants (physician, nurse, administrator, or unidentified staff), and findings.
Analysis of study findings were guided by our research question: How do staff members view tele-ICU coverage? We began by open coding17 the quantitative studies and then applying those codes to the qualitative data, which fit them well. Participants introduced few issues or processes unaddressed in researcher-defined surveys. One code represented overall acceptance (eg, satisfaction), and three codes represented staff evaluations of tele-ICU impact on quality of patient care, on staff, and on the organization.
Results
Description of Studies
Study Selection:
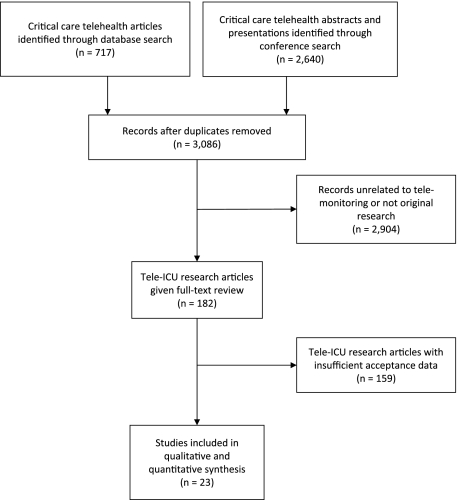
We identified 3,086 studies that focused on critical care telemedicine and subsequently excluded 2,904 studies that did not focus on tele-ICU coverage or that contained no original data (Fig 1). The remaining 182 studies were given full review, and 23 met the inclusion criteria.5,21‐42 When data from a single tele-ICU was reported in multiple articles or abstracts, the article with the most comprehensive results was used.43‐50 Table 1 summarizes the included studies; 10 (43%) were unpublished abstracts. Staff acceptance was the primary focus of 10 studies,23,26,29,30,34,36‐38,40,41 whereas it was a secondary focus of the remaining 13.5,21,22,24,25,27,28,31‐33,35,39,42
Figure 1.
Tele-ICU acceptance literature search flow diagram.
Table 1.
—Design of Studies Evaluating Staff Acceptance of TICU Coverage
| Study/Year | Publication Status | Study Method | Participants | Evaluation Point | Summary of Findings |
| Berenson et al5/2009 | Published | Interview | Administrators (n = 453 pre and 58+ post) | Pre/Post | • Pre: Perception that substantial costs are not justified by potential benefit, that current staffing was adequate, and that onsite was preferable to off-site staff. |
| • Post: Broad perception that TICU improves quality and safety, but no objective data support those beliefs. Frustration with IT interface problems. | |||||
| Coletti et al30/2008 | Published | Quantitative survey | Medical ICU residents (n = 35) | Post | • 77% reported improved patient safety. |
| • 63% reported improved ability to focus on urgent patient issues. | |||||
| • 51% reported increase in uninterrupted periods of rest. | |||||
| • 37% reported that TICU held educational value. | |||||
| Crawley31/2008 | Meeting abstract | Case study | Staff (n = NR) | Post | • Reports of enhanced training of physician staff, high system reliability, and enhanced Army-Navy cooperation. |
| • Perceived workload increase, big-brother concerns, lack of need, failure to recognize when help is needed, and IT interface/security challenges. | |||||
| DiMartino et al29/2009 | Meeting abstract | Quantitative survey | Nurses (n = 91) | Post | • 72% believed that TICU increases patient survival. |
| • 47% believed that TICU prevents errors. | |||||
| • 42% believed that TICU improves family satisfaction. | |||||
| • 13% felt “spied upon.” | |||||
| • 11% believed that TICU was intrusive. | |||||
| • 9% believed that TICU interrupted workflow. | |||||
| • 79% believed that knowing the telephysician was important, and 61% were more likely to contact the consultant if they knew the physician on call. | |||||
| Faiz et al32/2006 | Meeting abstract | Quantitative survey | Telephysicians (n = 16) | Post | • Of 16 fellows rotating through the eICU remote site, 14 of 16 would want to work in a place with TICU, and 13 of 16 believed that it protected against liability. |
| • All believed that TICU improved patient care. | |||||
| Grundy et al28/1977 | Published | Quantitative and qualitative survey | Physicians and nurses (n = NR) | Post | • 88% of nurses believed that TICU benefited patients, and 70% believed that it enhanced education. |
| • Nurses reported positive attitudes toward TICU on 40 occasions and negative attitudes on 21. | |||||
| • Over time, resistance was replaced by enthusiasm. | |||||
| • Physicians reported positive attitudes toward TICU on 17 occasions and negative attitudes on 4. | |||||
| • Although acceptance increased over time, physicians implemented only 46% of consultant suggestions in the last 84 d of the program. Some physicians resented the consultant. | |||||
| Heath et al33/2009 | Published | Quantitative survey | Physicians (n = 41consultations), Teleintensivists (n = 63 consultations) | Post | • Unit of analysis was the consultation. |
| • In 88% of pediatric consultations to rural EDs, the physician agreed that consultation improved care. | |||||
| • In 89% of consultations, the consulting intensivist agreed that the consultation improved care. | |||||
| Kowitlawakul34/2008 | Published | Quantitative and qualitative survey | Nurses (n = 117 quantitative and n = 34 qualitative) | Pre | • On a five-point Likert scale, the item mean was 3.3 on the 21-item Nurse Attitudes Toward eICU survey. |
| • The item mean was 3.2 on the six-item Intention to Use scale. | |||||
| • Nurses believed that TICU would benefit units without adequate physician coverage and might benefit new nurses. | |||||
| • Nurses believed that it was unnecessary in some units, that conflicts between on- and off-site staff could undermine patient outcomes, and that it could lead to extra work and staff cuts. | |||||
| Marcin et al35/2004 | Published | Quantitative survey | Physicians (n = 53), nurses, respiratory therapists (n = 17) | Post | • On a five-point Likert scale, overall satisfaction averaged 4.56 for referring physicians and 4.53 for nurses and respiratory therapists. |
| • Among aspects of TICU consultations, the physicians scored audiovisual quality lowest (mean, 4.31), and the nurses and respiratory therapists scored ease of equipment use lowest (mean, 3.59). | |||||
| Marttos et al27/2008 | Meeting abstract | Quantitative survey | Clinicians (physicians and nurses, n = 71 combined), both bedside and telepresence | Post | • Results were very positive on the basis of means of a five-point Likert scale: overall experience, 4.29; user satisfaction, 4.22; technical issues, 4.31; and clinical application, 4.17. |
| • No significant variation over time suggested positive attitudes toward TICU from first use. | |||||
| Mathews et al36/2007 | Published | Case study | Nurses (n = NR) | Pre/Post | • Prior to implementation, nurses were apprehensive and resistant, fearing repercussions from constant monitoring, increased workload, and increased nurse to patient ratios. |
| • A work team was able to decrease apprehension and increase acceptance of TICU staff. | |||||
| McNelis et al26/2008 | Meeting abstract | Quantitative survey | Physicians (n = NR) | Post | • Staff intensivists communicated with surgical ICU staff during off hours through robot or telephone. |
| • Satisfaction with the robot (mean, 6.5) was significantly greater than satisfaction with the telephone (mean, 4.5). | |||||
| Mora et al37/2007 | Meeting abstract | Quantitative survey | Residents (n = 96) | Post | • Of the residents with TICU experience, 82.3% believed that it improves patient care, and 73.8% believed that it improves the care they deliver to patients; 66.7% desired telemonitoring postresidency. |
| • Of events potentially benefiting from telemonitoring, ventilator management was mentioned by the most (70%), and supervision of online placement was mentioned the least (42%). | |||||
| Poropatich et al25,45,46/2008 | Meeting abstract | Quantitative survey | Physicians (n = 8), residents (n = 22), nurses (n = 45) | Post | • On a 10-point scale, overall satisfaction averaged 8.5 for physicians, 8.1 for residents, and 8.3 for nurses. |
| • A majority of physicians and residents believed that the robot saved time. | |||||
| • Measured collectively, no clinicians believed that the telephone was better than the robot or that the video or audio quality was poor. | |||||
| • 95% believed that remote telepresence improves care. There was high satisfaction with no difference in support between types of providers. | |||||
| Roberts and Dewoody38/2008 | Published | Quantitative survey | Nurses (n = NR) | Pre/Post | • The development of an orientation program for eICU care staff was associated with increased staff satisfaction with eICU and increased number of assistance calls and interactions with teleclinicians. |
| Rogove et al39/2009 | Meeting abstract | Quantitative survey | Physicians (n = NR) | Post | • Physician satisfaction by survey was excellent. |
| Siek et al24/2008 | Meeting abstract | Case study | Physicians, nurses (n = NR) | Post | • Pulmonary and critical care physicians appreciated consultations with colleagues, but the cardiovascular surgeon would not use the eICU resource. |
| • Nurses believed that the system was great and provided resources for the night shift, but they noted manipulation of physicians. | |||||
| Stafford et al40/2008 | Published | Interview | Telephysicians (n = 26), telenurses (n = 44) | Post | • Physical stress and boredom were challenges, but the telecenter fosters teamwork with a focus on improved patient care. |
| • Telestaff can become frustrated by the inability to directly intervene and by the resistance encountered from ICU staff. | |||||
| • Calls from ICU nurses increase when (they learn) consulting physicians are on duty. | |||||
| Sucher et al23/2009 | Meeting abstract | Quantitative survey | Physicians, nurses (n = NR) | Pre | • 67% agreed that the robot would facilitate patient care between intensivists and bedside clinicians, and 72% agreed that the robot would assist bedside clinicians in managing emergencies. |
| Thomas et al41/2007 | Published | Quantitative survey | Physicians (n = NR) | Pre/Post | • The Safety Attitudes Questionnaire revealed that a significant increase in the mean teamwork score (from 69.7 to 78.8) and safety climate score (from 66.4 to 73.4) after TICU was implemented. |
| • Item scores also revealed a decrease in perceived interruptions, an increase in confidence that patients are adequately covered, and an increase in belief that a physician can be accessed in an emergency. | |||||
| Westbrook et al22,47‐49/2008 | Published | Interviews, quantitative survey | Physicians (n = 6), nurses (n = 12),telephysicians (n = 13) | Post | • Following implementation of a virtual critical care unit in Australia, all consulting physicians reported that they were able to increase decision support to ED clinicians, and this had improved patient management. |
| • Many also noted increased workload and responsibility; 71% were satisfied with TICU design. | |||||
| • ED physicians perceived greater support, and nurses reported increased autonomy and less stress. | |||||
| • 65% of ED clinicians were satisfied with TICU design. | |||||
| • The majority of all respondents reported improved interhospital relationships. | |||||
| Youn42/2006 | Published | Quantitative survey | Nurses (n = NR) | Post | • Nursing satisfaction averaged 4.7 to 5.0 (on a five-point scale) for improved communication and collaboration and better patient outcomes. |
| Zawada et al21,43,50/2009 | Published | Quantitative survey | Physicians, nurse, telephysicians (n = NR) | Post | • Ten of 11 community hospitals responded. |
| • Using a five-point scale, 90% of hospital administrators and lead clinical staff agreed that tele-ICU improved patient care, was easy to use, and should be available to every small or critical access hospital. | |||||
| • More than 90% of telephysicians indicated that the TICU improved critical care in tertiary and community ICUs. | |||||
| • All of them agreed better, safer care can be delivered by a telecritical care team. |
eICU = electronic ICU; IT = information technology; NR = not reported; TICU = tele-ICU.
Tele-ICU Configuration:
There was significant variation in how tele-ICU was defined, used, and structured (Table 2). In 12 studies (52%), tele-ICU involved bedside monitors and cameras,5,24,29‐32,34,36‐38,40,41 whereas the remaining 11 (48%) used mobile cameras or robots.21‐23,25‐28,33,35,39,42 Likewise, 12 (52%) studies described systems using around-the-clock telemonitoring,5,21,24,29,30,32,34,36‐38,40,41 whereas seven (30%) entailed only on-call consultation,22,23,31,33,35,39,42 and four (17%) used a system of regularly scheduled telerounds.25‐28 Thirteen (57%) studies included tele-ICUs structured on a hub-and-spoke model,5,21,24,29,30,32,34,36‐38,40‐42 whereas 10 (43%) evaluated ICUs using parent-child or collaborative/network set-ups.22,23,25‐28,31,33,35,39
Table 2.
—Characteristics of TICUs
| Study/Year | Technology | Coverage | Structure |
| Berenson et al5/2009 | Bedside | Monitoring | Hub and spoke (eICU) |
| Coletti et al30/2008 | Bedside | Monitoring | Hub and spoke (eICU) |
| Crawley31/2008 | Bedside | Consultation | Parent and child (eICU) |
| DiMartino et al29/2009 | Bedside | Monitoring | Hub and spoke |
| Faiz et al32/2006 | Bedside | Monitoring | Hub and spoke (eICU) |
| Grundy et al28/1977 | Single mobile camera | ICU rounds | Parent and child |
| Heath et al33/2009 | Single mobile camera | Consultation | Parent and child |
| Kowitlawakul34/2008 | Bedside | Monitoring | Hub and spoke (eICU) |
| Marcin et al35/2004 | Single mobile camera | Consultation | Parent and child |
| Marttos et al27/2008 | Robot | ICU rounds | Collaborative/network |
| Mathews et al36/2007 | Bedside | Monitoring | Hub and spoke (eICU) |
| McNelis et al26/2008 | Robot | ICU rounds | Collaborative/network |
| Mora et al37/2007 | Bedside | Monitoring | Hub and spoke (eICU) |
| Poropatich et al25,45,46/2008 | Robot | ICU rounds | Collaborative/network |
| Roberts and Dewoody38/2008 | Bedside | Monitoring | Hub and spoke (eICU) |
| Rogove et al39/2009 | Robot | Consultation | Collaborative/network |
| Siek et al24/2008 | Bedside | Monitoring | Hub and spoke (eICU) |
| Stafford et al40/2008 | Bedside | Monitoring | Hub and spoke (eICU) |
| Sucher et al23/2009 | Robot | Consultation | Collaborative/network |
| Thomas et al41/2007 | Bedside | Monitoring | Hub and spoke |
| Westbrook et al22,47‐49/2008 | Single mobile camera | Consultation | Parent and child |
| Youn42/2006 | Robot | Consultation | Hub and spoke |
| Zawada et al21,43,50/2009 | Hybrid | Monitoring | Hub and spoke (eICU) |
See Table 1 legend for expansion of abbreviations.
Study Methodology:
Eighteen studies assessed acceptance using Likert or simple yes/no questions,21‐23,25‐30,32‐35,37‐39,41,42 and two of these included a qualitative component.28,34 Only two (11%) studies used validated survey instruments to assess acceptability.34,41 Among the five (22%) studies relying exclusively on qualitative methods, two reported interview findings,5,40 and three provided summaries of case studies.24,31,36
Participants:
Acceptance was examined among physicians in 16 (70%) studies,21‐28,30,32,33,35,37,39‐41 nurses in 13 (57%),21‐25,27‐29,34,36,38,40,42 and hospital administrators in one (4%).5 Five (22%) studies included data on clinicians providing teleservices.21,27,32,33,40
Findings
Sixteen (70%) studies provided staff members’ overall acceptance of tele-ICU coverage,21,22,24‐29,32‐39 22 (96%) assessed impact on patient care,5,21‐37,39‐42 all assessed impact on staff; and 11 (48%) assessed impact on the organization.5,21‐24,31,32,34,35,40,41 Table 3 summarizes findings in each category and identifies potential implementation barriers mentioned by participants.
Table 3.
—Summary of Acceptance and Potential Barriers Reported by Staff
| Evaluation Category | Summary | Potential Barriers |
| Overall acceptance of staff | • High satisfaction | • Ambivalence among nurses prior to implementation |
| • TICU desired by residents | • Preimplementation questions about usefulness of TICU | |
| Staff evaluation of patient care impact | • Anticipated enhancements to patient care | • Nurse refusal to take good advice from teleclinicians |
| • Positive evaluations of patient care impact | • Poaching of ICU clinicians in order to staff the telecenter | |
| • Better off-shift coverage and reductions in patient transfers | ||
| Staff evaluation of staff impact | • Anticipated fruitful collaboration between ICU and telecenter | • Conflicting recommendations from ICU and teleclinicians |
| • Communication between the ICU and telecenter highly rated | • Suspicion ICU nurses avoided or deferred consultations to receive desired advice from a preferred source | |
| • Better relationships in parent-child setups than in hub-and-spoke setups | • Concerns that big brother was watching and scrutinizing work | |
| • Enhanced autonomy | • Increased workload, particularly when equipment malfunctions | |
| • Enhanced clinical training | • Interruptions | |
| • Reduced workload | ||
| Staff evaluation of organizational impact | • Coverage unnecessary in all ICUs (eg, highly effective ICUs) | • Benefits unjustified by cost to hospital |
| • Needs and resources of the ICU should determine type of telecoverage | • Concerns about legal liability and vulnerability | |
| • TICU benefits underperforming ICUs and those with new nurses or physician gaps | ||
| • Leveraged intensivist services | ||
| • Enhanced hospital reputation |
See Table 1 for expansion of abbreviation.
Overall Acceptance:
Studies assessing overall acceptance generally were favorable. Studies used a variety of terms in describing acceptance, including acceptance,34,36 perception,27,29,30,37 experience,32 buy-in,38 receptiveness,23 and attitudes.41 Among the four studies using a five-point Likert scale (1 = poor acceptance, 5 = high acceptance), mean satisfaction with tele-ICU coverage ranged from 4.2227 to 4.53.35 Among residents training in ICUs equipped with tele-ICU, 66.7% wanted tele-ICU postresidency.37
In two studies evaluating preimplementation views of staff, there were significant misgivings about tele-ICU coverage. Initial resistance was most pronounced among nursing staff, but acceptance may improve over time.28 Another study that evaluated nurses’ preimplementation perceptions of tele-ICU coverage found that on a five-point Likert scale (1 = not favorable, 5 = favorable), perceived usefulness averaged 2.8 and attitude, 3.3.34
Evaluations of Impact on Quality of Patient Care:
Participants had positive views of the impact of tele-ICU coverage on patient care. Prior to implementation, 67% of the ICU physicians and nurses believed that tele-ICU coverage would enhance ICU quality of care23; postimplementation, between 82.3% and 100% of respondents reported tele-ICU coverage had successes in enhancing quality.28,32,33,37,45 Studies focusing exclusively on nursing perspectives were similarly favorable.21,27,42 Most ICU nurses believed that tele-ICU coverage increased patient survival (72%), but fewer thought it prevented medical errors (47%).29
Studies reported two potential negative consequences of tele-ICU coverage related to patient care. Two suggested that nurses in physical ICUs might not take advice from the monitoring center nurses.28,34 Four suggested that patient care might suffer if tele-ICU staffing diminished the quantity or quality of nurses in the ICU.5,34,36,40
Evaluations of Staff Impact:
Evaluations of how tele-ICU coverage affects an individual’s work were nuanced and complex. Before implementation, 67% of ICU staff believed that tele-ICU coverage would facilitate collaboration with intensivists23; after implementation, communication between the ICU and tele-ICU was rated good or very good by 94% of teleintensivists and by 98% of bedside physicians.33 Collaboration was perhaps more important to parent-child than to hub-and-spoke relationships,21,22,49,50 and compared with telephone contact, audiovisual interaction was associated with more intensivist suggestions and more-frequent implementation of those suggestions.22,28
Participants also cited potential barriers to acceptance of tele-ICU coverage. Nurses reported conflict arising when advice offered remotely conflicted with treatment prescribed by ICU attending physicians.34 Furthermore, some nurses practiced avoidance behaviors24 or simply waited until a consulting telephysician was on duty before seeking advice.40 Monitoring could foster resentment of the oversight process.5,22,29,31,34,40 Other challenges reported by staff included complaints that the tele-ICU coverage increased interruptions34 and workload,28,31 whereas other studies reported that the tele-ICU coverage may decrease interruptions41 and workload.5,25,30 Additionally, equipment shortcomings and malfunctions were reported in several studies.5,28,31,33‐35
Evaluations of Organizational Impact:
Staff consistently indicated that tele-ICU coverage should be tailored to the specific needs or capabilities of a particular ICU. In fact, preimplementation resistance often centered on concerns that the ICU was already functioning adequately and that external supervision would not be helpful.5,31,34 Even after implementation, some ICU staff saw little need for telecoverage at hospitals with a low volume of critically ill patients,31 although staff also recognized that tele-ICU coverage might allow certain higher complexity patients to be treated locally.21 Tele-ICU coverage also was perceived as more beneficial for ICUs with poorer baseline performance.5 Finally, ICUs with staffing challenges (eg, newly graduated nurses, gaps in physician coverage on nights and weekends) were thought to benefit more than others.34 In interviews with hospital administrators conducted by Berenson et al,5 three additional assessments emerged related to the tele-ICU impact on the organization. The first was a negative perception that the substantial cost did not justify the potential benefits. The second was a positive perception that tele-ICU coverage would leverage intensivist services, thereby enhancing patient care outside the hospital and facilitating partnerships with other hospitals and clinicians. The third was a positive perception that tele-ICU coverage would enhance the reputation of the hospital.
Discussion
In a systematic review of staff acceptance of tele-ICU coverage, we found that this technology generally was viewed favorably by physicians and nurses across an array of settings. In particular, staff generally viewed tele-ICU coverage as improving ICU quality despite initial reservations regarding the implementation of these systems. Staff also expressed the strong belief that the benefit of tele-ICU coverage would be greater for ICUs with specific quality issues (eg, difficulty in obtaining staffing) that could be affected. Our review also revealed important limitations in the methodologic rigor of many studies, highlighting the need for better evaluation of this costly new technology.
A number of our findings merit further discussion. First, it is important to address the quality and rigor of the available data. Although we identified 23 studies meeting our inclusion criteria, only seven were peer-reviewed studies that focused primarily on staff acceptance,30,33,34,36,38,40,41 and validated survey instruments were used in only two studies.34,41 This lack of rigorous data places hospital administrators and intensivists contemplating implementation of tele-ICU coverage in a difficult situation.
Second, our results suggest that staff acceptance of tele-ICU coverage is generally high. Although staff members have appropriate concerns about the impact of this technology ahead of implementation, most studies suggest that those who have worked in an ICU with tele-monitoring view the technology favorably.
Third, our review suggests that context matters. In other words, staff members seem to appreciate the fact that the benefit of tele-ICU coverage depends on the baseline performance of the ICU where coverage is initiated. In particular, ICUs with poorer baseline performance or more-significant challenges might benefit more, whereas ICUs with better baseline performance might benefit less. One could argue that this assumption is intuitive, but at the present time, it is actually quite uncertain which hospitals are choosing to implement tele-ICU coverage. Indeed, it is possible that ICUs with highly engaged intensivist leaders and high baseline quality may be the facilities choosing to purchase these systems.
Fourth, our review highlights several specific strategies that might facilitate tele-ICU acceptance by staff. ICU clinicians should participate early in the design and implementation of the tele-ICU.34 Physicians and hospital administrators should build support for tele-ICU coverage among the ICU staff prior to rollout.22,34 Clinicians from the monitoring center should visit the bedside teams in order to build trust on both sides of the camera.29,40 Audiovisual contact with the teleconsultant is better than audio contact alone.22,28 Hiring monitoring center physicians and nurses skilled in interpersonal communication is important for reducing the threat perceived by bedside teams.40
The findings allow us to speculate on additional ways to facilitate integration of the tele-ICU. Uncertain and conflicting treatment approaches undermine patient care, so hospital administrators must establish absolute agreement between the ICU staff and the monitoring center on best practices for operation. Procedures for physician-to-physician sign-out should be explicit so that ICU nurses know at all times the scope of the tele-ICU consultants’ authority. Administrators should encourage nurses to identify conflicting treatment directives and provide clear instructions for resolving those conflicts for the best care of the patient. Administrators also could enhance acceptance and decrease suspicion by arranging periodic face-to-face meetings or site visits for bedside and consulting clinicians.
Our review has several limitations. First, most of the included studies addressed staff acceptance only as a secondary consideration, so the level of detail reported often was deficient. Second, the heterogeneity of study designs and measures prevented us from conducting meta-analyses of the reported quantitative data. Nevertheless, the reporting of qualitative results was a strength of this review. Third, all but one study neglected to evaluate tele-ICU acceptance among administrators. This omission is important because administrators were typically the ones who determined whether tele-ICU coverage was purchased and implemented. Finally, acceptance by patients and families was not examined in the studies in this review and merits further investigation.
In conclusion, we found that although tele-ICU coverage was initially viewed with trepidation, after implementation, staff viewed this technology as improving ICU functioning in a number of diverse ways. This study highlights the need for careful planning and staff involvement prior to implementation of what can be viewed as a threatening and disruptive technology.
Acknowledgments
Author contributions: Dr Young had full access to the data and vouches for the integrity of the data analysis.
Dr Young: contributed to the conduct of the literature search and the analysis and wrote the original draft of the manuscript.
Dr Chan: contributed to the analysis and multiple revisions of the manuscript.
Dr Cram: contributed independent evaluation of the studies, to the analysis, and to the revision of subsequent drafts of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST to following conflicts: Dr Cram has received grant funding from the Veterans Administration for the research presented in this article and has given talks on tele-ICU but has not received or ever received funding from any corporate entities or other entities with a financial stake in tele-ICU care. Drs Young and Chan report that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. The funding sources had no role in the analyses or drafting of this manuscript.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (http://www.chestpubs.org/site/misc/reprints.xhtml).
Funding/Support: Dr Young is supported by a postdoctoral fellowship from the Department of Veterans Affairs. Dr Chan is supported by a K23 career development award [HL102224] from the National Heart, Lung, and Blood Institute. Dr Cram is supported by a K23 career development award [RR01997201] from the National Center for Research Resources at the National Institutes of Health and by the Robert Wood Johnson Physician Faculty Scholars Program. This work is also funded by the Veterans Administration Health Services Research and Development Service [grant IIR 09-336] and the National Heart, Lung, and Blood Institute at the National Institutes of Health [R01 HL085347]. This material is based on work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, and the VA Midwest Rural Health Resource Center.
References
- 1.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288(17):2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 2.Duke EM. Report to Congress: The Critical Care Workforce: A Study of the Supply and Demand for Critical Care Physicians. Washington, DC: US Department of Health and Human Services HRSA; 2006. [Google Scholar]
- 3.Gutsche JT, Kohl BA. Who should care for intensive care unit patients? Crit Care Med. 2007;35(2 suppl):S18–S23. doi: 10.1097/01.CCM.0000252907.47050.FE. [DOI] [PubMed] [Google Scholar]
- 4.National Library of Medicine . National Library of Medicine: medical subject Headings. Bethesda, MD: National Library of Medicine; 2010. [Google Scholar]
- 5.Berenson RA, Grossman JM, November EA. Does telemonitoring of patients—the eICU—improve intensive care? Health Aff (Millwood) 2009;28(5):w937–w947. doi: 10.1377/hlthaff.28.5.w937. [DOI] [PubMed] [Google Scholar]
- 6.Breslow MJ. Remote ICU care programs: current status. J Crit Care. 2007;22(1):66–76. doi: 10.1016/j.jcrc.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Society of Critical Care Medicine . Tele-ICU Monitoring and Care. Mount Prospect, IL: Society of Critical Care Medicine; 2009. [Google Scholar]
- 8.Thomas EJ, Lucke JF, Wueste L, Weavind L, Patel B. Association of telemedicine for remote monitoring of intensive care patients with mortality, complications, and length of stay. JAMA. 2009;302(24):2671–2678. doi: 10.1001/jama.2009.1902. [DOI] [PubMed] [Google Scholar]
- 9.Morrison JL, Cai Q, Davis N, et al. Clinical and economic outcomes of the electronic intensive care unit: Results from two community hospitals. Crit Care Med. 2010;38(1):2–8. doi: 10.1097/CCM.0b013e3181b78fa8. [DOI] [PubMed] [Google Scholar]
- 10.Rosenfeld BA, Dorman T, Breslow MJ, et al. Intensive care unit telemedicine: alternate paradigm for providing continuous intensivist care. Crit Care Med. 2000;28(12):3925–3931. doi: 10.1097/00003246-200012000-00034. [DOI] [PubMed] [Google Scholar]
- 11.Kohl BA, Gutsche JT, Kim P, et al. Effect of telemedicine on mortality and length of stay in a university ICU. Crit Care Med. 2007;35(12):A22. [Google Scholar]
- 12.Stern L. Care from afar: small hospitals use technology to run remote ICUs. Newsweek. 2007;150(12):E18. [PubMed] [Google Scholar]
- 13.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 14.Centre for Reviews and Dissemination . Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Healthcare. York, England: CRD, University of York; 2008. [Google Scholar]
- 15.Agency for Healthcare Research and Quality . Services UDoHaH. Rockville, MD: Public Health Service; 2002. Systems To Rate the Strength of Scientific Evidence; pp. 1–11. [Google Scholar]
- 16.Krippendorff K. Content Analysis: An Introduction to Its Methodology. 2nd ed. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 17.Baxter LA, Babbie E. The Basics of Communication Research. Belmont, CA: Wadsworth; 2004. [Google Scholar]
- 18.Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- 19.Tashakkori A, Teddlie C. Mixed Methodology: Combining Qualitative and Quantitative Approaches. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 20.Victoria, Australia: QSR International Pty Ltd; 2008. NVivo Qualitative Data Analysis Software [computer program] [Google Scholar]
- 21.Zawada ET, Jr, Herr P, Larson D, Fromm R, Kapaska D, Erickson D. Impact of an intensive care unit telemedicine program on a rural health care system. Postgrad Med. 2009;121(3):160–170. doi: 10.3810/pgm.2009.05.2016. [DOI] [PubMed] [Google Scholar]
- 22.Westbrook JI, Coiera EW, Brear M, et al. Impact of an ultrabroadband emergency department telemedicine system on the care of acutely ill patients and clinicians’ work. Med J Aust. 2008;188(12):704–708. doi: 10.5694/j.1326-5377.2008.tb01850.x. [DOI] [PubMed] [Google Scholar]
- 23.Sucher J, Jones S, Montoya I, et al. ICU staff receptiveness to remote telepresence. Paper presented at: American Telemedicine Association Fourteenth Annual Meeting and Exposition. April 2009 Las Vegas, NV. [Google Scholar]
- 24.Siek T, Cox R, Schmidt J. eICU impact in a rural community hospital. Paper presented at: American Telemedicine Association Thirteenth Annual Meeting and Exposition. April 2008 Seattle, WA. [Google Scholar]
- 25.Poropatich RK, Barrigan C, Chung KK, et al. Deployment of a robotic tele-presence capability in the US Army. Paper presented at: American Telemedicine Association Thirteenth Annual Meeting and Exposition. April 2008 Seattle, WA. [Google Scholar]
- 26.McNelis J, Spector R, Kiley M, et al. Off hours remote presence technology (RPT) enhances communication between intensivists and staff. Crit Care Med. 2008;36(12):A20. [Google Scholar]
- 27.Marttos A, Wilson K, Krauthamer S, et al. Telerounds in a trauma ICU dept. Crit Care Med. 2008;36(12):A53. [Google Scholar]
- 28.Grundy BL, Crawford P, Jones PK, et al. Telemedicine in critical care: an experiment in health care delivery. JACEP. 1977;6(10):439–444. doi: 10.1016/s0361-1124(77)80239-6. [DOI] [PubMed] [Google Scholar]
- 29.DiMartino J, Fortino-Mullen M, Entrikin L, et al. Bedside nurse perceptions of intensive care unit telemedicine. Crit Care Med. 2009;37(12):A283. doi: 10.4037/ajcc2012801. [DOI] [PubMed] [Google Scholar]
- 30.Coletti C, Elliott D, Zubrow M. Resident perceptions of an integrated remote ICU monitoring system. Crit Care Med. 2008;36(12):290. [Google Scholar]
- 31.Crawley EA. eICU impact in the military. Paper presented at: American Telemedicine Association Thirteenth Annual Meeting and Exposition. April 2008 Seattle, WA. [Google Scholar]
- 32.Faiz SA, Zachria A, Weavind L, et al. Fellowship education in remote telemonitoring units. Chest. 2006;130(4 suppl):112S–113S. [Google Scholar]
- 33.Heath B, Salerno R, Hopkins A, Hertzig J, Caputo M. Pediatric critical care telemedicine in rural underserved emergency departments. Pediatr Crit Care Med. 2009;10(5):588–591. doi: 10.1097/PCC.0b013e3181a63eac. [DOI] [PubMed] [Google Scholar]
- 34.Kowitlawakul Y. The Technology Acceptance Model: predicting nurses’ acceptance of telemedicine technology (eICU) Comput Inform Nurs. doi: 10.1097/NCN.0b013e3181f9dd4a. In press. doi:10.1097/NCN.0b013e3181f9dd4a. [DOI] [PubMed] [Google Scholar]
- 35.Marcin JP, Nesbitt TS, Kallas HJ, Struve SN, Traugott CA, Dimand RJ. Use of telemedicine to provide pediatric critical care inpatient consultations to underserved rural Northern California. J Pediatr. 2004;144(3):375–380. doi: 10.1016/j.jpeds.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 36.Mathews S, Wood C, Kagel E. Smile you’re on EICU: A collaborative critical care team to enhance patient outcomes. Crit Care Nurse. 2007;27(2):122. [Google Scholar]
- 37.Mora A, Faiz SA, Kelly T, et al. Resident perception of the educational and patient care value from remote telemonitoring in a medical intensive care unit. Chest. 2007;132(4):443a. [Google Scholar]
- 38.Roberts G, Dewoody S. Lights, camera, collaboration: implementation of an eICU orientation program. Crit Care Nurse. 2008;28:e12. [Google Scholar]
- 39.Rogove H, Atkins C, Kramer J, et al. Enhanced access to neurointensivists through a telemedicine program. Crit Care Med. 2009;37(12 suppl):A1. [Google Scholar]
- 40.Stafford TB, Myers MA, Young A, Foster JG, Huber JT. Working in an eICU unit: life in the box. Crit Care Nurs Clin North Am. 2008;20(4):441–450. doi: 10.1016/j.ccell.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 41.Thomas EJ, Chu-Weininger MYL, Lucke J, et al. The impact of a tele-ICU on provider attitudes about teamwork and safety climate. Crit Care Med. 2007;35(12 suppl):A145. doi: 10.1136/qshc.2007.024992. [DOI] [PubMed] [Google Scholar]
- 42.Youn BA. Utilizing robots and an ICU telemedicine program to provide intensivist support for rapid response teams. Chest. 2006;130(Suppl):102S. [Google Scholar]
- 43.Zawada ET, Herr P. ICU telemedicine improves care to rural hospitals reducing costly transports. Crit Care Med. 2008;36(4):668. [Google Scholar]
- 44.Grundy BL, Jones PK, Lovitt A. Telemedicine in critical care: problems in design, implementation, and assessment. Crit Care Med. 1982;10(7):471–475. doi: 10.1097/00003246-198207000-00014. [DOI] [PubMed] [Google Scholar]
- 45.Chung KK, Grathwohl KW, Poropatich RK, et al. Bedside nurse perceptions of intensive care unit telemedicine. Crit Care Med. 2009;37(12):A441. [Google Scholar]
- 46.Chung KK, Grathwohl KW, Poropatich RK, Wolf SE, Holcomb JB. Robotic telepresence: past, present, and future. J Cardiothorac Vasc Anesth. 2007;21(4):593–596. doi: 10.1053/j.jvca.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 47.Murphy M, Stapleton S, Cregan P, et al. Using remote critical care units in Australia. Paper presented at: American Telemedicine Association Twelfth Annual Meeting and Tradeshow. May 2007 Nashville, TN. [Google Scholar]
- 48.Wilson L, Hansen SK, Li J, et al. A broadband telemedicine application for critical care in Australia. Paper presented at: American Telemedicine Association Twelfth Annual Meeting and Tradeshow. May 2007 Nashville, TN. [Google Scholar]
- 49.Wilson L, Hansen SK, Skinner MW. Design and evaluation of a broadband telemedicine system for supporting ICUs in regional hospitals. Paper presented at: American Telemedicine Association Thirteenth Annual Meeting and Exposition. April 2008 Seattle, WA. [Google Scholar]
- 50.Herr P. eICU impact in a rural health system. Paper presented at: American Telemedicine Association Thirteenth Annual Meeting and Exposition. April 2008 Seattle, WA. [Google Scholar]