Abstract
Objectives
Depression during pregnancy is one of the strongest predictors of postpartum depression, which, in turn, has deleterious, lasting effects on infant and child well-being and on the mother’s and father’s mental health. The primary question guiding this randomized controlled trial was, Does culturally relevant, enhanced brief interpersonal psychotherapy (IPT-B) confer greater advantages to low-income, pregnant women than those that accrue from enhanced usual care in treating depression in this population? Enhanced IPT-B is a multicomponent model of care designed to treat antenatal depression and consists of an engagement session, followed by eight acute IPT-B sessions before the birth and maintenance IPT up to six months postpartum. IPT-B was specifically enhanced to make it culturally relevant to socioeconomically disadvantaged women.
Methods
Fifty-three non–treatment-seeking, pregnant African-American and white patients receiving prenatal services in a large, urban obstetrics and gynecology clinic and meeting criteria for depression on the Edinburgh Postnatal Depression Scale (score >12 on a scale of 0 to 30) were randomly assigned to receive either enhanced IPT-B (N=25) or enhanced usual care (N=28), both of which were delivered in the clinic. Participants were assessed before and after treatment on depression diagnoses, depressive symptoms, and social functioning.
Results
Intent-to-treat analyses showed that participants in enhanced IPT-B, compared with those in enhanced usual care, displayed significant reductions in depression diagnoses and depressive symptoms before childbirth (three months postbaseline) and at six months postpartum and showed significant improvements in social functioning at six months postpartum.
Conclusions
Findings suggest that enhanced IPT-B ameliorates depression during pregnancy and prevents depressive relapse and improves social functioning up to six months postpartum.
From a public health perspective, it is critical to consider the mental health treatment needs of women during the perinatal period, particularly those who are socioeconomically disadvantaged. Maternal postpartum depression, if not buffered by protective factors in the family, has deleterious, lasting effects on infant and child well-being (1,2) and on the mother’s and father’s subsequent mental health (3,4). A meta-analysis (5) indicated that depression during pregnancy has been repeatedly demonstrated to be the most potent predictor of postpartum depression. In this article, depression refers to major depressive disorder as defined in the DSM-IV (6), unless otherwise indicated.
Prevalence rates of antenatal major and minor depression have been estimated in community-based studies to range from 7% to 15% of all pregnancies (7,8), but higher rates have been observed among women of lower socioeconomic status (9–12). Some epidemiological studies also suggest that individuals living in poverty, compared with those in the general population, are at increased risk of major depression (13) and that women who are poor, compared with women in general, have higher rates of depressive symptoms (14). Pregnancy provides an opportunity to involve women in mental health interventions (15) and appears to be a time when women with depression prefer psychotherapy to pharmacotherapy (16), because of the potential adverse effects of medications on the developing fetus and the nursing infant (17). At the same time, however, childbearing and childrearing women with depression, especially those who are socioeconomically disadvantaged, have proven difficult to engage and retain in adequate mental health treatment (11,18,19).
Studies have identified a number of practical, psychological, and cultural barriers to mental health service use by low-income populations, including cost, inconvenient clinic locations, transportation, limited hours, childcare, stigma, discrimination, previous negative treatment experiences, burden of depression, and the provider’s cultural insensitivity (20,21). Women who are poor also more frequently experience threatening and uncontrollable life events, exposure to multiple forms of interpersonal and community violence (that is, emotional, physical, and sexual violence and witnessing violence), and chronic stressors (12,22). Thus, to be effective for treating depression among low-income, pregnant women, a psychotherapeutic intervention needs to take into account the stressful context of their lives.
The primary research question guiding the study presented here was, Does culturally relevant, enhanced brief interpersonal psychotherapy (IPT-B) for depression confer greater advantages to low-income, pregnant women than those that accrue from enhanced usual care? Enhanced IPT-B is a multicomponent model of care (23) consisting of an engagement session, followed by eight acute IPT-B sessions before the birth and maintenance IPT up to six months postpartum (24), and it is augmented with modifications to make it culturally relevant to women who are socioeconomically disadvantaged (23). IPT-B was derived from IPT (25), which has demonstrated efficacy in treating acute depression (26–28), in preventing depressive relapse through maintenance IPT (29), and in treating antenatal and postpartum depression (30,31). Enhanced IPT-B retains the essential theory, targets, and techniques of IPT and has received empirical support in a number of studies (32–35).
In a previous report (36), we presented data showing that non–treatment-seeking, pregnant, low-income African-American and white participants with depression who received enhanced IPT-B in an obstetrics and gynecology clinic had higher rates of engagement (defined as more participants attending an initial treatment session) and higher rates of retention (defined as more treatment sessions attended) than did those who received enhanced usual care. Those in the enhanced usual care group received depression education materials, their social worker received notification (with the patient’s permission) of their elevated depressive symptoms, and they received a referral to the behavioral health center in the same obstetrics and gynecology clinic. In the study presented here, using the same sample, we hypothesized that treatment with enhanced IPT-B, followed by maintenance IPT, would result in significant improvements in psychopathology and functioning during pregnancy and at six months postpartum, compared with enhanced usual care.
Methods
Participants and setting
All research procedures were approved by the institutional review board of the University of Pittsburgh. Potential participants were recruited from the public care outpatient obstetrics and gynecology clinic of a large women’s hospital in Pittsburgh, Pennsylvania, where most of the low-income patients were on Medicaid. Pregnant women were referred to the study by clinic health care professionals, the research registry, and clinic flyers. Potential participants were deemed eligible for inclusion in the protocol based on the following criteria: 18 years or older, ten to 32 weeks gestation, cutoff score >12 on the Edinburgh Postnatal Depression Scale (EPDS) (37) (possible scores on the EPDS range from 0 to 30, with higher scores indicating greater depression severity), English speaking, access to a telephone, and living in the Pittsburgh region. Participants were excluded from the study and referred for appropriate treatment if they met any of the following criteria: substance abuse or dependence within the preceding six months; actively suicidal; bipolar disorder, a psychotic disorder, or an organic mental disorder; an unstable medical condition that could produce symptoms confounding accurate assessment of mood symptoms (for example, untreated thyroid disease); severe intimate partner violence; and current receipt of another form of depression treatment (that is, psychotherapy or pharmacotherapy). After receiving a complete description of the study, participants gave written informed consent.
Randomization
Using a permuted block design stratified by race, we randomly assigned participants to receive either enhanced IPT-B or enhanced usual care after an initial screening procedure that determined whether participants met basic inclusion criteria but before full determination of eligibility. This permitted investigators to administer to those assigned to receive enhanced IPT-B the pretreatment engagement session immediately after initial screening, a procedure considered essential to addressing barriers to care in a difficult-to-engage, non–treatment-seeking population. A formal diagnostic assessment (see below) followed randomization and the engagement session to rule out exclusion criteria.
A total of 113 women consented to screening for inclusion in the study from March 2004 through December 2006. Of the 113 women, 42 did not meet the initial screening criterion (score >12 on the EPDS). Five met this criterion but declined to participate in a research study. Of the 66 participants randomly assigned to treatment, three met the initial screening criterion but did not meet criteria on the second diagnostic screening, because of severe intimate partner violence (N=1), bipolar disorder (N=1), and current marijuana abuse (N=1). Ten participants met the first screening criterion but dropped out before the second screening; a lack of time was given as the most common reason. Thus a total of 53 participants entered the study (25 in enhanced IPT-B and 28 in enhanced usual care).
Assessments
Participants were assessed during pregnancy at baseline, three months postbaseline, and six months postpartum via valid and reliable assessment tools. The ten-item EPDS was used to determine study eligibility (with a cutoff score of >12) and to measure depression severity over time. A cutoff score of 12 or 13 on the EPDS has shown a sensitivity of 86% and a specificity of 78% (37). Depression severity was also measured with the 21-item Beck Depression Inventory (BDI) (38), which has shown a sensitivity of 100% and a specificity of 84% in a randomly selected community sample of adults, using a cutoff score of 10 (39).
Anxiety symptoms were assessed with the 21-item Beck Anxiety Inventory (BAI) (40), which has been found to have a sensitivity of .76 and a specificity of .77 for any anxiety diagnosis when a cutoff score of 5.5 is used (41). Social functioning was measured with the Social and Leisure Domain of the Social Adjustment Scale (SAS) (42,43), using a cutoff of >2.2 to indicate normal functioning in this domain. The SAS has successfully measured social functioning in community samples and among persons with schizophrenia, those who have alcoholism, and those who are depressed (44). Lifetime and current major depressive disorder was assigned with the Structured Clinical Interview for DSM-IV, Clinician Version (SCID) (45), and other lifetime and current psychiatric disorders were assigned by using the Diagnostic Interview Schedule (DIS), a fully structured interview designed to be administered by lay interviewers (46).
At the six-month postpartum assessment, participants were also evaluated on how well they thought they were taking care of the new baby, as assessed with the nine-item new baby subscale of the Postpartum Adjustment Questionnaire (PPAQ) (47). In addition, IPT-B participants completed the EPDS and a four-item treatment satisfaction survey (available from the authors) at the beginning and end, respectively, of each treatment session. Assessments were administered by a master’s-level social worker and a doctoral-level psychologist trained and certified in the administration of the DIS and SCID (according to the standards of the Biometrics Division of the New York State Psychiatric Institute).
Culturally relevant, enhanced brief interpersonal psychotherapy
Participants assigned to culturally relevant, enhanced IPT-B were informed of their diagnoses, given written educational materials about depression, and referred for depression treatment provided in an office in the obstetrics and gynecology clinic where they were receiving prenatal services. Enhanced IPT-B is a multicomponent model of care (23) consisting of an engagement session, acute IPT-B, and maintenance IPT (24). It is also augmented with culturally relevant modifications. One doctoral-level clinician and one master’s-level clinician, both of whom had supervised training and experience in enhanced IPT-B, served as therapists, followed detailed treatment manuals, and received weekly supervision by an expert (NG or HS). Engagement and IPT-B sessions were audiotaped, and 77% were reviewed for fidelity to the model.
Briefly, the engagement session, described elsewhere (36,48), is based on principles of motivational interviewing and ethnographic interviewing and is designed to promote engagement by building trust and addressing the practical, psychological, and cultural barriers to care experienced by individuals who are socioeconomically disadvantaged. More specifically, during engagement, the interviewer elicits each participant’s unique barriers to care and engages in collaborative problem solving to ameliorate each barrier. For example, if a participant doubts the relevance of treatment to her problems—specifically whether enhanced IPT-B could reduce her depression triggered by losing her job—the interviewer would inform her that this treatment can assist her in finding a new job or job training, in addition to helping her manage the interpersonal difficulties resulting from the job loss. In addition, the interviewer approaches the participant in a culturally sensitive manner consistent with the principles of ethnographic interviewing: the interviewer adopts a one-down position as a learner; tries to understand the cultural perspectives and values of the woman without bias; inquires about the woman’s view of depression, health-related beliefs, and coping practices (for example, the importance of spirituality or familismo in her life); and asks what the woman would like in a therapist, including the importance of race-ethnicity.
IPT-B, similar to IPT, is designed to treat depression by helping patients resolve one of four interpersonal problem areas (that is, role transition, role dispute, grief, and interpersonal deficits) related to the onset or maintenance of a depressive episode, but it differs from IPT in a number of ways (23,Swartz HA, Grote NK, Frank E, et al., unpublished treatment manual, 2003). For example, to reduce treatment burden and activate change in the participant, the format of IPT-B treatment is restructured into eight rather than 16 sessions, a focus on the long-term problem area of interpersonal deficits is avoided, and between-session behavioral activation strategies that have an interpersonal focus are encouraged (23).
Given the considerable body of evidence that major depression is a chronic condition in which recurrence is expected (49), we provided biweekly or monthly maintenance IPT sessions up to six months postpartum to prevent depressive relapse by helping participants deal effectively with the social and interpersonal stressors associated with remission (24). Because the goal of maintenance IPT is to maintain recovery, the patient is encouraged to be watchful for the appearance of early somatic, affective, or cognitive symptoms related to prior depressive episodes and to practice skills learned in IPT-B to prevent relapse. Maintenance IPT also differs from IPT-B in that the patient can focus on more than one interpersonal problem area while she is in remission.
Finally, a number of culturally relevant additions (23) of a pragmatic nature were integrated into IPT-B, including free bus passes, childcare, and the facilitation of access to needed social services (that is, food, job training, housing, and free baby supplies), similar to the case management component added to cognitive-behavioral therapy in a previous depression treatment study with low-income women (50). Engagement and IPT-B sessions were delivered in an office in the large obstetrics and gynecology clinic to make treatment more accessible and less stigmatizing. At times when participants could not attend treatment, the session was conducted on the phone to maintain continuity, a practice found to be effective in the delivery of psychotherapy and pharmacotherapy for depression (51).
Further, as described previously (52), we enhanced IPT-B in ways that reflected seven out of the eight components delineated in the culturally centered framework of Bernal and colleagues (53): persons, metaphors, concepts, content, goals, methods, and contexts. For example, we addressed the component of persons by employing therapists who were trained in cultural competence and had considerable experience working with persons of racial-ethnic minority groups who were living in poverty. We also utilized the component of metaphors by displaying culturally relevant pictures of racially and ethnically diverse infants in the therapist’s office and by using stories from the participants’ cultural background to reinforce treatment goals. To address the component of concepts, therapists provided education about depression in a way that was congruent with the participant’s culture and used the word “stressed” instead of the word “depressed,” if a participant so desired, to minimize her perceived stigma of depression. The component of content was addressed by exploring what coping mechanisms and cultural resources, such as spirituality or familismo, had helped participants through adversity in the past and by building on these resources during treatment. Therapists helped clients develop treatment goals that were personally and culturally relevant to them. Methods were addressed by intensive outreach and shortening treatment to reduce participant burden. Contexts were addressed by the pragmatic additions described above, such as facilitation of access to needed social services.
Enhanced usual care
Participants assigned to enhanced usual care were informed of their diagnoses, given written educational materials about depression, and were strongly encouraged to seek treatment at the behavioral health center located in the obstetrics and gynecology clinic where they were receiving prenatal services (or at the neighborhood mental health center, if they preferred). Enhanced usual care participants were provided the same advantages as the IPT-B group to help them overcome practical barriers—easy access to depression treatment in the obstetrics and gynecology clinic, familiarity with the setting, decreased stigma, childcare, and free bus passes. In addition, participants in the enhanced usual care group received more monitoring of their depression severity and diagnostic status than they typically received in the clinic, inasmuch as research staff contacted them every three weeks to assess their mood and to encourage them to enter treatment, as indicated. With the participant’s permission, a note was placed in her medical record indicating the presence of major depression and her social worker was contacted to reinforce the treatment referral. True usual care for depressed pregnant or postpartum women would risk human subjects concerns for these women and their families.
Data analysis
Participants in enhanced IPT-B (N=25) and enhanced usual care (N=28) were compared at baseline on demographic and clinical characteristics by using chi square tests and analysis of variance, as appropriate. Overall study attrition rate was low (N=7, 13%) for this diverse sample (18) and equivalent across treatment groups. The amount of missing data for our primary outcome measure, the Edinburgh Postnatal Depression Scale, was 8% (N=4 out of 53) before childbirth (three months postbaseline [time 2]) and 13% (N=7 out of 53) at six months postpartum (time 3) and was equivalent across groups at each time point. By examining reasons for dropout, we concluded that the data were likely missing at random. Thus mixed-effects models using maximum likelihood procedures were employed to conduct intent-to-treat analyses to assess change in clinical and functioning variables from baseline to time 2 and time 3 (54). Typically, a 50% reduction in symptom score (an indication of treatment response) has been an accepted measurement of clinical improvement in randomized trials evaluating treatment for depression (55–57). To detect 50% improvement in depressive symptoms on the EPDS, we used mixed-effects models to impute the missing scores and then conducted chi square analyses. To detect improvement in depression diagnostic status at times 2 and 3, a likely indicator of remission, we conducted chi square analyses. Conventional alpha levels (p<.05) were used to determine statistically significant differences. Effect sizes, appropriate to each type of analysis, were also calculated (58). In the Results section, we refer to enhanced IPT-B and enhanced usual care as IPT-B and usual care, respectively.
Results
Baseline demographic and clinical characteristics
Demographic and clinical information for each group is summarized in Table 1. Analyses show that participants in the IPT-B and usual care groups did not differ significantly on any of these baseline demographic or clinical characteristics. Similar to the patient population at the obstetrics and gynecology clinic, a majority of our sample was African American (N=33, 62%); not married (N=43, 81%); had a high school degree, GED, vocational training, or some college (N=41, 77%); were currently unemployed (N=34, 64%); and had incomes less than $20,000 (N=45, 85%).
Table 1.
Demographic and clinical characteristics of pregnant women on low incomes scoring >12 on the Edinburgh Postnatal Depression Scale (EPDS)a
| Enhanced brief interpersonal psychotherapy (N=25) |
Enhanced usual care (N=28) |
||||
|---|---|---|---|---|---|
| Characteristic | N | % | N | % | p |
| Education | .162 | ||||
| Less than high school | 2 | 8 | 5 | 18 | |
| High school degree | 6 | 24 | 4 | 14 | |
| GED | 4 | 16 | 3 | 11 | |
| Vocational degree or some college | 9 | 36 | 15 | 54 | |
| College or graduate degree | 4 | 16 | 1 | 4 | |
| Employment | .729 | ||||
| Full-time | 5 | 20 | 3 | 11 | |
| Part-time | 6 | 24 | 5 | 18 | |
| Unemployed | 14 | 56 | 20 | 71 | |
| Income | .332 | ||||
| <$10,000 | 12 | 48 | 19 | 68 | |
| $10,000–$20,000 | 8 | 32 | 6 | 21 | |
| >$20,000 | 5 | 20 | 3 | 11 | |
| Race-ethnicity | .276 | ||||
| White | 5 | 20 | 10 | 36 | |
| African American | 17 | 68 | 16 | 57 | |
| Latina | 2 | 8 | 0 | — | |
| Biracial | 1 | 4 | 2 | 7 | |
| Marital status | .300 | ||||
| Never married | 14 | 56 | 12 | 43 | |
| Married | 2 | 8 | 2 | 7 | |
| Cohabiting | 9 | 36 | 8 | 29 | |
| Divorced, separated, or widowed | 0 | — | 6 | 21 | |
| Depression diagnosis | |||||
| Major depression | 23 | 92 | 22 | 79 | .173 |
| Dysthymia | 3 | 12 | 4 | 14 | .806 |
| Comorbid major depression and dysthymia | 3 | 12 | 4 | 14 | .806 |
| Minor depression | 1 | 4 | 2 | 7 | .621 |
| Anxiety diagnosis | |||||
| Panic disorder | 5 | 20 | 7 | 25 | .664 |
| Posttraumatic stress disorder | 7 | 28 | 5 | 18 | .378 |
| Social phobia | 6 | 24 | 3 | 11 | .198 |
| At least 1 anxiety disorder | 14 | 56 | 13 | 46 | .487 |
| Baseline functioning (M±SD score) | |||||
| EPDSa | 18.9±3.4 | 18.2±3.8 | .613 | ||
| BDIb | 24.3±10.2 | 25.9±11.1 | .286 | ||
| BAIc | 14.4±11.0 | 16.3±10.5 | .526 | ||
| Social and leisured | 3.1±.8 | 3.2 ±.6 | .565 | ||
| Median number of previous depressive episodese | 2.5 | 2.5 | |||
| Age (M±SD) | 24.3±5.3 | 24.7±5.6 | .791 | ||
| Weeks pregnant (M±SD) | 22.6±6.7 | 20.4±6.8 | .253 | ||
| Number of adults at home (M±SD) | 2.0±.7 | 2.1±1.0 | .653 | ||
| Number of children at home (M±SD) | 1.4±1.7 | 1.4±1.3 | .912 | ||
A score of >12 indicates the presence of depression. Possible scores range from 0 to 30, with higher scores indicating more symptoms.
Beck Depression Inventory. Possible scores range from 0 to 63, with higher scores indicating more symptoms.
Beck Anxiety Inventory. Possible scores range from 0 to 63, with higher scores indicating more symptoms.
Social and leisure domain on the Social Adjustment Scale. Possible scores range from 1 to 5, with higher scores indicating greater impairment.
Range for enhanced brief interpersonal therapy, 0 to 15; range for enhanced usual care, 0 to 25
Data shown in Table 1 indicate that at baseline the entire sample was moderately depressed on the EPDS and moderately to severely depressed on the BDI. Rates of recurrent depression in the two groups did not differ at baseline (IPT-B: N=14, 56%, and usual care: N=18, 64%). Over half of the sample met criteria for at least one anxiety disorder, with 23% meeting criteria for panic disorder and 23% meeting criteria for posttraumatic stress disorder (PTSD). Participants’ social functioning was compromised in the social and leisure domain (interacting with and confiding in friends), according to a cutoff >2.2 on the social and leisure domain of the SAS (44).
Treatment adherence and other characteristics
As reported previously (36), patients in the IPT-B group showed significantly higher rates of treatment engagement and retention than patients in the usual care group, with 68% (N=17) of the IPT-B group compared with 7% (N=2) in usual care completing a full course of treatment, defined as seven to eight sessions. Sixty-eight percent (N=17) participated in an average of six maintenance IPT sessions (range, two to ten). Half of the IPT-B group (N=12) participated in an average of two to three phone sessions (range, one to six) during IPT-B and maintenance IPT. The therapist facilitated access to social services for 48% of participants in the IPT-B group (N=12), with an average of two referrals per woman. Sixty-seven percent (N=8) of those receiving referrals in the IPT-B group reported successfully following through.
Change in depression diagnostic status and depressive symptoms
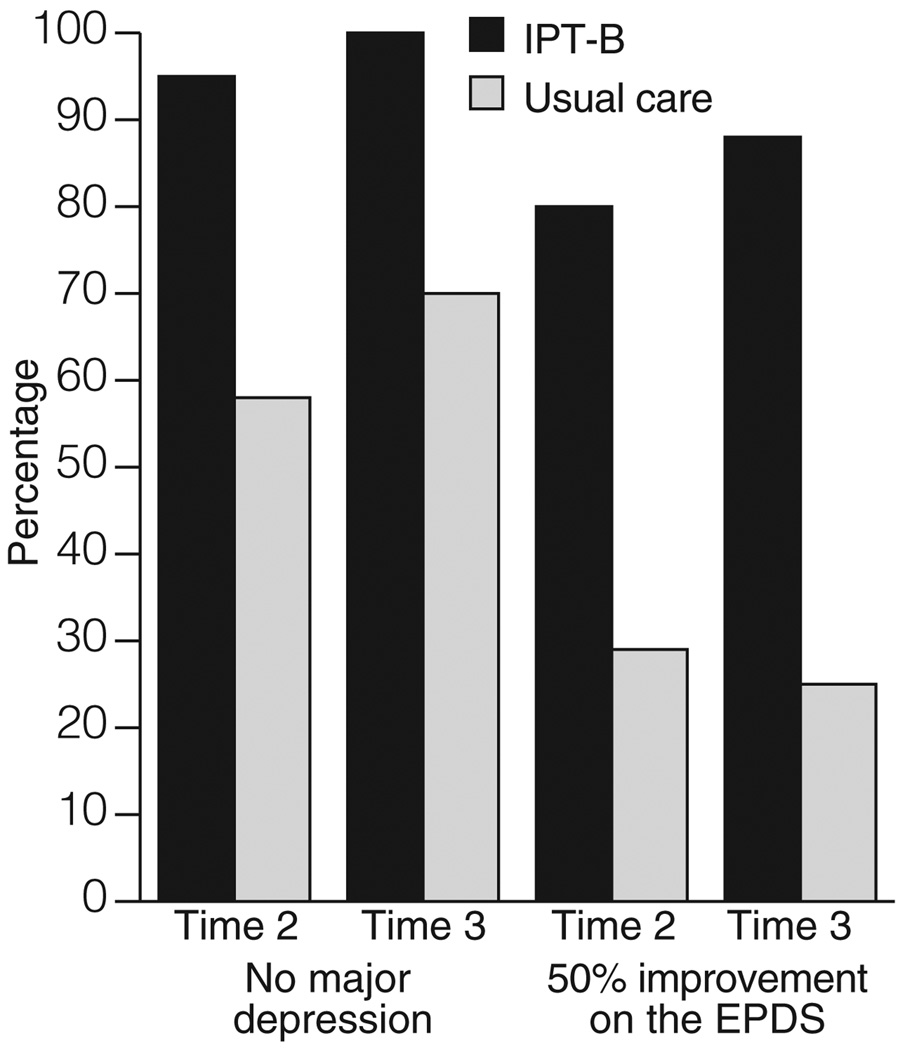
Figure 1 depicts the percentages of women in IPT-B and usual care who were not depressed at three months postbaseline (time 2, before childbirth) and at six months postpartum (time 3). At time 2, chi square analyses showed that a significantly larger proportion of women in the intervention group (N=21 of 22, 95%) no longer met criteria for major depression on the SCID, compared with those in usual care (N=15 of 26, 58%), with a large effect size (χ2=9.06, df=1, p<.003; Cohen’s h=.96). Similarly, at time 3, analyses revealed that none of the women assigned to IPT-B had major depression, compared with 70% of those in usual care (N=16 of 23), with a very large effect size (χ2=7.92, df=1, p<.005; Cohen’s h=1.22). Further, with respect to 50% improvement on the EPDS, chi square analyses showed that at time 2 (before childbirth), 80% (N=20 of 25) of the intervention group responded to treatment, compared with 29% (N=8 of 28) of the usual care group, with a large effect size (χ2=14.02, df=1, p<.001; Cohen’s h=1.08). At time 3, 88% (N=22 of 25) of women in IPT-B responded to treatment, compared with 25% (N=7 of 28) of those in usual care, with a large effect size (χ2=21.16, df=1, p<.001; Cohen’s h=1.17).
Figure 1.
Rates of clinical improvement over time among pregnant women with low incomes scoring >12 on the Edinburgh Postnatal Depression Scale (EPDS) and receiving enhanced brief interpersonal psychotherapy (IPT-B) or enhanced usual carea
a Measurements from baseline to three months postbaseline (before childbirth) (time 2) and from baseline to six months postpartum (time 3)
Change in clinical and social functioning symptom scores
Table 2 displays the statistical results of mixed-effects models using maximum likelihood procedures to assess the main effects of intervention group, time, and their interaction on clinical and functional outcomes. The pattern of findings indicates that symptoms of depression improved significantly more in the IPT-B group than in the usual care group between baseline and time 2 and between baseline and time 3. There was a trend showing that social functioning and anxiety symptoms also improved more in the IPT-B group than in the usual care group between baseline and time 2, but these findings were not significant (p=.063 and .051). Social functioning improved significantly more in the IPT-B group than in the usual care group between baseline and time 3. That is, over time participants in the IPT-B group were feeling significantly less depressed and anxious, having more enjoyable contact with and confiding in friends, and spending more time in interesting activities. Overall treatment satisfaction in the IPT-B group was quite high (mean±SD=4.4±.39; 1–5 rating scale). Table 2 also presents the pattern of effect sizes (Cohen’s d) computed for the interaction term estimates at times 2 and 3. It appears that from baseline to time 2 (before childbirth) effect sizes for the outcome variables range from medium to large (58). From baseline to six months postpartum, the effect sizes appear to become stronger. This pattern suggests that the effects of the intervention may become more potent over time.
Table 2.
Repeated-measures mixed-effects models evaluating effects of treatment assignment, time, and their interaction on symptoms and functioning among pregnant women with low incomes scoring >12 on the Edinburgh Postnatal Depression Scalea
| Enhanced usual care (N=28) |
Enhanced brief interpersonal psychotherapy (N=25) |
Treatment | Time | Treatment × time | Effect sizeb |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | M | SD | M | SD | F | df | p | F | df | p | F | df | p | |
| Baseline and time 2 (before childbirth) | ||||||||||||||||||
| EPDSc | 18.1 | 3.8 | 13.6 | 6.6 | 18.9 | 3.4 | 5.7 | 4.6 | 11.06 | 1, 51 | .002 | 115.36 | 1, 48 | <.001 | 26.80 | 1, 48 | <.001 | 71 |
| BDId | 25.9 | 11.1 | 21.3 | 11.1 | 24.3 | 10.2 | 10.0 | 7.7 | 10.30 | 1, 51 | .002 | 22.18 | 1, 47 | <.001 | 5.93 | 1, 47 | .019 | .33 |
| BAIe | 16.3 | 10.5 | 15.9 | 8.9 | 14.4 | 11.0 | 6.6 | 5.1 | 9.15 | 1, 51 | .004 | 4.83 | 1, 47 | .033 | 4.02 | 1, 47 | .051 | .27 |
| Social and leisuref | 3.18 | .64 | 3.00 | .76 | 3.07 | .78 | 2.37 | .51 | 7.43 | 1, 51 | .009 | 10.19 | 1, 46 | .003 | 3.64 | 1, 46 | .063 | .26 |
| Baseline and time 3 (6 months postpartum) | ||||||||||||||||||
| EPDSc | 18.1 | 3.8 | 13.2 | 5.8 | 18.9 | 3.4 | 3.6 | 3.2 | 21.51 | 1, 51 | <.001 | 184.22 | 1, 44 | <.001 | 46.18 | 1, 44 | <.001 | .89 |
| BDId | 25.9 | 11.1 | 20.8 | 10.5 | 24.3 | 10.3 | 6.0 | 4.7 | 17.70 | 1, 51 | <.001 | 38.49 | 1, 44 | <.001 | 11.56 | 1, 44 | .002 | .47 |
| BAIe | 16.3 | 10.5 | 11.8 | 6.6 | 14.4 | 11.0 | 3.6 | 5.3 | 7.83 | 1, 51 | .007 | 18.33 | 1, 44 | <.001 | 3.04 | 1, 44 | .088 | .24 |
| Social and leisuref | 3.18 | .64 | 3.14 | .77 | 3.07 | .78 | 2.12 | .44 | 17.20 | 1, 51 | <.001 | 13.27 | 1, 44 | <.001 | 11.01 | 1, 44 | .002 | .46 |
A score of >12 indicates the presence of depression.
Cohen’s d computed from the interaction term estimate.
Edinburgh Postnatal Depression Scale. Possible scores range from 0 to 30, with higher scores indicating more symptoms; a score <10 indicates remission.
Beck Depression Inventory. Possible scores range from 0 to 63, with higher scores indicating more symptoms; a score <9 indicates remission.
Beck Anxiety Inventory. Possible scores range from 0 to 63, with higher scores indicating more symptoms; a score <7 indicates remission.
Social and leisure domain on the Social Adjustment Scale. Possible scores range from 1 to 5, with higher scores indicating greater impairment; a score <2.2 indicates remission.
Finally, when asked about taking care of the new baby at six months postpartum, mothers in the IPT-B group were significantly more likely than mothers in the usual care group to report that they and their family members thought they were doing a good job in taking care of their baby’s needs and engaging in physical contact and play with their baby (1.47±.18 versus 1.78±.26, respectively; possible scores range from 1 to 5, with higher scores indicating greater impairment) (t=4.47, df=42, p<.001, d=1.35).
Discussion
This study demonstrates that among pregnant women with low incomes who scored >12 on the EPDS in a public care obstetrics and gynecology clinic, those who were randomly assigned to receive enhanced IPT-B and maintenance IPT, compared with those assigned to usual care, obtained significantly greater reductions in depression diagnoses and depressive symptoms before childbirth (three months after baseline) and at six months postpartum and showed significant improvements in social functioning at six months postpartum. There was a trend showing that social functioning and anxiety symptoms also improved more in the IPT-B group than in the usual care group between baseline and three months postbaseline (before childbirth), but these findings were not significant (p=.063 and .051). We were also particularly interested in the prevalence of anxiety disorders among our participants, given the stressful context of their lives and the empirical evidence that comorbid anxiety delays treatment response to IPT for recurrent major depression (59). Inasmuch as 56% of the IPT-B participants had at least one anxiety disorder, including 28% with PTSD and 20% with panic disorder, we might expect that they would show a slower or minimal response to treatment (41), but this did not appear to be the case. Two possible reasons exist for the timely response on the part of participants with comorbid anxiety: first, the behavioral activation component, as well as the shortened time frame, of enhanced IPT-B may have activated these participants to take more immediate control of stressful situations, thereby tending to reduce their anxiety symptoms, and second, the IPT maintenance phase may have provided reinforcement for the coping efficacy that they had achieved during the acute phase, thus maintaining the reduction in anxiety over time.
Although these results suggest that enhanced IPT-B is a promising intervention for this population, our randomized study had limitations. First, this report is based on data obtained from a small sample of low-income participants with depression who were not on antidepressant medication when they entered the study during the mid-trimester of pregnancy and, therefore, may not be generalizable to other pregnant, low-income African-American and white women with depression. Further, five women assigned to enhanced IPT-B did not enter treatment and three dropped out. Perhaps providing these women with a broader choice of antidepressant treatments, including psychotherapy or pharmacotherapy, might help to engage and retain them in treatment.
Second, to complete study assessments, the independent raters took extra time and effort to reestablish contact with participants in the enhanced usual care group who did not receive the engagement session and were more difficult to reach than patients in the enhanced IPT-B group. (Note that there were no group differences, however, in rates of study dropout or missing data.) Because of the clear differences encountered in being able to assess participants in both groups, study raters were less likely to remain blind to a participant’s treatment condition. Even though this limitation poses a threat to internal validity, we note that the measures of depressive symptoms, anxiety symptoms, and social functioning used by raters were fully structured, leaving little room for subjective judgment. Further, there was a high concordance between self-report measures and interviewer-administered measures (that is, SCID). For these reasons, it is difficult to attribute the overall pattern of results observed across two time periods to rater expectancy bias.
Third, another limitation is that our study did not compare two active psychotherapies. We thought that comparing psychotherapies would require very large sample sizes and commitment of resources, which seemed premature given previous evidence that it was difficult to engage low-income women with depression in an adequate dose of psychotherapy (18). Rather, at this phase of our research, our primary aim was to test a health services model of care designed to address barriers to care and to enhance exposure of pregnant, low-income women to an evidence-based psychotherapy for depression, compared with enhanced usual care. Based on the promising initial findings for enhanced IPT-B, future research should examine whether this intervention performs as well as another psychotherapeutic treatment for perinatal depression. Finally, we did not decompose the effects of the multiple components of enhanced IPT-B on clinical and functional outcomes. We thought it critical to first determine whether the multicomponent intervention yielded robust effects before disaggregating its components to determine which are more effective for specific outcomes. This is a matter for future research.
Conclusions
Despite these limitations, findings from the study presented here suggest that culturally relevant, enhanced IPT-B ameliorates depression during pregnancy and prevents depressive relapse and improves social functioning up to six months postpartum in a difficult-to-engage, non–treatment-seeking population. At the same time, enhanced IPT-B may contribute to reducing racial and economic disparities in access to and engagement in mental health treatment. That is, the combined data from this study and a previous report (36) suggest that a vulnerable, at-risk population—pregnant women with depression who are socioeconomically disadvantaged—can be engaged and retained in a brief, evidence-based psychotherapy and can obtain positive treatment outcomes before childbirth and at six months postpartum, compared with their peers assigned to enhanced usual care. It is noteworthy that participants in the enhanced IPT-B group, for the most part, recovered from major depression during pregnancy and stayed well through six months postpartum, an achievement that likely would confer benefits on the development of their newborn child.
Acknowledgments
This work was supported by grant K23-MH67595 from the National Institute of Mental Health, a grant from the Staunton Farm Foundation, and grant MO1-RR000056 from the General Clinical Research Centers, National Center for Research Resources. The authors thank Pam Dodge, R.N., M.S.N., for collaborating on recruiting pregnant women with depression.
Dr. Swartz has received grant support and serves on the advisory board for Bristol-Myers and has received honoraria from Servier and Astra Zeneca. Dr. Frank serves on the advisory board for Servier.
Footnotes
Portions of this article were presented at the Second International Conference on Interpersonal Psychotherapy, November 12–14, 2006, Toronto, Canada, at the 19th National Institute of Mental Health Research Conference on Mental Health Services, July 23–24, 2007, Washington, D.C., and at the Society for Social Work and Research 12th Annual Conference, “Research That Matters,” January 17–20, 2008, Washington, D.C.
disclosures
The other authors report no competing interests.
Contributor Information
Nancy K. Grote, Email: ngrote@u.washington.edu, School of Social Work, University of Washington, Campus Box 354900, 4101 15th Ave. East, Seattle, WA 98105.
Holly A. Swartz, Department of Psychiatry, University of Pittsburgh
Sharon L. Geibel, Office of Child Development, University of Pittsburgh
Allan Zuckoff, Department of Psychiatry, University of Pittsburgh
Patricia R. Houck, Department of Psychiatry, University of Pittsburgh
Ellen Frank, Department of Psychiatry, University of Pittsburgh
References
- 1.Moore GA, Cohn JF, Campbell SB. Infant affective responses to mother’s still face at 6 months differentially predict externalizing and internalizing behaviors at 18 months. Developmental Psychology. 2001;37:706–714. [PubMed] [Google Scholar]
- 2.Murray L, Cooper P. The role of infant and maternal factors in postpartum depression, mother-infant interactions, and infant outcome. In: Murray L, Cooper P, editors. Postpartum Depression and Child Development. New York: Guilford; 1997. [Google Scholar]
- 3.Areias ME, Kumar R, Barros H, et al. Correlates of postnatal depression in mothers and fathers. British Journal of Psychiatry. 1996;169:36–41. doi: 10.1192/bjp.169.1.36. [DOI] [PubMed] [Google Scholar]
- 4.Kumar R, Robson KM. A prospective study of emotional disorders in childbearing women. British Journal of Psychiatry. 1984;144:35–47. doi: 10.1192/bjp.144.1.35. [DOI] [PubMed] [Google Scholar]
- 5.O’Hara M, Swain A. Rates and risk of postpartum depression: a meta-analysis. International Review of Psychiatry. 1996;8:37–54. [Google Scholar]
- 6.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 7.Evans J, Heron J, Francomb H, et al. Cohort study of depressed mood during pregnancy and after childbirth. British Medical Journal. 2001;323:257–260. doi: 10.1136/bmj.323.7307.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gavin N, Gaynes B, Lohr K, et al. Perinatal depression: a systematic review of prevalence and incidence. Obstetrics and Gynecology. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 9.Hobfoll SE, Ritter C, Lavin J, et al. Depression prevalence and incidence among inner-city pregnant and postpartum women. Journal of Consulting and Clinical Psychology. 1995;63:445–453. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- 10.Hoffman S, Hatch MC. Depressive symptomatology during pregnancy: evidence for an association with decreased fetal growth in pregnancies of lower social class women. Health Psychology. 2000;19:535–543. [PubMed] [Google Scholar]
- 11.Marcus S, Flynn H, Blow F, et al. Depressive symptoms among pregnant women screened in obstetrics settings. Journal of Women’s Health. 2003;12:373–380. doi: 10.1089/154099903765448880. [DOI] [PubMed] [Google Scholar]
- 12.Scholle SH, Hasket RF, Hanusa BH, et al. Addressing depression in obstetrics/gynecology practice. General Hospital Psychiatry. 2003;25:83–90. doi: 10.1016/s0163-8343(03)00006-9. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Bergland P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 14.Siefert K, Bowman PJ, Heflin CM, et al. Social and environmental predictors of maternal depression in current and recent welfare recipients. American Journal of Orthopsychiatry. 2000;70:510–522. doi: 10.1037/h0087688. [DOI] [PubMed] [Google Scholar]
- 15.Stratton K, Howe C, Battaglia F, editors. Fetal Alcohol Syndrome: Diagnosis, Epidemiology, Prevention, and Treatment. Washington, DC: Institute of Medicine; 1996. [Google Scholar]
- 16.Azocar F, Miranda J, Dwyer EV. Treatment of depression in disadvantaged women. Women and Therapy. 1996;18:91–105. [Google Scholar]
- 17.Heath C, Yonkers K. Somatic treatments in depression: concerns during pregnancy and breastfeeding. In: Yonkers K, Little B, editors. Management of Psychiatric Disorders in Pregnancy. New York: Oxford University Press; 2001. [Google Scholar]
- 18.Miranda J, Chung JY, Green BL, et al. Treating depression in predominantly low-income young minority women: a randomized controlled trial. JAMA. 2003;290:57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- 19.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 20.Diamond RJ, Factor RM. Treatment-resistant patients or a treatment-resistant system? Hospital and Community Psychiatry. 1994;45:197. doi: 10.1176/ps.45.3.197. [DOI] [PubMed] [Google Scholar]
- 21.Hunt C, Andrews G. Drop-out rate as a performance indicator in psychotherapy. Acta Psychiatrica Scandinavica. 1992;85:275–278. doi: 10.1111/j.1600-0447.1992.tb01469.x. [DOI] [PubMed] [Google Scholar]
- 22.Belle D. Poverty and women’s mental health. American Psychologist. 1990;45:385–389. [Google Scholar]
- 23.Grote NK, Swartz HA, Zuckoff A. Enhancing interpersonal psychotherapy for mothers and expectant mothers on low incomes: additions and adaptations. Journal of Contemporary Psychotherapy. 2008;38:23–33. doi: 10.1007/s10879-007-9065-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frank E, Kupfer DJ, Cornes C, et al. Maintenance interpersonal psychotherapy for recurrent depression. In: Klerman G, Weissman MM, editors. New Applications of Interpersonal Psychotherapy. Washington, DC: American Psychiatric Press; 1993. [Google Scholar]
- 25.Klerman G, Weissman M, Rounsaville B, et al. Interpersonal Psychotherapy of Depression. London: Aronson; 1984. [Google Scholar]
- 26.Weissman M, Prusoff B, Demascio A, et al. The efficacy of drugs and psychotherapy in the treatment of acute depressive episodes. American Journal of Psychiatry. 1979;136:555–558. [PubMed] [Google Scholar]
- 27.Weissman M, Klerman G, Prusoff B, et al. Depressed outpatients: results after one year of treatment with drugs and/or interpersonal psychotherapy. Archives of General Psychiatry. 1981;38:51–55. doi: 10.1001/archpsyc.1981.01780260053005. [DOI] [PubMed] [Google Scholar]
- 28.Klerman GL, Weissman MM. Interpersonal psychotherapy (IPT) and drugs in the treatment of depression. Pharmacopsychiatry. 1987;20:3–7. doi: 10.1055/s-2007-1017067. [DOI] [PubMed] [Google Scholar]
- 29.Kupfer D, Frank E, Perel J, et al. Five-year outcomes for maintenance therapies in recurrent depression. Archives of General Psychiatry. 1992;49:769–773. doi: 10.1001/archpsyc.1992.01820100013002. [DOI] [PubMed] [Google Scholar]
- 30.Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. American Journal of Psychiatry. 2003;160:555–562. doi: 10.1176/appi.ajp.160.3.555. [DOI] [PubMed] [Google Scholar]
- 31.O’Hara MW, Stuart S, Gorman LL, et al. Efficacy of interpersonal psychotherapy for postpartum depression. Archives of General Psychiatry. 2000;57:1039–1045. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- 32.Grote NK, Bledsoe SE, Swartz HA, et al. Feasibility of providing culturally relevant, brief interpersonal psychotherapy for antenatal depression in an obstetrics clinic: a pilot study. Research on Social Work Practice. 2004;14:397–407. [Google Scholar]
- 33.Swartz HA, Frank E, Shear MK, et al. A pilot study of brief interpersonal psychotherapy for depression among women. Psychiatric Services. 2004;55:448–450. doi: 10.1176/appi.ps.55.4.448. [DOI] [PubMed] [Google Scholar]
- 34.Swartz HA, Frank E, Zuckoff A, et al. Brief interpersonal psychotherapy for depressed mothers whose children are seeking psychiatric treatment. American Journal of Psychiatry. 2008;165:1155–1162. doi: 10.1176/appi.ajp.2008.07081339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Swartz HA, Zuckoff A, Frank E, et al. An open-label trial of enhanced brief interpersonal psychotherapy in depressed mothers whose children are receiving psychiatric treatment. Depression and Anxiety. 2006;23:398–404. doi: 10.1002/da.20212. [DOI] [PubMed] [Google Scholar]
- 36.Grote NK, Zuckoff A, Swartz HA, et al. Engaging women who are depressed and economically disadvantaged in mental health treatment. Social Work. 2007;52:295–308. doi: 10.1093/sw/52.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 38.Beck AT, Steer RA. Manual for the Beck Depression Inventory. San Antonio, Tex: Psychological Corporation; 1993. [Google Scholar]
- 39.Oliver JM, Simmons ME. Depression as measured by the DSM–III and the Beck Depression Inventory in an unselected adult population. Journal of Consulting and Clinical Psychology. 1984;52:892–898. doi: 10.1037//0022-006x.52.5.892. [DOI] [PubMed] [Google Scholar]
- 40.Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 41.Leyfer O, Ruberg J. Woodruff-Borden J: Examination of the utility of the Beck Anxiety Inventory and its factors as a screener for anxiety disorders. Journal of Anxiety Disorders. 2006;20:444–458. doi: 10.1016/j.janxdis.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 42.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 43.Weissman M. SAS-SR Social Adjustment Scale-Self-Report: Technical Manual. North Tonawanda, NY: Multi-Health Systems; 1999. [Google Scholar]
- 44.Weissman MM, Prosoff B, Thompson W, et al. Social adjustment by self-report in a community sample and in psychiatric outpatients. Journal of Nervous and Mental Disease. 1978;166:317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- 45.First M, Spitzer R, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) New York: New York State Psychiatric Institute, Biometrics Research Department; 1995. [Google Scholar]
- 46.Robins LN, Cottler L, Bucholz K. DIS for DSM-IV. St Louis, Mo: Washington University; 1995. [Google Scholar]
- 47.O’Hara M, Hoffman J, Phillips L, et al. Adjustment in postpartum women: the Postpartum Adjustment Questionnaire. Psychological Assessment. 1992;4:160–169. [Google Scholar]
- 48.Zuckoff A, Swartz HA, Grote NK. Motivational interviewing as a prelude to psychotherapy of depression. In: Arkowitz H, Westra H, Miller WR, et al., editors. Motivational Interviewing in the Treatment of Psychological Psychological Problems. New York: Guilford; 2008. [Google Scholar]
- 49.Kupfer D. Long-term treatment of depression. Journal of Clinical Psychiatry. 1991;52:28–34. [PubMed] [Google Scholar]
- 50.Miranda J, Azocar F, Organista KC, et al. Treatment of depression among impoverished primary care patients from ethnic minority groups. Psychiatric Services. 2003;54:219–225. doi: 10.1176/appi.ps.54.2.219. [DOI] [PubMed] [Google Scholar]
- 51.Simon GE, Ludman EJ, Tutty S, et al. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292:935–942. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 52.Conner KO, Grote NK. A model for evaluating the cultural relevance of empirically-supported mental health interventions. Families in Society. 2008;89:1–9. doi: 10.1606/1044-3894.3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: issues for cultural adaptation and development of psychosocial treatments with Hispanics. Journal of Abnormal Child Psychology. 1995;23:67–82. doi: 10.1007/BF01447045. [DOI] [PubMed] [Google Scholar]
- 54.Mazumdar S, Tang G, Houck P, et al. Statistical analysis of longitudinal psychiatric data with dropouts. Journal of Psychiatric Research. 2007;41:1032–1041. doi: 10.1016/j.jpsychires.2006.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines: impact on depression in primary care. JAMA. 1995;273:1026–1031. [PubMed] [Google Scholar]
- 56.Unützer J, Katon W, Callahan CM, et al. Improving mood-promoting access to collaborative treatment: collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 57.Nierenberg A, DeCecco L. Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. Journal of Clinical Psychiatry. 2001;62 suppl 16:5–9. [PubMed] [Google Scholar]
- 58.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 59.Feske U, Frank E, Kupfer DJ, et al. Anxiety as a predictor of response to interpersonal psychotherapy for recurrent major depression: an exploratory investigation. Depression and Anxiety. 1998;8:135–141. [PubMed] [Google Scholar]