The prevalence of diabetes is increasing at staggering rates. In 2007 in the United States, estimates suggested that nearly 24 million individuals had diabetes, and another 57 million were at increased clinical risk of developing this chronic disease (i.e., pre-diabetes).1 Diabetes has consistently been among the top causes of morbidity and mortality among patients with chronic disease, and the costs associated with diabetes care place significant financial burden on our health care system.2,3 Additionally, care for patients with diabetes has remained suboptimal, particularly for racial and ethnic minorities, the poor, and the uninsured.4–7 As discussed in the previous articles in this From Research to Practice section (p. 216–237), potential barriers to the provision of optimal care and patients' execution of successful self-management may include low health literacy and numeracy.
Health Literacy, Numeracy, and Diabetes Care
A growing body of evidence supports the association between limited health literacy and numeracy and poorer diabetes outcomes.8–12 Patients with diabetes and limited health literacy or numeracy are more likely to have poorer disease knowledge and symptom recognition,13,14 poorer glycemic control,8,10 greater difficulty interpreting food labels and estimating portion sizes,15,16 lower self-confidence in diabetes management (i.e., self-efficacy), fewer self-management behaviors,8,12 and poorer communication with their providers.17 Analyses comparing the influence of low literacy and numeracy together on glycemic control suggest that numeracy is more closely related to glycemic control than literacy.8,11
The challenge in caring for patients with limited health literacy and numeracy is that deficits in these skills are not always intuitively obvious to providers and educators,18 and, if these skills are not specifically assessed, such deficits may go unrecognized. Some may argue that both patients and providers may become uncomfortable with providers' attempts to evaluate patients' health literacy and numeracy status; however, evidence in the literature supports the contrary among both patients and providers.19–21
Assessing Numeracy Skills
General numeracy
As diabetes providers and educators, we often attempt to tailor clinical recommendations and counseling to the specific needs and skills of individual patients. To tailor providers' efforts to address numeracy in diabetes care, it is important to assess patients' quantitative skills. Several general numeracy measures, with a focus on the understanding of probability and risk, have been developed and validated.22–24
Numeracy is a key component of the interpretation and application of dietary information—a crucial part of diabetes care. In a cross-sectional study of 200 primary care patients, we evaluated the relationship between numeracy skills and food label comprehension.16 Erroneous food label interpretation was common and included misapplication of portion size data, confusion over extraneous details contained in food labels, and incorrect calculations. Although 77% of these patients had literacy skills of at least the ninth-grade level, only 37% of participants had math skills of at least the ninth-grade level. Interestingly, even when patients had adequate health literacy, their numeracy skills often lagged behind, thus highlighting the importance of numeracy skills as a related yet separate patient factor. Finally, in this study, patients with lower health literacy or numeracy skills were significantly more likely to have poor comprehension of food labels.
Diabetes-specific numeracy
Diabetes-specific numeracy reflects patients' applied quantitative skills within the context of diabetes care. We have developed and validated both an English and Spanish version of the Diabetes Numeracy Test (DNT).25 Numeracy skills characterized by this scale include traditional math operations (i.e., addition, subtraction, and multiplication), numerical hierarchy, fractions and percentages, and multi-step calculations, among others. The test covers a wide variety of numeracy-dependent diabetes-related self-management skills including interpretation of glucose monitoring results, calculation of carbohydrate intake, and medication management. This original version of the DNT includes 43 test items and takes patients ∼ 30–45 minutes to complete. Patients may use a calculator on the DNT to simulate a real-world situation.
In a cross-sectional study of 398 adults with diabetes, we found that patients with higher diabetes-specific numeracy skills, as measured by the DNT, had significantly greater perceived self-efficacy for diabetes self-management and greater diabetes knowledge. We also observed a modest association between higher diabetes-specific numeracy skills and better glycemic control (i.e., lower A1C).8 Nearly 70% of participants had less than a ninth-grade level of general numeracy skills, and many patients demonstrated significant diabetes-related numeracy deficits. For example, 26% could not correctly identify, among a list of glucose values, which values fell within a target range of 60–120 mg/dl. Similarly, patients struggled with questions that required multi-step application of math skills such as calculating the total carbohydrate content in a container of snack chips and understanding titration instructions for long-acting insulin regimens. For patients with low literacy and numeracy levels, even a simple exercise such as identifying the correct dosage tier on an insulin syringe using a modified analog scale proved difficult for half of the participants.
The DNT15 is a validated shorter version of the DNT that includes 15 items from the original scale. Although several studies8,11,26,27 have used the DNT or DNT15 to assess diabetes-related numeracy, the DNT15 is faster to administer and may provide better practical utility in evaluating the numeracy skills of patients with diabetes and identifying those who may benefit from more targeted materials for ongoing diabetes management.
The Diabetes Literacy and Numeracy Toolkit
Toolkit development
The Diabetes Literacy and Numeracy Education Toolkit (DLNET) was developed to help meet the need for diabetes education and management materials for all diabetic patients, but particularly for those with low literacy or numeracy skills. Details of the development of the DLNET have been described previously.28
The general content of the toolkit was based on the recommendations of the National Standards for Diabetes Self-Management Education.29 A multidisciplinary team, including experts in health literacy and numeracy, physicians, certified diabetes educators (CDEs), registered dietitians, an advanced diabetes management nurse practitioner, and a clinical pharmacist CDE, determined the specific content of the DLNET. Educators all had 10 or more years of experience in diabetes education and management. Educational psychologists from Vanderbilt University Peabody College of Education with expertise in providing instruction for people with limited math and reading skills provided important critiques for the DLNET materials. Finally, diabetes patients with varying levels of literacy and numeracy skills provided feedback on the usability of the toolkit materials.
Toolkit components
The DLNET consists of 24 distinct modules. Some of these are considered core modules in that they address topics that are relevant to nearly all people with diabetes regardless of the type or treatment regimen. Core modules cover basic information about prevention of diabetes-related complications, awareness and management of hypoglycemia, blood glucose monitoring, exercise, foot care, and nutrition.
The remaining modules contain information that is designed to be relevant to specific categories of diabetic patients or to certain patients at a particular stage of their disease process and treatment. These modules contain materials about oral medication regimens, non-insulin injectable medication regimens, insulin regimens, insulin administration, and specific strategies for medical nutrition therapy. The materials address each topic with varying levels of complexity. For instance, the insulin regimen module covers the spectrum of insulin-dosing options from the most basic (i.e., fixed or set doses of insulin) to the most complex (i.e., basal insulin plus flexible meal dosing using a ratio for carbohydrate intake and a correction factor for glucose level). Nutrition modules contain materials that range in complexity from a modified plate method approach to carbohydrate counting and food label reading. The modules that address exercise and nutrition include shared goal-setting with the objective of enhancing patients' active involvement in their care.
Importantly, even the materials covering the most complex insulin dose regimens and most sophisticated nutrition instructions are designed to be understood by patients of all literacy and numeracy skills, including those with limited skills. Principles of clear health communication guided the creation of all toolkit materials. For example, prose content was kept at the fourth- to sixth-grade reading level, pictures and graphics were used to convey information, white space was maximized, and color coding was implemented to improve patient comprehension of the materials. At the end of many modules, providers will find sections that can be used to encourage shared decision-making with patients, as well as worksheets for patients to practice and apply skills.
Toolkit utilization
The efficacy of the DLNET materials as a component of enhanced diabetes education and management was described in two concurrent randomized, controlled trials at two academic medical centers (discussed in more detail below).27 The flexibility of the DLNET materials is demonstrated with the example of one patient with a high literacy level and diabetes numeracy score who responded better to low literacy/numeracy materials than to the more sophisticated materials we anticipated he could manage.
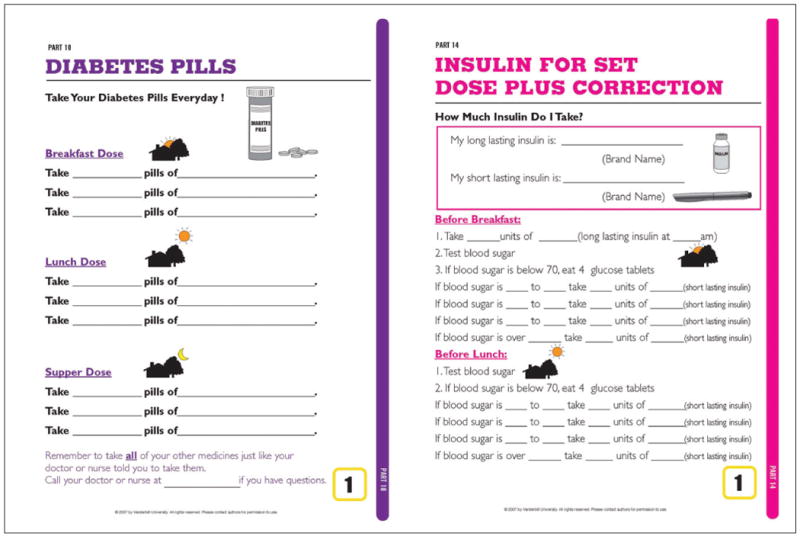
S.A. was a 49-year-old man diagnosed with diabetes at the age of 35 years and was working in the financial industry at the time of his initial visit. He had adequate literacy skills (greater than a ninth-grade reading level) and his DNT score was 88%, suggesting very good diabetes numeracy skills. At his first visit, he was taking 30 units glargine insulin at night, 12 units aspart insulin before meals, and 500 mg of metformin each night. His A1C was 10.9%. He was given the DLNET materials that cover flexible meal insulin dosing with daily basal insulin and oral medication dosing (including instructions to take metformin with meals) (Figure 1).
Figure 1. Sample DLNET module content: medication instructions and insulin management.
At his second visit, his A1C had improved to 8.1%. When asked what would help him improve his glycemic control further, he responded that, although he was capable of calculating an insulin-to-carbohydrate ratio and correction dose, it took him a long time to complete this multi-step math, and when he was busy, he was unwilling to take the time to do so. He also confessed that he had always struggled with math and was accustomed to finding ways to compensate for these difficulties. Based on this new information, he was taught to use an InsuCalc Wheel (InsuCalc, Salt Lake City, Utah) (Figure 2). This required that he estimate his carbohydrates and test his blood glucose, but the multi-step math was calculated by simply turning the wheel to line up appropriately.
Figure 2. InsuCalc wheel for calculating grams of carbohydrate.
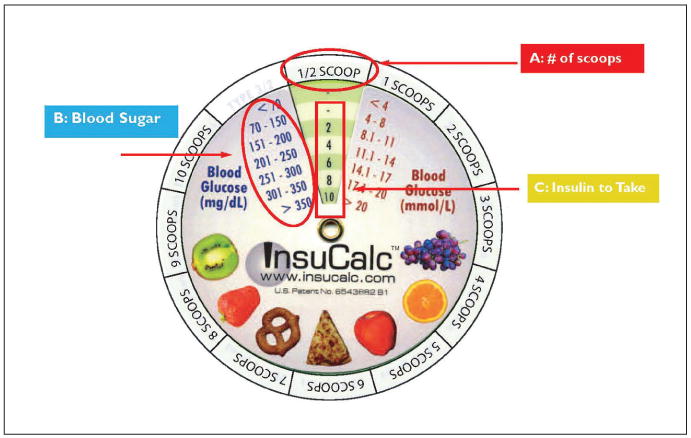
By his third visit, his A1C was 6.8%, in large part because of improved medication adherence. He was pleased with this improvement and reported that he carried the InsuCalc Wheel with him at all times.
Studies Addressing Literacy and Numeracy to Improve Diabetes Care
Recent efforts to improve diabetes processes of care (e.g., timely foot care and routine retinopathy screening) and outcome measures (e.g., A1C and hypoglycemia) by addressing limited health literacy and numeracy have shown modest success.
We have conducted a randomized, controlled trial comparing a comprehensive diabetes management program to usual care among 217 patients with type 2 diabetes.30 Intervention patients received intensive disease management from a multidisciplinary team, including clinical pharmacists and a diabetes care coordinator, with individualized care including use of techniques shown to enhance comprehension among patients with low literacy. At the 12-month follow-up, intervention patients had significant improvements in A1C, and, among those with low literacy, the intervention group patients were more likely than control patients to attain a goal A1C ≤ 7.0%. Patients with adequate literacy had similar odds of obtaining goal A1C regardless of intervention status.
In a separate study, short-term improvements in self-care behaviors, patient activation, and diabetes-related stress were seen when “Living with Diabetes” materials31 and a brief counseling session with collaborative goal-setting was used with patients with type 2 diabetes.32
Finally, we conducted two concurrent randomized, controlled trials using the DLNET materials to assess the impact of an enhanced educational intervention on glycemic control, self-efficacy, self-care behaviors, and patient satisfaction.27 Study subjects randomized to the intervention arm in these trials received materials from the DLNET toolkit as a component of enhanced diabetes education and management. Materials were customized to meet the needs of each patient at each visit. Study clinicians were provided with an assessment of patients' diabetes numeracy (measured by the DNT) before the initial visits. This score served as a guide for which materials within the DLNET would most likely be effective for each patient, particularly at their initial visit.
For most study patients, the core modules were utilized during the initial visit, and modules that address the specifics of diabetes treatment were used at subsequent visits based on individual patient needs. The range of complexity encompassed by the materials allowed maximum flexibility in customizing materials to each patient. There were instances wherein a patient's situation called for the use of simplified instructions at one point in time, followed by a transition to more complex materials at a later visit.
We found that, at the conclusion of the enhanced education program after 3 months, both intervention and control patients had significant improvements in A1C, and there was a greater improvement in A1C among intervention patients than among control patients in adjusted analyses. There were also significant improvements in self-efficacy in both groups, but no significant differences between groups were found for self-care behaviors or satisfaction measures. After an additional 3-month passive observation period, the A1C differences between groups were not sustained. Overall, this study demonstrated that a literacy- and numeracy-sensitive diabetes care program yielded modest benefit in improving glycemic control and self-efficacy compared to a standard enhanced diabetes care program, but that the results attenuated over time.
Integrating the DLNET Toolkit Into Clinical Practice
Multidisciplinary providers in the aforementioned trials using the DLNET materials found that the format and sequence of DLNET materials held the potential for clinical effectiveness and efficiency when they were utilized as a part of routine clinical practice. There are several advantages of the DLNET toolkit compared to other available diabetes educational materials. These include provision of a comprehensive, customizable array of topics that facilitate diabetes education for all patients with varying levels of literacy and numeracy skills. Our toolkit also has use for both initial care and ongoing diabetes education for established patients. Nearly every diabetes topic educators or providers will address is covered in the toolkit, reducing the need to pull information from multiple sources. Sources of diabetes education materials are often variable (e.g., pharmaceutical company, self-created, downloaded from Internet sites) and may be written at literacy levels that are too high for many diabetic patients. Furthermore, the ability to easily access two to three different materials of varying levels of sophistication that cover the same topic enhanced individualization of care. Storage of the materials as an organized set of modules also proved to be very convenient for providers.
Informal follow-up with DLNET study clinicians provided anecdotal evidence that the DLNET toolkit was user-friendly for providers and accepted by patients during the DLNET study. All of the study dietitians found the carbohydrate counting practice materials to be very useful in teaching carbohydrate counting skills. There was an added and some-what unanticipated benefit in that the step-by-step format utilized with the carbohydrate counting materials made it possible to identify which patients were unable to read a food label or sum carbohydrate grams accurately. The color coding utilized for the blood glucose log sheets was considered a benefit, but the log sheet format with mealtimes arranged along the vertical axis rather than the more typical horizontal axis was problematic for some study clinicians. DLNET study clinicians who utilized the oral medication and insulin regimen materials found these to be effective in clearly communicating instructions for medication dosing.
Although we have received requests from educators and clinicians who wished to use the DLNET materials in their practice, we have not received specific feedback about their experience. Despite this, we believe these materials can be utilized by providers and educators from all disciplines, and although the low-literacy and -numeracy format is unique, the content will be familiar to most. Overall, those who utilized the DLNET materials with diabetic patients found that the format and organization of the materials encouraged a more organized and comprehensive approach to diabetes education, allowed for identification of literacy and numeracy deficits, and provided the opportunity to optimally tailor educational materials to each patient's changing needs.
Possible limitations of the DLNET are that some of the medication information can become dated fairly quickly. As new non-insulin injectable medications become available and new formulations of preexisting drugs come on the market, the corresponding materials must be updated. Also, some DLNET study subjects failed to bring the DLNET notebook back and forth from home to clinic visits, indicating that the notebook may have proved to be too cumbersome for some patients. Nonetheless, it is fairly easy to modify existing materials and adapt them to individual needs and practice settings.
Conclusions
Diabetes care represents a unique opportunity for health care providers and educators to engage patients in a long-term therapeutic alliance in which the goals of adequate self-management and glycemic control can significantly affect quality of life and reduce the risk for diabetes-related complications.33–35 For many of our patients, significant sociodemographic barriers often hinder adequate diabetes control, including the less intuitive factors of limited health literacy and numeracy skills. In our work, we have identified significant deficits of health literacy and numeracy and have demonstrated modest improvements in various behavioral and clinical diabetes outcomes when these factors are specifically targeted during care.
To that end, we have developed tools for assessing diabetes-specific numeracy and educational materials that are geared toward patients with these limited skills and can be adapted and applied in both research and clinical settings. Use of these and other materials, as shown in Table 1, coupled with efforts to ensure effective communication during clinical encounters, is likely to yield positive clinical results and improve the diabetes experience for both patients and providers.
Table 1. Resources for Diabetes Educational and Management Materials.
| Product | Source | Internet Address |
|---|---|---|
| Health Literacy Universal Precautions Toolkit | Agency for Healthcare Research and Quality | http://www.ahrq.gov/qual/literacy |
| Diabetes Numeracy Test (DNT-15) | Vanderbilt University, Meharry Medical College | http://www.mc.vanderbilt.edu/diabetes/drtc/preventionandcontrol/tools.php |
| Diabetes Literacy and Numeracy Educational Toolkit (DLNET) | Vanderbilt University | http://www.mc.vanderbilt.edu/diabetes/drtc/preventionandcontrol/tools.php |
| A Family Physician's Practical Guide to Culturally Competent Care | U.S. Department of Health and Human Services Office of Minority Health | http://cccm.thinkculturalhealth.org |
| ACP Guide to Living With Diabetes | American College of Physicians | http://diabetes.acponline.org/clinician |
| Scientific and Technical Information: Simply Put | Centers for Disease Control and Prevention | http://www.cdc.gov/DHDSP/cdcynergy_training/content/activeinformation/resources/simpput.pdf |
Acknowledgments
The research included in this article was supported by the American Diabetes Association (Novo Nordisk Clinical Research Award), Pfizer Clear Health Communication Initiative, Vanderbilt Diabetes Research and Training Center (NIDDK 5P60DK020593), and the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Dr. White is supported by Pfizer's Fellowship in Health Literacy and Clear Health Communication Award, and Meharry Medical College's Clinical Research Education and Career Development Program (NIH NCRR CRECD 1R25RR17577). Dr. Rothman and Dr. Cavanaugh are supported by NIDDK Career Development awards (NIDDK 5K23DK065294 and K23DK080952, respectively).
When materials and topics discussed in this article were previously published, the authors have provided appropriate references. No financial support other than that stated has been received by any author.
Footnotes
In Brief: Health numeracy is an important component of health literacy that affects diabetes care. This article details current research in the field by highlighting efforts to address health literacy and numeracy as a means of improving diabetes education, self-management, and glycemic control. The authors provide evidence from their past and ongoing research in this area and offer guidelines for assessing literacy and numeracy skills in the clinical setting.
Author Contributions: All listed authors contributed significantly to the concept (RR, KW), format (KLC, RR, KW), writing (ROW, KW, KLC), and/or editing (ROW, RR, KW, KLC) of all written content.
Contributor Information
Richard O. White, Assistant professor in the Department of Internal Medicine at Meharry Medical College, Nashville, Tenn.
Kathleen Wolff, Diabetes nurse practitioner at the Vanderbilt Eskind Diabetes Center and Diabetes Research & Training Center and a clinical instructor at Vanderbilt University School of Nursing, Nashville, Tenn.
Kerri L. Cavanaugh, Assistant professor at the Vanderbilt Eskind Diabetes Center and Diabetes Research & Training Center and in the Division of Nephrology, Department of Medicine at Vanderbilt University Medical Center, Nashville, Tenn.
Russell Rothman, Associate professor at the Vanderbilt Eskind Diabetes Center and Diabetes Research & Training Center and in the Division of General Internal Medicine and Public Health at Vanderbilt University Medical Center, Nashville, Tenn.
References
- 1.Centers for Disease Control and Prevention National diabetes fact sheet: general information and national estimates on diabetes in the United States [article online[ [28 May 2010]; Available from http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf.
- 2.American Diabetes Association Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 3.Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. Natl Vital Stat Rep. 2008;56:1–120. [PubMed] [Google Scholar]
- 4.Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, Imperatore G, Narayan KM. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988–2002. Ann Intern Med. 2006;144:465–474. doi: 10.7326/0003-4819-144-7-200604040-00005. [DOI] [PubMed] [Google Scholar]
- 5.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291:335–342. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Dept. of Health and Human Services, Agency for Healthcare Research and Quality . 2007 National Healthcare Disparities Report. Rockville, Md.: U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality; 2008. [28 May 2010]. Available online from http://www.ahrq.gov/qual/qrdr07.htm#toc. [Google Scholar]
- 7.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 8.Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, Gregory RP, Fuchs L, Malone R, Cherrington A, Pignone M, DeWalt DA, Elasy TA, Rothman RL. Association of numeracy and diabetes control. Ann Intern Med. 2008;148:737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 9.Rothman R, Malone R, Bryant B, Dewalt D, Pignone M. Health literacy and diabetic control. JAMA. 2002;288:2687–2688. [PubMed] [Google Scholar]
- 10.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 11.Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care. 2009;32:1614–1619. doi: 10.2337/dc09-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karter AJ, Subramanian U, Saha C, Crosson JC, Parker MM, Swain BE, Moffet HH, Marrero DG. Barriers to insulin initiation: the translating research into action for diabetes insulin starts project. Diabetes Care. 2010;33:733–735. doi: 10.2337/dc09-1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rothman RL, Malone R, Bryant B, Wolfe C, Padgett P, DeWalt DA, Weinberger M, Pignone M. The Spoken Knowledge in Low Literacy in Diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educ. 2005;31:215–224. doi: 10.1177/0145721705275002. [DOI] [PubMed] [Google Scholar]
- 14.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 15.Huizinga MM, Carlisle AJ, Cavanaugh KL, Davis DL, Gregory RP, Schlundt DG, Rothman RL. Literacy, numeracy, and portion-size estimation skills. Am J Prev Med. 2009;36:324–328. doi: 10.1016/j.amepre.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, Shintani A, Elasy TA. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31:391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 17.Arthur SA, Geiser HR, Arriola KR, Kripalani S. Health literacy and control in the medical encounter: a mixed-methods analysis. J Natl Med Assoc. 2009;101:677–683. doi: 10.1016/s0027-9684(15)30976-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bass PF, 3rd, Wilson JF, Griffith CH, Barnett DR. Residents' ability to identify patients with poor literacy skills. Acad Med. 2002;77:1039–1041. doi: 10.1097/00001888-200210000-00021. [DOI] [PubMed] [Google Scholar]
- 19.Seligman HK, Wang FF, Palacios JL, Wilson CC, Daher C, Piette JD, Schillinger D. Physician notification of their diabetes patients' limited health literacy: a randomized, controlled trial. J Gen Intern Med. 2005;20:1001–1007. doi: 10.1111/j.1525-1497.2005.00189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ryan JG, Leguen F, Weiss BD, Albury S, Jennings T, Velez F, Salibi N. Will patients agree to have their literacy skills assessed in clinical practice? Health Educ Res. 2008;23:603–611. doi: 10.1093/her/cym051. [DOI] [PubMed] [Google Scholar]
- 21.Schlichting JA, Quinn MT, Heuer LJ, Schaefer CT, Drum ML, Chin MH. Provider perceptions of limited health literacy in community health centers. Patient Educ Couns. 2007;69:114–120. doi: 10.1016/j.pec.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:966–972. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 24.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Mockbee J, Hale FA. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huizinga MM, Elasy TA, Wallston KA, Cavanaugh K, Davis D, Gregory RP, Fuchs LS, Malone R, Cherrington A, Dewalt DA, Buse J, Pignone M, Rothman RL. Development and validation of the Diabetes Numeracy Test (DNT) BMC Health Serv Res. 2008;96:1–8. doi: 10.1186/1472-6963-8-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gerber BS, Cano AI, Caceres ML, Smith DE, Wilken LA, Michaud JB, Ruggiero LA, Sharp LK. A pharmacist and health promoter team to improve medication adherence among Latinos with diabetes. Ann Pharmacother. 2009;44:70–79. doi: 10.1345/aph.1M389. [DOI] [PubMed] [Google Scholar]
- 27.Cavanaugh K, Wallston KA, Gebretsadik T, Shintani A, Huizinga MM, Davis D, Gregory RP, Malone R, Pignone M, DeWalt D, Elasy TA, Rothman RL. Addressing literacy and numeracy to improve diabetes care: two randomized controlled trials. Diabetes Care. 2009;32:2149–2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolff K, Cavanaugh K, Malone R, Hawk V, Gregory BP, Davis D, Wallston K, Rothman RL. The Diabetes Literacy and Numeracy Education Toolkit (DLNET): materials to facilitate diabetes education and management in patients with low literacy and numeracy skills. Diabetes Educ. 2009;35:233–236. doi: 10.1177/0145721709331945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, Maryniuk M, Peyrot M, Piette JD, Reader D, Siminerio LM, Weinger K, Weiss MA. National standards for diabetes self-management education. Diabetes Care. 2009;32(Suppl. 1):S87–S94. doi: 10.2337/dc08-S087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rothman R, Malone R, Bryant B, Horlen C, DeWalt D, Pignone M. The relationship between literacy and glycemic control in a diabetes disease-management program. Diabetes Educ. 2004;30:263–273. doi: 10.1177/014572170403000219. [DOI] [PubMed] [Google Scholar]
- 31.Seligman HK, Wallace AS, DeWalt DA, Schillinger D, Arnold CL, Shilliday BB, Delgadillo A, Bengal N, Davis TC. Facilitating behavior change with low-literacy patient education materials. Am J Health Behav. 2007;31(Suppl. 1):S69–S78. doi: 10.5555/ajhb.2007.31.supp.S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wallace AS, Seligman HK, Davis TC, Schillinger D, Arnold CL, Bryant-Shilliday B, Freburger JK, DeWalt DA. Literacy-appropriate educational materials and brief counseling improve diabetes self-management. Patient Educ Couns. 2009;75:328–333. doi: 10.1016/j.pec.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.U.K. Prospective Diabetes Study Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet. 1998;352:854–865. [PubMed] [Google Scholar]
- 34.Boulton AJ. Lowering the risk of neuropathy, foot ulcers and amputations. Diabet Med. 1998;15(Suppl. 4):S57–S59. doi: 10.1002/(sici)1096-9136(1998120)15:4+<s57::aid-dia741>3.3.co;2-4. [DOI] [PubMed] [Google Scholar]
- 35.DeFronzo RA, Reasner C. The Diabetes Control and Complications Trial study: implications for the diabetic foot. J Foot Ankle Surg. 1994;33:551–556. [PubMed] [Google Scholar]


